Bone Mineral Density Compared to Trabecular Bone Score in Primary Hyperparathyroidism
Abstract
1. Introduction
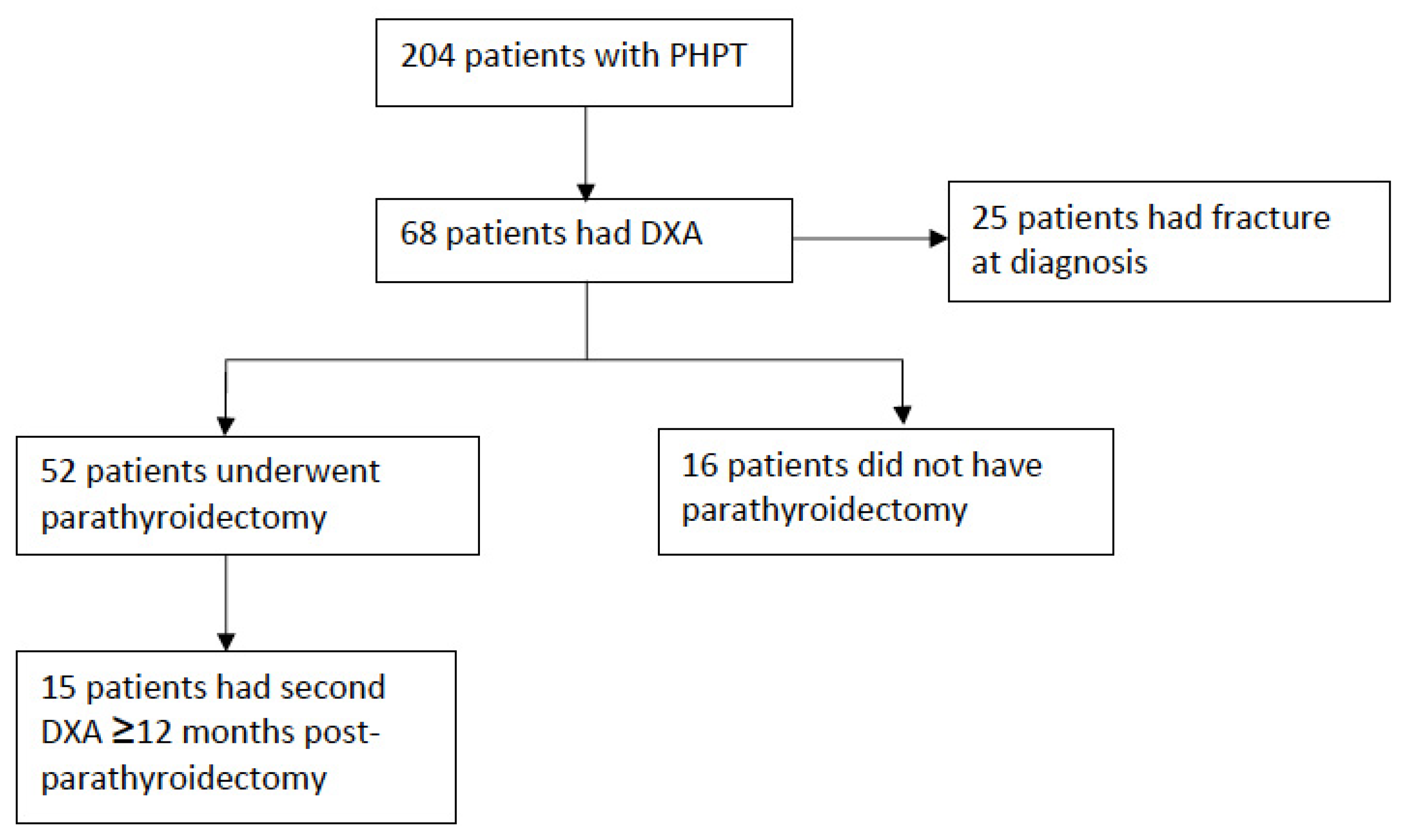
2. Materials and Methods
2.1. Participants and Setting
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
3.1. Classificaion of Bone Healh Using TBS Compared to BMD
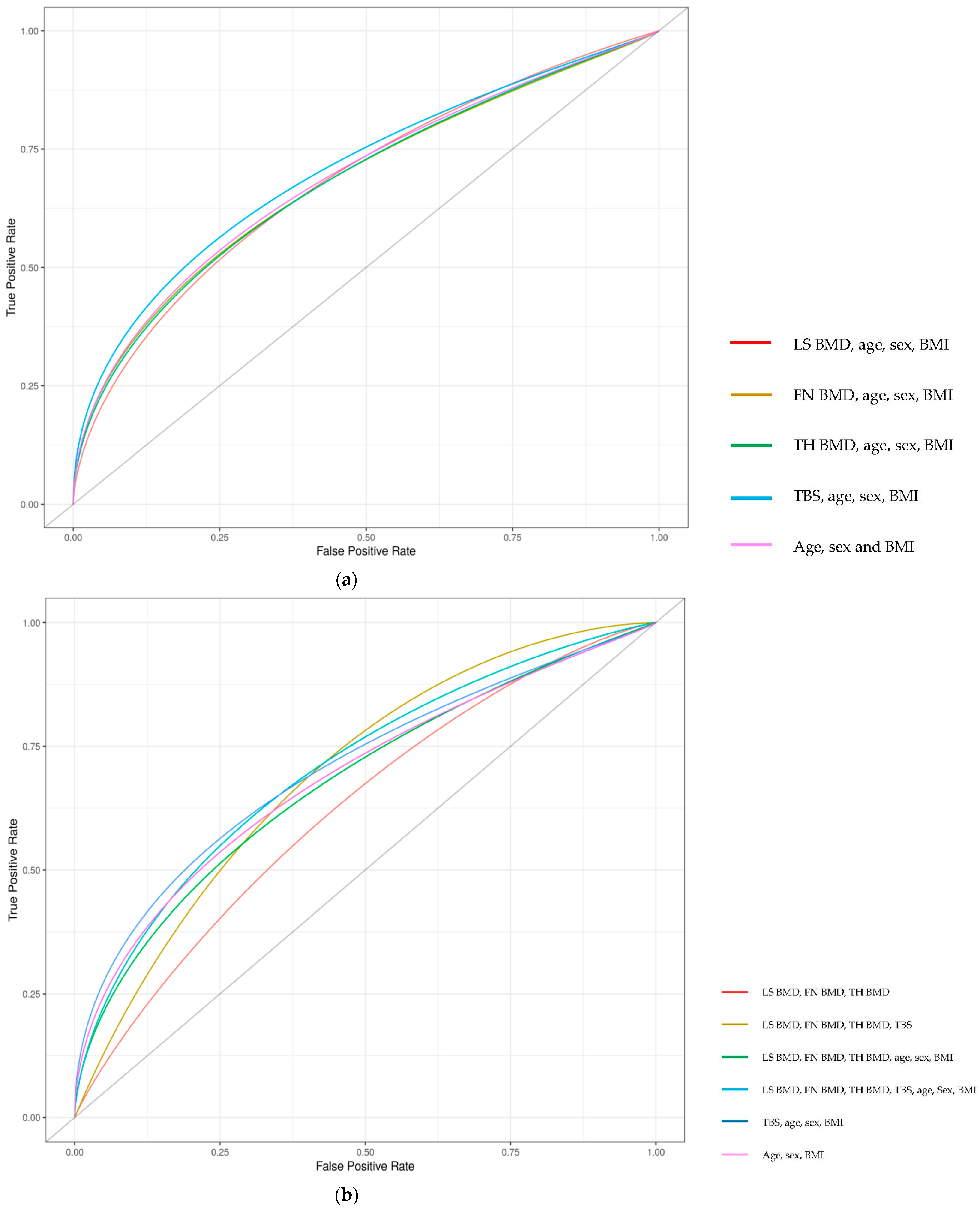
3.2. TBS Compared to BMD for Predicting Fracture
3.3. Changes in BMD and TBS after Parathyroidectomy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silverberg, S.J.; Bilezikian, J.P. Primary Hyperparathyroidism: Still Evolving? J. Bone Miner. Res. 1997, 12, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Mitlak, B.H.; Daly, M.; Potts, J.T.; Schoenfeld, D.; Neer, R.M. Asymptomatic primary hyperparathyroidism. J. Bone Miner. Res. 1991, 6, S103–S110. [Google Scholar] [CrossRef] [PubMed]
- Lewiecki, E.M.; Miller, P.D. Skeletal Effects of Primary Hyperparathyroidism: Bone Mineral Density and Fracture Risk. J. Clin. Densitom. 2013, 16, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, S.J.; Shane, E.; de la Cruz, L.; Dempster, D.W.; Feldman, F.; Seldin, D.; Jacobs, T.P.; Siris, E.S.; Cafferty, M.; Parisien, M.V.; et al. Skeletal disease in primary hyperparathyroidism. J. Bone Miner. Res. 2009, 4, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Wishart, J.; Horowitz, M.; Need, A.; Nordin, B.E.C. Relationship between Forearm and Vertebral Mineral Density in Postmenopausal Women with Primary Hyperparathyroidism. Arch. Intern. Med. 1990, 150, 1329. [Google Scholar] [CrossRef] [PubMed]
- Parisien, M.; Silverberg, S.J.; Shane, E.; De La Cruz, L.; Lindsay, R.; Bilezikian, J.P.; Dempster, D.W. The Histomorphometry of Bone in Primary Hyperparathyroidism: Preservation of Cancellous Bone Structure. J. Clin. Endocrinol. Metab. 