Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia
Abstract
1. Introduction
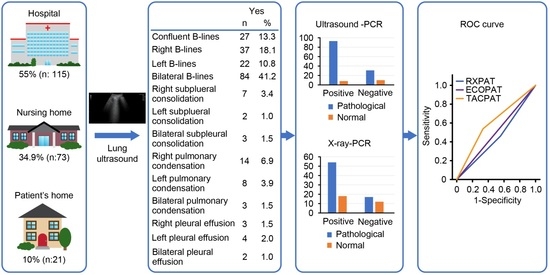
2. Materials and Methods
2.1. Patients and Methods
2.2. Statistical Analysis
2.3. Ethical Considerations
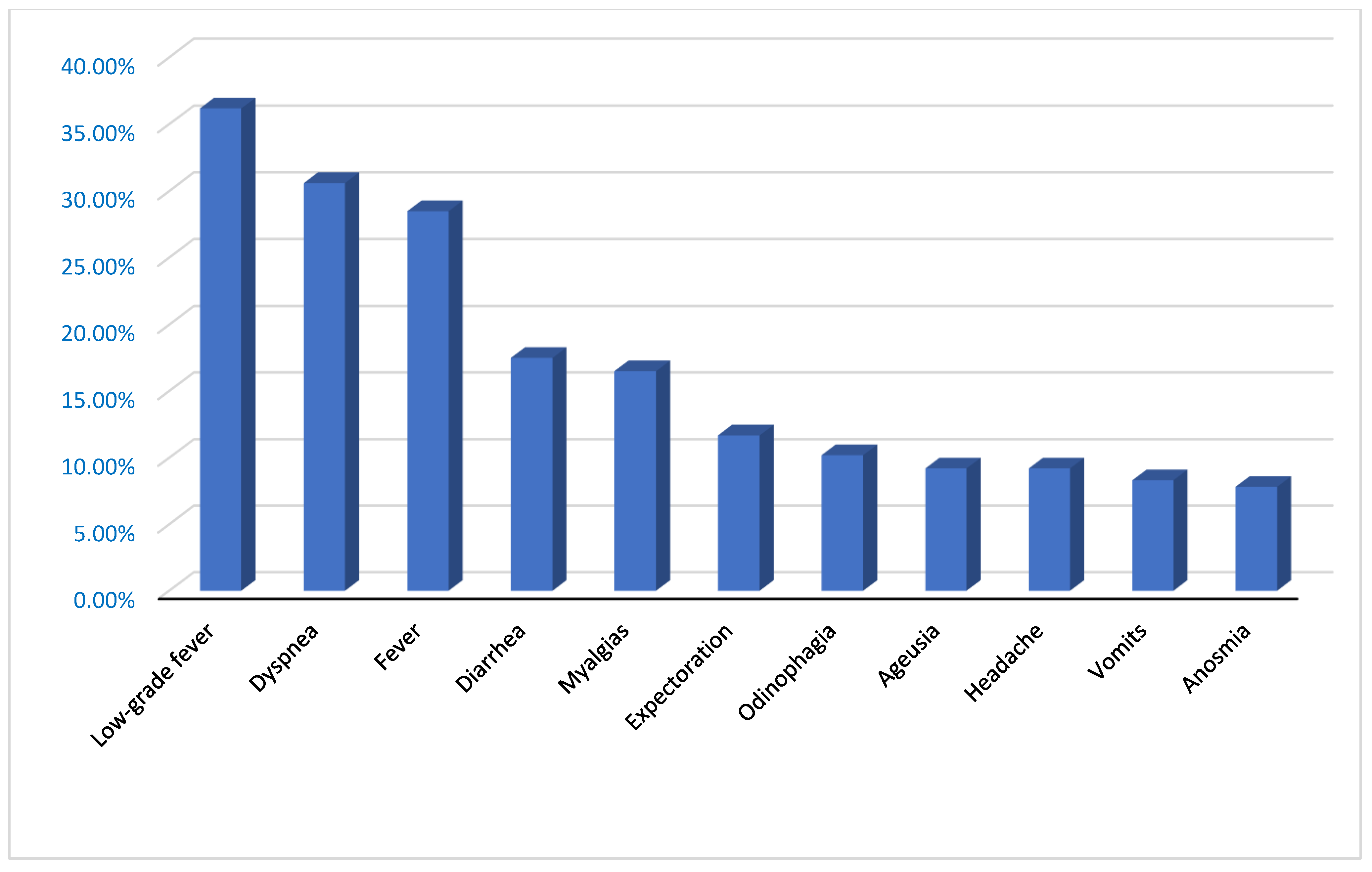
3. Results
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Spiteri, G.; Fielding, J.; Diercke, M.; Campese, C.; Enouf, V.; Gaymard, A.; Bella, A.; Sognamiglio, P.; Moros, M.J.S.; Riutort, A.N.; et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European region, 24 January to 21 February 2020. Euro Surveill. 2020, 25, 2000178. [Google Scholar] [CrossRef] [PubMed]
- Legislación Consolidada. BOE.es—BOE-A-2020-4208 Real Decreto-ley 11/2020, de 31 de Marzo, por el que se Adoptan Medidas Urgentes Complementarias en el Ámbito Social y Económico para Hacer Frente al COVID-19. Available online: https://www.boe.es/buscar/act.php?id=BOE-A-2020-4208 (accessed on 11 September 2022).
- Monge, S.; Zamalloa, P.L.; Moros, M.J.S.; Olaso, O.P.; Miguel, L.G.S.; Varela, C.; Ariza, S.R.; Torres, M.C.V.; Lucerón, M.; Yuste, P.G.; et al. Lifting COVID-19 mitigation measures in Spain (May–June 2020). Enferm. Infecc. Microbiol. Clin. 2021; in press. [Google Scholar] [CrossRef]
