Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Oversight
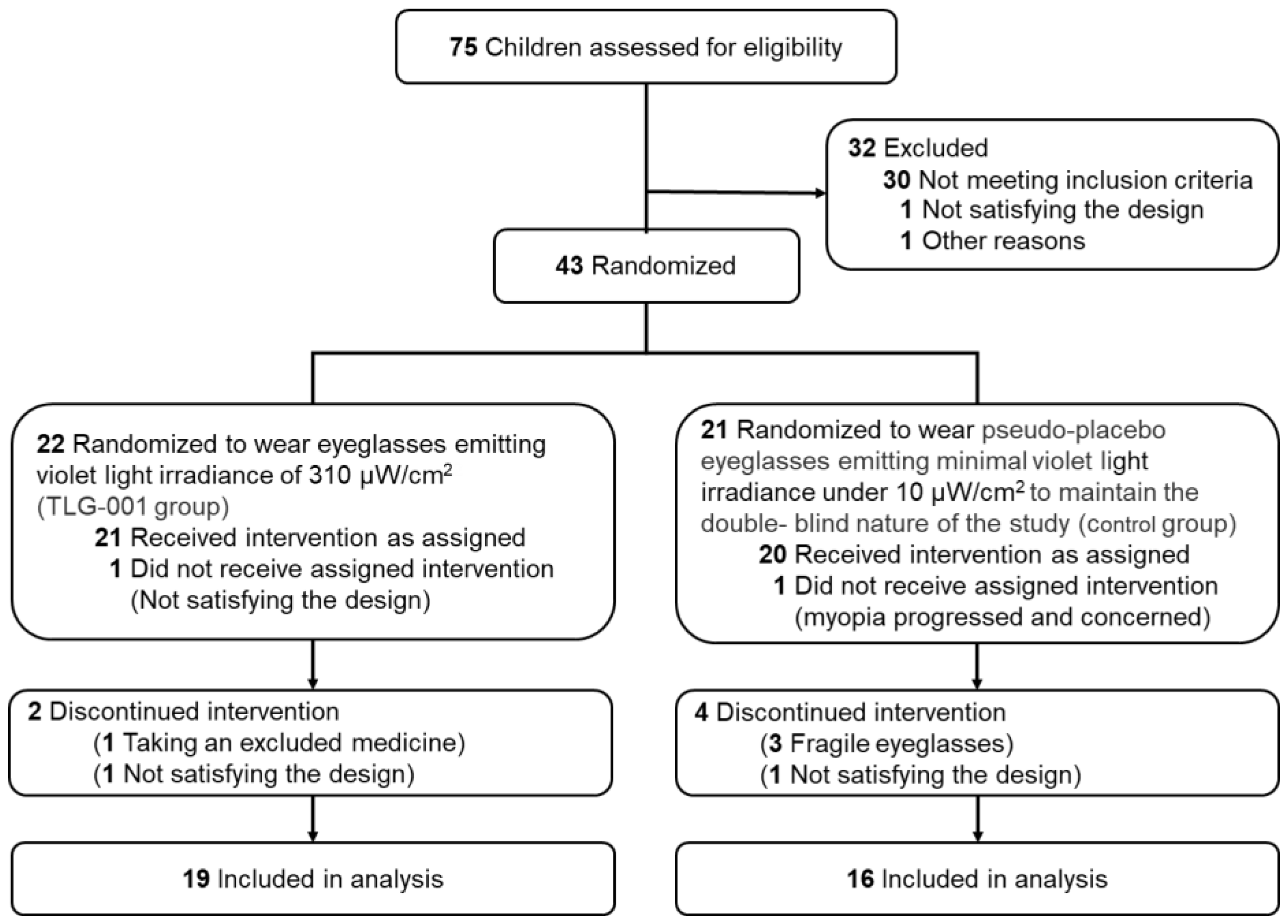
2.2. Study Objective, Design, and Setting
2.3. Randomization and Double Masking
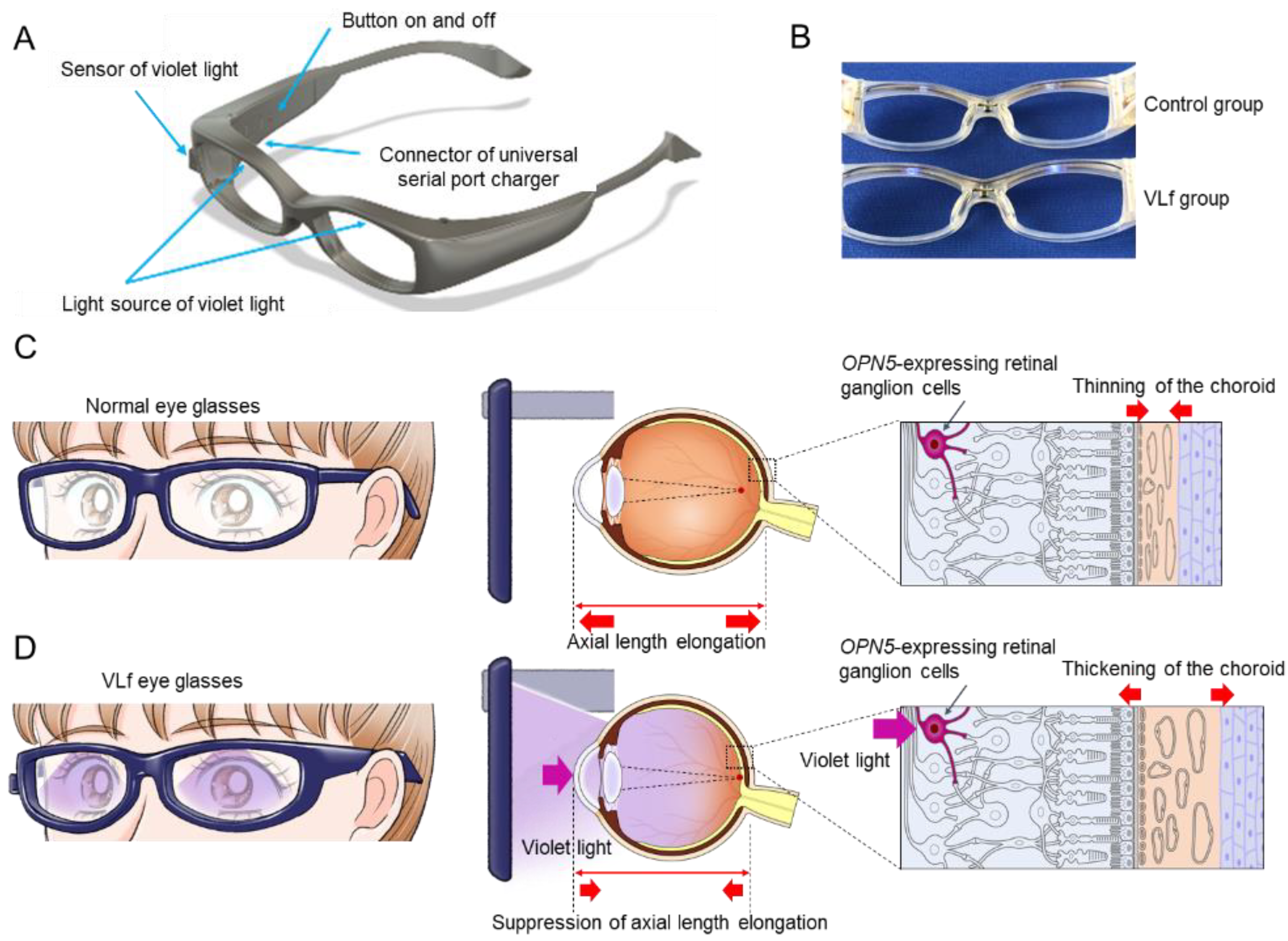
2.4. Intervention
2.5. Mechanism of Action of the Study Eyeglasses
2.6. Outcomes
2.7. Adverse Events
2.8. Statistical Analyses
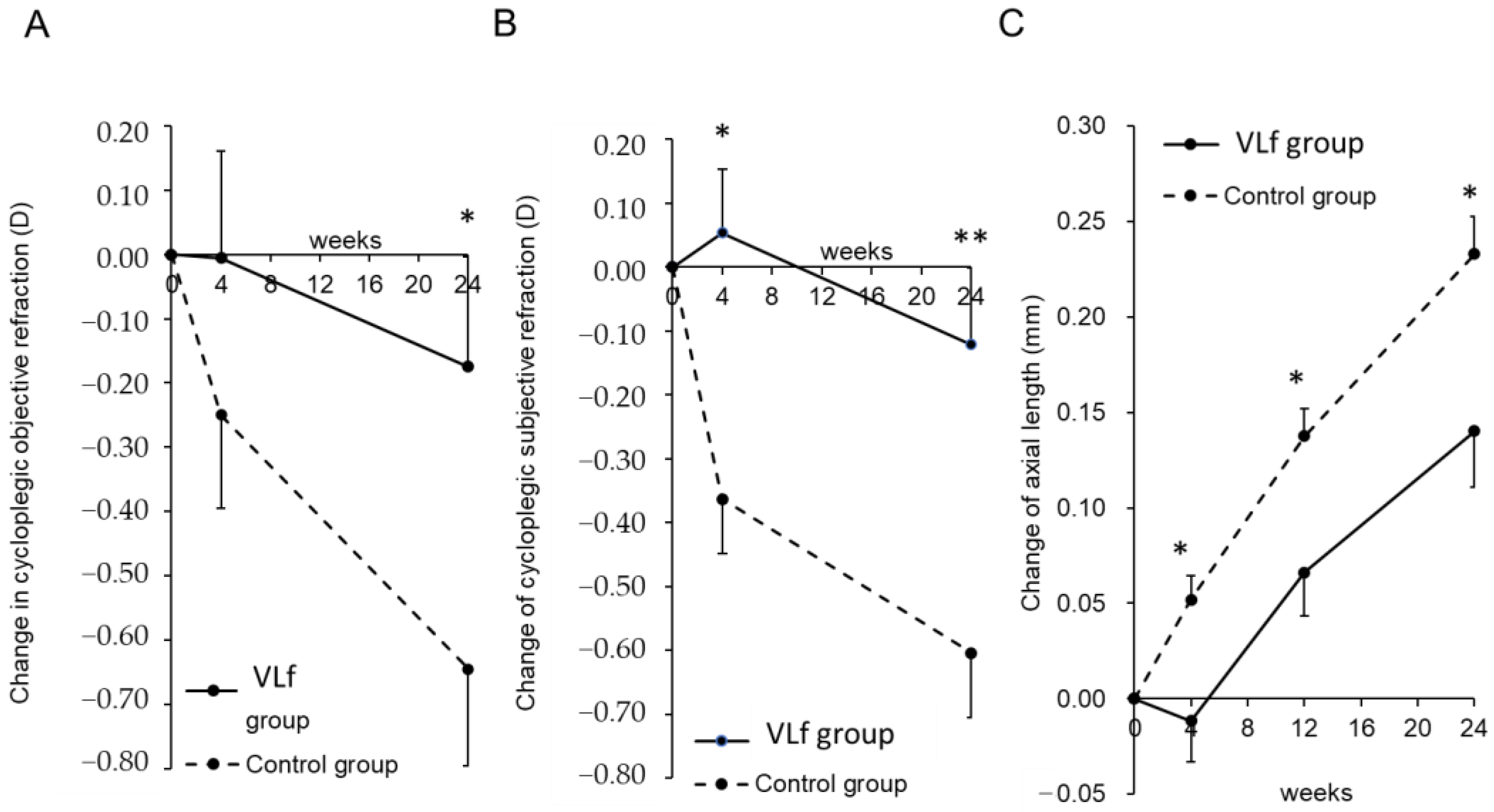
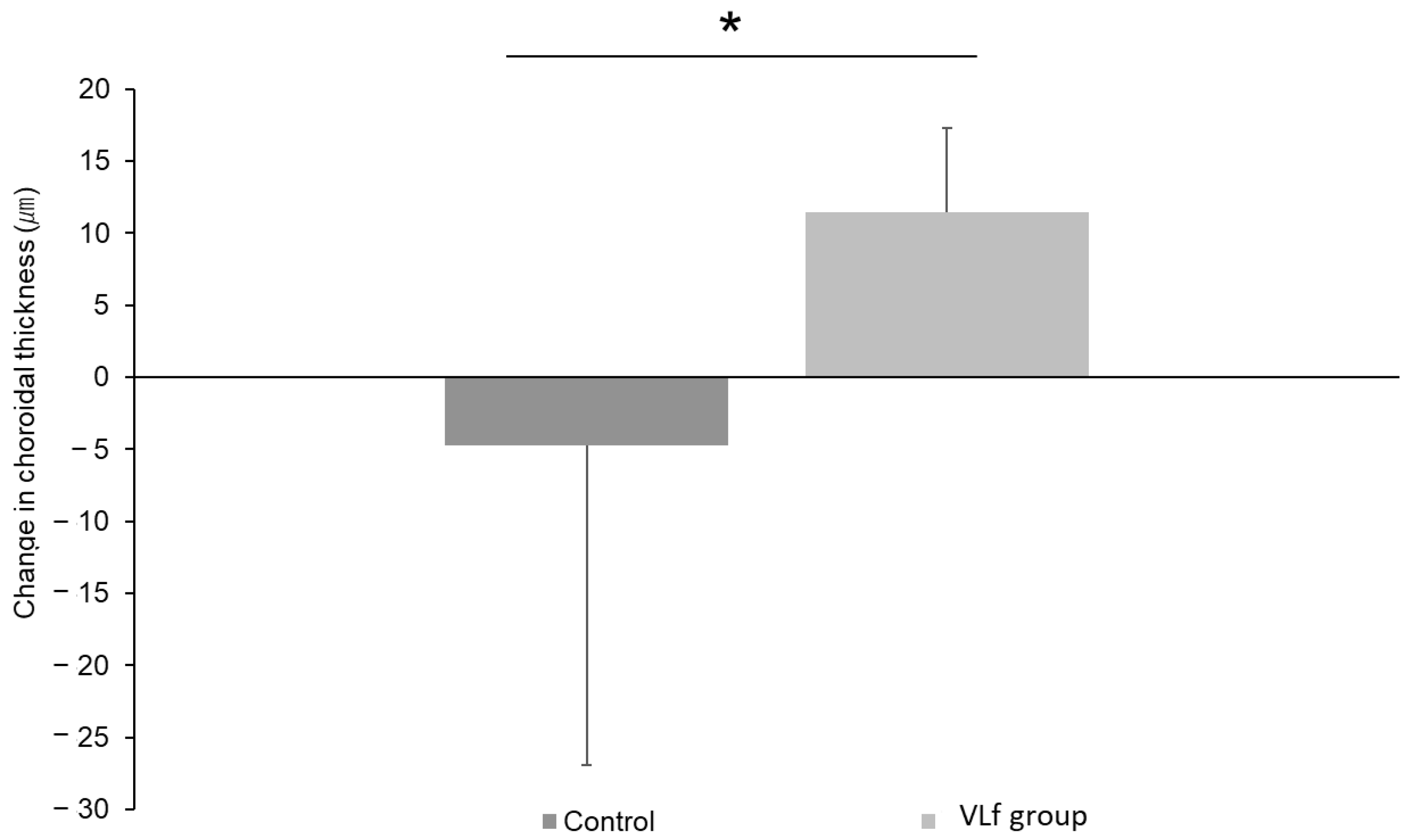
3. Results
3.1. Safety and Effectiveness Evaluations
3.2. Subgroup Analysis
3.3. Adverse Events
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef]
- Yotsukura, E.; Torii, H.; Inokuchi, M.; Tokumura, M.; Uchino, M.; Nakamura, K.; Hyodo, M.; Mori, K.; Jiang, X.; Ikeda, S.I.; et al. Current Prevalence of Myopia and Association of Myopia with Environmental Factors Among Schoolchildren in Japan. JAMA Ophthalmol. 2019, 137, 1233–1239. [Google Scholar] [CrossRef]
- Ip, J.M.; Saw, S.M.; Rose, K.A.; Morgan, I.G.; Kifley, A.; Wang, J.J.; Mitchell, P. Role of near work in myopia: Findings in a sample of Australian school children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2903–2910. [Google Scholar] [CrossRef]
- Read, S.A.; Collins, M.J.; Vincent, S.J. Light exposure and physical activity in myopic and emmetropic children. Optom. Vis. Sci. 2014, 91, 330–341. [Google Scholar] [CrossRef]
- French, A.N.; Ashby, R.S.; Morgan, I.G.; Rose, K.A. Time outdoors and the prevention of myopia. Exp. Eye Res. 2013, 114, 58–68. [Google Scholar] [CrossRef]
- Guggenheim, J.A.; Northstone, K.; McMahon, G.; Ness, A.R.; Deere, K.; Mattocks, C.; Pourcain, B.S.; Williams, C. Time outdoors and physical activity as predictors of incident myopia in childhood: A prospective cohort study. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2856–2865. [Google Scholar] [CrossRef]
