Efficacy of Dupilumab on Different Phenotypes of Adult with Moderate-to-Severe Atopic Dermatitis in Taiwan: A Real-World Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Ethical Considerations
2.3. Data Collection and Main Outcomes
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
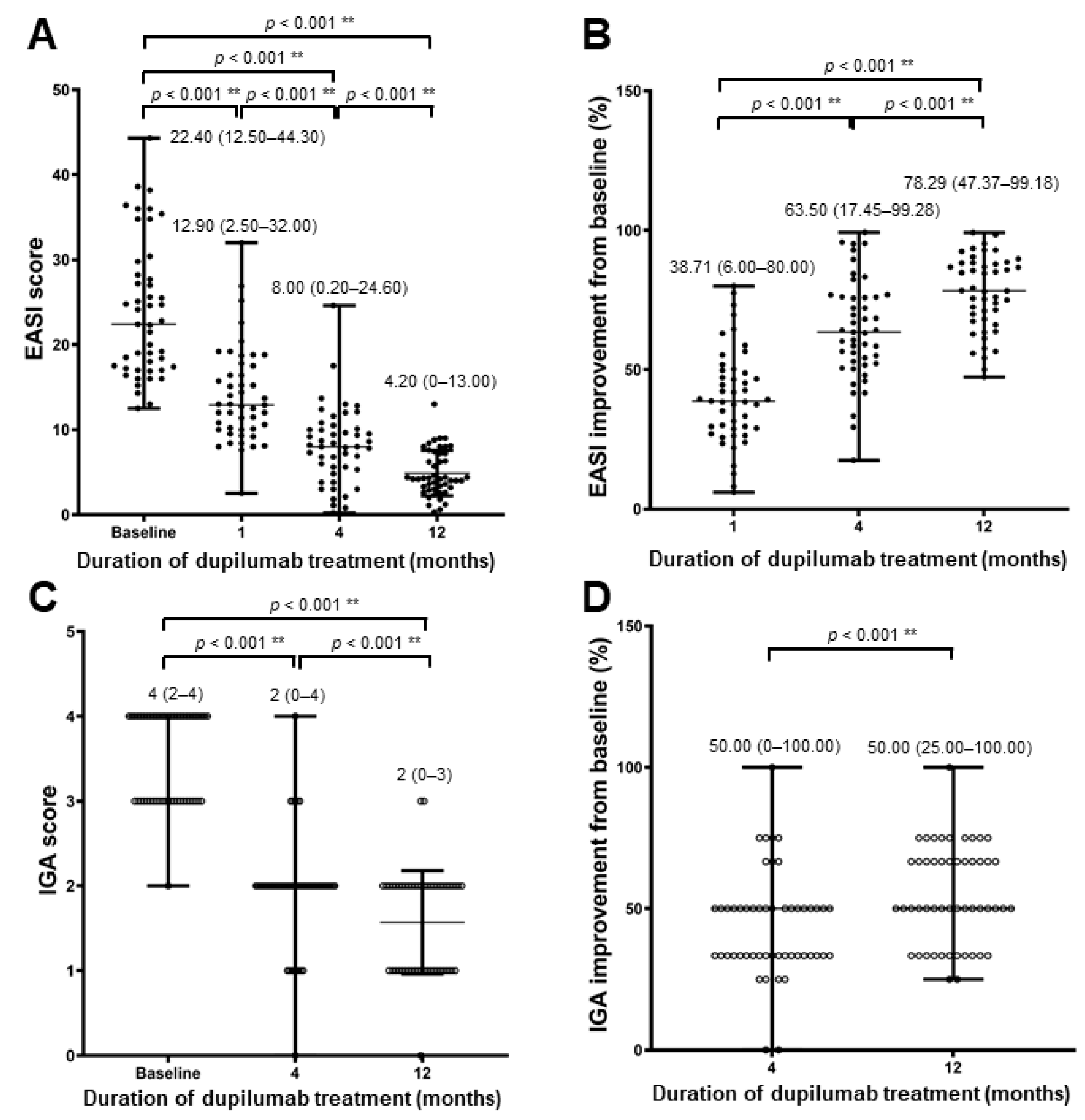
3.2. Efficacy of Dupilumab Treatment
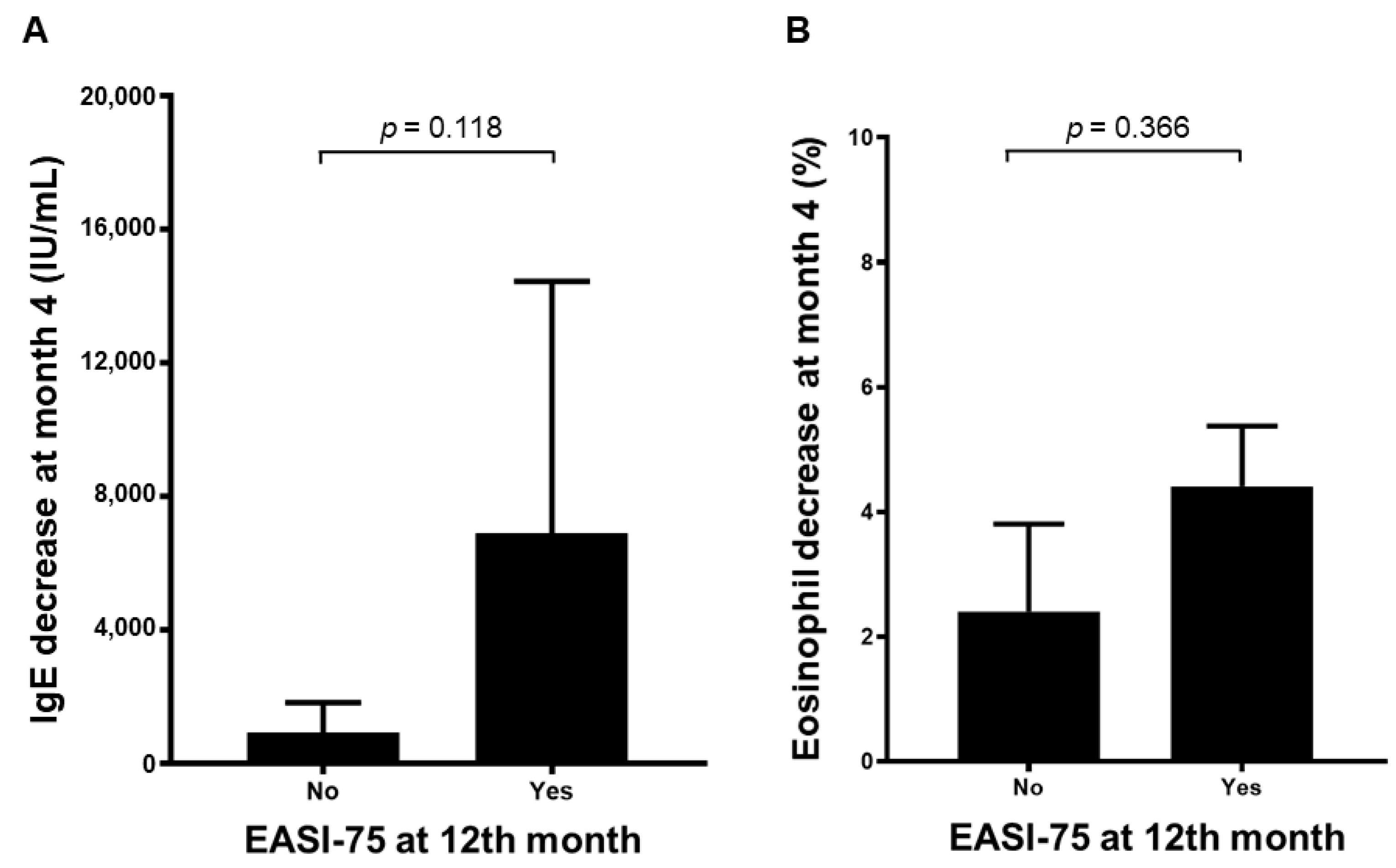
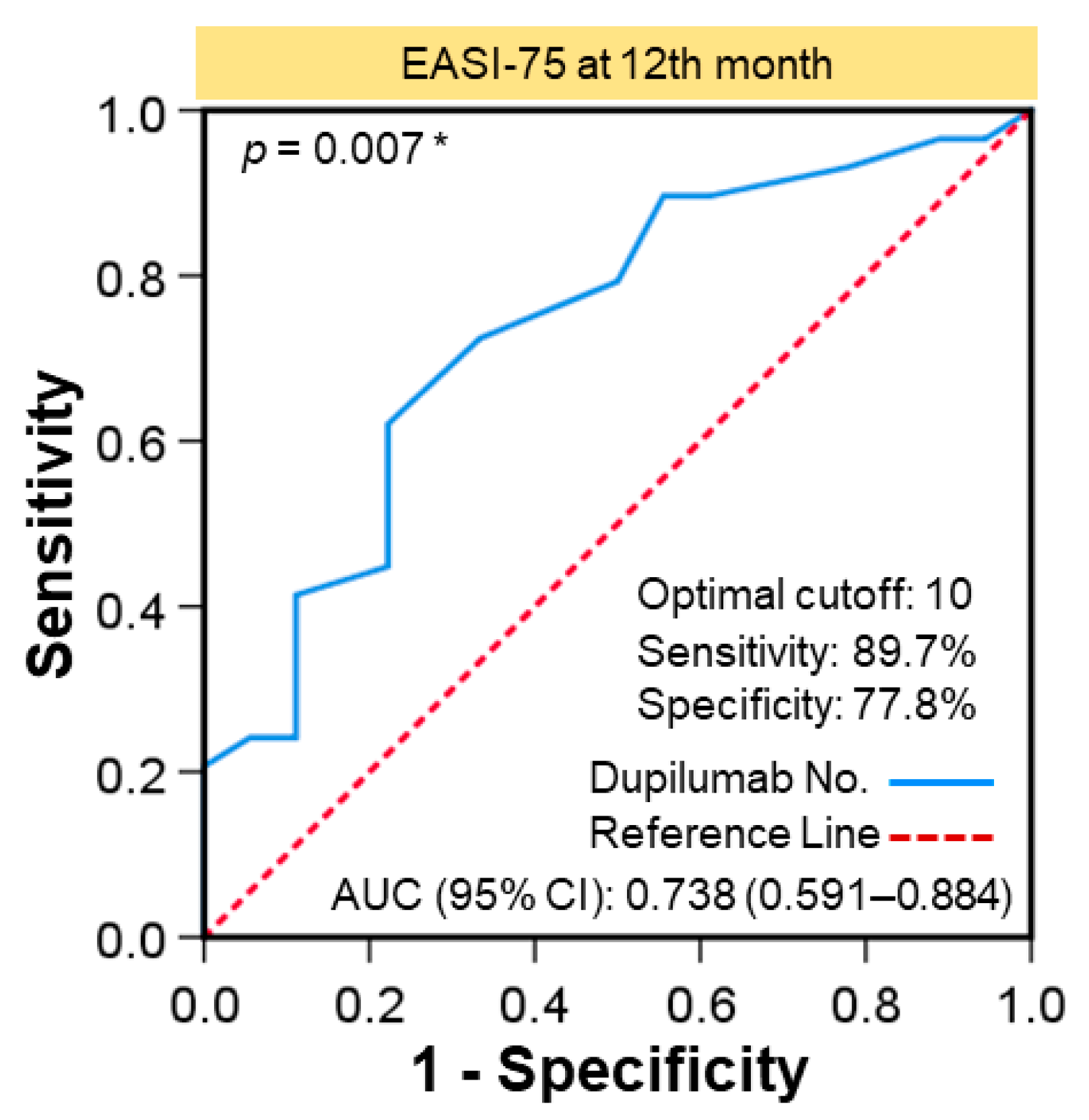
3.3. EASI-75 Related Factors
3.4. Safety of Dupilumab Treatment
3.5. Specific Cases
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bieber, T. Atopic dermatitis. N. Engl. J. Med. 2008, 358, 1483–1494. [Google Scholar] [CrossRef] [PubMed]
- DaVeiga, S.P. Epidemiology of atopic dermatitis: A review. Allergy Asthma Proc. 2012, 33, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Malajian, D.; Guttman-Yassky, E. New pathogenic and therapeutic paradigms in atopic dermatitis. Cytokine 2015, 73, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Gittler, J.K.; Shemer, A.; Suarez-Farinas, M.; Fuentes-Duculan, J.; Gulewicz, K.J.; Wang, C.Q.; Mitsui, H.; Cardinale, I.; de Guzman Strong, C.; Krueger, J.G.; et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis. J. Allergy Clin. Immunol. 2012, 130, 1344–1354. [Google Scholar] [CrossRef]
- Silvestre Salvador, J.F.; Romero-Perez, D.; Encabo-Duran, B. Atopic Dermatitis in Adults: A Diagnostic Challenge. J. Investig. Allergol. Clin. Immunol. 2017, 27, 78–88. [Google Scholar] [CrossRef]
- Guttman-Yassky, E.; Nograles, K.E.; Krueger, J.G. Contrasting pathogenesis of atopic dermatitis and psoriasis—part II: Immune cell subsets and therapeutic concepts. J. Investig. Allergol. Clin. Immunol. 2011, 127, 1420–1432. [Google Scholar] [CrossRef]
- Weidinger, S.; Beck, L.A.; Bieber, T.; Kabashima, K.; Irvine, A.D. Atopic dermatitis. Nat. Rev. Dis. Primers 2018, 4, 1. [Google Scholar] [CrossRef]
