Abstract
Background: Obesity, and in particular extreme obesity, as a global health problem is an important risk factor for many diseases, including atherosclerotic cardiovascular disease (ACVD). Bariatric surgery might stop or slow atherogenesis by decreasing excessive weight in the early stages of atherogenesis, by suppressing low-grade systemic inflammation as well as by inhibiting oxidative stress and endothelial dysfunction. The aim of this meta-analysis was to provide an answer to whether bariatric surgery has a significant effect on intima-media thickness (IMT) which is a surrogate marker of early atherosclerosis and has a good correlation with atherosclerotic coronary heart disease. Methods: A systematic literature search in PubMed, Scopus, Embase, and Web of Science as well as grey literature was performed from inception to 1 July 2022. The meta-analysis was performed using Comprehensive Meta-Analysis (CMA) V3 software. Overall, the estimate of effect size was measured by a random effects meta-analysis. To account for the heterogeneity of studies regarding study design, characteristics of the populations, and treatment duration, a random-effects model (using the DerSimonian–Laird method) and the generic inverse variance weighting approach were used. To assess the existence of publication bias in the meta-analysis, the funnel plot, Begg’s rank correlation, and Egger’s weighted regression tests were used. Results: The meta-analysis of 30 trials, including 1488 subjects, demonstrated a significant decrease in IMT after bariatric surgery. The reduction in IMT was also robust in the leave-one-out sensitivity analysis. It must be stressed that the results of the random-effects meta-regression did not suggest any relationship between the changes in IMT and delta body mass index (BMI) or duration of follow-up after the bariatric surgery. However, the subgroup analyses showed a better IMT reduction after laparoscopic sleeve gastrectomy (LSG) when compared to Roux-en-Y gastric bypass (RYGB). Within a year, the IMT follow-up values showed a further improvement. Conclusions: Bariatric surgery significantly reduced IMT. Significant associations were found between the surgery type and IMT changes, as well as a significant effect of follow-up duration on the changes of IMT after bariatric surgery.
1. Introduction
Almost all countries are witnessing a pandemic of overweight and obesity with a devastating trend, which is best illustrated by the fact that obesity has nearly tripled since 1975. In 2016, more than 1.9 billion adults aged 18 years and older were overweight and 3% of the world’s population, or more than 650 million people, were obese with an increasing prevalence [1]. In most developed countries, the rates of obesity are much higher so that, for example, in the USA more than 40% of adults are obese [2]. It is well known that obesity as a global health issue is also an important risk factor for many diseases, including atherosclerotic cardiovascular disease (ACVD), and it is associated with an increased ACVD morbidity and mortality [3]. This is primarily explained by a systemic low-grade inflammatory state in obesity which is not only a risk for ACVD but also for metabolic syndrome (MetSy), type 2 diabetes mellitus (T2DM), nonalcoholic fatty liver disease (NAFLD), nonalcoholic steatohepatitis (NASH), chronic kidney disease, different types of cancers, and other inflammatory diseases, including pancreatitis, psoriasis, atopic dermatitis, and autoimmune arthritis [4,5,6,7,8]. Obesity is also associated with oxidative stress which may promote the development of vascular wall lesions causing endothelial dysfunction; thus, predisposing the arterial wall to morphological and functional damages leading to atherogenesis.
No matter how it is achieved, weight reduction decreases the risk of ACVD, cardiovascular events, as well as cardiovascular and total mortality. Bariatric surgery is a surgical treatment, which is used primarily for patients who are severely obese to decrease their excessive weight. The types of bariatric surgery are sleeve gastrectomy (SG), laparoscopic adjustable gastric band (LAGB), Roux-en-Y gastric bypass (RYGB), biliopancreatic diversion/duodenal switch (BPD/DS), and one anastomosis gastric bypass/mini gastric bypass (OAGB/MGB) [9]. There are data suggesting the positive impact of bariatric surgery on several cardiometabolic indicators [10,11,12,13,14,15]. There have been reports indicating that bariatric surgery might prevent or slow down atherogenesis in the early stages by breaking the vicious circle between inflammation and endothelial dysfunction [16].
Measuring intima-media thickness (IMT), particularly carotid IMT (CIMT), by ultrasonography is considered to be a surrogate marker of early atherosclerotic changes in the arteries. This could help to improve the prediction of cardiovascular events in different arterial territories because of the positive correlation between increased IMT and atherosclerotic changes in coronary arteries, i.e., with coronary heart disease (CHD) [17,18,19,20]. Therefore, IMT is used in predicting CHD and improving the cardiovascular risk prediction models. Although some studies have suggested that bariatric surgery has a beneficial effect and might decrease IMT, other studies could not find any change in IMT in obese patients after bariatric surgery.
Following bariatric surgery, several cardiovascular-related risk factors can be improved, including insulin resistance, type 2 diabetes, hypertension, and hyperlipidemia; however, it is worth mentioning that these improvements are not the only effect of weight loss [21,22]. Since obesity provokes an inflammation-prone environment, bariatric surgery seems to decrease cytokines involved in this process, especially CRP and IL-6, as shown in a recent meta-analysis [23,24,25].
Since the data concerning the effects of bariatric surgery on IMT are conflicting, the aim of this systematic review and meta-analysis is to provide a clear answer as to whether bariatric surgery can decrease IMT or not.
