Psychological Distress in Patients Treated for Renal Cell Carcinoma: A Systematic Literature Review
Abstract
1. Introduction
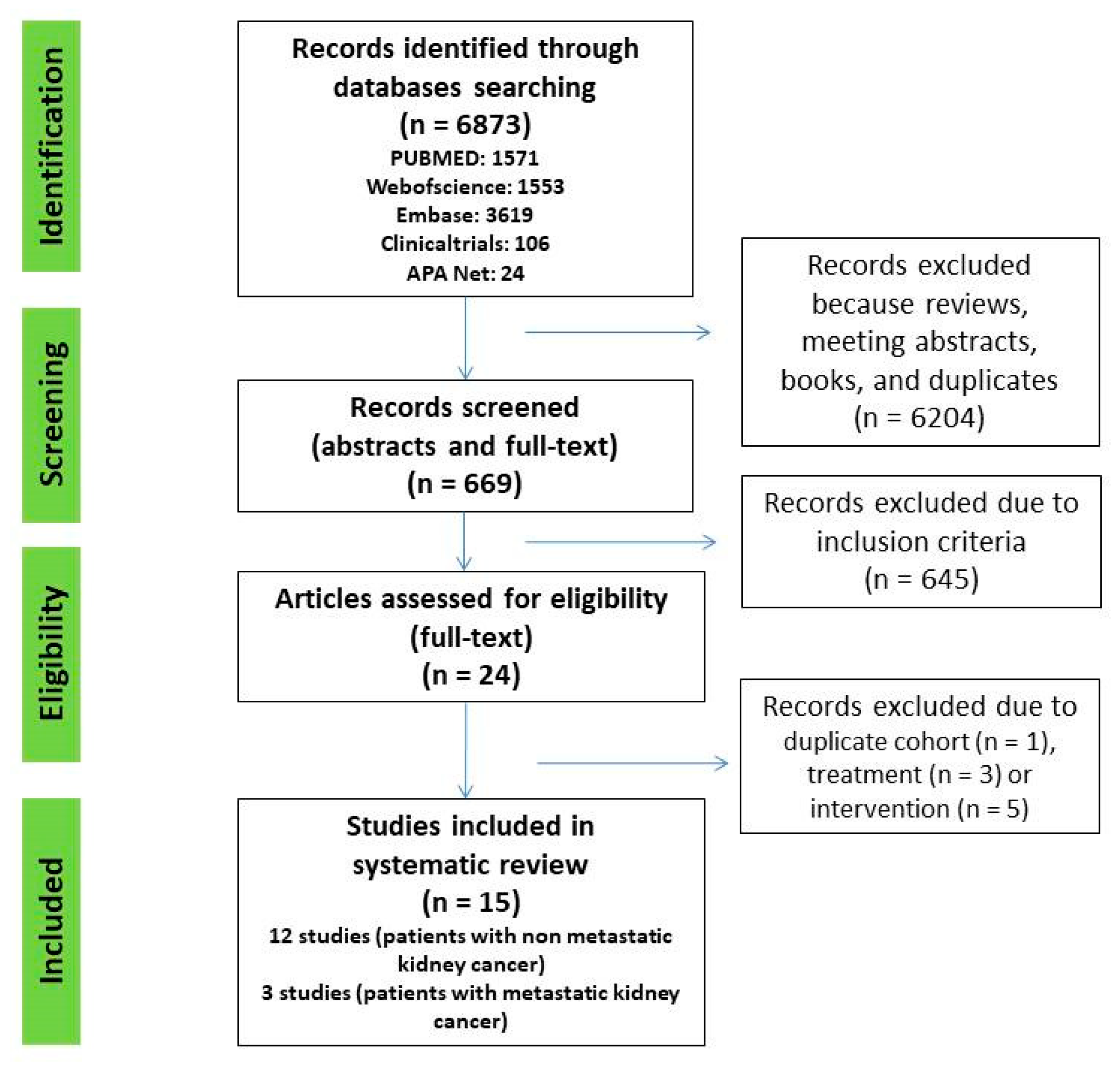
2. Materials and Methods
2.1. Protocol
2.2. Inclusion and Exclusion Criteria
2.3. Study Quality and Risk of Bias Evaluation
3. Results
3.1. Psychological Distress, Anxiety and/or Depression in Patients with Non-Metastatic Renal Cell Carcinoma
3.2. Impact of Anxiety and/or Depression on Oncological Outcomes in Patients with Non-Metastatic Renal Cell Carcinoma
3.3. Impact of Psychological Distress, Anxiety and/or Depression on Patients with Metastatic Renal Cell Carcinoma
| No. | First Author | Year | Country | Study Design | No. Patients | Patients Characteristics | Questionnaires | Results | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Bergerot et al. | 2019 [29] | United States of America | retrospective | 102 29 females (28.4%) | age ≥ 18 years, had histologically confirmed RCC, and had radiographic evidence of metastatic disease. | A touch screen–based instrument was used to assess biopsychosocial problem-related distress. The instrument surveyed 22 core items on a 5-point Likert scale ranging from 1 (not a problem) to 5 (very severe problem). Items rated ≥3 were considered to reflect high distress. | The median OS was 43.7 months (95% confidence interval [95%CI] = 35.5, 52.5) for the overall cohort; 20.0 months (95%CI = 16.0, 55.9) in patients with high distress, and 45.8 months (95%CI = 36.1, 55.5) in those with low distress (p = 0.81). | n.a |
| 2 | Wang et al. | 2018 [31] | China | prospective | 127 26 females (20.4%) | (I) diagnosed as mRCC according to clinical, imaging and pathological findings; (II) age above 18 years; (III) about to receive IFN-α treatment; (IV) life expectancy longer than 12 months; (V) able to be followed up regularly and complete the assessment questionnaires. Patients were excluded if they (I) had brain metastasis; (II) accompanied with other solid tumors or hematological malignance; (III) had uncontrolled hypertension, severe infection or primary organ failure; (IV) were pregnant or lactating, or planned for pregnancy | HADS-Anxiety score, HADS-Depression score and EORTC QLQ-C30 Scale at baseline and at 12 weeks | The percentages of anxiety and depression both increased at W12 compared with W0. Depression (43.3% vs. 31.5%, p = 0.004) and anxiety (32.3% vs. 22%, p = 0.035) | 12 weeks |
