The Impact of Different Antihypertensive Drugs on Cardiovascular Risk in Isolated Systolic Hypertension with Type 2 Diabetes Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Outcome Measurements
2.3. Statistical Analysis
3. Results
3.1. Clinical Characteristics of Patients
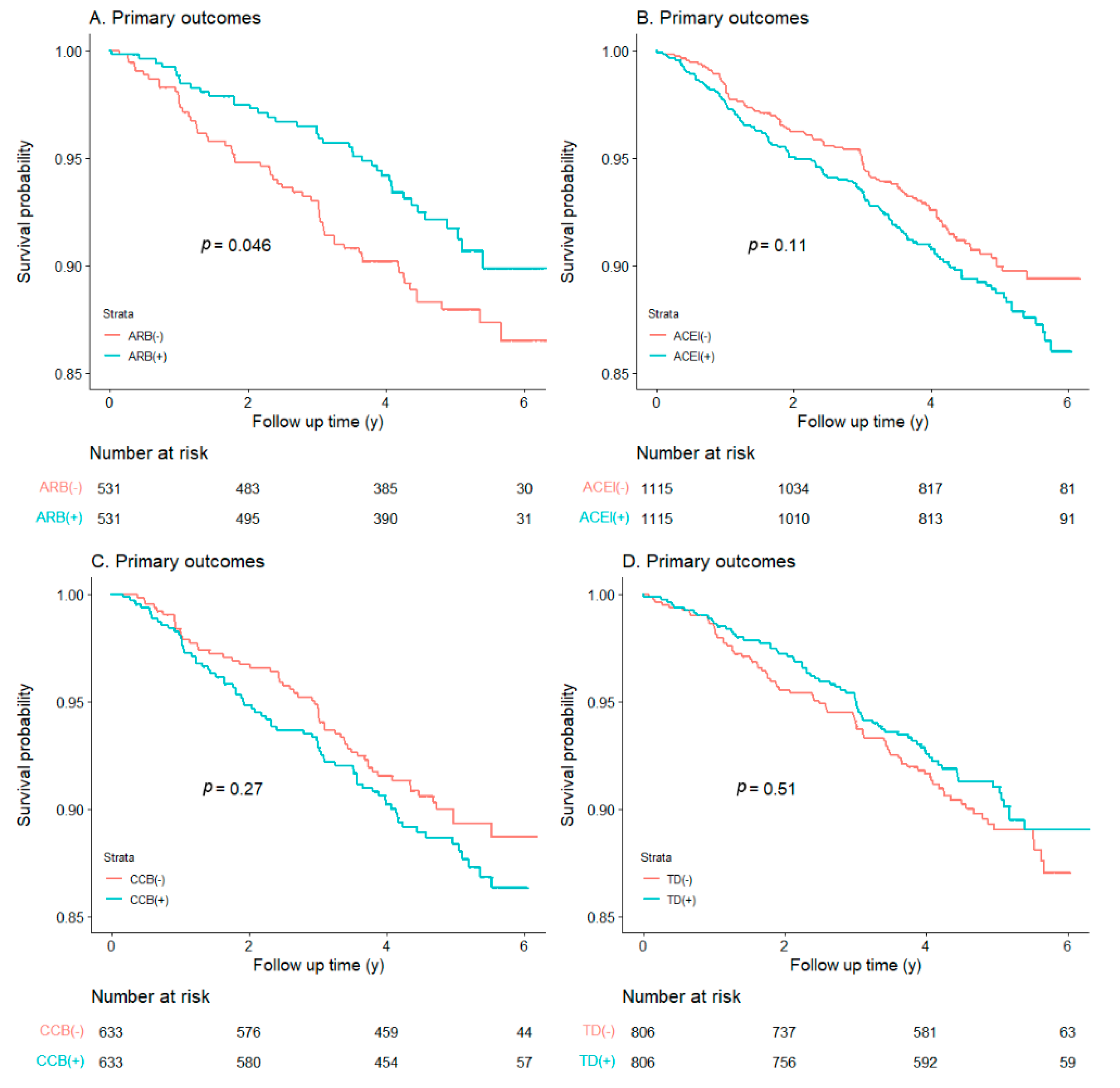
3.2. Cardiovascular Outcomes and Mortalities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| T2DM | Type 2 diabetes mellitus |
| BMI | Body Mass Index |
| HbA1c | Glycated hemoglobin A1c |
| CI | Confidence interval |
| ISH | Isolated systolic hypertension |
| ARB | Angiotensin receptor blocker |
| ACEI | Angiotensin-converting enzyme inhibitor |
| CCB | Calcium channel blocker |
| TD | Thiazide diuretics |
| PO | Primary outcomes |
| CM | Cardiovascular mortality |
| NMI | Non-fatal myocardial infarction |
| NST | Non-fatal stroke |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| CVD | Cardiovascular disease |
References
- Balakumar, P.; Maung, U.K.; Jagadeesh, G. Prevalence and Prevention of Cardiovascular Disease and Diabetes Mellitus. Pharmacol. Res. 2016, 113, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Henning, R.J. Type-2 Diabetes Mellitus and Cardiovascular Disease. Futur. Cardiol. 2018, 14, 491–509. [Google Scholar] [CrossRef] [PubMed]
- Glovaci, D.; Fan, W.; Wong, N.D. Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Curr. Cardiol. Rep. 2019, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Starzak, M.; Stanek, A.; Jakubiak, G.K.; Cholewka, A.; Cieślar, G. Arterial Stiffness Assessment by Pulse Wave Velocity in Patients with Metabolic Syndrome and Its Components: Is It a Useful Tool in Clinical Practice? Int. J. Environ. Res. Public Health 2022, 19, 10368. [Google Scholar] [CrossRef] [PubMed]
- Yano, Y.; Lloyd-Jones, D.M. Isolated Systolic Hypertension in Young and Middle-Aged Adults. Curr. Hypertens. Rep. 2016, 18, 78. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.A.; Kim, S.M.; Choi, Y.S.; Yoon, D.; Park, H.S.; Kim, H.A.; Oh, H.J.; Choi, K.M.; Lee, J.S.; Lee, J. The Prevalence and Risk Factors Associated with Isolated Untreated Systolic Hypertension in Korea: The Korean National Health and Nutrition Survey 2001. J. Hum. Hypertens. 2006, 21, 107–113. [Google Scholar] [CrossRef]
- Os, I.; Gudmundsdottir, H.; Kjeldsen, S.E.; Oparil, S. Treatment of Isolated Systolic Hypertension in Diabetes Mellitus Type 2. Diabetes Obes. Metab. 2006, 8, 381–387. [Google Scholar] [CrossRef]