2. Methods
2.1. Search Strategy
The 2009 preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines were used to prepare this systematic review and meta-analysis [26]. PubMed, Scopus, Embase, Web of Science, as well as grey literature (CareSearch, Google, and the Grey Literature Report), and all reference lists of retrieved articles were searched from inception to 1 July 2022 using the following keywords in titles and abstracts: (“intima media thickness” OR “intima-media thickness” OR “carotid intima media thickness” OR “carotid intima media” OR “artery intima media thickness” OR “intima media thickness measurement” OR “intima media thickness cardiovascular” OR “carotid intima media thickness measurement” OR “intima-media thickness measurements” OR “carotid intima media thickness cardiovascular” OR “intima-media thickness” OR CIMT OR IMT OR “carotid intima-media thickness” OR “carotid intima media” OR “Carotid atherosclerosis” OR “intima-media”) AND (“bariatric surgery” OR gastroplast* OR “gastric bypass” OR “Roux-en-Y” OR “gastric band” OR “biliopancreatic diversion” OR gastrectom* OR “duodenal switch” OR “weight loss surgery” OR “gastrointestinal diversion” OR gastroenterostom* OR “jejunoileal bypass” OR “obesity surgery” OR “weight-loss surgery” OR “bariatric procedure” OR “sleeve surgery” OR “metabolic surgery”).
2.2. Study Selection
All studies investigating the effects of bariatric surgery on carotid intima media thickness (CIMT) were included, based upon our pre-determined inclusion criteria. Case studies, non-English studies, reviews, and animal studies were not considered. A study had to provide documented CIMT data before surgery and after a post-operative observation period to be included in this meta-analysis. This systematic review and meta-analysis was not registered in any registry.
2.3. Data Extraction
All titles and abstracts were separately screened by two authors (TJ and MA). When there was a disagreement concerning the eligibility of a study, the paper was examined collaboratively, and a decision was reached. Study characteristics (the name of the primary author, the year of publication, study design, type of surgery, length of follow-up, health status of the participants, major clinical and demographic variables, values of IMT, and sample size) were extracted from each study.
2.4. Quality Assessment
The Newcastle–Ottawa Scale (NOS) was used to estimate the quality of the studies included in this meta-analysis [27,28]. This scale considers three features of each qualified study: (1) study patient selection (4 elements); (2) study population comparability (one item); and (3) exposure determination (3 items) in case-control studies or result of interest in cohort studies.
2.5. Quantitative Data Synthesis
The meta-analysis was performed using Comprehensive Meta-Analysis (CMA) V3 software (Biostat Inc., Englewood, NJ, USA) [29]. The weighted mean difference (WMD) with relevant CIs was determined for continuous outcomes. From each group, sample sizes, means, and standard deviations were obtained for each relevant outcome to calculate WMD. Overall, the estimate of effect size was measured by a random effects meta-analysis. To account for the heterogeneity of studies with regard to study design, characteristics of the populations, and treatment duration, the random-effects model (using the DerSimonian–Laird method) and the generic inverse variance weighting approach were used [26]. Sensitivity analysis using the leave-one-out approach (i.e., deleting one study each time and repeating the analysis) was applied to analyze the effect of each study on the overall effect size [30].
2.6. Meta-Regression
To investigate the association between BMI change and follow-up duration after surgery with the estimated effect size, these parameters were included into a random-effect meta-regression model.
2.7. Subgroup Analysis
A subgroup analysis was completed to describe heterogeneity, and to further characterize outcomes for the type of surgery and follow-up period.
2.8. Publication Bias
The funnel plot, Egger’s weighted regression, as well as Begg’s rank correlation tests were used to examine the presence of publication bias in the meta-analysis. The “trim and fill” approach was used to insert potentially missing studies when there were indications of funnel plot asymmetry. In the case of a significant result, the number of potentially missing studies needed to make the p-value non-significant was determined using the “fail-safe N” approach as another evidence of publication bias [31].
3. Results
Among 356 published studies identified by a systematic databases search, 173 were directly related to the topic of this study. In total, 143 studies were excluded after careful evaluation (43 studies were reviews, 38 studies were excluded because they did not match the inclusion criteria, 34 studies did not report sufficient data, and 8 were non-English papers). Therefore, 30 studies which evaluated IMT after bariatric surgery were included (Table 1). Figure 1 shows the process of study selection.

Table 1.
Characteristics of studies measuring IMT.
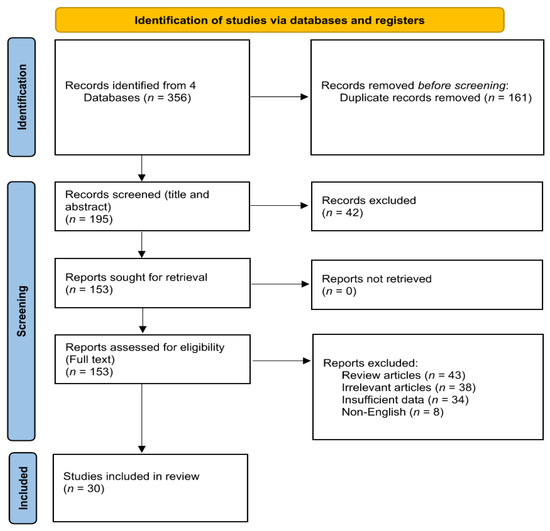
Figure 1.
Flowchart of the included studie.
3.1. Quality Assessment of the Included Studies
In cohort studies, although most of the selected studies [16,32,33,35,36,37,38,39,40,41,42,43,44,45,46,48,49,50,51,52,53,54,55,56,57,58,59,60] showed representativeness of the cases, the majority of them were distinguished by a lack of nonexposed group definition information. Since most of the studies did not include a control group, they were not assessed for comparability. In case-control studies [34,47], the included studies met the selection and exposure criteria. Quality assessment of the selected studies is presented in Table 2 and Table 3.

Table 2.
Quality of bias assessment of the included publication in accordance with the Newcastle–Ottawa scale (cohort studies).

Table 3.
Quality of bias assessment of the included publication in accordance with the Newcastle–Ottawa scale (case-control studies).