| 3 | Cohen et al. | 2012 [30] | United States of America | prospective | 202 46 females (23%) | newly diagnosed metastatic RCC, a life expectancy of greater than 4 months, a Zubrod performance status of less than or equal to 2, and no serious intercurrent illnesses. | (Centers for Epidemiologic Studies—Depression; SF-36 Health Status Survey; Duke Social Support Index; Coping Operations Preference Enquiry | CES-D scores (p = 0.05, HR = 1.5, 95%CI for HR: 1.00–2.23) were predictors for decrease survival | 1.8 years |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Ljungberg, B.; Albiges, L.; Abu-Ghanem, Y.; Bedke, J.; Capitanio, U.; Dabestani, S.; Fernández-Pello, S.; Giles, R.H.; Hofmann, F.; Hora, M.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Eur. Urol. 2022, 82, 399–410. [Google Scholar] [CrossRef]
- Cuijpers, P.; Smits, N.; Donker, T.; ten Have, M.; de Graaf, R. Screening for Mood and Anxiety Disorders with the Five-Item, the Three-Item, and the Two-Item Mental Health Inventory. Psychiatry Res. 2009, 168, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Livingston, J.D.; Youssef, G.J.; Francis, L.M.; Greenwood, C.J.; Olsson, C.A.; Macdonald, J.A. Hidden in Plain Sight? Men’s Coping Patterns and Psychological Distress Before and During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 772942. [Google Scholar] [CrossRef]
- Ho, C.S.H.; Chua, J.; Tay, G.W.N. The Diagnostic and Predictive Potential of Personality Traits and Coping Styles in Major Depressive Disorder. BMC Psychiatry 2022, 22, 301. [Google Scholar] [CrossRef] [PubMed]
- Mc Hugh, R.; McBride, O. Investigating the Nature of Depressive Experiences in Adults Who Self-Medicate Low Mood with Alcohol. Alcohol Fayettev. N 2022, 103, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Asselin, A.; Lamarre, O.B.; Chamberland, R.; McNeil, S.-J.; Demers, E.; Zongo, A. A Description of Self-Medication with Cannabis among Adults with Legal Access to Cannabis in Quebec, Canada. J. Cannabis Res. 2022, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-H.; Li, J.-Q.; Shi, J.-F.; Que, J.-Y.; Liu, J.-J.; Lappin, J.M.; Leung, J.; Ravindran, A.V.; Chen, W.-Q.; Qiao, Y.-L.; et al. Depression and Anxiety in Relation to Cancer Incidence and Mortality: A Systematic Review and Meta-Analysis of Cohort Studies. Mol. Psychiatry 2020, 25, 1487–1499. [Google Scholar] [CrossRef]
- Vartolomei, L.; Ferro, M.; Mirone, V.; Shariat, S.F.; Vartolomei, M.D. Systematic Review: Depression and Anxiety Prevalence in Bladder Cancer Patients. Bladder Cancer Amst. Neth. 2018, 4, 319–326. [Google Scholar] [CrossRef]
- Brunckhorst, O.; Hashemi, S.; Martin, A.; George, G.; Van Hemelrijck, M.; Dasgupta, P.; Stewart, R.; Ahmed, K. Depression, Anxiety, and Suicidality in Patients with Prostate Cancer: A Systematic Review and Meta-Analysis of Observational Studies. Prostate Cancer Prostatic Dis. 2021, 24, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.B.; Butow, P.; Olver, I.; Luckett, T.; Grimison, P.; Toner, G.C.; Stockler, M.R.; Hovey, E.; Stubbs, J.; Turner, S.; et al. The Prevalence, Severity, and Correlates of Psychological Distress and Impaired Health-Related Quality of Life Following Treatment for Testicular Cancer: A Survivorship Study. J. Cancer Surviv. Res. Pract. 