- Rose, K.A.; Morgan, I.G.; Ip, J.; Kifley, A.; Huynh, S.; Smith, W.; Mitchell, P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008, 115, 1279–1285. [Google Scholar] [CrossRef]
- Jones, L.A.; Sinnott, L.T.; Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Zadnik, K. Parental history of myopia, sports and outdoor activities, and future myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3524–3532. [Google Scholar] [CrossRef]
- Jones-Jordan, L.A.; Sinnott, L.T.; Graham, N.D.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Twelker, J.D.; Zadnik, K. The contributions of near work and outdoor activity to the correlation between siblings in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study. Invest. Ophthalmol. Vis. Sci. 2014, 55, 6333–6339. [Google Scholar] [CrossRef]
- French, A.N.; Morgan, I.G.; Mitchell, P.; Rose, K.A. Risk factors for incident myopia in Australian schoolchildren: The Sydney adolescent vascular and eye study. Ophthalmology 2013, 120, 2100–2108. [Google Scholar] [CrossRef]
- Jin, J.X.; Hua, W.J.; Jiang, X.; Wu, X.Y.; Yang, J.W.; Gao, G.P.; Fang, Y.; Pei, C.L.; Wang, S.; Zhang, J.Z.; et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: The Sujiatun Eye Care Study. BMC Ophthalmol. 2015, 15, 73. [Google Scholar] [CrossRef]
- He, M.; Xiang, F.; Zeng, Y.; Mai, J.; Chen, Q.; Zhang, J.; Smith, W.; Rose, K.; Morgan, I.G. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. Jama 2015, 314, 1142–1148. [Google Scholar] [CrossRef]
- Wu, P.C.; Chen, C.T.; Chang, L.C.; Niu, Y.Z.; Chen, M.L.; Liao, L.L.; Rose, K.; Morgan, I.G. Increased Time Outdoors Is Followed by Reversal of the Long-Term Trend to Reduced Visual Acuity in Taiwan Primary School Students. Ophthalmology 2020, 127, 1462–1469. [Google Scholar] [CrossRef]
- Wu, P.C.; Chen, C.T.; Lin, K.K.; Sun, C.C.; Kuo, C.N.; Huang, H.M.; Poon, Y.C.; Yang, M.L.; Chen, C.Y.; Huang, J.C.; et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 2018, 125, 1239–1250. [Google Scholar] [CrossRef]