- De, S. Centro de Coordinación de Alertas y Emergencias Sanitarias. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Documento_GRUPOS_PERSONAS.pdf (accessed on 11 September 2022).
- Técnica, E.; En, M.; Ambiental, I.; Sostenibles, Y.P.; Aznar, M.G. Universidad Politécnica de Cartagena. Available online: https://repositorio.upct.es/bitstream/handle/10317/8979/tfg-gar-ama.pdf?sequence=1&isAllowed=y (accessed on 11 September 2022).
- Guías. Guía Clínica de Enfermedad por Coronavirus 2019 (SARS-CoV-2)—Fisterra. Available online: https://www.fisterra.com/guias-clinicas/covid-19/ (accessed on 11 September 2022).
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef]
- World Health Organization. Laboratory Testing of 2019 Novel Coronavirus (2019-nCoV) in Suspected Human Cases: Interim Guidance. 17 January 2020. Available online: https://www.who.int/publications/i/item/laboratory-testing-of-2019-novel-coronavirus-(-2019-ncov)-in-suspected-human-cases-interim-guidance-17-january-2020 (accessed on 11 September 2022).
- AEPap. Grupos. Available online: https://aepap.org/grupos/grupo-de-Patologiainfecciosa/contenido/documentos-del (accessed on 11 September 2022).