3.2. Effect of Bariatric Surgery on IMT
The meta-analysis of 30 trials, including 1488 subjects, demonstrated a significant decrease in IMT after bariatric surgery (WMD: −0.081, 95% CI: −0.101, −0.061, p < 0.001) (Figure 2A). The reduction in IMT was robust in the leave-one-out sensitivity analysis (Figure 2B). In other words, the iterative removal of each included trial from the meta-analysis did not cause a significant change in the pooled estimate of effect size.
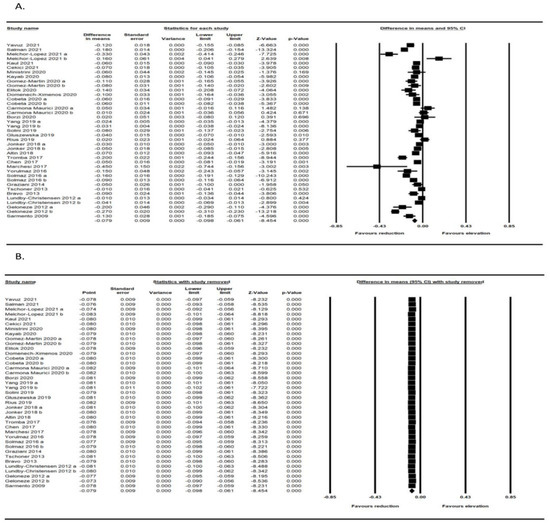
Figure 2.
(A) Forest plot displaying standardized mean difference and 95% confidence intervals showing the consequence of bariatric surgery on IMT [16,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60]; (B) Leave-one-out sensitivity analyses indicating the effect of bariatric surgery on IMT [16,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60].
3.3. Meta-Regression
The impact of potential confounders on the IMT reducing the effect of bariatric surgery was assessed by random-effects meta-regression. The findings did not suggest any relationship between the changes in IMT and delta body mass index (BMI) (slope: 0.002; 95% CI: −0.005, 0.010; p = 0.670) or duration of follow-up (slope: 0.001; 95% CI: −0.0008, 0.0034; p = 0.227) (Figure 3A,B).
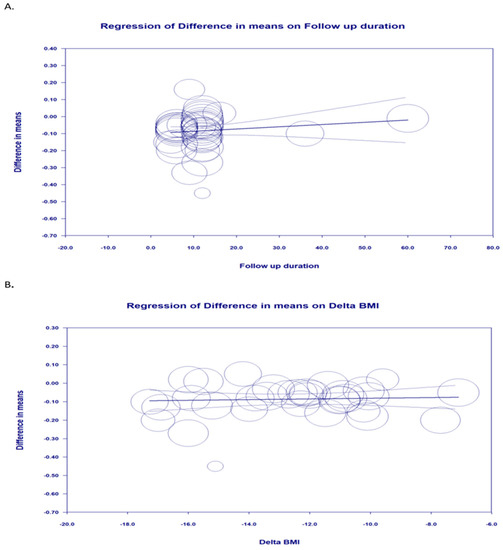
Figure 3.
Random-effects meta-regression for evaluating the effect of: (A) delta BMI; (B) follow-up duration.
3.4. Subgroup Analysis
A subgroup analysis was also performed based on surgery type and treatment duration (<12 months and ≥12 months). The subgroup analyses demonstrated significant associations between surgery types and IMT changes (p < 0.001). The improvement of IMT in patients who had laparoscopic sleeve gastrectomy (LSG) surgery was better than in those who had Roux-en-Y gastric bypass (RYGB). Furthermore, a significant effect of follow-up duration on the changes of IMT after bariatric surgery was observed with further improvement in IMT in the follow-up period of less than 12 months (Figure 4A,B).
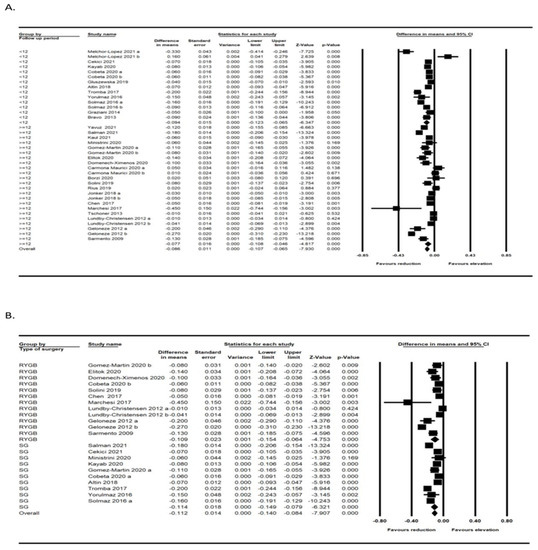
Figure 4.
Subgroup analysis based on the follow-up period [32,33,34,35,36,37,39,40,41,42,43,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60] (A) and type of surgery [33,37,38,39,40,41,42,45,49,50,52,53,54,58,59,60] (B).
3.5. Publication Bias
Although the results of Egger’s linear regression test (intercept = −2.685, standard error = 0.892; 95% CI = −4.493, −0.877, t = 3.009, df = 37, two-tailed p = 0.004) suggested that publication bias existed in the meta-analysis concerning the effect of bariatric surgery on IMT, Begg’s rank correlation test (Kendall’s Tau with continuity correction = −0.143, z = 1.282, two-tailed p-value = 0.199) did not indicate the presence of publication bias. The trim and fill test showed three “missing” studies in order to adjust publication bias. The “fail-safe N” test showed that 39 missing studies would be needed to reduce the effect size to a non-significant (p < 0.001) level (Figure 5).
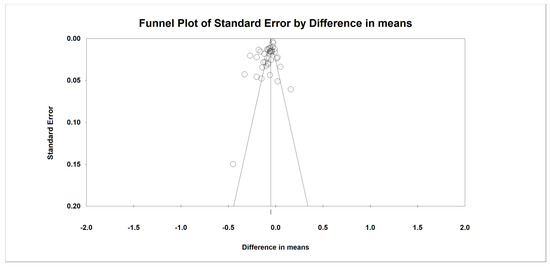
Figure 5.