- Hamilton, J.D.; Suarez-Farinas, M.; Dhingra, N.; Cardinale, I.; Li, X.; Kostic, A.; Ming, J.E.; Radin, A.R.; Krueger, J.G.; Graham, N.; et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J. Allergy Clin. Immunol. 2014, 134, 1293–1300. [Google Scholar] [CrossRef]
- Beck, L.A.; Thaci, D.; Hamilton, J.D.; Graham, N.M.; Bieber, T.; Rocklin, R.; Ming, J.E.; Ren, H.; Kao, R.; Simpson, E.; et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N. Engl. J. Med. 2014, 371, 130–139. [Google Scholar] [CrossRef]
- Simpson, E.L.; Bieber, T.; Guttman-Yassky, E.; Beck, L.A.; Blauvelt, A.; Cork, M.J.; Silverberg, J.I.; Deleuran, M.; Kataoka, Y.; Lacour, J.P.; et al. Two Phase 3 Trials of Dupilumab versus Placebo in Atopic Dermatitis. N. Engl. J. Med. 2016, 375, 2335–2348. [Google Scholar] [CrossRef]
- Thaci, D.; Simpson, E.L.; Beck, L.A.; Bieber, T.; Blauvelt, A.; Papp, K.; Soong, W.; Worm, M.; Szepietowski, J.C.; Sofen, H.; et al. Efficacy and safety of dupilumab in adults with moderate-to-severe atopic dermatitis inadequately controlled by topical treatments: A randomised, placebo-controlled, dose-ranging phase 2b trial. Lancet 2016, 387, 40–52. [Google Scholar] [CrossRef]
- Hanifin, J.M.; Rajka, G. Diagnostic features of atopic dermatitis. Acta Derm. Venereol. 1980, 60, 44–47. [Google Scholar]
- Tavecchio, S.; Angileri, L.; Pozzo Giuffrida, F.; Germiniasi, F.; Marzano, A.V.; Ferrucci, S. Efficacy of Dupilumab on Different Phenotypes of Atopic Dermatitis: One-Year Experience of 221 Patients. J. Clin. Med. 2020, 9, 2684. [Google Scholar] [CrossRef] [PubMed]
- Schram, M.E.; Spuls, P.I.; Leeflang, M.M.; Lindeboom, R.; Bos, J.D.; Schmitt, J. EASI, (objective) SCORAD and POEM for atopic eczema: Responsiveness and minimal clinically important difference. Allergy 2012, 67, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Blauvelt, A.; de Bruin-Weller, M.; Gooderham, M.; Cather, J.C.; Weisman, J.; Pariser, D.; Simpson, E.L.; Papp, K.A.; Hong, H.C.; Rubel, D.; et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): A 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet 2017, 389, 2287–2303. [Google Scholar] [CrossRef]
