Abstract
The ion shift index (ISI) is a suggested marker to reflect the magnitude of ischemic damage. This study aimed to investigate the prognostic value of the ISI for predicting poor neurological outcomes at 6 months in comatose out-of-hospital cardiac arrest (OHCA) survivors by comparing it with the OHCA and Cardiac Arrest Hospital Prognosis (CAHP) scores. This observational registry-based cohort study included adult comatose OHCA survivors admitted to a tertiary care hospital in Korea between 2015 and 2021. The ISI was calculated using the serum electrolyte levels obtained within one hour of resuscitation. The primary outcome was poor neurological function (Cerebral Performance Category score of 3–5) at 6 months. Of the 250 OHCA survivors, 164 (65.6%) had poor neurological outcomes. These patients had a higher median ISI than those with good neurological outcomes (4.95 vs. 3.26, p < 0.001). ISI (adjusted odds ratio, 2.107; 95% confidence interval, 1.350–3.288, p = 0.001) was associated with poor neurological outcomes. The prognostic performance of ISI (area under the curve [AUC], 0.859) was similar to that of the OHCA score (AUC, 0.858; p = 0.968) and the CAHP score (AUC, 0.894; p = 0.183). ISI would be a prognostic biomarker for comatose OHCA survivors that is available during the immediate post-cardiac arrest period.
1. Introduction
Hypoxic-ischemic brain injury is a major complication of out-of-hospital cardiac arrest (OHCA), which leads to about two-thirds of deaths, after intensive care unit admission, of cardiac arrest survivors [1,2]. The active withdrawal of life-sustaining treatment (WLST) for OHCA survivors presumed to survive with a poor neurological outcome accounts for most deaths rather than the direct consequence of loss of brain function [3,4,5]. The current post-resuscitation care guidelines recommend the multimodal neurologic prognostication strategy and postponing the conclusions about the neurological outcome of comatose OHCA survivors until at least 72 h after cardiac arrest; therefore, to minimize premature WLST in patients who might have a chance at neurological recovery [6]. However, the early distinguishment of OHCA survivors presumed to have an irreversible brain injury and anticipated with the minimal benefit of aggressive life-sustaining treatment is essential to avoid futile treatment [6,7].
Recently, many risk scores for supporting emergency clinical decision-making for OHCA survivors, such as the OHCA, MIRACLE2, and Cardiac Arrest Hospital Prognosis (CAHP) scores, were developed; however, they require precise history taking [8,9,10]. Although, cardiac arrest characteristics such as initial cardiac arrest rhythms, collapse time, and the time of initiation of cardiopulmonary resuscitation (CPR) are generally available at the emergency department (ED) admission for OHCA survivors. The reliability of the information is limited due to inaccurate recall or recording, even in the well-established emergency medical service system [8,11]. From that point of view, biomarkers are independent of such bias and are easy to interpret [12,13]. The ion shift index (ISI) has been introduced as a prognostic factor to reflect the magnitude of ischemia damage, defined as the ratio between the concentration of serum intracellular fluid (ICF) ions, i.e., potassium, phosphate, and magnesium, and that of serum extracellular fluid (ECF) ion, i.e., calcium [14,15].
This study aimed to investigate the prognostic value of ISI, during the immediate post-cardiac arrest period, for predicting poor neurological outcomes at 6 months in comatose OHCA survivors and compare the performance to previous prognostic scores, including OHCA and CAHP [8,10].
2. Materials and Methods
2.1. Study Design and Population
This retrospective, observational, registry-based cohort study was conducted in the emergency department (ED) of a tertiary university-affiliated hospital in Seoul, South Korea. Consecutive adult OHCA patients (aged ≥ 18 years) admitted to the ED have been enrolled in the OHCA registry since 2010, and we extracted the data from this registry [16]. All patients in the registry were followed-up with up to 6 months after ED admission. Their neurological status at 1 and 6 months were assessed using the Cerebral Performance Category (CPC) scores by reviewing the electronic medical records for hospitalized patients or interviewing via a follow-up telephone call with the patient or primary caregiver [16]. The Institutional Review Board of Asan Medical Center approved the study protocol (No. 2022-0743) and waived the need for informed consent due to the retrospective nature of the study.
This study included all consecutive adult patients with successfully resuscitated OHCA, who were admitted to the hospital between January 2015 and December 2021. The excluded patients were those who: (1) were transferred from other hospitals after the return of spontaneous circulation (ROSC); (2) signed advance directives before cardiac arrest; (3) did not undergo the laboratory test within an hour after ROSC; (4) had a poor neurological status prior to cardiac arrest, defined as a CPC of 3 or 4; (5) had chronic renal failure; or (6) refused to participate in the follow-up.