Funnel plot of standard error by difference in means.
4. Discussion
The results of this meta-analysis of 30 trials, including 1488 subjects, showed a significant decrease in IMT after bariatric surgery, and the reduction in IMT was also robust in the leave-one-out sensitivity analysis. It must be stressed that the results of the random-effects meta-regression did not suggest any relationship between the changes in IMT and delta BMI or duration of follow-up after the bariatric surgery. However, the subgroup analyses showed significant associations between the surgery types and IMT changes and a significant effect of follow-up duration on the changes of IMT after bariatric surgery.
One important question which might theoretically influence the results of this meta-analysis is a sex difference in obese subjects concerning IMT. However, this issue was clarified in a recent study showing that IMT was significantly higher in men than in women but this difference disappeared after adjustment for covariables, such as waist circumference, age, HDL-cholesterol, and mean arterial blood pressure [61]. It has also been shown that bariatric surgery caused a significant IMT decrease in subjects with obesity in all age categories; however, the beneficial effects were more pronounced in younger individuals, which is quite understandable and easily explicable [48].
As already mentioned, it has been previously shown that obesity is associated with thicker arterial walls, i.e., increased IMT which seems to be independent of other cardiovascular risk factors [62,63]. It has been also shown that obesity is associated with T2DM and other risk factors for CHD such as dyslipidemia [64]. On the other hand, patients with severe dyslipidemia, such as familial hypercholesterolemia (FH), have increased IMT when compared with controls [65]. This is true not only for adult patients with FH but also for children with FH [66]. However, bariatric surgery in patients who had severe obesity caused a decrease in extremely atherogenic oxidized LDL particles in the blood and this phenomenon seemed to be dependent on BMI changes [10]. An earlier study showed that bariatric surgery caused a decrease in total cholesterol, triglycerides, oxidized LDL particles, and apolipoprotein B, and an increase in HDL-cholesterol and apolipoprotein A concentrations that occurred regardless of the type of surgical procedure; however, LDL-cholesterol only decreased after RYGB [67]. However, these authors could not find any correlation between the changes in serum lipid concentrations and those in IMT. A recent meta-analysis showed that pulse wave velocity (PWV) as a measure of arterial stiffness decreased significantly after bariatric surgery. This is important because atherosclerosis causes arteries to lose their elasticity and become more stiff; thereby resulting in increased PWV which predicts subsequent ACVD events [11].
Similar to our meta-analysis, a previously published small meta-analysis showed a significant reduction in IMT after bariatric surgery and indicated that the percentage of changes in BMI were associated with changes in IMT [68]. The results of the present meta-analysis also fit well with the results of another most recently published meta-analysis of 21 population-based cohort studies, involving 2,857,016 participants, which compared the effects of bariatric surgery and nonsurgical approaches on cardiovascular outcomes in patients with obesity [69]. This meta-analysis showed that bariatric surgery reduced major adverse cardiovascular events, including the risk of myocardial infarction, stroke, cardiovascular death, and all-cause death.
The present study has some limitations. Perhaps the most important one is the fact that until relatively recently there was a lack of IMT measurement standardization (method, mean/maximal thickness, carotid segment, including or excluding plaque) which could influence the predictive value in CHD risk estimation in different studies; therefore, this might also have an impact on the results of this meta-analysis [70]. In addition, according to the observational design of the included studies, we could not perform a comparative evaluation of the effects of bariatric surgery and medical treatment on IMT.
5. Conclusions
The results of this meta-analysis suggest that bariatric surgery significantly reduced IMT. Since increased IMT reflecting early structural atherosclerotic changes in patients with severe obesity seems to be independently associated with ACVD, the results of this study may have clinical implications for individuals with severe obesity and high cardiovascular risk. This suggests a beneficial antiatherosclerotic effect of bariatric surgery. Future prospective studies with a precise follow-up, bigger sample size, and different markers that could predict the outcomes of bariatric surgery regarding elimination of co-morbidities should add more objective data to the spectrum of benefits of weight loss surgery.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Tannaz Jamialahmadi was supported by the Wael-Almahmeed and IAS research training grant.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO (World Health Organisation). Obesity and Overweight; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Centers for Disease Control and Prevention. Adult Obesity Facts; CDC: Atlanta, GA, USA, 2021.
