The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Protocol
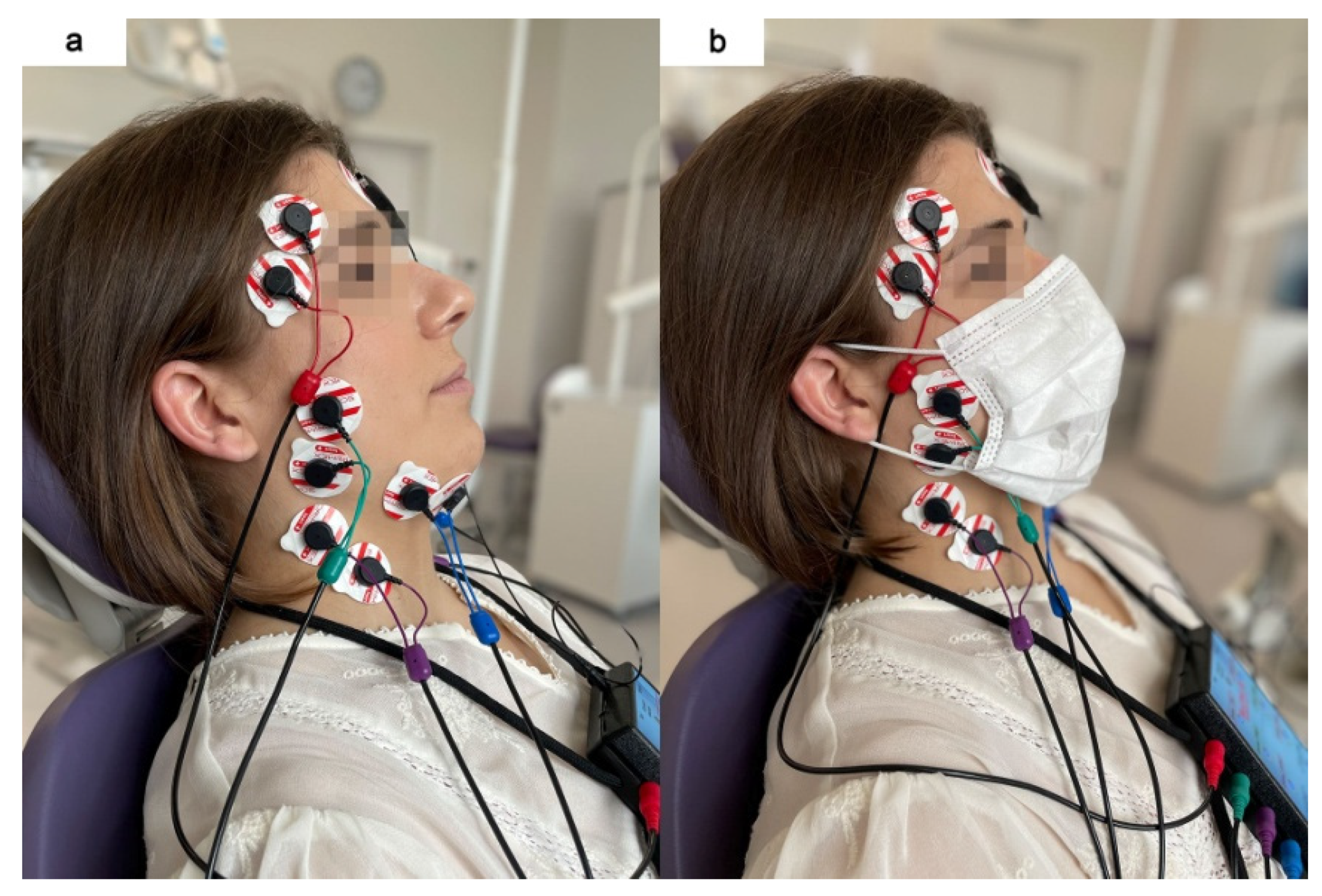
2.3. Electromyographic Examination
2.4. sEMG Signal Processing and Normalization
2.5. Statistical Analysis
3. Results
3.1. RMS sEMG Activity
3.2. Asymmetry and Activity Indices
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A Familial Cluster of Pneumonia Associated with the 2019 Novel Coronavirus Indicating Person-to-Person Transmission: A Study of a Family Cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- Rahmani, A.M.; Mirmahaleh, S.Y.H. Coronavirus Disease (COVID-19) Prevention and Treatment Methods and Effective Parameters: A Systematic Literature Review. Sustain. Cities Soc. 2021, 64, 102568. [Google Scholar] [CrossRef]
- Fowlkes, A.; Gaglani, M.; Groover, K.; Thiese, M.S.; Tyner, H.; Ellingson, K.; Cohorts, H.-R. Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers before and during B.1.617.2 (Delta) Variant Predominance—Eight U.S. Locations, December 2020–August 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1167–1169. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An Evidence Review of Face Masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Chan, J.F.-W.; Yuan, S.; Zhang, A.J.; Poon, V.K.-M.; Chan, C.C.-S.; Lee, A.C.-Y.; Fan, Z.; Li, C.; Liang, R.; Cao, J.; et al. Surgical Mask Partition Reduces the Risk of Noncontact Transmission in a Golden Syrian Hamster Model for Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 2139–2149. [Google Scholar] [CrossRef]
- Gandhi, M.; Beyrer, C.; Goosby, E. Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer. J. Gen. Intern. Med. 2020, 35, 3063–3066. [Google Scholar] [CrossRef] [PubMed]
- Coclite, D.; Napoletano, A.; Gianola, S.; Del Monaco, A.; D’Angelo, D.; Fauci, A.; Iacorossi, L.; Latina, R.; Torre, G.L.; Mastroianni, C.M.; et al. Face Mask Use in the Community for Reducing the Spread of COVID-19: A Systematic Review. Front. Med. 2020, 7, 594269. [Google Scholar] [CrossRef] [PubMed]
- Bartoszko, J.J.; Farooqi, M.A.M.; Alhazzani, W.; Loeb, M. Medical Masks vs N95 Respirators for Preventing COVID-19 in Healthcare Workers: A Systematic Review and Meta-Analysis of Randomized Trials. Influenza Other Respir. Viruses 2020, 14, 365–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Royo-Bordonada, M.A.; García-López, F.J.; Cortés, F.; Zaragoza, G.A. Face Masks in the General Healthy Population. Scientific and Ethical Issues. Gac. Sanit. 2021, 35, 580–584. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health 2021, 18, 4344. [Google Scholar] [CrossRef] [PubMed]