- Noda, S.; Suarez-Farinas, M.; Ungar, B.; Kim, S.J.; de Guzman Strong, C.; Xu, H.; Peng, X.; Estrada, Y.D.; Nakajima, S.; Honda, T.; et al. The Asian atopic dermatitis phenotype combines features of atopic dermatitis and psoriasis with increased TH17 polarization. J. Allergy Clin. Immunol. 2015, 136, 1254–1264. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N. Chronic rhinosinusitis and asthma: Novel understanding of the role of IgE ‘above atopy’. J. Intern. Med. 2012, 272, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Hello, M.; Aubert, H.; Bernier, C.; Neel, A.; Barbarot, S. Atopic dermatitis of the adult. Rev. Med. Interne 2016, 37, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, C.; de Bruin-Weller, M.; Deleuran, M.; Fargnoli, M.C.; Staumont-Salle, D.; Hong, C.H.; Sanchez-Carazo, J.; Foley, P.; Seo, S.J.; Msihid, J.; et al. Dupilumab in Adults with Moderate-to-Severe Atopic Dermatitis and Prior Use of Systemic Non-Steroidal Immunosuppressants: Analysis of Four Phase 3 Trials. Dermatol. Ther. 2021, 11, 1357–1372. [Google Scholar] [CrossRef]
- Galli, E.; Gianni, S.; Auricchio, G.; Brunetti, E.; Mancino, G.; Rossi, P. Atopic dermatitis and asthma. Allergy Asthma Proc. 2007, 28, 540–543. [Google Scholar] [CrossRef]
- Jang, D.H.; Heo, S.J.; Jung, H.J.; Park, M.Y.; Seo, S.J.; Ahn, J. Retrospective Study of Dupilumab Treatment for Moderate to Severe Atopic Dermatitis in Korea: Efficacy and Safety of Dupilumab in Real-World Practice. J. Clin. Med. 2020, 9, 1982. [Google Scholar] [CrossRef]
- Patel, G.P.; Pasha, M.A.; D’Souza, S. Group 2 Innate Lymphoid Cells in Patients with Severe Atopic Dermatitis on Dupilumab. J. Allergy Clin. Immunol. 2019, 143, 2. [Google Scholar] [CrossRef][Green Version]