- Tkatchenko, T.V.; Shen, Y.; Braun, R.D.; Bawa, G.; Kumar, P.; Avrutsky, I.; Tkatchenko, A.V. Photopic visual input is necessary for emmetropization in mice. Exp. Eye Res. 2013, 115, 87–95. [Google Scholar] [CrossRef]
- Norton, T.T.; Siegwart, J.T., Jr. Light levels, refractive development, and myopia--a speculative review. Exp. Eye Res. 2013, 114, 48–57. [Google Scholar] [CrossRef]
- Karouta, C.; Ashby, R.S. Correlation between light levels and the development of deprivation myopia. Investig. Ophthalmol. Vis. Sci. 2014, 56, 299–309. [Google Scholar] [CrossRef]
- Stone, R.A.; Pardue, M.T.; Iuvone, P.M.; Khurana, T.S. Pharmacology of myopia and potential role for intrinsic retinal circadian rhythms. Exp. Eye Res. 2013, 114, 35–47. [Google Scholar] [CrossRef]
- Smith, E.L., 3rd; Hung, L.F.; Huang, J. Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Investig. Ophthalmol. Vis. Sci. 2012, 53, 421–428. [Google Scholar] [CrossRef]
- Torii, H.; Kurihara, T.; Seko, Y.; Negishi, K.; Ohnuma, K.; Inaba, T.; Kawashima, M.; Jiang, X.; Kondo, S.; Miyauchi, M.; et al. Violet Light Exposure Can Be a Preventive Strategy Against Myopia Progression. EBioMedicine 2017, 15, 210–219. [Google Scholar] [CrossRef]
- Jiang, X.; Pardue, M.T.; Mori, K.; Ikeda, S.I.; Torii, H.; D’Souza, S.; Lang, R.A.; Kurihara, T.; Tsubota, K. Violet light suppresses lens-induced myopia via neuropsin (OPN5) in mice. Proc. Natl. Acad. Sci. USA 2021, 118, e2018840118. [Google Scholar] [CrossRef]
- Ofuji, Y.; Torii, H.; Yotsukura, E.; Mori, K.; Kurihara, T.; Negishi, K.; Tsubota, K. Axial length shortening in a myopic child with anisometropic amblyopia after wearing violet light-transmitting eyeglasses for 2 years. Am. J. Ophthalmol. Case Rep. 2020, 20, 101002. [Google Scholar] [CrossRef]