- Pifarré, F.; Zabala, D.D.; Grazioli, G.; i Maura, I.D.Y. COVID-19 and Mask in Sports. Apunt. Sports Med. 2020, 55, 143–145. [Google Scholar] [CrossRef]
- Beder, A.; Büyükkoçak, U.; Sabuncuoğlu, H.; Keskil, Z.A.; Keskil, S. Preliminary Report on Surgical Mask Induced Deoxygenation during Major Surgery. Neurocir. Astur. Spain 2008, 19, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Rebmann, T.; Carrico, R.; Wang, J. Physiologic and Other Effects and Compliance with Long-Term Respirator Use among Medical Intensive Care Unit Nurses. Am. J. Infect. Control 2013, 41, 1218–1223. [Google Scholar] [CrossRef]
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological Impact of the N95 Filtering Facepiece Respirator on Healthcare Workers. Respir. Care 2010, 55, 569–577. [Google Scholar]
- Georgi, C.; Haase-Fielitz, A.; Meretz, D.; Gäsert, L.; Butter, C. The Impact of Commonly-Worn Face Masks on Physiological Parameters and on Discomfort During Standard Work-Related Physical Effort. Dtsch. Arzteblatt Int. 2020, 117, 674–675. [Google Scholar] [CrossRef]
- Li, Y.; Tokura, H.; Guo, Y.P.; Wong, A.S.W.; Wong, T.; Chung, J.; Newton, E. Effects of Wearing N95 and Surgical Facemasks on Heart Rate, Thermal Stress and Subjective Sensations. Int. Arch. Occup. Environ. Health 2005, 78, 501–509. [Google Scholar] [CrossRef]
- Rosner, E. Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. J. Infect. Epidemiol. 2020. [Google Scholar] [CrossRef]
- Ong, J.J.Y.; Bharatendu, C.; Goh, Y.; Tang, J.Z.Y.; Sooi, K.W.X.; Tan, Y.L.; Tan, B.Y.Q.; Teoh, H.-L.; Ong, S.T.; Allen, D.M.; et al. Headaches Associated With Personal Protective Equipment—A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache 2020, 60, 864–877. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, J.L.; Ohde, S.; Takahashi, O.; Tokuda, Y.; Omata, F.; Fukui, T. Use of Surgical Face Masks to Reduce the Incidence of the Common Cold among Health Care Workers in Japan: A Randomized Controlled Trial. Am. J. Infect. Control. 2009, 37, 417–419. [Google Scholar] [CrossRef]