- Kim, M.S.; Kim, W.J.; Khera, A.V.; Kim, J.Y.; Yon, D.K.; Lee, S.W.; Shin, J.I.; Won, H.-H. Association between adiposity and cardiovascular outcomes: An umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur. Heart J. 2021, 42, 3388–3403. [Google Scholar] [CrossRef] [PubMed]
- Theel, W.; Boxma-de Klerk, B.M.; Dirksmeier-Harinck, F.; van Rossum, E.F.; Kanhai, D.A.; Apers, J.; van Dalen, B.M.; de Knegt, R.J.; Holleboom, A.G.; Tushuizen, M.E. Evaluation of nonalcoholic fatty liver disease (NAFLD) in severe obesity using noninvasive tests and imaging techniques. Obes. Rev. 2022, 23, e13481. [Google Scholar] [CrossRef] [PubMed]
- Stasi, A.; Cosola, C.; Caggiano, G.; Cimmarusti, M.T.; Palieri, R.; Acquaviva, P.M.; Rana, G.; Gesualdo, L. Obesity-Related Chronic Kidney Disease: Principal Mechanisms and New Approaches in Nutritional Management. Front. Nutr. 2022, 9, 925619. [Google Scholar] [CrossRef]
- Cottam, D.R.; Mattar, S.G.; Barinas-Mitchell, E.; Eid, G.; Kuller, L.; Kelley, D.E.; Schauer, P.R. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: Implications and effects of weight loss. Obes. Surg. 2004, 14, 589–600. [Google Scholar] [CrossRef]
- Guo, Z.; Yang, Y.; Liao, Y.; Shi, Y.; Zhang, L.-J. Emerging Roles of Adipose Tissue in the Pathogenesis of Psoriasis and Atopic Dermatitis in Obesity. JID Innov. 2022, 2, 100064. [Google Scholar] [CrossRef] [PubMed]
- Van Raemdonck, K.; Umar, S.; Szekanecz, Z.; Zomorrodi, R.K.; Shahrara, S. Impact of obesity on autoimmune arthritis and its cardiovascular complications. Autoimmun. Rev. 2018, 17, 821–835. [Google Scholar] [CrossRef]
- Coelho, C.; Crane, J.; Agius, R.; McGowan, B. The bariatric-metabolic physician’s role in managing clinically severe obesity. Curr. Obes. Rep. 2021, 10, 263–273. [Google Scholar] [CrossRef]
- Jamialahmadi, T.; Reiner, Ž.; Alidadi, M.; Kroh, M.; Cardenia, V.; Xu, S.; Al-Rasadi, K.; Santos, R.D.; Sahebkar, A. The Effect of Bariatric Surgery on Circulating Levels of Oxidized Low-Density Lipoproteins Is Apparently Independent of Changes in Body Mass Index: A Systematic Review and Meta-Analysis. Oxidative Med. Cell. Longev. 2021, 2021, 4136071. [Google Scholar] [CrossRef]
- Jamialahmadi, T.; Reiner, Ž.; Alidadi, M.; Kroh, M.; Simental-Mendia, L.E.; Pirro, M.; Sahebkar, A. Impact of Bariatric Surgery on Pulse Wave Velocity as a Measure of Arterial Stiffness: A Systematic Review and Meta-analysis. Obes. Surg. 2021, 31, 4461–4469. [Google Scholar] [CrossRef]
- Jamialahmadi, T.; Alidadi, M.; Atkin, S.L.; Kroh, M.; Almahmeed, W.; Moallem, S.A.; Al-Rasadi, K.; Rodriguez, J.H.; Santos, R.D.; Ruscica, M.; et al. Effect of Bariatric Surgery on Flow-Mediated Vasodilation as a Measure of Endothelial Function: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 4054. [Google Scholar] [CrossRef]
- Jamialahmadi, T.; Jangjoo, A.; Rezvani, R.; Goshayeshi, L.; Tasbandi, A.; Nooghabi, M.J.; Rajabzadeh, F.; Ghaffarzadegan, K.; Mishamandani, Z.J.; Nematy, M. Hepatic Function and Fibrosis Assessment Via 2D-Shear Wave Elastography and Related Biochemical Markers Pre- and Post-Gastric Bypass Surgery. Obes. Surg. 2020, 30, 2251–2258. [Google Scholar] [CrossRef]
- Nabavi, N.; Ghodsi, A.; Rostami, R.; Torshizian, A.; Jamialahmadi, T.; Jangjoo, A.; Nematy, M.; Bahari, A.; Ebrahimzadeh, F.; Mahmoudabadi, E.; et al. Impact of Bariatric Surgery on Carotid Intima-Media Thickness in Patients with Morbid Obesity: A Prospective Study and Review of the Literature. Obes. Surg. 2022, 32, 1563–1569. [Google Scholar] [CrossRef]
- van Veldhuisen, S.L.; Gorter, T.M.; van Woerden, G.; de Boer, R.A.; Rienstra, M.; Hazebroek, E.J.; van Veldhuisen, D.J. Bariatric surgery and cardiovascular disease: A systematic review and meta-analysis. Eur. Heart J. 2022, 43, 1955–1969. [Google Scholar] [CrossRef] [PubMed]
- Carmona-Maurici, J.; Cuello, E.; Sánchez, E.; Miñarro, A.; Rius, F.; Bueno, M.; de la Fuente, M.C.; Olsina Kissler, J.J.; Vidal, T.; Maria, V.; et al. Impact of bariatric surgery on subclinical atherosclerosis in patients with morbid obesity. Surg. Obes. Relat. Dis. 2020, 16, 1419–1428. [Google Scholar] [CrossRef] [PubMed]
- Roumeliotis, A.; Roumeliotis, S.; Panagoutsos, S.; Theodoridis, M.; Argyriou, C.; Tavridou, A.; Georgiadis, G.S. Carotid intima-media thickness is an independent predictor of all-cause mortality and cardiovascular morbidity in patients with diabetes mellitus type 2 and chronic kidney disease. Ren. Fail. 2019, 41, 131–138. [Google Scholar] [CrossRef]
- Zhang, Y.; Fang, X.; Hua, Y.; Tang, Z.; Guan, S.; Wu, X.; Liu, H.; Liu, B.; Wang, C.; Zhang, Z. Carotid artery plaques, carotid intima–media thickness, and risk of cardiovascular events and all-cause death in older adults: A 5-year prospective, community-based study. Angiology 2018, 69, 120–129. [Google Scholar] [CrossRef]
- Saba, L.; Antignani, P.L.; Gupta, A.; Cau, R.; Paraskevas, K.I.; Poredos, P.; Wasserman, B.; Kamel, H.; Avgerinos, E.D.; Salgado, R. International Union of Angiology (IUA) consensus paper on imaging strategies in atherosclerotic carotid artery imaging: From basic strategies to advanced approaches. Atherosclerosis 2022, 354, 23–40. [Google Scholar] [CrossRef]
- Abeysuriya, V.; Perera, B.; Wickremasinghe, A. Regional and demographic variations of Carotid artery Intima and Media Thickness (CIMT): A Systematic review and meta-analysis. PLoS ONE 2022, 17, e0268716. [Google Scholar] [CrossRef]
- Gloy, V.L.; Briel, M.; Bhatt, D.L.; Kashyap, S.R.; Schauer, P.R.; Mingrone, G.; Bucher, H.C.; Nordmann, A.J. Bariatric surgery versus non-surgical treatment for obesity: A systematic review and meta-analysis of randomised controlled trials. BMJ 2013, 347, f5934. [Google Scholar] [CrossRef]
- Vest, A.R.; Heneghan, H.M.; Agarwal, S.; Schauer, P.R.; Young, J.B. Bariatric surgery and cardiovascular outcomes: A systematic review. Heart 2012, 98, 1763–1777. [Google Scholar] [CrossRef]
- Zagorski, S.M.; Papa, N.N.; Chung, M.H. The effect of weight loss after gastric bypass on Creactive protein levels. Surg. Obes. Relat. Dis. 2005, 1, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Yudkin, J.S.; Stehouwer, C.D.A.; Emeis, J.J.; Coppack, S.W. C-reactive protein in healthy subjects: Associations with obesity, insulin resistance, and endothelial dysfunction: A potential role for cytokines originating from adipose tissue? Arterioscler. Thromb. Vasc. Biol. 1999, 19, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.R. Inflammatory markers and bariatric surgery: A meta-analysis. Inflamm. Res. 2012, 61, 789–807. [Google Scholar] [CrossRef]
- Sutton, A.J.; Abrams, K.R.; Jones, D.R.; Jones, D.R.; Sheldon, T.A.; Song, F. Methods for Meta-Analysis in Medical Research; Wiley Chichester: Chichester, UK, 2000; Volume 348. [Google Scholar]
- Higgins, J.P. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.0.1; The Cochrane Collaboration: London, UK, 2008; Available online: http://www.cochrane-handbook.org (accessed on 25 April 2022).