- Pan, Y.; Zhang, D.; Yang, P.; Poon, L.L.M.; Wang, Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect. Dis. 2020, 20, 411–412. [Google Scholar] [CrossRef]
- Salehi, S.; Abedi, A.; Balakrishnan, S.; Gholamrezanezhad, A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. AJR Am. J. Roentgenol. 2020, 215, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Choe, P.G.; Oh, Y.; Oh, K.J.; Kim, J.; Park, S.J.; Park, J.H.; Na, H.K.; Oh, M.D. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: Implication for infection prevention and control measures. J. Korean Med. Sci. 2020, 35, e61. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Guan, H.; Zhou, S.; Wang, Y.; Li, Q.; Zhu, T.; Hu, Q.; Xia, L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): A study of 63 patients in Wuhan, China. Eur. Radiol. 2020, 30, 3306–3309. [Google Scholar] [CrossRef] [PubMed]
- Devaux, C.A.; Rolain, J.M.; Colson, P.; Raoult, D. New insights on the antiviral effects of chloroquine against coronavirus: What to expect for COVID-19? Int. J. Antimicrob. Agents 2020, 55, 105938. [Google Scholar] [CrossRef]
- Poggio, G.A.; Mariano, J.; Gopar, L.A.; Ucar, M.E. La ecografía primero: ¿Por qué, cómo y cuándo? Rev. Argent. Radiol. 2017, 81, 192–203. [Google Scholar] [CrossRef]
- Narinx, N.; Smismans, A.; Symons, R.; Frans, J.; Demeyere, A.; Gillis, M. Feasibility of using point-of-care lung ultrasound for early triage of COVID-19 patients in the emergency room. Emerg. Radiol. 2020, 27, 663–670. [Google Scholar] [CrossRef]
- Ecografia Clinica. Evidencias en Ecografia Clinica. Available online: https://www.fesemi.org/sites/default/files/documentos/grupos/ecografia/newsletters/evid_ecog_clinica.pdf (accessed on 11 September 2022).
- Butterflynetwork.com. Handheld Portable Ultrasound Machine. Available online: https://www.butterflynetwork.com/es/ (accessed on 11 September 2022).
- Markarian, T.; Persico, N.; Roch, A.; Ahriz, D.; Taguet, C.; Birman, G.; Mahboubi, A.; Ducassou, J.; Bourenne, J.; Zieleskiewicz, L.; et al. Early assessment of patients with COVID-19 and dyspnea using lung ultrasound scoring. Emergencias 2021, 33, 354–360. [Google Scholar] [PubMed]
- Miller, A. Practical approach to lung ultrasound. BJA Educ. 2016, 16, 39–45. [Google Scholar] [CrossRef]
- Lichtenstein, D.A.; Mezière, G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest 2008, 134, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, S.D.; Ferrín, L.C.; Barrancos, I.M.S.; Salud, J.P.; Suárez, J.A.T.; Cano, J.M.M. Usefulness and reliability of point of care ultrasound in family medicine: Focused cardiac and lung ultrasound. Aten. Primaria 2019, 51, 172–183. [Google Scholar] [CrossRef]
- Comite de Bioetica de España. Informe del Comité de Bioética de España Sobre los Requisitos Ético-Legales en la Investigación con Datos de Salud y Muestras Biológicas en el Marco de la Pandemia de COVID-19. Available online: http://assets.comitedebioetica.es/files/documentacion/Informe%20CBE%20investigacion%20COVID-19.pdf (accessed on 11 September 2022).
- Volpicelli, G.; Gargani, L. Sonographic signs and patterns of COVID-19 pneumonia. Ultrasound J. 2020, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Buonsenso, D.; Perrone, T.; Briganti, D.F.; Perlini, S.; Torri, E.; Mariani, A.; Mossolani, E.E.; et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19: A simple, quantitative, reproducible method. J. Ultrasound Med. 2020, 39, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Senter, R.; Capone, F.; Pasqualin, S.; Cerruti, L.; Molinari, L.; Fonte Basso, E.; Zanforlin, N.; Previato, L.; Toffolon, A.; Sensi, C.; et al. Lung Ultrasound Patterns and Clinical-Laboratory Correlates during COVID-19 Pneumonia: A Retrospective Study from North East Italy. J. Clin. Med. 2021, 10, 1288. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Redondo, J.; Comas, C.; Pujol Salud, J.; Crespo-Pons, M.; García-Serrano, C.; Bravo, M.O.; Peruga, J.M.P. The Risk of Hospitalization in COVID-19 Patients Can Be Predicted by Lung Ultrasound in Primary Care. Int. J. Environ. Res. Public Health 2021, 18, 6083. [Google Scholar] [CrossRef]
- Gob.Es. Manejo en Atención Primaria del COVID-19. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Manejo_Atencion_Primaria_180620.pdf (accessed on 11 September 2022).