2016, 10, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Dinesh, A.A.; Helena Pagani Soares Pinto, S.; Brunckhorst, O.; Dasgupta, P.; Ahmed, K. Anxiety, Depression and Urological Cancer Outcomes: A Systematic Review. Urol. Oncol. 2021, 39, 816–828. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Handbook for Systematic Reviews of Interventions. Available online: http://handbook-5-1.cochrane.org/ (accessed on 19 April 2018).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Int. J. Surg. Lond. Engl. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Ames, S.C.; Parker, A.S.; Crook, J.E.; Diehl, N.N.; Tan, W.W.; Williams, C.R.; Ames, G.E. Quality of Life of Patients Undergoing Surgical Treatment for Newly-Diagnosed, Clinically Localized Renal Cell Carcinoma. J. Psychosoc. Oncol. 2011, 29, 593–605. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed on 1 October 2022).
- Demirtaş, T.; Temircan, Z. Examining the Relationship between Depression, Anxiety and Stress in Kidney Cancer Patients. J. Kidney Cancer VHL 2022, 9, 19–26. [Google Scholar] [CrossRef]
- Ajaj, R.; Cáceres, J.O.H.; Berlin, A.; Wallis, C.J.D.; Chandrasekar, T.; Klaassen, Z.; Ahmad, A.E.; Leao, R.; Finelli, A.; Fleshner, N.; et al. Gender-Based Psychological and Physical Distress Differences in Patients Diagnosed with Non-Metastatic Renal Cell Carcinoma. World J. Urol. 2020, 38, 2547–2554. [Google Scholar] [CrossRef]
- Shin, D.W.; Park, H.S.; Lee, S.H.; Jeon, S.H.; Cho, S.; Kang, S.H.; Park, S.C.; Park, J.H.; Park, J. Health-Related Quality of Life, Perceived Social Support, and Depression in Disease-Free Survivors Who Underwent Curative Surgery Only for Prostate, Kidney and Bladder Cancer: Comparison among Survivors and with the General Population. Cancer Res. Treat. 2019, 51, 289–299. [Google Scholar] [CrossRef]
- Bergerot, C.D.; Battle, D.; Staehler, M.D.; Pal, S.K. Distress in Patients with Renal Cell Carcinoma: A Curious Gap in Knowledge. BJU Int. 2019, 123, 208–209. [Google Scholar] [CrossRef]
- Draeger, D.L.; Sievert, K.-D.; Hakenberg, O.W. Analysis of Psychosocial Stress Factors in Patients with Renal Cancer. Ther. Adv. Urol. 2018, 10, 175–182. [Google Scholar] [CrossRef]
- Li, M.; Wang, L. The Associations of Psychological Stress with Depressive and Anxiety Symptoms among Chinese Bladder and Renal Cancer Patients: The Mediating Role of Resilience. PLoS ONE 2016, 11, e0154729. [Google Scholar] [CrossRef] [PubMed]