2.2. Management and Data Collection
All patients received treatment in accordance with the then-current advanced cardiac life support guidelines [6,17,18,19,20]. During the immediate post-cardiac arrest period, diagnostic studies such as electrocardiography, bedside echocardiography, and computed tomography were performed to identify the cause of OHCA with general intensive care management. The patients received coronary reperfusion and targeted temperature management (TTM) with a target core body temperature of 33 °C or 36 °C using an Arctic Sun Energy Transfer Pad (Medivance Corp., Louisville, CO, USA) if indicated. WSLT was legally prohibited in South Korea until February 2018, and all patients were admitted to hospitals with conservative treatment until death or recovery.
Demographic and clinical data regarding age, sex, previous medical history, presence of a witness on collapse, initial monitored rhythm, arrest cause, time from collapse to CPR, the resuscitation duration, laboratory data during the immediate post-cardiac arrest period, and neurological outcome at 6 months were extracted. For this study, the ISI, OHCA, and CAHP scores were calculated [8,10,14,15]. The ISI was calculated using the following equation:
The primary endpoint of this study was a poor neurological outcome at 6 months, defined as a CPC score of 3 (severe cerebral disability), 4 (coma or vegetative status), or 5 (brain death).
2.3. Statistical Analysis
Continuous variables were presented as a mean with standard deviations when normally distributed and a median with interquartile ranges when non-normally distributed, based on the Kolmogorov–Smirnov test. Categorical data were presented as absolute numbers with percentages. Comparisons of the characteristics between the good and poor neurological outcome groups were performed using the chi-square test or Fisher’s exact test for categorical variables and the Mann–Whitney U test or Student’s t-test for continuous variables, as appropriate. Univariate logistic analysis was first performed to evaluate the prognostic ability of each variable, and the variables with a p-value of <0.10 in the univariate analysis were analyzed by multivariate logistic regression based on a backward elimination method. The results of the logistic regression analysis were summarized using odds ratios (ORs) and the respective 95% confidence intervals (CIs). Variables were tested for goodness of fit using a Hosmer–Lemeshow test. The receiver operating characteristic curves were examined to determine the performance of ISI, OHCA, and CAHP scores in predicting a poor neurological outcome at 6 months [8,10]. The area under the curve (AUC) for each variable was calculated and compared using DeLong’s test [21]. The optimal cutoff value of ISI was determined using the Youden index, which defines the cutoff in terms of the maximal sum of sensitivity and specificity. A two-tailed p-value of <0.05 was considered significant. All statistical analyses were performed using IBM SPSS for Windows, version 21.0 (IBM Corp., Armonk, NY, USA) and R (version 3.6.1; R Foundation for Statistical Computing, Vienna, Austria; https://www.R-project.org, accessed on 30 May 2022).
3. Results
From January 2015 to December 2021, 364 adult OHCA patients were admitted to the ED of our hospital and received post-cardiac arrest care (Figure 1). Among these cases, 250 patients were finally included in our study after the exclusion of 114 patients who were transferred from other hospitals after the ROSC (n = 52), underwent laboratory tests an hour after ROSC (n = 8), had a poor pre-arrest neurological status (n = 11), had chronic renal failure (n = 42), or refused to follow-up (n = 1). A total of 164 patients (65.6%) in this cohort had a poor neurological outcome (CPC score ≥ 3) at 6 months after ROSC.
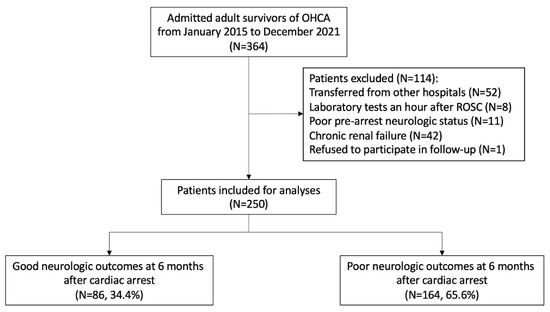
Figure 1.
Flow diagram for the enrolment of the patients in the study. Abbreviations: OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation.