- Baena-Díez, J.M.; Gonzalez-Casafont, I.; Cordeiro-Coelho, S.; Fernández-González, S.; Rodríguez-Jorge, M.; Pérez-Torres, C.U.F.; Larrañaga-Cabrera, A.; García-Lareo, M.; de la Arada-Acebes, A.; Martín-Jiménez, E.; et al. Effectiveness of Telephone Monitoring in Primary Care to Detect Pneumonia and Associated Risk Factors in Patients with SARS-CoV-2. Healthcare 2021, 9, 1548. [Google Scholar] [CrossRef]
- Schmid, B.; Feuerstein, D.; Lang, C.N.; Fink, K.; Steger, R.; Rieder, M.; Duerschmied, D.; Busch, H.J.; Damjanovic, D. Lung ultrasound in the emergency department—A valuable tool in the management of patients presenting with respiratory symptoms during the SARS-CoV-2 pandemic. BMC Emerg. Med. 2020, 20, 96. [Google Scholar] [CrossRef] [PubMed]
- Short, J.; Acebes, C.; Rodriguez-de-Lema, G.; La Paglia, G.M.C.; Pavón, M.; Sánchez-Pernaute, O.; Vazquez, J.C.; Romero-Bueno, F.; Garrido, J.; Naredo, E. Visual versus automatic ultrasound scoring of lung B-lines: Reliability and consistency between systems. Med. Ultrason. 2019, 21, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Abu-Zidan, F.M. Point-of-care ultrasound in critically ill patients: Where do we stand? J. Emerg. Trauma Shock 2012, 5, 70–71. [Google Scholar] [CrossRef]
- Gil-Rodrigo, A.; Llorens, P.; Buendía, C.; Hernández, M.; Espinosa, B.; Ramos-Rincón, J.; Gil, A.; Martín-Sánchez, F. Capacidad diagnóstica de la ecografía clínica pulmonar en pacientes con COVID-19 diagnostic yield of point-of-care ultrasound imaging of the lung in patients with COVID-19. Emergencias 2020, 32, 340–344. [Google Scholar] [PubMed]
- Gibbons, R.C.; Magee, M.; Goett, H.; Murrett, J.; Genninger, J.; Mendez, K.; Tripod, M.; Tyner, N.; Costantino, T.G. Lung ultrasound vs. chest X-ray study for the radiographic diagnosis of COVID-19 pneumonia in a high-prevalence population. J. Emerg. Med. 2021, 60, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Nouvenne, A.; Zani, M.D.; Milanese, G.; Parise, A.; Baciarello, M.; Bignami, E.G.; Odone, A.; Sverzellati, N.; Meschi, T.; Ticinesi, A. Lung