- Thekdi, S.M.; Milbury, K.; Spelman, A.; Wei, Q.; Wood, C.; Matin, S.F.; Tannir, N.; Jonasch, E.; Pisters, L.; Cohen, L. Posttraumatic Stress and Depressive Symptoms in Renal Cell Carcinoma: Association with Quality of Life and Utility of Single-Item Distress Screening. Psychooncology 2015, 24, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadis, A.G.; Davis, A.R.; Sawczuk, I.S.; Fleming, M.; Perelman, M.A.; Burchardt, M.; Shabsigh, R. Quality of Life Aspects in Kidney Cancer Patients: Data from a National Registry. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2003, 11, 700–706. [Google Scholar] [CrossRef]
- Ficarra, V.; Novella, G.; Sarti, A.; Novara, G.; Galfano, A.; Cavalleri, S.; Artibani, W. Psycho-Social Well-Being and General Health Status after Surgical Treatment for Localized Renal Cell Carcinoma. Int. Urol. Nephrol. 2002, 34, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Packiam, V.T.; Tyson Ii, M.D.; Tsivian, M.; Lohse, C.M.; Boorjian, S.A.; Cheville, J.C.; Costello, B.A.; Leibovich, B.C.; Thompson, R.H. The Association of Anxiety and Depression with Perioperative and Oncologic Outcomes among Patients with Clear Cell Renal Cell Carcinoma Undergoing Nephrectomy. Urol. Oncol. 2020, 38, 41.e19–41.e27. [Google Scholar] [CrossRef] [PubMed]
- Song, B.; Zhang, Y.; Wang, Y.; An, X. Intensive Patients’ Care Program Ameliorates Anxiety and Depression, and Sustained Anxiety Correlates with Worse Overall Survival in Renal Cell Carcinoma Patients Underwent Radical Nephrectomy. Transl. Cancer Res. 2018, 7, 1601–1613. [Google Scholar] [CrossRef]
- Bergerot, C.D.; Clark, K.L.; Ashing, K.T.; Bergerot, P.G.; Obenchain, R.; Dizman, N.; Hsu, J.; Philip, E.; Loscalzo, M.; Pal, S.K. Biopsychosocial Distress and Clinical Outcome in Metastatic Renal Cell Carcinoma. Palliat. Support. Care 2019, 17, 353–355. [Google Scholar] [CrossRef]
- Cohen, L.; Cole, S.W.; Sood, A.K.; Prinsloo, S.; Kirschbaum, C.; Arevalo, J.M.G.; Jennings, N.B.; Scott, S.; Vence, L.; Wei, Q.; et al. Depressive Symptoms and Cortisol Rhythmicity Predict Survival in Patients with Renal Cell Carcinoma: Role of Inflammatory Signaling. PLoS ONE 2012, 7, e42324. [Google Scholar] [CrossRef]
- Wang, Y.; Song, B.; Zhang, Y.; Li, H. Evaluation and Predictive Factors Analyses for Patient-Self-Reported Depression, Anxiety and Quality of Life in Patients with Metastatic Renal Cell Carcinoma Underwent Interferon-α Treatment: A Prospective Cohort Study. Transl. Cancer Res. 2018, 7, 1460–1473. [Google Scholar] [CrossRef]
- Vartolomei, L.; Vartolomei, M.D.; Shariat, S.F. Bladder Cancer: Depression, Anxiety, and Suicidality among the Highest-Risk Oncology Patients. Eur. Urol. Focus 2020, 6, 1158–1161. [Google Scholar] [CrossRef]
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). Available online: http://Ghdx.Healthdata.Org/Gbd-Results-Tool?Params=gbd-Api-2019-Permalink/D780dffbe8a381b25e1416884959e88b (accessed on 1 May 2022).