- Janka, H.U.; Dirschedl, P. Systolic Blood Pressure as a Predictor for Cardiovascular Disease in Diabetes. A 5-Year Longitudinal Study. Hypertension 1985, 7, II90–II94. [Google Scholar] [CrossRef]
- Ko, G.T.; Cockram, C.S.; Chow, C.-C.; Chan, W.-B.; So, W.-Y.; Ma, R.; Osaki, R.; Chan, J.C. Effects of Body Mass Index, Plasma Glucose and Cholesterol Levels on Isolated Systolic Hypertension. Int. J. Cardiol. 2005, 101, 429–433. [Google Scholar] [CrossRef]
- Bavishi, C.; Goel, S.; Messerli, F.H. Isolated Systolic Hypertension: An Update after Sprint. Am. J. Med. 2016, 129, 1251–1258. [Google Scholar] [CrossRef]
- Adler, A.I.; Stratton, I.M.; Neil, H.A.W.; Yudkin, J.S.; Matthews, D.R.; Cull, C.A.; Wright, A.D.; Turner, R.C.; Holman, R.R. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): Prospective observational study. BMJ 2000, 321, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Aronow, W.S.; Shamliyan, T.A. Blood Pressure Targets for Hypertension in Patients with Type 2 Diabetes. Ann. Transl. Med. 2018, 6, 199. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.; Cheng, H.; Chuang, S.; Chia, Y.; Soenarta, A.A.; Van Minh, H.; Siddique, S.; Turana, Y.; Tay, J.C.; Kario, K.; et al. Isolated Systolic Hypertension in Asia. J. Clin. Hypertens 2021, 23, 467–474. [Google Scholar] [CrossRef]
- Beckett, N.S.; Peters, R.; Fletcher, A.E.; Staessen, J.A.; Liu, L.; Dumitrascu, D.; Stoyanovsky, V.; Antikainen, R.L.; Nikitin, Y.; Anderson, C.; et al. Treatment of Hypertension in Patients 80 Years of Age or Older. N. Engl. J. Med. 2008, 358, 1887–1898. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 Acc/Aha/Aapa/Abc/Acpm/Ags/Apha/Ash/Aspc/Nma/Pcna Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Accord Study Group; Buse, J.B.; Bigger, J.T.; Byington, R.P.; Cooper, L.S.; Cushman, W.C.; Friedewald, W.T. Action to Control Cardiovascular Risk in Diabetes (Accord) Trial: Design and Methods. Am. J. Cardiol. 2007, 99, S21–S33. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 Esc/Esh Guidelines for the Management of Arterial Hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Haukoos, J.S.; Lewis, R.J. The Propensity Score. JAMA 2015, 314, 1637–1638. [Google Scholar] [CrossRef]
- Hao, G.; Wang, Z.; Guo, R.; Chen, Z.; Wang, X.; Zhang, L.; Li, W. Effects of Acei/Arb in Hypertensive Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Studies. BMC Cardiovasc. Disord. 2014, 14, 148. [Google Scholar] [CrossRef]