- Ramirez-Moreno, J.M.; Ceberino, D.; Gonzalez Plata, A.; Rebollo, B.; Macias Sedas, P.; Hariramani, R.; Roa, A.M.; Constantino, A.B. Mask-Associated “de Novo” Headache in Healthcare Workers during the COVID-19 Pandemic. Occup. Environ. Med. 2021, 78, 548–554. [Google Scholar] [CrossRef]
- Bharatendu, C.; Ong, J.J.Y.; Goh, Y.; Tan, B.Y.Q.; Chan, A.C.Y.; Tang, J.Z.Y.; Leow, A.S.; Chin, A.; Sooi, K.W.X.; Tan, Y.L.; et al. Powered Air Purifying Respirator (PAPR) Restores the N95 Face Mask Induced Cerebral Hemodynamic Alterations among Healthcare Workers during COVID-19 Outbreak. J. Neurol. Sci. 2020, 417, 117078. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of Recommendations for SEMG Sensors and Sensor Placement Procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Naeije, M.; McCarroll, R.S.; Weijs, W.A. Electromyographic Activity of the Human Masticatory Muscles during Submaximal Clenching in the Inter-Cuspal Position. J. Oral Rehabil. 1989, 16, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Miani, A.; D’Addona, A.; Barbini, E. Electromyographic Activity of Human Masticatory Muscles in Normal Young People. Statistical Evaluation of Reference Values for Clinical Applications. J. Oral Rehabil. 1993, 20, 271–280. [Google Scholar] [CrossRef]
- Ginszt, M.; Zieliński, G. Novel Functional Indices of Masticatory Muscle Activity. J. Clin. Med. 2021, 10, 1440. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect Size Estimates: Current Use, Calculations, and Interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Tian, L.; Li, X.; Qi, F.; Tang, Q.-Y.; Tang, V.; Liu, J.; Li, Z.; Cheng, X.; Li, X.; Shi, Y.; et al. Calibrated Intervention and Containment of the COVID-19 Pandemic. arXiv 2020, arXiv:2003.07353. [Google Scholar]
- Pietropaoli, D.; Ortu, E.; Giannoni, M.; Cattaneo, R.; Mummolo, A.; Monaco, A. Alterations in Surface Electromyography Are Associated with Subjective Masticatory Muscle Pain. Pain Res. Manag. 2019, 2019, 6256179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manfredini, D.; Cocilovo, F.; Favero, L.; Ferronato, G.; Tonello, S.; Guarda-Nardini, L. Surface Electromyography of Jaw Muscles and Kinesiographic Recordings: Diagnostic Accuracy for Myofascial Pain. J. Oral Rehabil. 2011, 38, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, G.; Byś, A.; Szkutnik, J.; Majcher, P.; Ginszt, M. Electromyographic Patterns of Masticatory Muscles in Relation to Active Myofascial Trigger Points of the Upper Trapezius and Temporomandibular Disorders. Diagnostics 2021, 11, 580. [Google Scholar] [CrossRef] [PubMed]