1990, 70, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Vignali, E.; Viccica, G.; Diacinti, D.; Cetani, F.; Cianferotti, L.; Ambrogini, E.; Banti, C.; Del Fiacco, R.; Bilezikian, J.P.; Pinchera, A.; et al. Morphometric Vertebral Fractures in Postmenopausal Women with Primary Hyperparathyroidism. J. Clin. Endocrinol. Metab. 2009, 94, 2306–2312. [Google Scholar] [CrossRef] [PubMed]
- Khosla, S.; Melton, L.J.; Wermers, R.A.; Crowson, C.S.; O’Fallon, W.M.; Riggs, B.L. Primary Hyperparathyroidism and the Risk of Fracture: A Population-Based Study. J. Bone Miner. Res. 1999, 14, 1700–1707. [Google Scholar] [CrossRef] [PubMed]
- Ejlsmark-Svensson, H.; Bislev, L.S.; Lajlev, S.; Harsløf, T.; Rolighed, L.; Sikjaer, T.; Rejnmark, L. Prevalence and Risk of Vertebral Fractures in Primary Hyperparathyroidism: A Nested Case-Control Study. J. Bone Miner. Res. 2018, 33, 1657–1664. [Google Scholar] [CrossRef]
- Charopoulos, I.; Tournis, S.; Trovas, G.; Raptou, P.; Kaldrymides, P.; Skarandavos, G.; Katsalira, K.; Lyritis, G.P. Effect of Primary Hyperparathyroidism on Volumetric Bone Mineral Density and Bone Geometry Assessed by Peripheral Quantitative Computed Tomography in Postmenopausal Women. J. Clin. Endocrinol. Metab. 2006, 91, 1748–1753. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.M.; Silva, B.C.; Boutroy, S.; Zhou, B.; Wang, J.; Udesky, J.; Zhang, C.; McMahon, D.J.; Romano, M.; Dworakowski, E.; et al. Primary hyperparathyroidism is associated with abnormal cortical and trabecular microstructure and reduced bone stiffness in postmenopausal women. J. Bone Miner. Res. 2013, 28, 1029–1040. [Google Scholar] [CrossRef]
- Vu, T.D.; Wang, X.F.; Wang, Q.; Cusano, N.E.; Irani, D.; Silva, B.; Ghasem-Zadeh, A.; Udesky, J.; Romano, M.E.; Zebaze, R.; et al. New insights into the effects of primary hyperparathyroidism on the cortical and trabecular compartments of bone. Bone 2013, 55, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.C.; Broy, S.B.; Boutroy, S.; Schousboe, J.T.; Shepherd, J.; Leslie, W. Fracture Risk Prediction by Non-BMD DXA Measures: The 2015 ISCD Official Positions Part 2: Trabecular Bone Score. J. Clin. Densitom. 2015, 18, 309–330. [Google Scholar] [CrossRef]
