Modified Target Angle as a Predictor of Success in Strabismus Management after Orbital Fracture
Abstract
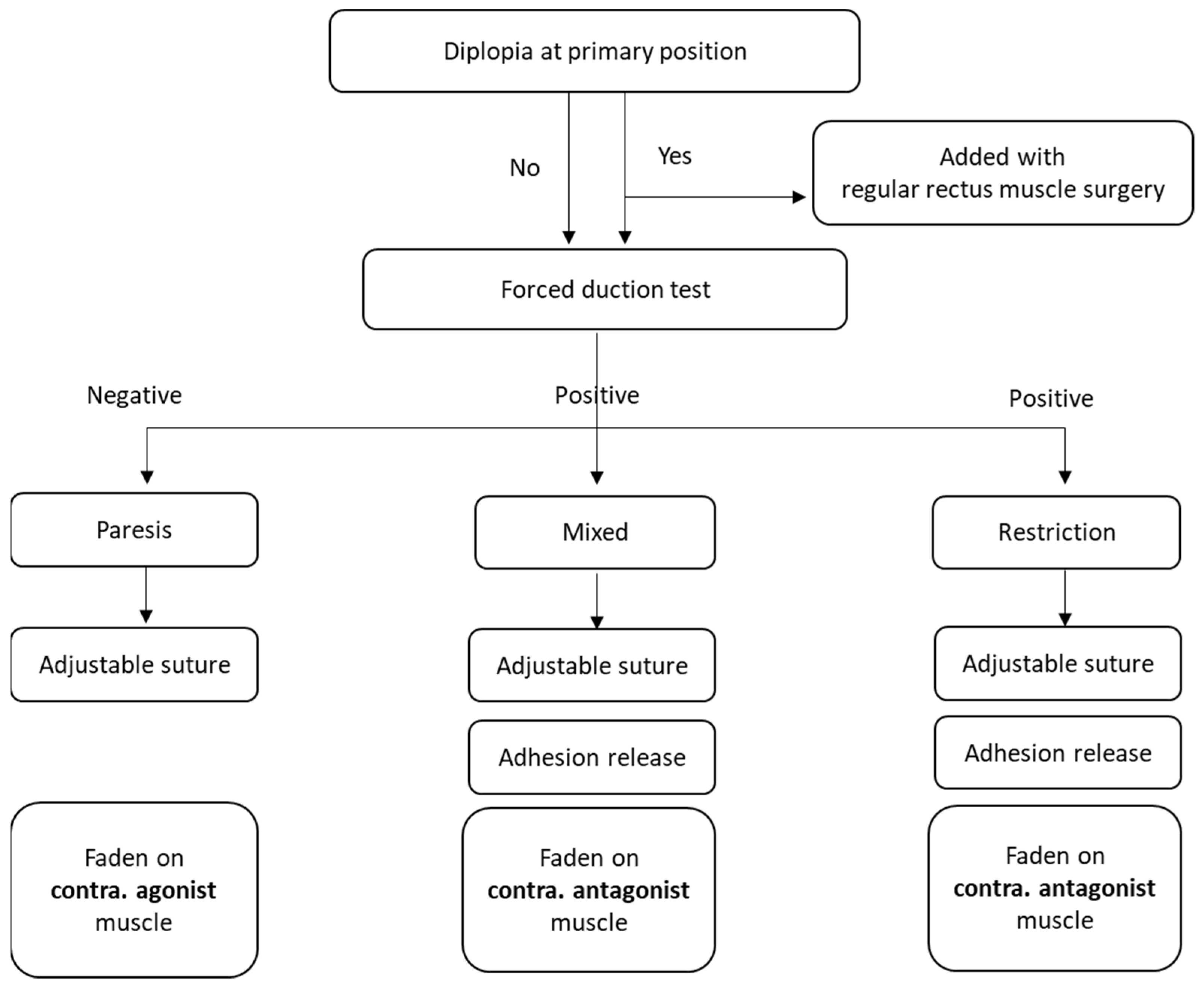
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harris, G.J. Avoiding complications in the repair of orbital floor fractures. JAMA Facial Plast. Surg. 2014, 16, 290–295. [Google Scholar] [CrossRef]
- Biesman, B.S.; Hornblass, A.; Lisman, R.; Kazlas, M. Diplopia after surgical repair of orbital floor fractures. Ophthal. Plast. Reconstr. Surg. 1996, 12, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Gosse, E.M.; Ferguson, A.W.; Lymburn, E.G.; Gilmour, C.; MacEwen, C.J. Blow-out fractures: Patterns of ocular motility and effect of surgical repair. Br. J. Oral Maxillofac. Surg. 2010, 48, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.K.; Hsieh, M.W.; Chang, H.C.; Tai, M.C.; Chien, K.H. Anatomic Factors Predicting Postoperative Strabismus in Orbital Wall Fracture Repair. Sci. Rep. 2019, 9, 14785. [Google Scholar] [CrossRef]
- Balaji, S. Residual diplopia in treated orbital bone fractures. Ann. Maxillofac. Surg. 2013, 3, 40. [Google Scholar] [CrossRef] [PubMed]
- Jazayeri, H.E.; Khavanin, N.; Yu, J.W.; Lopez, J.; Ganjawalla, K.P.; Shamliyan, T.; Tannyhill, R.J.; Dorafshar, A.H. Does Early Repair of Orbital Fractures Result in Superior Patient Outcomes? A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2020, 78, 568–577. [Google Scholar] [CrossRef]
- Lee, S.H.; Lew, H.; Yun, Y.S. Ocular motility disturbances in orbital wall fracture patients. Yonsei Med. J. 2005, 46, 359–367. [Google Scholar] [CrossRef]
- Loba, P.; Kozakiewicz, M.; Nowakowska, O.; Omulecki, W.; Broniarczyk-Loba, A. Management of persistent diplopia after surgical repair of orbital fractures. J. AAPOS 2012, 16, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Lipton, J.R.; Page, A.B.; Lee, J.P. Management of diplopia on down-gaze following orbital trauma. Eye 1990, 4, 535–537. [Google Scholar] [CrossRef]
- Kushner, B.J. Management of Diplopia Limited to Down Gaze. Arch. Ophthalmol. 1995, 113, 1426–1430. [Google Scholar] [CrossRef] [PubMed]
- VanEeckhoutte, L.; DeClippeleir, L.; Apers, R.; VanLammeren, M.; Janssens, H.; Baekeland, L. A protocol for extraocular muscle surgery after orbital floor fracture (“blow-out”). Binocul. Vis. Strabismus Q. 1998, 13, 29–36. [Google Scholar]
- Kugelberg, U.; Zetterstrom, C.; Sjukhus, H. Diplopia in down-gaze after a blow-out fracture. Acta Ophthalmol. Scand. 1998, 76, 629–631. [Google Scholar] [CrossRef]