- Guttman-Yassky, E.; Bissonnette, R.; Ungar, B.; Suarez-Farinas, M.; Ardeleanu, M.; Esaki, H.; Suprun, M.; Estrada, Y.; Xu, H.; Peng, X.; et al. Dupilumab progressively improves systemic and cutaneous abnormalities in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2019, 143, 155–172. [Google Scholar] [CrossRef]
- Wang, C.; Kraus, C.N.; Patel, K.G.; Ganesan, A.K.; Grando, S.A. Real-world experience of dupilumab treatment for atopic dermatitis in adults: A retrospective analysis of patients’ records. Int. J. Dermatol. 2020, 59, 253–256. [Google Scholar] [CrossRef]
- Halling, A.S.; Loft, N.; Silverberg, J.I.; Guttman-Yassky, E.; Thyssen, J.P. Real-world evidence of dupilumab efficacy and risk of adverse events: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2021, 84, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Thibodeaux, Q.; Smith, M.P.; Ly, K.; Beck, K.; Liao, W.; Bhutani, T. A review of dupilumab in the treatment of atopic diseases. Hum. Vaccines Immunother. 2019, 15, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Narla, S.; Silverberg, J.I.; Simpson, E.L. Management of inadequate response and adverse effects to dupilumab in atopic dermatitis. J. Am. Acad. Dermatol. 2022, 86, 628–636. [Google Scholar] [CrossRef]
- Fowler, E.; Silverberg, J.I.; Fox, J.D.; Yosipovitch, G. Psoriasiform Dermatitis After Initiation of Treatment with Dupilumab for Atopic Dermatitis. Dermatitis 2019, 30, 234–236. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.Y. Keeping an eye on the ocular problems in dupilumab clinical trials. Br. J. Dermatol. 2019, 181, 436–437. [Google Scholar] [CrossRef] [PubMed]
- Soria, A.; Du-Thanh, A.; Seneschal, J.; Jachiet, M.; Staumont-Salle, D.; Barbarot, S. Development or Exacerbation of Head and Neck Dermatitis in Patients Treated for Atopic Dermatitis with Dupilumab. JAMA Dermatol. 2019, 155, 1312–1315. [Google Scholar] [CrossRef]