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global Prevalence of Mental Health Issues among the General Population during the Coronavirus Disease-2019 Pandemic: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.M.C.; Ho, M.K.; Bharwani, A.A.; Cogo-Moreira, H.; Wang, Y.; Chow, M.S.C.; Fan, X.; Galea, S.; Leung, G.M.; Ni, M.Y. Mental Disorders Following COVID-19 and Other Epidemics: A Systematic Review and Meta-Analysis. Transl. Psychiatry 2022, 12, 205. [Google Scholar] [CrossRef] [PubMed]
- Chan, V.W.-S.; Tan, W.S.; Leow, J.J.; Tan, W.P.; Ong, W.L.K.; Chiu, P.K.-F.; Gurung, P.; Pirola, G.M.; Orecchia, L.; Liew, M.P.C.; et al. Delayed Surgery for Localised and Metastatic Renal Cell Carcinoma: A Systematic Review and Meta-Analysis for the COVID-19 Pandemic. World J. Urol. 2021, 39, 4295–4303. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, C.; Mistretta, F.A.; Knipper, S.; Pecoraro, A.; Tian, Z.; Shariat, S.F.; Saad, F.; Simeone, C.; Briganti, A.; Antonelli, A.; et al. Conditional Survival of Patients With Nonmetastatic Renal Cell Carcinoma: How Cancer-Specific Mortality Changes After Nephrectomy. J. Natl. Compr. Cancer Netw. 2020, 18, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Yussof, I.; Mohd Tahir, N.A.; Hatah, E.; Mohamed Shah, N. Factors Influencing Five-Year Adherence to Adjuvant Endocrine Therapy in Breast Cancer Patients: A Systematic Review. Breast Edinb. Scotl. 2022, 62, 22–35. [Google Scholar] [CrossRef]
- Kim, S.J.; Kang, D.; Park, Y.; Mun, Y.-C.; Kim, K.; Kim, J.S.; Min, C.-K.; Cho, J. Impact of Depression on Adherence to Lenalidomide plus Low-Dose Dexamethasone in Patients with Relapsed or Refractory Myeloma. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2021, 29, 4969–4977. [Google Scholar] [CrossRef]
- Giles, R.H.; Marconi, L.; Martinez, R.; Maskens, D.; Kastrati, K.; Castro, C.; Julian Mauro, J.C.; Bick, R.; Heng, D.Y.C.; Larkin, J.; et al. Patient-Reported Experience of Diagnosis, Management, and Burden of Renal Cell Carcinomas: Results >2,000 Patients in 41 Countries, with Focus on Older Patients. J. Clin. Oncol. 2022, 40, 306. [Google Scholar] [CrossRef]
| No. | First Author | Year | Country | Study Design | No. Patients | Patients Characteristics | Treatment | Questionnaires | Results | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Demirtaş et al. | 2021 [18] | Turkey | Cross-sectional | 250 (66 females 27%) | Kidney cancer | surgery had 102 patients (40.8%) type of surgery n.a | Hospital Depression and Anxiety Scale (HADS), and Perceived Stress Scale (PSS) | HADS-Anxiety symptoms in the study were found in 91.2% patients; 98 (39.2%) participants had mild, 99 (39.6%) had moderate, 31 (12.4%) had severe anxiety symptoms. HADS-Depression symptoms were found in 87.2% patients; 87 (34.8%) participants had mild, 101 (40.4%) had moderate, 30 (12%) had severe depression symptoms. | None Evaluation some time (n.a) after treatment |
| 2 | Ajaj et al. | 2020 [19] | Canada | Retrospective 2014–2017 | 495 (184 females 37.2%) | Consecutive patients diagnosed with non-metastatic RCC | PN 93 females (62.8%) vs. 148 males (61.7%) | The Edmonton Symptom Assessment System—revised (ESAS-r) | Increasing age was shown to be associated with a lower Psychological distress sub-score (PDSS) score after diagnosis [B = −0.135, 95%CI −0.238 to (−0.032), p = 0.011] and after nephrectomy [B = −0.078, 95%CI −0.139 to (−0.018), p = 0.012]. PDSS was significantly higher in females after diagnosis (8.5 vs. 5.1, p = 0.018), after biopsy (8.9 vs. 4.1, p = 0.003), and after surgery (6.5 vs. 4.4, p = 0.007), while there was no difference at the last follow-up (5.9 vs. 5, p = 0.379). | None Evaluation at 37 mo. for females and 26 mo. for males after treatment |