- Torii, H.; Ohnuma, K.; Kurihara, T.; Tsubota, K.; Negishi, K. Violet Light Transmission is Related to Myopia Progression in Adult High Myopia. Sci. Rep. 2017, 7, 14523. [Google Scholar] [CrossRef]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef]
- Wang, J.; Li, Y.; Musch, D.C.; Wei, N.; Qi, X.; Ding, G.; Li, X.; Li, J.; Song, L.; Zhang, Y.; et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021, 139, 293–300. [Google Scholar] [CrossRef]
- Kaido, M.; Matsumoto, Y.; Shigeno, Y.; Ishida, R.; Dogru, M.; Tsubota, K. Corneal fluorescein staining correlates with visual function in dry eye patients. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9516–9522. [Google Scholar] [CrossRef]
- Mori, K.; Torii, H.; Fujimoto, S.; Jiang, X.; Ikeda, S.I.; Yotsukura, E.; Koh, S.; Kurihara, T.; Nishida, K.; Tsubota, K. The Effect of Dietary Supplementation of Crocetin for Myopia Control in Children: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 1179. [Google Scholar] [CrossRef]
- Chua, S.Y.; Sabanayagam, C.; Cheung, Y.B.; Chia, A.; Valenzuela, R.K.; Tan, D.; Wong, T.Y.; Cheng, C.Y.; Saw, S.M. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 2016, 36, 388–394. [Google Scholar] [CrossRef]
- Takeuchi, M.; Meguro, A.; Yoshida, M.; Yamane, T.; Yatsu, K.; Okada, E.; Mizuki, N. Longitudinal analysis of 5-year refractive changes in a large Japanese population. Sci. Rep. 2022, 12, 2879. [Google Scholar] [CrossRef]
- Qian, D.J.; Zhong, H.; Li, J.; Niu, Z.; Yuan, Y.; Pan, C.W. Myopia among school students in rural China (Yunnan). Ophthalmic Physiol. Opt. 2016, 36, 381–387. [Google Scholar] [CrossRef]
- Gajjar, S.; Ostrin, L.A. A systematic review of near work and myopia: Measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol. 2022, 100, 376–387. [Google Scholar] [CrossRef] [PubMed]
- Ayaki, M.; Torii, H.; Tsubota, K.; Negishi, K. Decreased sleep quality in high myopia children. Sci. Rep. 2016, 6, 33902. [Google Scholar] [CrossRef]