- Kurtz, T.W. New Treatment Strategies for Patients with Hypertension and Insulin Resistance. Am. J. Med. 2006, 119, S24–S30. [Google Scholar] [CrossRef]
- Benson, S.C.; Pershadsingh, H.A.; Ho, C.I.; Chittiboyina, A.; Desai, P.; Pravenec, M.; Qi, N.; Wang, J.; Avery, M.A.; Kurtz, T.W. Identification of Telmisartan as a Unique Angiotensin Ii Receptor Antagonist with Selective Ppargamma-Modulating Activity. Hypertension 2004, 43, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Izuhara, Y.; Nangaku, M.; Inagi, R.; Tominaga, N.; Aizawa, T.; Kurokawa, K.; Strihou, C.V.Y.D.; Miyata, T. Renoprotective Properties of Angiotensin Receptor Blockers Beyond Blood Pressure Lowering. J. Am. Soc. Nephrol. 2005, 16, 3631–3641. [Google Scholar] [CrossRef] [PubMed]
- Berl, T.; Hunsicker, L.G.; Lewis, J.B.; Pfeffer, M.A.; Porush, J.G.; Rouleau, J.-L.; Drury, P.L.; Esmatjes, E.; Hricik, D.; Parikh, C.; et al. Cardiovascular Outcomes in the Irbesartan Diabetic Nephropathy Trial of Patients with Type 2 Diabetes and Overt Nephropathy. Ann. Intern. Med. 2003, 138, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Deferrari, G.; Ravera, M.; Deferrari, L.; Vettoretti, S.; Ratto, E.; Parodi, D. Renal and Cardiovascular Protection in Type 2 Diabetes Mellitus: Angiotensin Ii Receptor Blockers. J. Am. Soc. Nephrol. 2002, 13, S224–S229. [Google Scholar] [CrossRef]
- Strauss, M.H.; Hall, A.S. The Divergent Cardiovascular Effects of Angiotensin-Converting Enzyme Inhibitors and Angiotensin Ii Type 1 Receptor Blockers in Adult Patients with Type 2 Diabetes Mellitus. Can. J. Diabetes 2018, 42, 124–129. [Google Scholar] [CrossRef]
- Pai, P.-Y.; Muo, C.-H.; Sung, F.-C.; Ho, H.-C.; Lee, Y.-T. Angiotensin Receptor Blockers (Arb) Outperform Angiotensin-Converting Enzyme (Ace) Inhibitors on Ischemic Stroke Prevention in Patients with Hypertension and Diabetes—A Real-World Population Study in Taiwan. Int. J. Cardiol. 2016, 215, 114–119. [Google Scholar] [CrossRef]
- Sarafidis, P.A.; Alexandrou, M.E.; Ruilope, L.M. A Review of Chemical Therapies for Treating Diabetic Hypertension. Expert Opin. Pharmacother. 2017, 18, 909–923. [Google Scholar] [CrossRef]
- Shete, M.M. Cilnidipine: Next Generation Calcium Channel Blocker. J. Assoc. Physicians India 2016, 64, 95–99. [Google Scholar]
- Sethi, B.K.; Baruah, M.P.; Kumar, A.S. Blood Pressure Variability in Patients with Diabetes Mellitus with Hypertension: Treatment Recommendations and Role of Amlodipine. J. Assoc. Phys. India 2017, 65, 67–71. [Google Scholar]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood Pressure Lowering for Prevention of Cardiovascular Disease and Death: A Systematic Review and Meta-Analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef]