- Kouri, A.S.; Bessant, D.A.R.; Adams, G.G.W.; Sloper, J.J.; Lee, J.P. Quantitative changes in the field of binocular single vision following a fadenoperation to a vertical rectus muscle. J. AAPOS 2002, 6, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Xia, Q.; Wang, Z.; Yan, J. Surgical management of strabismus in patients with orbital fracture. J. Craniofac. Surg. 2018, 29, 1865–1869. [Google Scholar] [CrossRef]
- Kerr, N.C. Management of Strabismus Following Orbital Fracture Repair. Am. Orthopt. J. 2004, 54, 24–31. [Google Scholar] [CrossRef]
- Kushner, B.J. Paresis and restriction of the inferior rectus muscle after orbital floor fracture. Am. J. Ophthalmol. 1982, 94, 81–86. [Google Scholar] [CrossRef]
- Scott, A.B. The faden operation: Mechanical effects. Am. Orthopt. J. 1977, 27, 44–47. [Google Scholar] [CrossRef]
- Mireskandari, K.; Schofield, J.; Cotesta, M.; Stephens, D.; Kraft, S.P. Achieving postoperative target range increases success of strabismus surgery in adults: A case for adjustable sutures? Br. J. Ophthalmol. 2015, 99, 1697–1701. [Google Scholar] [CrossRef] [PubMed]
- Astudillo, P.P.; Cotesta, M.; Schofield, J.; Kraft, S.; Mireskandari, K. The effect of achieving immediate target angle on success of strabismus surgery in children. Am. J. Ophthalmol. 2015, 160, 913–918. [Google Scholar] [CrossRef]
- Nishiike, S.; Nagai, M.; Nakagawa, A.; Konishi, M.; Kato, T.; Sakata, Y.; Yasukura, T.; Harada, T. Endoscopic transantral orbital floor repair with antral bone grafts. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.R.; Song, X.F.; Li, Z.K.; Shen, Q.; Fan, X.Q. Postoperative improvement of diplopia and extraocular muscle movement in patients with reconstructive surgeries for orbital floor fractures. J. Craniofac. Surg. 2016, 27, 2043–2049. [Google Scholar] [CrossRef] [PubMed]
- Nishida, Y.; Hayashi, O.; Miyake, T.; Kakinoki, M.; Yoshida, K.; Iwami, T.; Mekada, A.; Yakushigawa, H.; Suzuki, M. Quantitative evaluation of ocular motility in blow-out fractures for selection of nonsurgically managed cases. Am. J. Ophthalmol. 2004, 137, 777–779. [Google Scholar] [CrossRef]
- Scott, W.; Martin-Casals, A.J.; Jackson, O.B. Adjustable sutures in strabismus surgery. J. Pediatr. Ophthalmol. Strabismus 1977, 14, 71–75. [Google Scholar] [CrossRef]
- Zhang, M.S.; Hutchinson, A.K.; Drack, A.V.; Cleveland, J.; Lambert, S.R. Improved ocular alignment with adjustable sutures in adults undergoing strabismus surgery. Ophthalmology 2012, 119, 396–402. [Google Scholar] [CrossRef][Green Version]
- Liu, D.; Kumar, A.; Shieh, D.; Bhargava, S.; Zobal-Ratner, J.; Simon, J.W. One-Month Postoperative Horizontal Strabismus Surgery Outcomes Using Adjustable and Nonadjustable Sutures. J. Binocul. Vis. Ocul. Motil. 2020, 70, 94–97. [Google Scholar] [CrossRef]
- Bishop, F.; Doran, R.M.L. Adjustable and non-adjustable strabismus surgery: A retrospective case-matched study. Strabismus 2004, 12, 3–11. [Google Scholar] [CrossRef]