- Jee, D.; Morgan, I.G.; Kim, E.C. Inverse relationship between sleep duration and myopia. Acta Ophthalmol. 2016, 94, e204–e210. [Google Scholar] [CrossRef]
- Mineshita, Y.; Kim, H.K.; Shinto, T.; Kuwahara, M.; Shibata, S. Attending a Sports Club Can Help Prevent Visual Impairment Caused by Cram School in Elementary School Children in Japan. Int. J. Environ. Res. Public Health 2021, 18, 12440. [Google Scholar] [CrossRef]
- Donovan, L.; Sankaridurg, P.; Ho, A.; Chen, X.; Lin, Z.; Thomas, V.; Smith, E.L., 3rd; Ge, J.; Holden, B. Myopia progression in Chinese children is slower in summer than in winter. Optom. Vis. Sci. 2012, 89, 1196–1202. [Google Scholar] [CrossRef]
- Fujiwara, M.; Hasebe, S.; Nakanishi, R.; Tanigawa, K.; Ohtsuki, H. Seasonal variation in myopia progression and axial elongation: An evaluation of Japanese children participating in a myopia control trial. Jpn. J. Ophthalmol. 2012, 56, 401–406. [Google Scholar] [CrossRef]
- Cui, D.; Trier, K.; Munk Ribel-Madsen, S. Effect of day length on eye growth, myopia progression, and change of corneal power in myopic children. Ophthalmology 2013, 120, 1074–1079. [Google Scholar] [CrossRef]
- Gwiazda, J.; Deng, L.; Manny, R.; Norton, T.T. Seasonal variations in the progression of myopia in children enrolled in the correction of myopia evaluation trial. Investig. Ophthalmol. Vis. Sci. 2014, 55, 752–758. [Google Scholar] [CrossRef]
- Liu, Y.; Lv, H.; Jiang, X.; Hu, X.; Zhang, M.; Li, X. Intraocular Pressure Changes during Accommodation in Progressing Myopes, Stable Myopes and Emmetropes. PLoS ONE 2015, 10, e0141839. [Google Scholar] [CrossRef]
- Yan, L.; Huibin, L.; Xuemin, L. Accommodation-induced intraocular pressure changes in progressing myopes and emmetropes. Eye 2014, 28, 1334–1340. [Google Scholar] [CrossRef] [PubMed]