- Boutroy, S.; Hans, D.; Sornay-Rendu, E.; Vilayphiou, N.; Winzenrieth, R.; Chapurlat, R. Trabecular bone score improves fracture risk prediction in non-osteoporotic women: The OFELY study. Osteoporos. Int. 2013, 24, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Hans, D.; Goertzen, A.; Krieg, M.-A.; Leslie, W. Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: The manitoba study. J. Bone Miner. Res. 2011, 26, 2762–2769. [Google Scholar] [CrossRef] [PubMed]
- Leib, E.; Winzenrieth, R.; Lamy, O.; Hans, D. Comparing Bone Microarchitecture by Trabecular Bone Score (TBS) in Caucasian American Women with and without Osteoporotic Fractures. Calcif. Tissue Int. 2014, 95, 201–208. [Google Scholar] [CrossRef]
- Leslie, W.; Aubry-Rozier, B.; Lix, L.; Morin, S.; Majumdar, S.; Hans, D. Spine bone texture assessed by trabecular bone score (TBS) predicts osteoporotic fractures in men: The Manitoba Bone Density Program. Bone 2014, 67, 10–14. [Google Scholar] [CrossRef]
- Nassar, K.; Paternotte, S.; Kolta, S.; Fechtenbaum, J.; Roux, C.; Briot, K. Added value of trabecular bone score over bone mineral density for identification of vertebral fractures in patients with areal bone mineral density in the non-osteoporotic range. Osteoporos. Int. 2014, 25, 243–249. [Google Scholar] [CrossRef]
- Colson, F.; Picard, A.; Rabier, B.; Vignon, E. Trabecular bone microarchitecture alteration in glucocorticoid treated women in clinical routine? A TBS evaluation. J. Bone Miner. Res. 2009, 24, 129. [Google Scholar]