The baseline characteristics and laboratory results are presented in Table 1. Patients with poor neurological outcomes were older (median, 55.6 vs. 64.0 years, p = 0.001) and had a lower rate of witnessed cardiac arrest (88.4% vs. 71.3%, p = 0.002) and initial shockable rhythm (70.9% vs. 23.8%; p < 0.001). Total collapse time and resuscitation duration were longer in the poor neurological outcome group, while the no flow time did not significantly differ between the two groups. All laboratory results during the immediate post-cardiac arrest period significantly differed between the two groups; the concentrations of serum ICF ions, including potassium, phosphate, and magnesium, were higher in the poor neurological outcome group, while that of the serum ECF, i.e., calcium, was lower. The proportion of TTM did not differ significantly between the patients with good and poor neurological outcomes (77.9% vs. 84.1%, p = 0.223). In patients with a poor neurological outcome, the ISI was higher than that of those with a good neurological outcome (median, 3.26 vs. 4.95, p < 0.001), as were the OHCA (mean, 21.35 vs. 41.24, p < 0.001) and CAHP (median, 118.35 vs. 203.62, p < 0.001) scores.

Table 1.
Demographic and clinical characteristics of the patients with out-of-hospital cardiac arrest.
In the univariate logistic regression analysis, age, previous diabetes mellitus, unwitnessed collapse, initial non-shockable rhythm, arrest cause, resuscitation duration, pH, lactate levels, and ISI were associated with a poor neurological outcome at 6 months (Table 2). In multivariate logistic regression analysis, ISI (adjusted OR, 2.107; 95% CI, 1.350–3.288; p = 0.001) is associated with poor neurological outcomes at six months. The AUC for ISI was 0.859 (95% CI, 0.812–0.906), similar to that of the OHCA (0.858; 95% CI, 0.810–0.906; p = 0.968) and CAHP (0.894; 95% CI, 0.849–0.938; p = 0.183) scores (Figure 2).

Table 2.
Logistic regression analysis for a 6-month poor neurological outcome in the patients with out-of-hospital cardiac arrest.
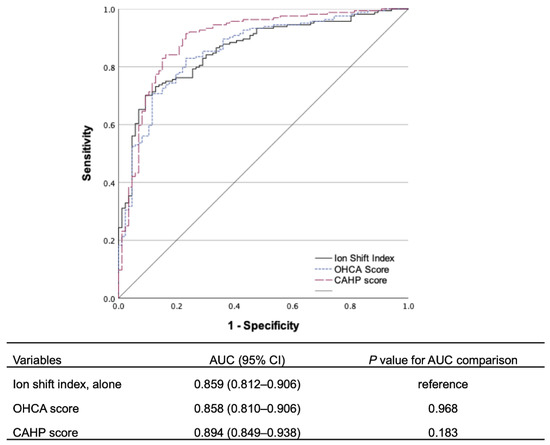
Figure 2.
Comparison of the prognostic performances of ion shift index, out-of-hospital cardiac arrest (OHCA), and Cardiac Arrest Hospital Prognosis (CAHP) scores for predicting a poor neurological outcome at 6 months. Abbreviations: AUC, area under the curve; CI, confidence interval.
The optimal cutoff value for ISI, based on the Youden index, was 4.25, with a 70.1% sensitivity and a 90.7% specificity (Table 3). An ISI-value of >6.40 predicted a poor neurological outcome at 6 months with a 0% false positive rate and a 24.4% sensitivity.

Table 3.
Ion Shift Index cutoff values in predicting a poor neurological outcome at 6 months.
4. Discussion
This registry-based cohort study demonstrated that ISI during the immediate post-cardiac arrest period was independently associated with a poor neurological outcome at 6 months, which implied that ISI could be used as a prognostic biomarker available within an hour after ROSC. Without other clinical factors, ISI, using the serum concentration level of potassium, phosphate, magnesium, and calcium, showed similar prognostic performance for a 6-month neurological outcome in comatose OHCA survivors compared to the OHCA and CAHP scores. Considering that ISI is an objective prognostic biomarker that does not rely on memory and records, it could be useful for OHCA survivors during the immediate post-cardiac arrest period, especially when combined with other predictive clinical features.
Electrolyte derangement is common in cardiac arrest survivors. Ischemic injury due to cardiac arrest alters the energy-dependent membrane-bound ionic pumps and results in cell membrane dysfunction and homeostasis loss. The efflux of potassium and magnesium ions from the cytoplasm and rapid phosphate production from the adenosine triphosphate breakdown occurs in the early phase of hypoxia without the inhibition of the sodium-potassium adenosine triphosphatase pump and the absence of cell injury. This is followed by the influx of sodium, chloride, and calcium ions and a further loss of cytoplasmic potassium and magnesium in accord with the ionic pump dysfunction and cellular injury [22,23]. The cell swelling and electrolyte derangements are evident even in the reversible phase of cell injury. The high permeability of the cellular membrane in the irreversible phase of cell injury results in the influx of extracellular calcium and exacerbates damage to the mitochondria and cytoskeleton, leading to cell death [23].