ultrasound in COVID-19 pneumonia: Correlations with chest CT on hospital admission. Respiration 2020, 99, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Maggi, L.; Biava, A.M.; Fiorelli, S.; Coluzzi, F.; Ricci, A.; Rocco, M. Lung Ultrasound: A Diagnostic Leading Tool for SARS-CoV-2 Pneumonia: A Narrative Review. Diagnostics 2021, 11, 2381. [Google Scholar] [CrossRef] [PubMed]
| Pathological or Positive | Normal or Negative | |
|---|---|---|
| PCR (n: 142) | 101 (71%) | 41 (29%) |
| Ultrasound (n: 209) | 167 (80%) | 42 (20%) |
| X-ray (n: 117) | 77 (65.8%) | 40 (34.2%) |
| Yes | No | n Total | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Confluent B-lines | 27 | 13.3 | 176 | 86.7 | 203 |
| Right unilateral B-lines | 37 | 18.1 | 167 | 81.9 | 204 |
| Left unilateral B-lines | 22 | 10.8 | 182 | 89.2 | 204 |
| Bilateral B-lines | 84 | 41.2 | 120 | 58.8 | 204 |
| Right subpleural consolidation | 7 | 3.4 | 197 | 96.6 | 204 |
| Left subpleural consolidation | 2 | 1.0 | 202 | 99.0 | 204 |
| Bilateral subpleural consolidation | 3 | 1.5 | 201 | 98.5 | 204 |
| Right pulmonary condensation | 14 | 6.9 | 190 | 93.1 | 204 |
| Left pulmonary condensation | 8 | 3.9 | 196 | 961 | 204 |
| Bilateral pulmonary condensation | 3 | 1.5 | 201 | 98.5 | 204 |
| Right pleural effusion | 3 | 1.5 | 201 | 98.5 | 204 |
| Left pleural effusion | 4 | 2.0 | 201 | 98.5 | 205 |
| Bilateral pleural effusion | 2 | 1.0 | 202 | 99.0 | 204 |
| Pathological PCR | ||||
|---|---|---|---|---|
| YES | NO | Total | ||
| Pathological Ultrasound | YES | 93 (75%) | 31 (25%) | 124 (100%) |
| NO | 8 (44.4%) | 10 (55.6%) | 18 (100%) | |
| Total | 101 (71.1%) | 41 (28.9%) | 142 (100%) | |
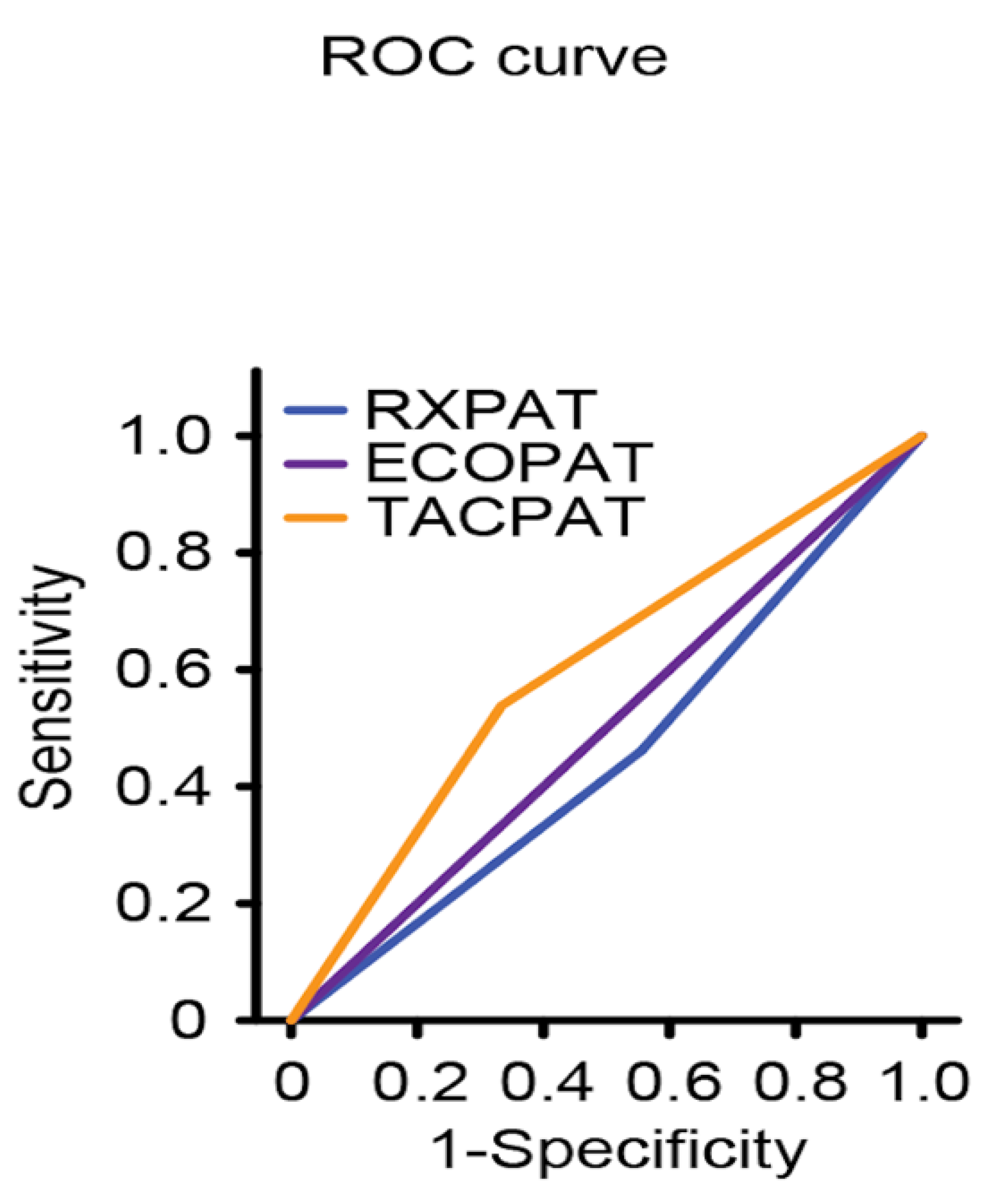
| Time between PCR and Ultrasound | |||
|---|---|---|---|
| 7–14 Days n = 102 (48%) | Less than 7 Days n = 83 (39.7%) | Less than 5 Daysn = 72 (34.4%) | |
| Sensitivity (%) | 96 (95% CI: 92–100) | 98 (95% CI: 95–102) | 98 (95% CI: 94–102) |