- Leslie, W.D.; Aubry-Rozier, B.; Lamy, O.; Hans, D.; Manitoba Bone Density Program. TBS (Trabecular Bone Score) and Diabetes-Related Fracture Risk. J. Clin. Endocrinol. Metab. 2013, 98, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Tai, N.; Hirano, J.; Ban, Y.; Inoue, D.; Okazaki, R. Independent association of bone mineral density and trabecular bone score to vertebral fracture in male subjects with chronic obstructive pulmonary disease. Osteoporos. Int. 2017, 29, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Aleksova, J.; Kurniawan, S.; Elder, G.J. The trabecular bone score is associated with bone mineral density, markers of bone turnover and prevalent fracture in patients with end stage kidney disease. Osteoporos. Int. 2018, 29, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.; Boutroy, S.; Zhang, C.; McMahon, D.J.; Zhou, B.; Wang, J.; Udesky, J.; Cremers, S.; Sarquis, M.; Guo, X.-D.E.; et al. Trabecular bone score (TBS)--a novel method to evaluate bone microarchitectural texture in patients with primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 2013, 98, 1963–1970. [Google Scholar] [CrossRef]
- Romagnoli, E.; Cipriani, C.; Nofroni, I.; Castro, C.; Angelozzi, M.; Scarpiello, A.; Pepe, J.; Diacinti, D.; Piemonte, S.; Carnevale, V.; et al. “Trabecular Bone Score” (TBS): An indirect measure of bone micro-architecture in postmenopausal patients with primary hyperparathyroidism. Bone 2013, 53, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Eller-Vainicher, C.; Filopanti, M.; Palmieri, S.; Ulivieri, F.M.; Morelli, V.; Zhukouskaya, V.V.; Cairoli, E.; Pino, R.; Naccarato, A.; Verga, U.; et al. Bone quality, as measured by trabecular bone score, in patients with primary hyperparathyroidism. Eur. J. Endocrinol. 2013, 169, 155–162. [Google Scholar] [CrossRef]