- de Wijs, L.E.M.; Nguyen, N.T.; Kunkeler, A.C.M.; Nijsten, T.; Damman, J.; Hijnen, D.J. Clinical and histopathological characterization of paradoxical head and neck erythema in patients with atopic dermatitis treated with dupilumab: A case series. Br. J. Dermatol. 2020, 183, 745–749. [Google Scholar] [CrossRef] [PubMed]
- de Beer, F.S.A.; Bakker, D.S.; Haeck, I.; Ariens, L.; van der Schaft, J.; van Dijk, M.R.; de Bruin-Weller, M.S. Dupilumab facial redness: Positive effect of itraconazole. JAAD Case Rep. 2019, 5, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.J.; Sugarman, J.L.; Silverberg, N.B.; Gonzalez, M.E.; Ramien, M.L.; Teng, J.M.C.; Paller, A.S. Psoriasiform dermatitis during dupilumab treatment for moderate-to-severe atopic dermatitis in children. Pediatric Dermatol. 2021, 38, 1500–1505. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 111) |
|---|---|
| Age, years, median (range) | 30 (18–79) |
| Gender, n (%) | |
| Male | 71 (64.0) |
| Female | 40 (36.0) |
| Weight, kg, median (range) | 66.0 (29.6–129.5) |
| Prior allergic rhinitis, n (%) | 78 (70.3) |
| Prior asthma, n (%) | 29 (26.1) |
| BSA%, baseline, median (range) | 50 (15–97) |
| IGA score, baseline, n (%) | |
| 3 | 58 (52.3) |
| 4 | 53 (47.7) |
| EASI score, baseline, median (range) | 21.9 (10.8–56.3) |
| <16 | 18 (16.2) |
| ≧16 | 93 (83.8) |
| Onset age, years, median (range) | 18 (0–72) |
| Adult Onset | 52/100 (52.0) |
| Childhood | 48/100 (48.0) |
| Renal Insufficiency | 5 (4.5) |
| Liver disease (HCV, HBV, fatty liver) | 4 (3.6) |
| Hyper IgE syndrome | 2 (1.8) |
| AD phenotype, n (%) | |
| Type I a | 50/99 (50.5) |
| Type II b | 6/99 (6.1) |
| Type III c | 7/99 (7.1) |
| Type IV d | 20/99 (20.2) |
| Type V e | 7/99 (7.1) |
| Type VI f | 7/99 (7.1) |
| Type VII g | 2/99 (2.0) |