Previous studies revealed that levels of even a single electrolyte, including potassium and phosphate, had a significant association with the outcome in cardiac arrest survivors [24,25]. Lee et al. hypothesized that the ISI would reflect the degree of cellular damage and demonstrated that a higher ISI was associated with poor neurological outcomes at discharge in 580 in-hospital and out-of-hospital cardiac arrest survivors (adjusted OR, 2.916; 95% CI, 1.798–4.730) with an AUC of 0.878 [14]. Consistent with this previous study, our study also demonstrated that a higher ISI was associated with a poor neurological outcome at 6 months in comatose OHCA survivors (adjusted OR, 2.107; 95% CI, 1.350–3.288) with an AUC of 0.859.
Many risk stratification tools for OHCA survivors in the immediate post-cardiac arrest period have been developed for better treatment strategies and allocations of medical resources [8,10,26]. In this study, the prognostic performance of ISI (AUC, 0.859) was similar to other risk stratification scores including the OHCA (0.858; 95% CI, 0.810–0.906; p = 0.968) and CAHP (0.894; 95% CI, 0.849–0.938; p = 0.183) scores in predicting the poor neurological outcome of OHCA survivors. Compared to these clinical scores, ISI is easier to calculate and can be used in emergencies independent of clinical information. Several established clinical variables used in the OHCA and CAHP scores, including age, a witnessed arrest, initial rhythm, resuscitation duration, and pH, were also significantly associated with outcome in this cohort. Combining ISI with these clinical factors would result in an enhanced prognostic performance, which suggests that ISI is a potential biomarker to be incorporated into future studies to establish optimal treatment strategies for OHCA patients in immediate post-resuscitation duration.
This study has several limitations. First, this study was a retrospective, observational, registry-based cohort study performed in a single center, which limited the generalizability of the results and made the presence of unmeasurable confounding bias inevitable. Second, this study included OHCA patients between 2015 and 2021, and the treatment guidelines have been since updated [6,17,18,19,20]. This could affect the clinical decision-making of the physician and, consequently, the outcome for OHCA survivors. In addition, not all patients underwent TTM, which could affect the outcome. Third, this study excluded 42 patients (11.5% from the registry) diagnosed with chronic renal failure before OHCA, which might cause a selection bias. However, patients with chronic renal failure might have electrolyte derangement, such as hyperkalaemia, before cardiac arrest, and therefore the ISI of such patients would not purely reflect the degree of the cell injury after cardiac arrest [27,28]. In addition, other medical conditions such as endocrine disorders or medications such as furosemide, indapamide, and spironolactone could result in the pre-arrest electrolyte imbalance and would interfere with the ISI performance. Finally, the withdrawal of life-sustaining treatments (WLST) or death after awakening would confound the 6-month neurological outcome. In our cohort, there was no premature WLST during targeted temperature management, and the WLST was illegal before February 2018 in South Korea, indicating the low risk of self-fulfilling prophecy bias.
5. Conclusions
This study validated that the ISI reflects the degree of cell damage in OHCA survivors, and its use alone (without other added measures) showed a similar prognostic performance to other risk stratification scores. ISI is a potential objective prognostic biomarker for predicting neurological outcomes, which does not rely on memory and records and can be easily applied during the immediate post-cardiac arrest period. Further studies incorporating ISI into other variables for predicting neurological outcomes in OHCA survivors are warranted.
Author Contributions
Conceptualization, Y.-J.K.; methodology, Y.-J.K.; validation, B.K., H.K., S.-M.K., J.-S.K., and S.M.R.; formal analysis, Y.-J.K.; investigation, B.K. and Y.-J.K.; resources, H.K., S.-M.K., J.-S.K., and W.Y.K.; data curation, B.K., H.K., S.-M.K., J.-S.K., and S.M.R.; writing—original draft preparation, B.K. and Y.-J.K.; writing—review and editing, all authors; visualization, B.K.; supervision, W.Y.K.; project administration, Y.-J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the National Research Foundation of Korea (NRF-2021R1A2C2014304) and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI18C2383). The study sponsors had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by The Institutional Review Board of Asan Medical Center who also approved the study protocol (No. 2022-0743).