- Rolighed, L.; Rejnmark, L.; Sikjaer, T.; Heickendorff, L.; Vestergaard, P.; Mosekilde, L.; Christiansen, P. Vitamin D Treatment in Primary Hyperparathyroidism: A Randomized Placebo Controlled Trial. J. Clin. Endocrinol. Metab. 2014, 99, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.C.; Cusano, N.; Zhang, C.; Abraham, A.; Boutroy, S.; Fan, W.; Hans, D.; Bilezikian, J.P. Changes in Bone Micro-archi-tectural Texture Assessed by Trabecular Bone Score after Parathyroidectomy in Primary Hyperparathyroidism (Poster presentation). In Journal of Bone and Mineral Research; Wiley-Blackwell: Hoboken, NJ, USA, 2013. [Google Scholar]
- Maury, E.; Winzenrieth, R.; Souberbielle, J.-C.; Sarfati, E.; Cormier, C. BMD and TBS Micro Architecture Parameters As-sessment at Spine in Patients with Primary Hyperparathyroidism (PHPT) before and One Year after Parathyroidectomy (abstract). J. Bone Miner. Res. 2010, 25, S82–S135. [Google Scholar]
- Cipriani, C.; Abraham, A.; Silva, B.; Cusano, N.E.; Rubin, M.R.; McMahon, D.J.; Zhang, C.; Hans, D.; Silverberg, S.J.; Bilezikian, J.P. Skeletal changes after restoration of the euparathyroid state in patients with hypoparathyroidism and primary hyperparathyroidism. Endocrine 2017, 55, 591–598. [Google Scholar] [CrossRef]
- Tay, Y.-K.D.; E Cusano, N.; Rubin, M.R.; Williams, J.; Omeragic, B.; Bilezikian, J.P. Trabecular Bone Score in Obese and Nonobese Subjects with Primary Hyperparathyroidism before and after Parathyroidectomy. J. Clin. Endocrinol. Metab. 2018, 103, 1512–1521. [Google Scholar] [CrossRef] [PubMed]
- Miguel, G.A.; Carranza, F.H.; Rodríguez, J.C.R.; Ramos, M.A.; Pablos, D.L.; Herrero, E.F.; Díaz-Guerra, G.M. Trabecular Bone Score, Bone Mineral Density and Bone Markers in Patients with Primary Hyperparathyroidism 2 Years after Parathyroidectomy. Horm. Metab. Res. 2019, 51, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Cormier, C.; Lamy, O.; Poriau, S. TBS in Routine Clinial Practice: Proposals of Use. 2012. Available online: https://www.roentgen-baden.at/home/wp-content/uploads/TBS%20in%20der%20klinischen%20Routine.pdf (accessed on 10 August 2017).