- Mapelli, A.; Zanandréa Machado, B.C.; Giglio, L.D.; Sforza, C.; De Felício, C.M. Reorganization of Muscle Activity in Patients with Chronic Temporomandibular Disorders. Arch. Oral Biol. 2016, 72, 164–171. [Google Scholar] [CrossRef] [PubMed]

| Masticatory Activity | RMS sEMG Activity | No Mask Measurement n = 66 | Medical Mask Measurement n = 66 | Test | Test Result | p | ||
|---|---|---|---|---|---|---|---|---|
| M (µV) | SD (µV) | M (µV) | SD (µV) | |||||
| Resting activity | TAR | 2.45 | 1.71 | 2.04 | 1.28 | Z | 1.84 | 0.07 |
| TAL | 2.71 | 1.65 | 2.29 | 1.48 | Z | 1.73 | 0.08 | |
| TAMean | 2.58 | 1.48 | 2.16 | 1.20 | Z | 2.00 | 0.05 * ES = 0.2 | |
| MMR | 2.14 | 1.16 | 1.87 | 1.12 | Z | 1.77 | 0.08 | |
| MML | 2.17 | 1.06 | 1.75 | 0.96 | Z | 2.75 | 0.01 * ES = 0.3 | |
| MMMean | 2.15 | 1,.03 | 1.81 | 0.96 | Z | 2.35 | 0.02 * ES = 0.2 | |
| DAR | 1.87 | 0.83 | 1.89 | 1.07 | Z | 0.67 | 0.50 | |
| DAL | 1.75 | 0.76 | 1.78 | 0.98 | Z | 0.30 | 0.77 | |
| DAMean | 1.81 | 0.77 | 1.83 | 0.99 | Z | 0.53 | 0.59 | |
| SCMR | 1.23 | 0.42 | 1.13 | 0.31 | Z | 1.36 | 0.17 | |
| SCML | 1.34 | 0.46 | 1.24 | 0.41 | Z | 1.20 | 0.23 | |
| SCMMean | 1.28 | 0.39 | 1.18 | 0.30 | Z | 1.27 | 0.20 | |
| Maximum voluntary clenching in intercuspal position | TAR | 136.46 | 80.88 | 121.40 | 72.88 | Z | 1.12 | 0.26 |
| TAL | 134.46 | 67.33 | 121.91 | 68.21 | T | 1.06 | 0.29 | |
| TAMean | 135.46 | 70.05 | 121.66 | 68.37 | Z | 1.12 | 0.26 | |
| MMR | 143.25 | 86.80 | 120.77 | 83.17 | Z | 1.65 | 0.10 | |
| MML | 139.44 | 85.97 | 120.28 | 79.74 | Z | 1.29 | 0.20 | |
| MMMean | 141.35 | 83.30 | 120.53 | 78.99 | Z | 1.47 | 0.14 | |
| DAR | 22.13 | 14.76 | 19.38 | 13.49 | Z | 1.12 | 0.26 | |
| DAL | 23.50 | 19.94 | 18.99 | 15.29 | Z | 1.47 | 0.14 | |
| DAMean | 22.82 | 15.61 | 19.18 | 13.47 | Z | 1.52 | 0.13 | |
| SCMR | 10.58 | 7.57 | 8.60 | 6.04 | Z | 1.60 | 0.11 | |
| SCML | 10.18 | 8.14 | 8.52 | 6.39 | Z | 1.19 | 0.23 | |
| SCMMean | 10.38 | 7.51 | 8.56 | 5.77 | Z | 1.40 | 0.16 | |
| Maximum voluntary clenching with dental cotton rolls between teeth | TAR | 124.13 | 68.93 | 125.27 | 68.69 | Z | −0.28 | 0.78 |
| TAL | 122.34 | 60.90 | 123.45 | 64.05 | Z | −0.02 | 0.98 | |