- Wells, G.A.; Shea, B.; O’Connell, D.A.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Oxford: Oxford, UK, 2000. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis; Version 2 Biostat; Meta-Analysis: Englewood, NJ, USA, 2005. [Google Scholar]
- Banach, M.; Serban, C.; Ursoniu, S.; Rysz, J.; Muntner, P.; Toth, P.P.; Jones, S.R.; Rizzo, M.; Glasser, S.P.; Watts, G.F. Statin therapy and plasma coenzyme Q10 concentrations—A systematic review and meta-analysis of placebo-controlled trials. Pharmacol. Res. 2015, 99, 329–336. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Yavuz, D.G.; Apaydin, T.; Imre, E.; Uygur, M.M.; Yazici, D. Skin Autofluorescence and Carotid Intima-Media Thickness Evaluation Following Bariatric Surgery in Patients with Severe Obesity. Obes. Surg. 2021, 31, 1055–1061. [Google Scholar] [CrossRef] [PubMed]
- Salman, M.A.; Salman, A.A.; El Sherbiny, M.; Elkholy, S.; Youssef, A.; Labib, S.; El-Din, M.T.; Monazea, K.A.; Tourky, M.S.; Mikhail, H.M.S.; et al. Changes of Carotid Intima-Media Thickness After Sleeve Gastrectomy in High Cardiovascular Risk Patients: A Prospective Study. Obes. Surg. 2021, 31, 3541–3547. [Google Scholar] [CrossRef]
- Melchor-López, A.; Suárez-Cuenca, J.A.; Banderas-Lares, D.Z.; Peña-Sosa, G.D.L.; Salamanca-García, M.; Vera-Gómez, E.; Hernández-Patricio, A.; Gutiérrez-Buendía, J.A.; Zamora-Alemán, C.R.; Alcaráz-Estrada, S.L.; et al. Identification of adipose tissue-related predictors of the reduction in cardiovascular risk induced by metabolic surgery. J. Int. Med. Res. 2021, 49, 03000605211012569. [Google Scholar] [CrossRef]
- Kaul, A.; Kumar, A.; Baksi, A.; Singla, V.; Aggarwal, S.; Gulati, G.; Narang, R.; Kashyap, L. Impact of bariatric surgery on carotid intima-medial thickness and cardiovascular risk: Results of a prospective study. Surg. Endosc. Other Interv. Tech. 2021, 35, 6006–6012. [Google Scholar] [CrossRef]
- Cekici, Y.; Kaya, B.C.; Elkan, H. The Effect of Laparoscopic Sleeve Gastrectomy on Subclinical Atherosclerosis in Patients with Severe Obesity. Obes. Surg. 2021, 31, 738–745. [Google Scholar] [CrossRef]
- Ministrini, S.; Ricci, M.A.; Nulli Migliola, E.; De Vuono, S.; D’Abbondanza, M.; Paganelli, M.T.; Vaudo, G.; Siepi, D.; Lupattelli, G. Chemerin predicts carotid intima-media thickening in severe obesity. Eur. J. Clin. Investig. 2020, 50, e13256. [Google Scholar] [CrossRef] [PubMed]
- Kaya, B.C.; Elkan, H. The impact of weight loss after laparoscopic sleeve gastrectomy on early markers of atherosclerotic vascular disease: A prospective study. Kardiol. Pol. 2020, 78, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Martin, J.M.; Aracil, E.; Insenser, M.; de la Peña, G.; Lasunción, M.A.; Galindo, J.; Escobar-Morreale, H.F.; Balsa, J.A.; Botella-Carretero, J.I. Changes in Soluble TWEAK Concentrations, but Not Those in Amyloid-β(1–40), Are Associated with a Decrease in Carotid Intima-Media Thickness after Bariatric Surgery in Obese Women. Obes. Facts 2020, 13, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Elitok, A.; Emet, S.; Bayramov, F.; Karaayvaz, E.; Türker, F.; Barbaros, U.; Özcan, M. Effect of bariatric surgery on flow-mediated dilation and carotid intima-media thickness in patients with morbid obesity: 1-year follow-up study. Anatol. J. Cardiol. 2020, 23, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Domenech-Ximenos, B.; Cuba, V.; Daunis-i-Estadella, P.; Thio-Henestrosa, S.; Jaldo, F.; Biarnes, C.; Molina, X.; Xifra, G.; Ricart, W.; Bardera, A.; et al. Bariatric Surgery-Induced Changes in Intima-Media Thickness and Cardiovascular Risk Factors in Class 3 Obesity: A 3-Year Follow-Up Study. Obesity 2020, 28, 1663–1670. [Google Scholar] [CrossRef]
- Cobeta, P.; Osorio, A.; Cuadrado-Ayuso, M.; Garcia-Moreno, F.; Pestana, D.; Galindo, J.; Botella-Carretero, J.I. Sleeve Gastrectomy and Gastric Bypass Decrease the Carotid Intima-Media Thickness in Obese Men: Association with Weight Loss, Cardiovascular Risk Factors, and Circulating Testosterone. Obes. Surg. 2020, 30, 851–859. [Google Scholar] [CrossRef]