- Muñoz-Torres, M.; Córdova, R.M.; García-Martín, A.; Avilés-Pérez, M.D.; Serrano, R.N.; Andújar-Vera, F.; García-Fontana, B. Usefulness of Trabecular Bone Score (TBS) to Identify Bone Fragility in Patients with Primary Hyperparathyroidism. J. Clin. Densitom. 2019, 22, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Grigorie, D.; Ivan, M.; Teodorescu, A.; Ilinca, L.; Brezeanu, L.; Sucaliuc, A. Trabecular Bone Score measurements in 123 Ro-manian patients with primary hyperparathyroidism (abstract). Osteoporos. Int. 2017, 28, 127–636. [Google Scholar]
- Hiller, R.G.G.; Patecki, M.; Neunaber, C.; Reifenrath, J.; Kielstein, J.T.; Kielstein, H. A comparative study of bone biopsies from the iliac crest, the tibial bone, and the lumbar spine. BMC Nephrol. 2017, 18, 134. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Amling, M.; Herden, S.; Pösl, M.; Hahn, M.; Ritzel, H.; Delling, G. Heterogeneity of the skeleton: Comparison of the trabecular microarchitecture of the spine, the iliac crest, the femur, and the calcaneus. J. Bone Miner. Res. 2009, 11, 36–45. [Google Scholar] [CrossRef]
- Vestergaard, P.; Mosekilde, L. Parathyroid surgery is associated with a decreased risk of hip and upper arm fractures in primary hyperparathyroidism: A controlled cohort study. J. Intern. Med. 2004, 255, 108–114. [Google Scholar] [CrossRef]
- Silverberg, S.J.; Shane, E.; Jacobs, T.P.; Siris, E.; Bilezikian, J.P. A 10-Year Prospective Study of Primary Hyperparathyroidism with or without Parathyroid Surgery. N. Engl. J. Med. 1999, 341, 1249–1255. [Google Scholar] [CrossRef]
- Bollerslev, J.; Jansson, S.; Mollerup, C.L.; Nordenström, J.; Lundgren, E.; Tørring, O.; Varhaug, J.-E.; Baranowski, M.; Aanderud, S.; Franco, C.; et al. Medical Observation, Compared with Parathyroidectomy, for Asymptomatic Primary Hyperparathyroidism: A Prospective, Randomized Trial. J. Clin. Endocrinol. Metab. 2007, 92, 1687–1692. [Google Scholar] [CrossRef]
| Parameter | Whole Cohort (n = 68) | Underwent Parathyroidectomy (n = 52) | No Parathyroidectomy (n = 16) |
|---|---|---|---|
| Age (years) | 65.3 ± 17.9 | 61.8 ± 17.6 | 76.6 ± 14.3 |
| Female | 54 (79.4) | 41 (78.8) | 12 (75.0) |
| Caucasian ethnicity | 54 (79.4) | 39 (75) | 14 (87.5) |
| BMI (kg/m2) | 29.0 ± 7.87 | 29.1 ± 8.7 | 28.9 ± 4.7 |
| Antiresorptive therapy | 10 (14.7) | 6 (11.5) | 4 (25) |
| Fracture number at diagnosis ∧ | |||
| 0 | 36 (52.9) | 30 (57.7) | 6 (37.5) |
| 1 | 15 (22.1) | 9 (17.3) | 6 (37.5) |
| >1 | 10 (14.7) | 7 (13.5) | 3 (18.8) |
| Fracture type | |||
| VF | 12 (17.6) | 8 (15.4) | 4 (25.0) |
| Hip fracture | 3 (4.4) | 1 (1.9) | 2 (12.5) |
| Upper limb | 9 (13.2) | 6 (11.5) | 3 (18.8) |