- Leffler, C.T.; Vaziri, K.; Cavuoto, K.M.; McKeown, C.A.; Schwartz, S.G.; Kishor, K.S.; Pariyadath, A. Strabismus Surgery Reoperation Rates With Adjustable and Conventional Sutures. Am. J. Ophthalmol. 2015, 160, 385–390.e4. [Google Scholar] [CrossRef] [PubMed]
- Awadein, A.; Sharma, M.; Bazemore, M.G.; Saeed, H.A.; Guyton, D.L. Adjustable suture strabismus surgery in infants and children. J. AAPOS 2008, 12, 585–590. [Google Scholar] [CrossRef]
- Pineles, S.L.; Ela-Dalman, N.; Zvansky, A.G.; Yu, F.; Rosenbaum, A.L. Long-term results of the surgical management of intermittent exotropia. J. AAPOS 2010, 14, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, X. Comparison between graded unilateral and bilateral medial rectus recession for esotropia. Br. J. Ophthalmol. 2012, 96, 540–543. [Google Scholar] [CrossRef]
- Tsai, C.B. Adjustable suture strabismus surgery in pediatric patients using pull-string technique. Taiwan J. Ophthalmol. 2017, 7, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.K.J.; Rosenbaum, A.L.; Hall, L. The results of adjustable suture technique in paediatric strabismus surgery. Eye 1999, 13, 567–570. [Google Scholar] [CrossRef]
- Kamal, A.M.; Abozeid, D.; Seif, Y.; Hassan, M. A comparative study of adjustable and non-adjustable sutures in primary horizontal muscle surgery in children. Eye 2016, 30, 1447–1451. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Furuta, M.; Yago, K.; Iida, T. Correlation between ocular motility and evaluation of computed tomography in orbital blowout fracture. Am. J. Ophthalmol. 2006, 142, 1019–1025.e2. [Google Scholar] [CrossRef] [PubMed]
- Leow, P.L.; Ko, S.T.C.; Wu, P.K.W.; Chan, C.W.N. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J. Pediatr. Ophthalmol. Strabismus 2010, 47, 12–16. [Google Scholar] [CrossRef]
- Lyon, D.B.; Newman, S.A. Evidence of direct damage to extraocular muscles as a cause of diplopia following orbital trauma. Ophthal. Plast. Reconstr. Surg. 1989, 5, 81–91. [Google Scholar] [CrossRef]
- Seiff, S.R.; Good, W.V. Hypertropia and the posterior blowout fracture: Mechanism and management. Ophthalmology 1996, 103, 152–156. [Google Scholar] [CrossRef]
- Jordan, D.R.; St. Onge, P.; Anderson, R.L.; Patrinely, J.R.; Nerad, J.A. Complications Associated with Alloplastic Implants used in Orbital Fracture Repair. Ophthalmology 1992, 99, 1600–1608. [Google Scholar] [CrossRef]
- Hoşal, B.M.; Beatty, R.L. Diplopia and enophthalmos after surgical repair of blowout fracture. Orbit 2002, 21, 27–33. [Google Scholar] [CrossRef]