- Borzi, A.M.; Buscemi, C.; Corleo, D.; Randazzo, C.; Rosafio, G.; Pantuso, G.; Buscemi, S. Endothelial Function in Obese Patients Treated with Bariatric Surgery. Diabetes Metab. Syndr. Obes.-Targets Ther. 2020, 13, 247–256. [Google Scholar] [CrossRef]
- Yang, W.; Jiang, S.; Cheung, P.N.; Wang, C. Effects and predictive factors of bariatric surgery on carotid intima-media thickness in patients with obesity Cardiovascular risk and bariatric surgery. Obes. Surg. 2019, 29, 140. [Google Scholar]
- Solini, A.; Seghieri, M.; Santini, E.; Giannini, L.; Biancalana, E.; Taddei, S.; Volterrani, D.; Bruno, R.M. Renal Resistive Index Predicts Post-Bariatric Surgery Renal Outcome in Nondiabetic Individuals with Severe Obesity. Obesity 2019, 27, 68–74. [Google Scholar] [CrossRef]
- Gluszewska, A.; Gryglewska, B.; Rewiuk, K.; Zarzycki, B.; Dzieza-Grudnik, A.; Kwater, A.; Major, P.; Budzynski, A.; Gasowski, J.; Grodzicki, T. Arterial structure and function and its short- and long-term changes after bariatric surgery. J. Physiol. Pharmacol. 2019, 70, 909–916. [Google Scholar] [CrossRef]
- Rius, F.; Sanchez, E.; Betriu, A.; Baena-Fustegueras, J.A.; Yeramian, A.; Vidal, T.; Hernandez, M.; Lopez-Cano, C.; Bueno, M.; Gutierrez-Carrasquilla, L.; et al. Influence of Morbid Obesity and Bariatric Surgery Impact on the Carotid Adventitial Vasa Vasorum Signal. Obes. Surg. 2018, 28, 3935–3942. [Google Scholar] [CrossRef] [PubMed]
- Jonker, F.H.W.; van Houten, V.A.A.; Wijngaarden, L.H.; Klaassen, R.A.; de Smet, A.A.E.A.; Niezen, A.; Schelfhout, L.J.D.M.; Bruning, T.A.; van der Harst, E. Age-Related Effects of Bariatric Surgery on Early Atherosclerosis and Cardiovascular Risk Reduction. Obes. Surg. 2018, 28, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- Altin, C.; Erol, V.; Aydin, E.; Yilmaz, M.; Tekindal, M.A.; Sade, L.E.; Gulay, H.; Muderrisoglu, H. Impact of weight loss on epicardial fat and carotid intima media thickness after laparoscopic sleeve gastrectomy: A prospective study. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Tromba, L.; Tartaglia, F.; Carbotta, S.; Sforza, N.; Pelle, F.; Colagiovanni, V.; Carbotta, G.; Cavaiola, S.; Casella, G. The Role of Sleeve Gastrectomy in Reducing Cardiovascular Risk. Obes. Surg. 2017, 27, 1145–1151. [Google Scholar] [CrossRef]
- Chen, J.; Yu, H.Y.; Chen, L.; Wu, L.; Hu, B.; Bao, Y.Q.; Jiang, L.X. Effect of Roux-en-Y gastric bypass on carotid intima-media thickness in Chinese obese patients with type 2 diabetes. Surg. Obes. Relat. Dis. 2017, 13, 1530–1535. [Google Scholar] [CrossRef]
- Marchesi, F.; Giacosa, R.; Reggiani, V.; De Sario, G.; Tartamella, F.; Melani, E.; Mita, M.T.; Cinieri, F.G.; Cecchini, S.; Ricco, M.; et al. Morphological Changes in the Carotid Artery Intima after Gastric Bypass for Morbid Obesity. Obes. Surg. 2017, 27, 357–363. [Google Scholar] [CrossRef]
- Yorulmaz, G.; Cilekar, M.; Bilge, U.; Akcan, E.; Akalin, A. Carotid intima-media thickness and insulin resistance changes in patients who underwent sleeve gastrectomy: A prospective study. Niger. J. Clin. Pract. 2016, 19, 344–348. [Google Scholar] [CrossRef]
- Solmaz, A.; Arlcl, S.; Gülçiçek, O.B.; Yavuz, E.; Yiǧitbaş, H.; Erçetin, C.; Öncü, M.; Çelebi, F.; Çelik, A.; Kutaniş, R. Influence of Bariatric Surgery on Carotid Intima-Media Thickness. Bariatr. Surg. Pract. Patient Care 2016, 11, 56–60. [Google Scholar] [CrossRef]
- Graziani, F.; Leone, A.M.; Basile, E.; Cialdella, P.; Tritarelli, A.; Della Bona, R.; Liuzzo, G.; Nanni, G.; Iaconelli, A.; Iaconelli, A.; et al. Endothelial Progenitor Cells in Morbid Obesity-Pathogenetic Implications. Circ. J. 2014, 78, 977–985. [Google Scholar] [CrossRef]
- Tschoner, A.; Sturm, W.; Gelsinger, C.; Ress, C.; Laimer, M.; Engl, J.; Laimer, E.; Muhlmann, G.; Mittermair, R.; Kaser, S.; et al. Long-term Effects of Weight Loss after Bariatric Surgery on Functional and Structural Markers of Atherosclerosis. Obesity 2013, 21, 1960–1965. [Google Scholar] [CrossRef]
- Bravo, G.G.; Bunout, D.; Mella, J.; Quiroga, E.; de la Maza, M.P.; Cavada, G.; Hirsch, S. Bariatric surgery decreases carotid intima-media thickness in obese subjects. Nutr. Hosp. 2013, 28, 1102–1108. [Google Scholar] [CrossRef]