| cCa (mmol/L) | 2.83 ± 0.26 | 2.86 ± 0.28 | 2.73 ± 0.15 |
| PTH (pmol/L) | 26.2 ± 37.2 | 30.0 ± 41.7 | 13.8 ± 6.7 |
| 25(OH)Vit D (nmol/L) ∨ | 52.0 ± 18.8 | 52.1 ± 16.8 | 52.0 ± 24.8 |
| Deficient <50 nmol/L | 31 (46.3) | 23 (44.2) | 8 (50.0) |
| Severely deficient, <30 nmol/L | 9 (13.4) | 6 (11.5) | 3 (18.8) |
| Cr (umol/L, mean) ≈ | 79.4 ± 34.0 | 80.3 ± 35.4 | 76.5 ± 23.5 |
| eGFR (mL/min/1.73 m2, mean) ≈ | 70.5 ± 19.4 | 70.5 ± 20.1 | 70.7 ± 17.3 |
| LS BMD | 0.890 ± 0.184 | 0.872 ± 0.179 | 0.948 ± 0.193 |
| LS T-Score | −1.51 ± 1.63 | −1.66 ± 1.58 | −1.00 ± 1.71 |
| FN BMD | 0.630 ± 0.126 | 0.634 ± 0.127 | 0.615 ± 0.128 |
| FN T-Score | −2.07 ± 0.99 | −2.04 ± 0.97 | −2.18 ± 1.06 |
| TH BMD | 0.794 ± 0.163 | 0.801 ± 0.166 | 0.771 ± 0.157 |
| TH T-Score | −1.32 ± 1.17 | −1.25 ± 1.18 | −1.54 ± 1.14 |
| TBS | 1.19 ± 0.12 | 1.19 ± 0.12 | 1.18 ± 0.12 |
| LS BMD | FN BMD ∧ | TH BMD | Any BMD | |
|---|---|---|---|---|
| Osteoporosis | 14 (20.6) | 25 (37.3) | 9 (13.2) | 29 (42.6) |
| Osteopenia | 30 (44.1) | 31 (46.3) | 33 (48.5) | 31 (45.6) |
| Normal | 24 (35.3) | 11 (16.4) | 26 (38.3) | 8 (11.8) |
| Classification | TBS |
|---|---|
| Degraded | 39 (57.4) |
| Partially degraded | 24 (35.3) |
| Normal | 5 (7.3) |
| Parameter | Pre-Parathyroidectomy | Post-Parathyroidectomy |
|---|---|---|
| LS BMD | 0.839 (0.631, 0.888) | 0.862 (0.713, 0.937) |
| LS T-Score | −2.3 (−4.2, −1.4) | −1.8 (−3.2, −1.0) |
| FN BMD | 0.592 (0.505, 0.700) | 0.624 (0.534, 0.739) |
| FN T-Score | −2.3 (−3.1, −1.4) | −2.0 (−3.1, −1.2) |
| TH BMD | 0.831 (0.578, 0.966) | 0.847 (0.658, 0.970) |
| TH T-Score | −0.9 (−2.6, −0.4) | −0.8 (−2.3, −0.2) |
| TBS | 1.17 (1.05, 1.20) | 1.13 (0.95, 1.21) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, A.R.; Simons, K.; Harvey, S.; Grill, V. Bone Mineral Density Compared to Trabecular Bone Score in Primary Hyperparathyroidism. J. Clin. Med. 2022, 11, 330. https://doi.org/10.3390/jcm11020330
Jones AR, Simons K, Harvey S, Grill V. Bone Mineral Density Compared to Trabecular Bone Score in Primary Hyperparathyroidism. Journal of Clinical Medicine. 2022; 11(2):330. https://doi.org/10.3390/jcm11020330
Chicago/Turabian StyleJones, Alicia R., Koen Simons, Susan Harvey, and Vivian Grill. 2022. "Bone Mineral Density Compared to Trabecular Bone Score in Primary Hyperparathyroidism" Journal of Clinical Medicine 11, no. 2: 330. https://doi.org/10.3390/jcm11020330
APA StyleJones, A. R., Simons, K., Harvey, S., & Grill, V. (2022). Bone Mineral Density Compared to Trabecular Bone Score in Primary Hyperparathyroidism. Journal of Clinical Medicine, 11(2), 330. https://doi.org/10.3390/jcm11020330