Informed Consent Statement
Patient consent was waived due to the retrospective study.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Sandroni, C.; Cronberg, T.; Sekhon, M. Brain injury after cardiac arrest: Pathophysiology, treatment, and prognosis. Intensiv. Care Med. 2021, 47, 1393–1414. [Google Scholar] [CrossRef] [PubMed]
- Lemiale, V.; Dumas, F.; Mongardon, N.; Giovanetti, O.; Charpentier, J.; Chiche, J.D.; Carli, P.; Mira, J.P.; Nolan, J.; Cariou, A. Intensive care unit mortality after cardiac arrest: The relative contribution of shock and brain injury in a large cohort. Intensiv. Care Med. 2013, 39, 1972–1980. [Google Scholar] [CrossRef]
- Sandroni, C.; D’Arrigo, S.; Callaway, C.W.; Cariou, A.; Dragancea, I.; Taccone, F.S.; Antonelli, M. The rate of brain death and organ donation in patients resuscitated from cardiac arrest: A systematic review and meta-analysis. Intensiv. Care Med. 2016, 42, 1661–1671. [Google Scholar] [CrossRef]
- Elmer, J.; Torres, C.; Aufderheide, T.P.; Austin, M.A.; Callaway, C.W.; Golan, E.; Herren, H.; Jasti, J.; Kudenchuk, P.J.; Scales, D.C.; et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation 2016, 102, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Witten, L.; Gardner, R.; Holmberg, M.J.; Wiberg, S.; Moskowitz, A.; Mehta, S.; Grossestreuer, A.V.; Yankama, T.; Donnino, M.W.; Berg, K.M. Reasons for death in patients successfully resuscitated from out-of-hospital and in-hospital cardiac arrest. Resuscitation 2019, 136, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Sandroni, C.; Böttiger, B.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Genbrugge, C.; Haywood, K.; Lilja, G.; Moulaert, V.R.M.; et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: Post-resuscitation care. Intensiv. Care Med. 2021, 47, 369–421. [Google Scholar] [CrossRef]
- Sandroni, C.; D’Arrigo, S.; Cacciola, S.; Hoedemaekers, C.W.E.; Westhall, E.; Kamps, M.J.A.; Taccone, F.S.; Poole, D.; Meijer, F.J.A.; Antonelli, M.; et al. Prediction of good neurological outcome in comatose survivors of cardiac arrest: A systematic review. Intensiv. Care Med. 2022, 48, 389–413. [Google Scholar] [CrossRef]
- Adrie, C.; Cariou, A.; Mourvillier, B.; Laurent, I.; Dabbane, H.; Hantala, F.; Rhaoui, A.; Thuong, M.; Monchi, M. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: The OHCA score. Eur. Heart J. 2006, 27, 2840–2845. [Google Scholar] [CrossRef]
- Pareek, N.; Kordis, P.; Beckley-Hoelscher, N.; Pimenta, D.; Kocjancic, S.T.; Jazbec, A.; Nevett, J.; Fothergill, R.; Kalra, S.; Lockie, T.; et al. A practical risk score for early prediction of neurological outcome after out-of-hospital cardiac arrest: MIRACLE2. Eur. Heart J. 2020, 41, 4508–4517. [Google Scholar] [CrossRef]
- Maupain, C.; Bougouin, W.; Lamhaut, L.; Deye, N.; Diehl, J.L.; Geri, G.; Perier, M.C.; Beganton, F.; Marijon, E.; Jouven, X.; et al. The CAHP (Cardiac Arrest Hospital Prognosis) score: A tool for risk stratification after out-of-hospital cardiac arrest. Eur. Heart J. 2016, 37, 3222–3228. [Google Scholar] [CrossRef]
- Yoon, J.C.; Kim, Y.J.; Ahn, S.; Jin, Y.H.; Lee, S.W.; Song, K.J.; Shin, S.D.; Hwang, S.O.; Kim, W.Y. Factors for modifying the termination of resuscitation rule in out-of-hospital cardiac arrest. Am. Heart J. 2019, 213, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Lascarrou, J.B.; Miailhe, A.F.; le Gouge, A.; Cariou, A.; Dequin, P.F.; Reignier, J.; Coupez, E.; Quenot, J.P.; Legriel, S.; Pichon, N.; et al. NSE as a predictor of death or poor neurological outcome after non-shockable cardiac arrest due to any cause: Ancillary study of HYPERION trial data. Resuscitation 2021, 158, 193–200. [Google Scholar] [CrossRef]