- Ilhan, N.; Ilhan, O.; Ayhan Tuzcu, E.; Daglioglu, M.C.; Coskun, M.; Parlakfikirer, N.; Keskin, U. Is there a relationship between pathologic myopia and dry eye syndrome? Cornea 2014, 33, 169–171. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.L.; Wu, W.F.; Liou, Y.M. Dose-Response Relationship of Outdoor Exposure and Myopia Indicators: A Systematic Review and Meta-Analysis of Various Research Methods. Int. J. Environ. Res. Public Health 2019, 16, 2595. [Google Scholar] [CrossRef] [PubMed]
- Mori, K.; Torii, H.; Hara, Y.; Hara, M.; Yotsukura, E.; Hanyuda, A.; Negishi, K.; Kurihara, T.; Tsubota, K. Effect of Violet Light-Transmitting Eyeglasses on Axial Elongation in Myopic Children: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 5462. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Chen, W.; Zhao, F.; Zhou, Q.; Reinach, P.S.; Deng, L.; Ma, L.; Luo, S.; Srinivasalu, N.; Pan, M.; et al. Scleral hypoxia is a target for myopia control. Proc. Natl. Acad. Sci. USA 2018, 115, E7091–E7100. [Google Scholar] [CrossRef]
- Zhao, F.; Zhang, D.; Zhou, Q.; Zhao, F.; He, M.; Yang, Z.; Su, Y.; Zhai, Y.; Yan, J.; Zhang, G.; et al. Scleral HIF-1α is a prominent regulatory candidate for genetic and environmental interactions in human myopia pathogenesis. EBioMedicine 2020, 57, 102878. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, L.; Xu, Y.; Pang, Z.; Mu, G. The influence of the choroid on the onset and development of myopia: From perspectives of choroidal thickness and blood flow. Acta Ophthalmol. 2021, 99, 730–738. [Google Scholar] [CrossRef]
- Zhou, X.; Zhang, S.; Yang, F.; Yang, Y.; Huang, Q.; Huang, C.; Qu, J.; Zhou, X. Decreased Choroidal Blood Perfusion Induces Myopia in Guinea Pigs. Investig. Ophthalmol. Vis. Sci. 2021, 62, 30. [Google Scholar] [CrossRef]
| Characteristic | Category | VLf | Control | p–Value | |
|---|---|---|---|---|---|
| Number of cases | 21 | 20 | |||
| Number of eyes | 42 | 40 | |||