| TAMean | 123.24 | 62.23 | 124.36 | 64.27 | Z | −0.08 | 0.93 | |
| MMR | 160.33 | 79.99 | 154.80 | 75.60 | Z | 0.35 | 0.73 | |
| MML | 159.39 | 82.41 | 151.83 | 76.70 | Z | 0.38 | 0.70 | |
| MMMean | 159.86 | 77.94 | 153.31 | 71.58 | Z | 0.44 | 0.66 | |
| DAR | 23.07 | 11.62 | 22.00 | 10.59 | Z | 0.52 | 0.61 | |
| DAL | 23.77 | 14.10 | 21.54 | 13.80 | Z | 1.37 | 0.17 | |
| DAMean | 23.42 | 11.80 | 21.77 | 11.23 | Z | 0.98 | 0.33 | |
| SCMR | 12.62 | 7.27 | 13.30 | 14.42 | Z | 0.92 | 0.36 | |
| SCML | 11.73 | 6.98 | 11.45 | 8.27 | Z | 0.73 | 0.46 | |
| SCMMean | 12.17 | 6.77 | 12.38 | 9.50 | Z | 0.71 | 0.48 | |
| Maximum active mouth opening | TAR | 7.00 | 3.70 | 9.49 | 19.02 | Z | −0.27 | 0.79 |
| TAL | 6.77 | 3.96 | 13.00 | 48.71 | Z | 0.03 | 0.98 | |
| TAMean | 6.89 | 3.42 | 11.25 | 25.97 | Z | −0.39 | 0.70 | |
| MMR | 9.07 | 8.57 | 10.71 | 11.52 | Z | −0.46 | 0.64 | |
| MML | 8.29 | 5.82 | 9.45 | 7.19 | Z | −0.29 | 0.77 | |
| MMMean | 8.68 | 6.93 | 10.08 | 8.93 | Z | −0.45 | 0.65 | |
| DAR | 74.54 | 36.91 | 80.72 | 39.30 | Z | −0.93 | 0.35 | |
| DAL | 75.98 | 38.99 | 83.95 | 40.66 | Z | −1.21 | 0.23 | |
| DAMean | 75.26 | 36.10 | 82.33 | 37.67 | Z | −1.04 | 0.30 | |
| SCMR | 8.90 | 6.53 | 10.67 | 10.92 | Z | −0.47 | 0.64 | |
| SCML | 8.72 | 7.29 | 10.36 | 10.80 | Z | −0.73 | 0.47 | |
| SCMMean | 8.81 | 6.63 | 10.52 | 10.44 | Z | −0.57 | 0.57 | |
| Masticatory Activity | Asymmetry Index | No Mask Measurement n = 66 | Medical Mask Measurement n = 66 | Z | p | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Resting activity | AsITA | −4.59 | 25.32 | −3.96 | 24.09 | 0.06 | 0.95 |
| AsIMM | −1.12 | 16.96 | 2.33 | 18.66 | −0.91 | 0.36 | |
| AsIDA | 2.50 | 10.06 | 2.00 | 11.42 | 0.42 | 0.68 | |
| AsISCM | −4.19 | 14.05 | −3.96 | 13.67 | −0.08 | 0.93 | |
| Maximum voluntary clenching in intercuspal position | AsITA | −0.43 | 19.97 | 0.19 | 19.47 | −0.25 | 0.80 |
| AsIMM | 2.92 | 17.51 | 1.51 | 19.13 | 0.47 | 0.64 | |
| AsIDA | 0.07 | 22.82 | 2.17 | 20.24 | −0.48 | 0.63 | |
| AsISCM | 3.08 | 18.49 | 0.93 | 20.33 | 0.50 | 0.62 | |
| Maximum voluntary clenching with dental cotton rolls between teeth | AsITA | −0.57 | 14.67 | 0.55 | 14.43 | −0.50 | 0.62 |
| AsIMM | 0.68 | 14.36 | 1.60 | 15.60 | −0.28 | 0.78 | |
| AsIDA | −0.69 | 18.04 | 2.85 | 17.45 | −1.31 | 0.19 | |