- Remonti, L.R.; Dias, S.; Leitão, C.B.; Kramer, C.K.; Klassman, L.P.; Welton, N.J.; Ades, A.; Gross, J.L. Classes of Antihypertensive Agents and Mortality in Hypertensive Patients with Type 2 Diabetes-Network Meta-Analysis of Randomized Trials. J. Diabetes its Complicat. 2016, 30, 1192–1200. [Google Scholar] [CrossRef] [PubMed]
- Nosadini, R.; Tonolo, G. Cardiovascular and Renal Protection in Type 2 Diabetes Mellitus: The Role of Calcium Channel Blockers. J. Am. Soc. Nephrol. 2002, 13, S216–S223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Emeriau, J.-P.; Knauf, H.; Pujadas, J.O.; Calvo-Gomez, C.; Abate, G.; Leonetti, G.; Chastang, C. A Comparison of Indapamide Sr 1.5 Mg with Both Amlodipine 5 Mg and Hydrochlorothiazide 25 Mg in Elderly Hypertensive Patients: A Randomized Double-Blind Controlled Study. J. Hypertens. 2001, 19, 343–350. [Google Scholar] [CrossRef]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; Lefevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (Jnc 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 Esh/Esc Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (Esh) and of the European Society of Cardiology (Esc). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef] [PubMed]
- de Boer, I.H.; Bangalore, S.; Benetos, A.; Davis, A.M.; Michos, E.D.; Muntner, P.; Rossing, P.; Zoungas, S.; Bakris, G. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care 2017, 40, 1273–1284. [Google Scholar] [CrossRef]
- Ravioli, S.; Bahmad, S.; Funk, G.-C.; Schwarz, C.; Exadaktylos, A.; Lindner, G. Risk of Electrolyte Disorders, Syncope, and Falls in Patients Taking Thiazide Diuretics: Results of a Cross-Sectional Study. Am. J. Med. 2021, 134, 1148–1154. [Google Scholar] [CrossRef]
- Scheen, A.J. Type 2 Diabetes and Thiazide Diuretics. Curr. Diabetes Rep. 2018, 18, 6. [Google Scholar] [CrossRef]
- Price, A.L.; Lingvay, I.; Szczepaniak, E.W.; Wiebel, J.; Victor, R.G.; Szczepaniak, L.S. The Metabolic Cost of Lowering Blood Pressure with Hydrochlorothiazide. Diabetol. Metab. Syndr. 2013, 5, 35. [Google Scholar] [CrossRef]
- Eriksson, J.W.; Jansson, P.-A.; Carlberg, B.; Hägg, A.; Kurland, L.; Svensson, M.K.; Ahlström, H.; Ström, C.; (Lönn), L.L.; Öjbrandt, K.; et al. Hydrochlorothiazide, but Not Candesartan, Aggravates Insulin Resistance and Causes Visceral and Hepatic Fat Accumulation: The Mechanisms for the Diabetes Preventing Effect of Candesartan (Medica) Study. Hypertension 2008, 52, 1030–1037. [Google Scholar] [CrossRef]