- Lundby-Christensen, L.; Tarnow, L.; Vaag, A.; Wiinberg, N.; Hansen, D.; Worm, D.; Hvolris, L.; Naver, L.; Almdal, T. Carotid intima-media thickness is reduced 12 months after gastric bypass surgery in patients with type 2 diabetes. Diabetologia 2012, 55, S505. [Google Scholar]
- Geloneze, S.R.; Geloneze, B.; Morari, J.; Matos-Souza, J.R.; Lima, M.M.; Chaim, E.A.; Pareja, J.C.; Velloso, L.A. PGC1α gene Gly482Ser polymorphism predicts improved metabolic, inflammatory and vascular outcomes following bariatric surgery. Int. J. Obes. 2012, 36, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Sarmento, P.L.F.A.; Plavnik, F.L.; Zanella, M.T.; Pinto, P.E.; Miranda, R.B.; Ajzen, S.A. Association of carotid intima-media thickness and cardiovascular risk factors in women pre- and post-bariatric surgery. Obes. Surg. 2009, 19, 339–344. [Google Scholar] [CrossRef] [PubMed]
- van Mil, S.R.; Biter, L.U.; van de Geijn, G.J.M.; Birnie, E.; Dunkelgrun, M.; Ijzermans, J.N.; van der Meulen, N.; Mannaerts, G.H.; Castro Cabezas, M. The effect of sex and menopause on carotid intima-media thickness and pulse wave velocity in morbid obesity. Eur. J. Clin. Investig. 2019, 49, e13118. [Google Scholar]
- Dalmas, E.; Kahn, J.-F.; Giral, P.; Abdennour, M.; Bouillot, J.-L.; Fellahi, S.; Oppert, J.-M.; Clément, K.; Guerre-Millo, M.; Poitou, C. Intima-media thickness in severe obesity: Links with BMI and metabolic status but not with systemic or adipose tissue inflammation. Diabetes Care 2013, 36, 3793–3802. [Google Scholar] [CrossRef]
- Sandgren, T.; Sonesson, B.; Ahlgren, Å.R.; Länne, T. The diameter of the common femoral artery in healthy human: Influence of sex, age, and body size. J. Vasc. Surg. 1999, 29, 503–510. [Google Scholar] [CrossRef]
- Boras, J.; Ljubic, S.; Car, N.; Metelko, Z.; Petrovecki, M.; Lovrencic, M.V.; Reiner, Z. Lipoprotein (a) predicts progression of carotid artery intima-media thickening in patients with type 2 diabetes: A four-year follow-up. Wien. Klin. Wochenschr. 2010, 122, 159–164. [Google Scholar] [CrossRef]
- Reiner, Ž.; Simental-Mendía, L.; Ruscica, M.; Katsiki, N.; Banach, M.; Rasadi, K.; Jamialahmadi, T.; Sahebkar, A. Pulse wave velocity as a measure of arterial stiffness in patients with familial hypercholesterolemia: A systematic review and meta-analysis. Arch. Med. Sci. 2019, 15, 1365–1374. [Google Scholar] [CrossRef]
- Reiner, Ž. Impact of Early Evidence of Atherosclerotic Changes on Early Treatment in Children with Familial Hypercholesterolemia; American Heart Association: Dallas, TX, USA, 2014; Volume 114, pp. 233–235. [Google Scholar]
- Gómez-Martin, J.M.; Balsa, J.; Aracil, E.; Cuadrado-Ayuso, M.; Rosillo, M.; De la Peña, G.; Lasunción, M.; Escobar-Morreale, H.F.; Botella-Carretero, J.I. Beneficial changes on plasma apolipoproteins A and B, high density lipoproteins and oxidized low density lipoproteins in obese women after bariatric surgery: Comparison between gastric bypass and sleeve gastrectomy. Lipids Health Dis. 2018, 17, 145. [Google Scholar] [CrossRef]
- Lupoli, R.; Di Minno, M.; Guidone, C.; Cefalo, C.; Capaldo, B.; Riccardi, G.; Mingrone, G. Effects of bariatric surgery on markers of subclinical atherosclerosis and endothelial function: A meta-analysis of literature studies. Int. J. Obes. 2016, 40, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Borui, T.; Zhang, Y.; Wang, Y.; Wang, X.; An, Z.; Yu, X. Effect of Bariatric Surgery on Long-Term Cardiovascular Outcomes: A Systematic Review and Meta-analysis of Population-Based Cohort Studies. Surg. Obes. Relat. Dis. 2022, 18, 1074–1086. [Google Scholar]
- Poredoš, P.; Cífková, R.; Maier, J.A.M.; Nemcsik, J.; Šabovič, M.; Jug, B.; Ježovnik, M.K.; Schernthaner, G.H.; Antignani, P.L.; Catalano, M. Preclinical atherosclerosis and cardiovascular events: Do we have a consensus about the role of preclinical atherosclerosis in the prediction of cardiovascular events? Atherosclerosis 2022, 348, 25–35. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).