| Disease duration until start of dupilumab, years, median (range) | 8 (0–43) |
| Previous use of cyclosporine, azathioprine, or methotrexate, n (%) | 52 (46.8) |
| Cyclosporine | 38 (34.2) |
| Azathioprine | 25 (22.5) |
| Methotrexate | 21 (18.9) |
| Laboratory index, baseline, median (range) | |
| Eosinophil, % | 9.1 (0.7–44.0) |
| LDH, U/L | 220 (140–461) |
| IgE, IU/mL | 5000 (17.2–38,700) |
| Extrinsic AD (IgE > 100) | 63/65 (96.9) |
| Intrinsic AD | 2/65 (3.1) |
| Variables | Total (n = 111) |
|---|---|
| EASI-75, n (%) | |
| Change in score from baseline to 1 month | 18/111 (16.2) |
| Change in score from baseline to 4 months | 49/111 (44.1) |
| Change in score from baseline to 12 months | 29/47 (61.7) |
| EASI-50, n (%) | |
| Change in score from baseline to 1 month | 41/111 (36.9) |
| Change in score from baseline to 4 months | 96/111 (86.5) |
| Change in score from baseline to 12 months | 46/47 (97.9) |
| IGA < 2, n (%) | |
| 4 months | 29/106 (27.4) |
| 12 months | 23/47 (48.9) |
| EASI reaching MCID after 1 month of treatment | 72/111 (64.9) |
| EASI reaching MCID after 4 months of treatment | 104/111 (93.7) |
| EASI reaching MCID after 12 months of treatment | 47/47 (100.0) |
| EASI-75 at 4 Months (n = 111) | p-Value | EASI-75 at 12 Months (n = 47) | p-Value | |||
|---|---|---|---|---|---|---|
| Variables | No | Yes | No | Yes | ||
| Age, years, median (range) | 34 (18–79) | 25 (18–64) | 0.005 * | 34 (19–76) | 28 (19–50) | 0.174 |
| Gender/Male, n (%) | 39 (63.9) | 27 (61.4) | 0.839 | 10 (55.6) | 22 (75.9) | 0.202 |
| Weight, kg, median (range) | 68.5 (46.0–103.0) | 60.2 (29.6–110.0) | 0.077 | 66.1 (50.0–79.4) | 69.8 (46.0–110.0) | 0.360 |
| Prior allergic rhinitis, n (%) | 47 (77.0) | 27 (61.4) | 0.089 | 14 (77.8) | 25 (86.2) | 0.692 |
| Prior asthma, n (%) | 12 (19.7) | 16 (36.4) | 0.074 | 3 (16.7) | 14 (48.3) | 0.034 * |