| Age (years) | 9.8 ± 1.7 | 9.6 ± 1.3 | 0.588 | † | |
| Sex | Male | 15 (71.4%) | 11 (55.0%) | 0.275 | †† |
| Female | 6 (28.6%) | 9 (45.0%) | |||
| Parents with myopia | Both parents | 14 (66.7%) | 15 (75.0%) | 0.473 | †† |
| Only father | 5 (23.8%) | 2 (10.0%) | |||
| Only mother | 2 (9.5%) | 3 (15.0%) | |||
| Uncorrected visual acuity (log MAR) | 0.81 ± 0.23 | 0.86 ± 0.25 | 0.312 | † | |
| Best corrected visual acuity (log MAR) | −0.09 ± 0.03 | −0.08 ± 0.03 | 0.291 | † | |
| Cycloplegic subjective refraction (SE, diopters) | −2.41 ± 1.01 | −2.40 ± 0.83 | 0.97 | † | |
| Cycloplegic objective refraction (SE, diopters) | −2.53 ± 0.99 | −2.57 ± 0.80 | 0.853 | † | |
| Axial length (mm) | 24.58 ± 0.61 | 24.59 ± 0.75 | 0.928 | † | |
| Intraocular pressure (mmHg) | 17.1 ± 2.6 | 17.5 ± 2.5 | 0.482 | † | |
| Tear film breakup time (seconds) | 7.0 ± 2.2 | 6.0 ± 1.2 | 0.014 * | † | |
| Fluorescein corneal and conjunctival | 0.1 ± 0.3 | 0.1 ± 0.3 | 0.951 | † | |
| staining score | |||||
| Corneal endothelial cell density | 2917 ± 207 | 2940 ± 226 | 0.634 | † | |
| (cells/mm2) | |||||
| Environmental factors | |||||
| Time of near work (min/day) | 88.8 ± 89.2 | 59.3 ± 59.1 | 0.221 | † | |
| Time of sunlight exposure (min/day) | 52.9 ± 41.2 | 64.0 ± 68.4 | 0.527 | † | |
| Time of sleeping (min/day) | 520.0 ± 41.7 | 533.5 ± 36.7 | 0.279 | † | |
| Distance of reading (cm) | 24.6 ± 7.8 | 24.8 ± 6.6 | 0.962 | † | |
| Club activity | Outdoor | 12 (57.1%) | 15 (75.0%) | 0.2 | †† |
| Indoor | 8 (38.1%) | 4 (20.0%) | |||
| None/unknown | 1 (4.8%) | 1 (5.0%) | |||
| Time of outdoor activity | 0≤ <30 | 0 (0%) | 0 (0%) | 0.522 | †† |
| before entering elementary school | |||||
| (min/day) | 30≤ <60 | 2 (9.5%) | 1 (5.0%) | ||
| 60≤ <120 | 9 (42.9%) | 6 (30.0%) | |||
| 120≤ | 10 (47.6%) | 13 (65.0%) | |||
| No. of Subjects | 41 Patients | VLf (n = 20) | Control (n = 21) |
|---|---|---|---|