| Characteristics | ARB | pValue | ACEI | pValue | ||
| (−) | (+) | (−) | (+) | |||
| Number | 531 | 531 | 1115 | 1115 | ||
| Age, mean (SD) | 64.83 (6.95) | 64.97 (6.74) | 0.741 | 64.55 (6.74) | 64.58 (6.63) | 0.910 |
| Female, no. (%) | 273 (51.4) | 254 (47.8) | 0.269 | 496 (44.5) | 458 (41.1) | 0.113 |
| Glycated hemoglobin, mean (SD) | 8.11 (0.93) | 8.13 (0.96) | 0.694 | 8.23 (1.04) | 8.24 (0.98) | 0.890 |
| BMI, mean (SD) | 32.43 (5.27) | 32.62 (5.52) | 0.570 | 32.16 (5.51) | 32.24 (5.30) | 0.723 |
| Smoke lifetime, no. (%) | 243 (45.8) | 245 (46.1) | 0.951 | 547 (49.1) | 546 (49.0) | 1.000 |
| Lipid, mean (SD) | ||||||
| LDL | 104.79 (33.72) | 101.81 (33.15) | 0.146 | 105.99 (34.18) | 105.55 (33.29) | 0.755 |
| HDL | 43.08 (12.34) | 43.15 (12.35) | 0.921 | 43.25 (12.03) | 43.10 (11.77) | 0.726 |
| Triglyceride | 183.73 (168.81) | 186.82 (127.36) | 0.737 | 187.71 (135.27) | 186.28 (162.61) | 0.822 |
| BP, mean (SD) | ||||||
| SBP | 151.93 (10.57) | 151.75 (11.10) | 0.788 | 151.51 (10.53) | 151.91 (10.74) | 0.368 |
| DBP | 76.46 (8.25) | 76.25 (8.18) | 0.668 | 76.90 (7.74) | 76.78 (8.10) | 0.724 |
| Race, no. (%) | 0.322 | 0.896 | ||||
| White | 293 (55.2) | 310 (58.4) | 683 (61.3) | 687 (61.6) | ||
| Non-White | 238 (44.8) | 221 (41.6) | 432 (38.7) | 428 (38.4) | ||
| Education, no. (%) | 0.700 | 0.261 | ||||
| Less than high school | 84 (15.8) | 73 (13.7) | 176 (15.8) | 192 (17.2) | ||
| High school | 140 (26.4) | 151 (28.4) | 317 (28.4) | 298 (26.7) | ||
| Some college | 178 (33.5) | 172 (32.4) | 373 (33.5) | 346 (31.0) | ||
| College degree or higher | 129 (24.3) | 135 (25.4) | 249 (22.3) | 279 (25.0) | ||
| Intensive glycemia therapy, no. (%) | 255 (48.0) | 267 (50.3) | 0.500 | 562 (50.4) | 561 (50.3) | 1.000 |
| Previous CVD, no. (%) | 192 (32.3) | 194 (36.5) | 0.986 | 379 (34.0) | 402 (36.1) | 0.329 |
| Previous heart failure, no. (%) | 21 (4.0) | 20 (3.8) | 0.990 | 35 (3.1) | 48 (4.3) | 0.179 |
| Medicines use, no. (%) | ||||||
| Sulfonylureas | 271 (51.2) | 255 (48.0) | 0.326 | 553 (49.6) | 568 (50.9) | 0.553 |
| Biguanides | 329 (62.2) | 346 (65.2) | 0.347 | 679 (60.9) | 692 (62.1) | 0.602 |
| Meglitinide | 14 (2.6) | 11 (2.1) | 0.679 | 28 (2.5) | 33 (3.0) | 0.604 |
| Alpha-glucosidase inhibitors | 0 (0.0) | 5 (0.9) | 0.074 | 1 (0.1) | 4 (0.4) | 0.371 |