| Specificity (%) | 28 (95% CI 10–46) | 26 (95% CI: 8–44) | 29(95% CI: 9–48) |
| Area under the ROC curve | 0.471 (95% CI: 0.308–0.633) | 0.5 (95% CI: 0.333–0.667) | 0.5 (95% CI: 0.322–0.678) |
| Positive predictive value (%) | 80 (95% CI: 72–89) | 78 (95% CI: 68–87) | 77 (95% CI: 67–87) |
| Negative predictive value (%) | 70 (95% CI: 42–98%) | 86 (95% CI: 60–112) | 86 (95% CI: 60–112) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guzmán-García, M.B.; Mohedano-Moriano, A.; González-González, J.; Morales-Cano, J.M.; Campo-Linares, R.; Lozano-Suárez, C.; Estrada-Álvarez, T.P.; Romero-Fernández, M.M.; Aguilar-Galán, E.V.; Criado-Álvarez, J.J. Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia. J. Clin. Med. 2022, 11, 6420. https://doi.org/10.3390/jcm11216420
Guzmán-García MB, Mohedano-Moriano A, González-González J, Morales-Cano JM, Campo-Linares R, Lozano-Suárez C, Estrada-Álvarez TP, Romero-Fernández MM, Aguilar-Galán EV, Criado-Álvarez JJ. Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia. Journal of Clinical Medicine. 2022; 11(21):6420. https://doi.org/10.3390/jcm11216420
Chicago/Turabian StyleGuzmán-García, María Belén, Alicia Mohedano-Moriano, Jaime González-González, José Manuel Morales-Cano, Ricardo Campo-Linares, César Lozano-Suárez, Tyrone Paul Estrada-Álvarez, Mª Mar Romero-Fernández, Esther Vanesa Aguilar-Galán, and Juan José Criado-Álvarez. 2022. "Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia" Journal of Clinical Medicine 11, no. 21: 6420. https://doi.org/10.3390/jcm11216420
APA StyleGuzmán-García, M. B., Mohedano-Moriano, A., González-González, J., Morales-Cano, J. M., Campo-Linares, R., Lozano-Suárez, C., Estrada-Álvarez, T. P., Romero-Fernández, M. M., Aguilar-Galán, E. V., & Criado-Álvarez, J. J. (2022). Lung Ultrasound as a Triage Method in Primary Care for Patients with Suspected SARS-CoV-2 Pneumonia. Journal of Clinical Medicine, 11(21), 6420. https://doi.org/10.3390/jcm11216420