| 3 | Shin et al. | 2019 [20] | Korea | Case-control between April 2014 and December 2015 | 108 (31 females 28.7%) | non-metastatic RCC | n.a | European Organization for Research and Treatment of Cancer QLQ-C30, the Duke-UNC Functional Social Support Questionnaire and the Patient Health Questionnaire-9. | At 2 years no statistically significant difference was observed in terms of depressive symptoms between kidney cancer survivors and the general population. | None Evaluation at least 1 year after surgery |
| 4 | Bergerot et al. | 2019 [21] | USA | Online survey from 1 April to 15 June 2017 | 450 (224 females 56%) | non-metastatic RCC (74%) | n.a | NCCN Distress Thermometer (NCCN-DT) | 77 % of patients reported moderate-to-severe distress. Distress was significantly associated with female gender, younger age, non-clear cell histology and presence of recurrence | None Evaluation some time (n.a) after treatment |
| 5 | Draeger et al. | 2018 [22] | Germany | Cross-sectional | 74 (20 females 27%) | Consecutive RCC patients irrespective of tumor stage (localized versus advanced) 71 were N0M0 | 71 RN | [NCCN Distress Thermometer (NCCN-DT), Hornheider Screening Instrument (HSI)] | The main identified stressors were anxiety (28%), pain (27%), nervousness (26%), sadness (20%), sorrow (20%) and sleep difficulties (20%) | None Evaluation at time of treatment |
| 6 | Li et al. | 2016 [23] | China | Cross-sectional from July 2013 to July 2014 | 268 (100 females 37.3%) | Kidney cancer stage I-III (mostly non-metastatic RCC) | n.a | Center for Epidemiologic Studies Depression Scale (CES-D), Zung Self-Rating Anxiety Scale, Resilience Scale-14, and Perceived Stress Scale-10 | The prevalence of depressive and anxiety symptoms was 77.6% and 68.3% in renal cancer patients. | None Evaluation one week after surgery |
| 7 | Thekdi et al. | 2016 [24] | USA | Baseline data of a randomized controlled trial evaluating the benefits of an expressive writing intervention on quality of life outcomes | 287 (118 females 42%) | Kidney cancer Stage I-IV (mostly non-metastatic RCC) | Surgery 195 (70.3) | CES-D, Impact of Events Scale (IES), MD Anderson Symptom Inventory (MDASI), Brief Fatigue Inventory (BFI) and Pittsburgh Sleep Quality Index (PSQI) | 15.2% were identified as having comorbid (Post-traumatic Stress Symptoms) PTSS and depressive symptoms; 24.1% PTSS alone; 5.9% depressive symptoms alone | None Evaluation before treatment |
| 8 | Ames et al. | 2011 [16] | USA | Prospective between October 2005 and January 2008 | 28 (8 females 29%) | localized RCC | RN | The Functional Assessment of Cancer Therapy–General (FACT-G), Medical Outcomes Study 36-item short form survey (SF-36), The Profile of Mood States–Brief (POMS-B), Beck Depression Inventory–II (BDI-II), State-Trait Anxiety Inventory (STAI) prior to nephrectomy and at 4, 12, and 24 weeks post-nephrectomy and completion of individual semi-structured interviews 4 weeks post-nephrectomy | No significant change was observed in BDI –II scores: 5.5 (4.8) baseline vs. 8.7 (9.7) at 24 weeks, p = 0.081 No significant change was observed in STAI scores at baseline 34.9 (12.9) vs. 32.1 (8.9) at 24 weeks, p = 0.25 | Evaluation at baseline and at 24 weeks after treatment |