| BSA %, baseline, median (range) | 50 (15–90) | 50 (20–97) | 0.817 | 40 (25–90) | 60 (20–97) | 0.216 |
| Onset age, years, median (range) | 20 (0–72) | 13 (0–51) | 0.009 * | 20 (8–72) | 10 (0.25–46) | 0.011 * |
| AD phenotype, n (%) | 0.012 * | 0.017 * | ||||
| Type I a | 22 (40.0) | 26 (65.0) | Ref. | 5 (29.4) | 16 (61.5) | Ref. |
| Type II b | 4 (7.3) | 2 (5.0) | 0.413 | 0 (0) | 2 (7.7) | 1.000 |
| Type III c | 6 (10.9) | 1 (2.5) | 0.101 | 3 (17.6) | 0 (0) | 0.028 * |
| Type IV d | 8 (14.5) | 10 (25.0) | 1.000 | 4 (23.5) | 5 (19.2) | 0.389 |
| Type V e | 7 (12.7) | 0 (0) | 0.010 * | 2 (11.8) | 3 (11.5) | 0.588 |
| Type VI f | 6 (10.9) | 1 (2.5) | 0.101 | 3 (17.6) | 0 (0) | 0.028 * |
| Type VII g | 2 (3.6) | 0 (0) | 0.225 | 0 (0) | 0 (0) | — |
| Previous use of cyclosporine, azathioprine, or methotrexate, n (%) | 36 (59.0) | 14 (31.8) | 0.010 * | 12 (66.7) | 13 (44.8) | 0.229 |
| Cyclosporine | 29 (47.5) | 9 (20.5) | 0.007 * | 10 (55.6) | 12 (41.4) | 0.382 |
| Azathioprine | 17 (27.9) | 8 (18.2) | 0.353 | 4 (22.2) | 4 (13.8) | 0.692 |
| Methotrexate | 14 (23.0) | 5 (11.4) | 0.198 | 6 (33.3) | 2 (6.9) | 0.052 |
| Disease duration until start of dupilumab, years, median (range) | 4 (0–43) | 10 (0–34) | 0.019 * | 3.5 (0–34) | 14 (0–34) | 0.091 |
| Number of dupilumab doses, median (range) | — | — | — | 18 (11–25) | 20 (14–28) | 0.010 * |
| Laboratory index, baseline, median (range) | ||||||
| Eosinophils, % | 8.1 (0.7–44.0) | 12.1 (2.0–23.8) | 0.202 | 7.7 (2.7–44.0) | 12.0 (0.9–31.0) | 0.320 |
| LDH, U/L | 189 (140–398) | 354 (241–445) | 0.045 * | 198 (198–198) | 316 (196–435) | 1.000 |
| IgE, IU/mL | 5060 (17.2–36,400) | 4101 (755–38,700) | 0.417 | 5060 (17.2–25,400) | 5000 (755–34,800) | 0.707 |
| Atopic/allergic conditions, n (%) | ||||||
| Allergic conjunctivitis | 8 (13.1) | 19 (43.2) | 0.001 * | 1 (5.6) | 9 (31.0) | 0.065 |
| Facial redness | 11 (18.3) | 9 (20.5) | 0.806 | 1 (5.6) | 10 (35.7) | 0.032 * |