| Associated adverse reactions | No. of subjects | 0 | 0 |
| Conjunctival hyperemia | 0 | 0 | |
| Corneal abnormality | 0 | 0 | |
| Lens opacity | 0 | 0 | |
| Inflammation of anterior chamber | 0 | 0 | |
| Fundus abnormality | 0 | 0 | |
| Abnormal findings in OCT | 0 | 0 | |
| Periorbital skin abnormality | 0 | 0 | |
| Adverse events | No. of subjects | 11 | 7 |
| Influenza infection | 1 | 1 | |
| EB virus infection | 1 | 0 | |
| Streptococcal infection | 1 | 0 | |
| Epipharyngitis | 3 | 2 | |
| Mumps | 1 | 0 | |
| Sudden deafness | 1 | 0 | |
| Nausea | 0 | 1 | |
| Abdominal pain | 0 | 1 | |
| Application site erythema | 1 | 1 | |
| Fracture | 1 | 2 | |
| Eyelid contusion | 1 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torii, H.; Mori, K.; Okano, T.; Kondo, S.; Yang, H.-Y.; Yotsukura, E.; Hanyuda, A.; Ogawa, M.; Negishi, K.; Kurihara, T.; et al. Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial. J. Clin. Med. 2022, 11, 6000. https://doi.org/10.3390/jcm11206000
Torii H, Mori K, Okano T, Kondo S, Yang H-Y, Yotsukura E, Hanyuda A, Ogawa M, Negishi K, Kurihara T, et al. Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial. Journal of Clinical Medicine. 2022; 11(20):6000. https://doi.org/10.3390/jcm11206000
Chicago/Turabian StyleTorii, Hidemasa, Kiwako Mori, Takashi Okano, Shinichiro Kondo, Hao-Yung Yang, Erisa Yotsukura, Akiko Hanyuda, Mamoru Ogawa, Kazuno Negishi, Toshihide Kurihara, and et al. 2022. "Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial" Journal of Clinical Medicine 11, no. 20: 6000. https://doi.org/10.3390/jcm11206000
APA StyleTorii, H., Mori, K., Okano, T., Kondo, S., Yang, H.-Y., Yotsukura, E., Hanyuda, A., Ogawa, M., Negishi, K., Kurihara, T., & Tsubota, K. (2022). Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial. Journal of Clinical Medicine, 11(20), 6000. https://doi.org/10.3390/jcm11206000