| 9 | Anastasiadis et al. | 2003 [25] | USA | Cross-sectional survey of a random sample of patients | 84 (42 females 50%) | Kidney cancer | RN (up to 90%) | Watts Sexual Function Questionnaire (WSFQ), the SF-12 Health Survey, CES-D, and the Revised Dyadic Adjustment Scale | 51% of men and 57% of women reported depressive symptoms (CES-D > 16) at more than 3 years after diagnosis | None Evaluation at 3.2 years for females and 3.7 years for males after treatment |
| 10 | Ficarra et al. | 2002 [26] | Italy | Cross-sectional | 144 (48 females 33.3%) | T1N0M0 RCC | 56 patients (39%) have been treated with elective NSS and 88 (61%) underwent RN | General Health Questionnaire (GHQ), HADS, Social Problem Questionnaire (SPQ.) | Higher scores for anxiety 2.77 ± 2.77 vs. 1.79 ± 2.47, p = 0.003 and depression 2.08 ± 2.32 vs. 1.70 ± 2.80 p = 0.015 were reported in the RN group compared to those that underwent NSS | None Evaluation at 55 ± 36 months after treatment |
| No. | First Author | Year | Country | Study Design | No. Patients | Patients Characteristics | Treatment | Questionnaires | Results | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Packiam et al. | 2020 [27] | USA | Retrospective between 1995 and 2011 | 1990 (701 females 35%) | non-metastatic RCC | RN 1144 (57%) | Baseline anxiety and depression were identified using ICD-9 Codes (197 patients with anxiety and/or depression) | No significant differences were noted regarding local ipsilateral recurrence, distant metastases, overall survival or death from RCC between patients with vs. without anxiety or depression. | 10 years |
| 2 | Song et al. | 2018 [28] | China | Randomized clinical trial | 182 | RCC patients were randomly allocated 1:1 in two groups intensive patients’ care program IPCP group (IPCP plus usual care) or a control group (only usual care) (I) diagnosed as RCC according to clinical, imaging and pathological findings; (II) age above 18 years; (III) unilateral renal cell carcinoma; (IV) received radical nephrectomy; (V) able to complete the questionnaire of assessments. | RN | Hospital Anxiety and Depression Scale anxiety/ depression (HADS-A/HADS-D) Zung Self Rating Anxiety/Depression Scale (SAS/SDS) Evaluation at baseline and at 12 months after treatment | Patients with sustained anxiety assessed by the HADS-A score had worse OS compared with that of patients without sustained anxiety assessed by HADS-A score (p = 0.026). Patients with sustained anxiety assessed by SDS score also had a shorter OS compared with patients without sustained anxiety assessed by SAS score (p = 0.012). No difference of OS between patients with or without depression assessed by HADS-D score (p = 0.166) or SDS score (p = 0.131) | 43 mo. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vartolomei, L.; Schmidinger, M.; Vartolomei, M.D.; Shariat, S.F. Psychological Distress in Patients Treated for Renal Cell Carcinoma: A Systematic Literature Review. J. Clin. Med. 2022, 11, 6383. https://doi.org/10.3390/jcm11216383
Vartolomei L, Schmidinger M, Vartolomei MD, Shariat SF. Psychological Distress in Patients Treated for Renal Cell Carcinoma: A Systematic Literature Review. Journal of Clinical Medicine. 2022; 11(21):6383. https://doi.org/10.3390/jcm11216383
Chicago/Turabian StyleVartolomei, Liliana, Manuela Schmidinger, Mihai Dorin Vartolomei, and Shahrokh F. Shariat. 2022. "Psychological Distress in Patients Treated for Renal Cell Carcinoma: A Systematic Literature Review" Journal of Clinical Medicine 11, no. 21: 6383. https://doi.org/10.3390/jcm11216383
APA StyleVartolomei, L., Schmidinger, M., Vartolomei, M. D., & Shariat, S. F. (2022). Psychological Distress in Patients Treated for Renal Cell Carcinoma: A Systematic Literature Review. Journal of Clinical Medicine, 11(21), 6383. https://doi.org/10.3390/jcm11216383