| Dry eye | 3 (4.9) | 6 (13.6) | 0.161 | 1 (5.6) | 3 (10.3) | 1.000 |
| Drug interval change, n (%) | — | — | — | 14 (87.5) | 18 (62.1) | 0.094 |
| 3 weeks | — | — | — | 2 (14.3) | 8 (44.4) | 0.036 * |
| 1 month | — | — | — | 8 (57.1) | 10 (55.6) | — |
| 2 months | — | — | — | 3 (21.4) | 0 (0) | — |
| 3 months | — | — | — | 1 (7.1) | 0 (0) | — |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, C.-Y.; Lai, P.-J.; Chen, C.-B.; Chan, T.C.; Hui, R.C.-Y.; Huang, Y.-H.; Tseng, H.-C.; Lin, S.-H.; Lu, C.-W.; Lee, H.-E.; et al. Efficacy of Dupilumab on Different Phenotypes of Adult with Moderate-to-Severe Atopic Dermatitis in Taiwan: A Real-World Study. J. Clin. Med. 2022, 11, 6209. https://doi.org/10.3390/jcm11206209
Yang C-Y, Lai P-J, Chen C-B, Chan TC, Hui RC-Y, Huang Y-H, Tseng H-C, Lin S-H, Lu C-W, Lee H-E, et al. Efficacy of Dupilumab on Different Phenotypes of Adult with Moderate-to-Severe Atopic Dermatitis in Taiwan: A Real-World Study. Journal of Clinical Medicine. 2022; 11(20):6209. https://doi.org/10.3390/jcm11206209
Chicago/Turabian StyleYang, Chin-Yi, Po-Ju Lai, Chun-Bing Chen, Tom C. Chan, Rosaline Chung-Yee Hui, Yu-Huei Huang, Han-Chi Tseng, Shang-Hung Lin, Chun-Wei Lu, Hua-En Lee, and et al. 2022. "Efficacy of Dupilumab on Different Phenotypes of Adult with Moderate-to-Severe Atopic Dermatitis in Taiwan: A Real-World Study" Journal of Clinical Medicine 11, no. 20: 6209. https://doi.org/10.3390/jcm11206209
APA StyleYang, C.-Y., Lai, P.-J., Chen, C.-B., Chan, T. C., Hui, R. C.-Y., Huang, Y.-H., Tseng, H.-C., Lin, S.-H., Lu, C.-W., Lee, H.-E., Lin, J.-Y., Chi, M.-H., Tsai, M.-F., Hwang, Y.-S., Wang, C.-W., Chu, C.-Y., & Chung, W.-H. (2022). Efficacy of Dupilumab on Different Phenotypes of Adult with Moderate-to-Severe Atopic Dermatitis in Taiwan: A Real-World Study. Journal of Clinical Medicine, 11(20), 6209. https://doi.org/10.3390/jcm11206209