| Thiazolidinediones | 114 (21.6) | 133 (25.0) | 0.203 | 258 (23.1) | 237 (21.3) | 0.308 |
| Regular insulins | 80 (15.1) | 84 (15.8) | 0.819 | 141 (12.6) | 160 (14.3) | 0.265 |
| Statins | 328 (62.0) | 341 (64.2) | 0.125 | 690 (61.9) | 721 (64.7) | 0.188 |
| Characteristics | CCB | pValue | DT | pValue | ||
| (−) | (+) | (−) | (+) | |||
| Number | 633 | 633 | 806 | 806 | ||
| Age, mean (SD) | 65.76 (6.96) | 65.38 (6.64) | 0.321 | 64.86 (6.79) | 64.72 (6.43) | 0.680 |
| Female, no. (%) | 260 (41.1) | 267 (42.2) | 0.732 | 360 (44.7) | 363 (45.0) | 0.920 |
| Glycated hemoglobin, mean (SD) | 8.19 (0.99) | 8.17 (0.92) | 0.794 | 8.18 (1.00) | 8.19 (0.93) | 0.731 |
| BMI, mean (SD) | 32.23 (5.45) | 32.48 (5.56) | 0.404 | 32.57 (5.73) | 32.76 (5.04) | 0.467 |
| Smoke lifetime, no. (%) | 307 (48.5) | 293 (46.3) | 0.464 | 362 (44.9) | 382 (47.4) | 0.342 |
| Lipid, mean (SD) | ||||||
| LDL | 100.32 (31.01) | 102.59(31.87) | 0.205 | 103.00 (33.12) | 103.98 (34.63) | 0.561 |
| HDL | 43.45 (12.41) | 43.49 (11.66) | 0.952 | 43.24 (12.46) | 43.04 (11.29) | 0.734 |
| Triglyceride | 182.68 (147.30) | 178.13(159.05) | 0.597 | 188.07 (155.43) | 183.87 (129.08) | 0.555 |
| BP, mean (SD) | ||||||
| SBP | 153.00 (11.73) | 152.40 (10.35) | 0.335 | 152.18 (10.59) | 152.12 (11.10) | 0.916 |
| DBP | 75.73 (8.29) | 75.39 (8.51) | 0.472 | 76.55 (7.72) | 76.61 (8.21) | 0.876 |
| Race, no. (%) | 0.533 | 0.841 | ||||
| White | 353 (55.8) | 365 (57.7) | 450 (55.8) | 445 (55.2) | ||
| Non-White | 280 (44.2) | 268 (42.3) | 356 (44.2) | 361 (44.8) | ||
| Education, no. (%) | 0.471 | 0.782 | ||||
| Less than high school | 117 (18.5) | 120 (19.0) | 132 (16.4) | 128 (15.9) | ||
| High school | 184 (29.1) | 184 (29.1) | 233 (28.9) | 231 (28.7) | ||
| Some college | 191 (30.2) | 193 (30.5) | 263 (32.6) | 252 (31.3) | ||
| College degree or higher | 141 (22.3) | 136 (21.5) | 178 (22.1) | 195 (24.2) | ||
| Intensive glycemia therapy, no. (%) | 316 (49.9) | 302 (47.7) | 0.465 | 406 (50.4) | 411 (51.0) | 0.842 |
| Previous CVD, no. (%) | 266 (42.0) | 259 (40.9) | 0.732 | 303 (37.6) | 290 (36.0) | 0.535 |
| Previous heart failure, no. (%) | 29 (4.6) | 28 (4.4) | 1.000 | 16 (2.0) | 22 (2.7) | 0.412 |
| Medicines use, no. (%) | ||||||
| Sulfonylureas | 321 (50.7) | 322 (50.9) | 1.000 | 399 (49.5) | 404 (50.1) | 0.842 |
| Biguanides | 410 (64.8) | 403 (63.7) | 0.725 | 533 (66.1) | 535 (66.4) | 0.958 |
| Meglitinide | 25 (3.9) | 19 (3.0) | 0.443 | 20 (2.5) | 18 (2.2) | 0.870 |