- Ryoo, S.M.; Kim, Y.J.; Sohn, C.H.; Ahn, S.; Seo, D.W.; Kim, W.Y. Prognostic Abilities of Serial Neuron-Specific Enolase and Lactate and their Combination in Cardiac Arrest Survivors During Targeted Temperature Management. J. Clin. Med. 2020, 9, 159. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Jung, Y.H.; Jeung, K.W.; Lee, B.K.; Youn, C.S.; Mamadjonov, N.; Kim, J.W.; Heo, T.; Min, Y.I. Ion shift index as a promising prognostic indicator in adult patients resuscitated from cardiac arrest. Resuscitation 2019, 137, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Lee, S.M.; Jeung, K.W.; Lee, B.K.; Han, J.H.; Heo, T.; Min, Y.I. Association between ion shift index and prognosis in severe trauma patients without isolated head injury. Injury 2021, 52, 1151–1157. [Google Scholar] [CrossRef]
- Kim, Y.J.; Kim, M.J.; Koo, Y.S.; Kim, W.Y. Background Frequency Patterns in Standard Electroencephalography as an Early Prognostic Tool in Out-of-Hospital Cardiac Arrest Survivors Treated with Targeted Temperature Management. J. Clin. Med. 2020, 9, 1113. [Google Scholar] [CrossRef]
- Callaway, C.W.; Donnino, M.W.; Fink, E.L.; Geocadin, R.G.; Golan, E.; Kern, K.B.; Leary, M.; Meurer, W.J.; Peberdy, M.A.; Thompson, T.M.; et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S465–S482. [Google Scholar] [CrossRef]
- Nolan, J.P.; Soar, J.; Cariou, A.; Cronberg, T.; Moulaert, V.R.; Deakin, C.D.; Bottiger, B.W.; Friberg, H.; Sunde, K.; Sandroni, C. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care 2015: Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015, 95, 202–222. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef]
- Kim, Y.-M.; Jeung, K.W.; Kim, W.Y.; Park, Y.S.; Oh, J.S.; You, Y.H.; Lee, D.H.; Chae, M.K.; Jeong, Y.J.; Kim, M.C.; et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 5. Post-cardiac arrest care. Clin. Exp. Emerg. Med. 2021, 8, S41–S64. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Thandroyen, F.T.; Bellotto, D.; Katayama, A.; Hagler, H.K.; Willerson, J.T.; Buja, L.M. Subcellular electrolyte alterations during progressive hypoxia and following reoxygenation in isolated neonatal rat ventricular myocytes. Circ. Res. 1992, 71, 106–119. [Google Scholar] [CrossRef]
- Miller, M.; Zachary, J. Mechanisms and Morphology of Cellular Injury, Adaptation, and Death. Pathol. Basis of Vet. Dis. 2017, 17. [Google Scholar]
- Skrifvars, M.B.; Pettilä, V.; Rosenberg, P.H.; Castrén, M. A multiple logistic regression analysis of in-hospital factors related to survival at six months in patients resuscitated from out-of-hospital ventricular fibrillation. Resuscitation 2003, 59, 319–328. [Google Scholar] [CrossRef]
- Jung, Y.H.; Lee, B.K.; Jeung, K.W.; Youn, C.S.; Lee, D.H.; Lee, S.M.; Heo, T.; Min, Y.I. Prognostic value of serum phosphate level in adult patients resuscitated from cardiac arrest. Resuscitation 2018, 128, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Sauneuf, B.; Dupeyrat, J.; Souloy, X.; Leclerc, M.; Courteille, B.; Canoville, B.; Ramakers, M.; Goddé, F.; Beygui, F.; du Cheyron, D.; et al. The CAHP (cardiac arrest hospital prognosis) score: A tool for risk stratification after out-of-hospital cardiac arrest in elderly patients. Resuscitation 2020, 148, 200–206. [Google Scholar] [CrossRef]
- Pun, P.H.; Goldstein, B.A.; Gallis, J.A.; Middleton, J.P.; Svetkey, L.P. Serum Potassium Levels and Risk of Sudden Cardiac Death Among Patients with Chronic Kidney Disease and Significant Coronary Artery Disease. Kidney Int. Rep. 2017, 2, 1122–1131. [Google Scholar] [CrossRef]
- Shamseddin, M.K.; Parfrey, P.S. Sudden cardiac death in chronic kidney disease: Epidemiology and prevention. Nat. Rev. Nephrol. 2011, 7, 145–154. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).