| AsISCM | 4.15 | 17.72 | 3.80 | 20.90 | 0.36 | 0.72 | |
| Maximum active mouth opening | AsITA | 2.06 | 18.39 | 2.73 | 25.14 | 0.17 | 0.86 |
| AsIMM | 0.64 | 19.31 | 2.23 | 16.54 | −0.33 | 0.74 | |
| AsIDA | −0.62 | 11.96 | −1.51 | 13.59 | 0.36 | 0.72 | |
| AsISCM | 1.93 | 16.59 | 0.98 | 17.79 | 0.52 | 0.61 | |
| Masticatory Activity | Activity Index | No Mask Measurement n = 66 | Medical Mask Measurement n = 66 | Test | Test Result | p | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Resting activity | AcIR | −4.05 | 30.86 | 2.79 | 28.50 | T | −0.24 | 0.81 |
| AcIL | −7.71 | 31.63 | 8.42 | 32.30 | T | 0.13 | 0.90 | |
| AcITotal | −6.94 | 29.36 | −6.34 | 29.31 | T | −0.12 | 0.91 | |
| Maximum voluntary clenching in intercuspal position | AcIR | 0.08 | 25.20 | −4.78 | 25.86 | Z | 1.19 | 0.23 |
| AcIL | −3.05 | 26.29 | −6.21 | 24.45 | Z | 0.91 | 0.36 | |
| AcITotal | −1.66 | 22.21 | −5.47 | 21.97 | Z | 1.04 | 0.30 | |
| Maximum voluntary clenching with dental cotton rolls between teeth | AcIR | 13.11 | 21.64 | 11.87 | 20.77 | T | 0.34 | 0.74 |
| AcIL | 12.05 | 18.18 | 10.88 | 18.30 | Z | 0.37 | 0.71 | |
| AcITotal | 12.72 | 16.99 | 11.57 | 16.63 | Z | 0.35 | 0.72 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ginszt, M.; Zieliński, G.; Szkutnik, J.; Wójcicki, M.; Baszczowski, M.; Litko-Rola, M.; Rózyło-Kalinowska, I.; Majcher, P. The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women. J. Clin. Med. 2022, 11, 303. https://doi.org/10.3390/jcm11020303
Ginszt M, Zieliński G, Szkutnik J, Wójcicki M, Baszczowski M, Litko-Rola M, Rózyło-Kalinowska I, Majcher P. The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women. Journal of Clinical Medicine. 2022; 11(2):303. https://doi.org/10.3390/jcm11020303
Chicago/Turabian StyleGinszt, Michał, Grzegorz Zieliński, Jacek Szkutnik, Marcin Wójcicki, Michał Baszczowski, Monika Litko-Rola, Ingrid Rózyło-Kalinowska, and Piotr Majcher. 2022. "The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women" Journal of Clinical Medicine 11, no. 2: 303. https://doi.org/10.3390/jcm11020303
APA StyleGinszt, M., Zieliński, G., Szkutnik, J., Wójcicki, M., Baszczowski, M., Litko-Rola, M., Rózyło-Kalinowska, I., & Majcher, P. (2022). The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women. Journal of Clinical Medicine, 11(2), 303. https://doi.org/10.3390/jcm11020303