| Alpha-glucosidase inhibitors | 3 (0.5) | 3 (0.5) | 1.000 | 1 (0.1) | 1 (0.1) | 1.000 |
| Thiazolidinediones | 144 (22.7) | 152 (24.0) | 0.642 | 194 (24.1) | 184 (22.8) | 0.597 |
| Regular Insulins | 98 (15.5) | 109 (17.2) | 0.447 | 131 (16.3) | 135 (16.7) | 0.840 |
| Statins | 429 (67.8) | 413 (65.2) | 0.372 | 528 (65.5) | 525 (65.1) | 0.917 |
| Antihypertensive Therapy | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| ARB (+)/ARB (−) | 0.67 (0.45, 0.99) | 0.047 | 0.66 (0.44, 0.98) | 0.040 | 0.53 (0.34, 0.83) | 0.006 |
| ACEI (+)/ACEI (−) | 1.24 (0.95, 1.61) | 0.155 | 1.22 (0.94, 1.59) | 0.126 | 1.19 (0.91, 1.54) | 0.209 |
| CCB (+)/CCB (−) | 1.21 (0.86, 1.70) | 0.268 | 1.27 (0.90, 1.78) | 0.173 | 1.23 (0.87, 1.73) | 0.245 |
| TD (+)/TD (−) | 0.89 (0.66, 1.23) | 0.508 | 0.90 (0.66, 1.23) | 0.503 | 0.88 (0.64, 1.21) | 0.438 |
| Outcomes | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Cardiovascular mortality | 0.31 (0.15, 0.66) | 0.002 | 0.30 (0.14, 0.64) | 0.002 | 0.32 (0.18, 0.90) | 0.004 |
| Non-fatal myocardial infarction | 0.87 (0.53, 1.45) | 0.605 | 0.87 (0.52, 1.44) | 0.576 | 0.89 (0.53, 1.52) | 0.692 |
| Non-fatal stroke | 1.01 (0.38, 2.71) | 0.977 | 1.01 (0.38, 2.72) | 0.977 | 1.04 (0.38, 2.84) | 0.933 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, M.; Lin, W.; Ma, T.; Luo, Y.; Xie, H.; Cheng, X.; Bai, Y. The Impact of Different Antihypertensive Drugs on Cardiovascular Risk in Isolated Systolic Hypertension with Type 2 Diabetes Patients. J. Clin. Med. 2022, 11, 6486. https://doi.org/10.3390/jcm11216486
Gao M, Lin W, Ma T, Luo Y, Xie H, Cheng X, Bai Y. The Impact of Different Antihypertensive Drugs on Cardiovascular Risk in Isolated Systolic Hypertension with Type 2 Diabetes Patients. Journal of Clinical Medicine. 2022; 11(21):6486. https://doi.org/10.3390/jcm11216486
Chicago/Turabian StyleGao, Ming, Wenrui Lin, Tianqi Ma, Yi Luo, Hejian Xie, Xunjie Cheng, and Yongping Bai. 2022. "The Impact of Different Antihypertensive Drugs on Cardiovascular Risk in Isolated Systolic Hypertension with Type 2 Diabetes Patients" Journal of Clinical Medicine 11, no. 21: 6486. https://doi.org/10.3390/jcm11216486
APA StyleGao, M., Lin, W., Ma, T., Luo, Y., Xie, H., Cheng, X., & Bai, Y. (2022). The Impact of Different Antihypertensive Drugs on Cardiovascular Risk in Isolated Systolic Hypertension with Type 2 Diabetes Patients. Journal of Clinical Medicine, 11(21), 6486. https://doi.org/10.3390/jcm11216486