- Loba, P.; Ordon, A.J. Management of simultaneous ocular elevation and depression deficit in patients after reconstruction surgery for orbital floor fracture. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 1443–1449. [Google Scholar] [CrossRef]
- Strube, Y.N.J.; Conte, F.; Faria, C.; Yiu, S.; Wright, K.W. Amniotic membrane transplantation for restrictive strabismus. Ophthalmology 2011, 118, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
| Whole Group | Group 1 | Group 2 | p | |
|---|---|---|---|---|
| Subjects (N) (%) | 63 (100%) | 49 (77.8%) | 14 (22.2%) | <0.01 * |
| Male (N) (%) | 47 (74.6%) | 38 (77.6%) | 9 (64.3%) | <0.01 * |
| Female (N) (%) | 16 (25.4%) | 11 (22.4%) | 5 (35.7%) | |
| Age (years) (mean) (SD) | 41.53 (13.62) | 40.74 (15.23) | 42.06 (17.45) | 1.32 |
| Follow-up period (months) (mean) (SD) | 15.14 (9.17) | 15.22 (9.17) | 14.75 (8.63) | 1.14 |
| Type of orbital fracture (N) (%) | ||||
| Orbital floor | 53 (84.1%) | 39 (79.6%) | 14 (100%) | <0.01 * |
| Orbital medial wall | 38 (60.3%) | 28 (57.1%) | 10 (71.4%) | <0.01 * |
| Orbital rim involvement | 12 (19.0%) | 3 (6.1%) | 9 (64.3%) | <0.01 * |
| Materials used in orbital reconstruction (N) (%) | ||||
| Porous polyethylene sheets | 11 (17.5%) | 10 (20.4%) | 1 (7.1%) | <0.01 * |
| Titanium mesh | 9 (14.3%) | 5 (10.2%) | 4 (28.6%) | <0.01 * |
| pre-bent titanium mesh | 41 (65.1%) | 32 (65.3%) | 9 (64.3%) | 1.38 |
| Bone graft | 2 (3.2%) | 2 (4.1%) | 0 (0%) | 0.06 |
| Time from trauma to orbital reconstruction (day) (mean) (SD) | 17.77 (5.45) | 17.36 (5.12) | 19.01 (6.44) | 1.02 |
| Whole Group | Group 1 | Group 2 | p | |
|---|---|---|---|---|
| Major strabismus type (N) (%) (Component ≥ 5 PD at primary position) | ||||
| Orthophoria | 24 (38.1%) | 17 (34.7%) | 7 (50%) | 0.06 |
| Vertical misalignment | 16 (25.4%) | 15 (30.6%) | 1 (7.1%) | 0.03 * |
| Horizontal misalignment | 3 (4.8%) | 3 (6.1%) | 0 (0%) | 0.24 |
| Mixed component | 20 (31.7%) | 14 (28.6%) | 6 (42.9%) | 0.08 |
| Strabismus cause (N) (%) | ||||
| Paresis | 9 (14.3%) | 7 (14.3%) | 2 (14.3%) | 1.65 |
| Restriction | 15 (23.8%) | 12 (24.5%) | 3 (21.4%) | 1.32 |
| Mixed cause | 39 (61.9%) | 30 (61.2%) | 9 (64.3%) | 1.28 |
| Time from reconstruction to strabismus surgery (month) (mean) (SD) | 4.70 (1.60) | 4.72 (1.54) | 4.63 (1.79) | 1.41 |
| Whole Group | Group 1 | Group 2 | p | |
|---|---|---|---|---|
| Preoperative HAR% (mean) (SD) | 47.17 (27.19) | 47.36 (26.68) | 43.77 (27.12) | 0.13 |
| Postoperative HAR% at first week (mean) (SD) | 73.03 (15.59) | 74.11 (14.76) | 65.31 (17.21) | <0.01 * |
| Adjustment done after strabismus surgery (N) (%) | 56 (88.9%) | 43 (87.8%) | 13 (92.9%) | 0.11 |
| HAR% > 65% at first week (N) (%) | 53 (84.1%) | 41 (83.7%) | 9 (64.3%) | <0.01 * |
| HAR% > 85% at 6-month visit (N) (%) | 52 (82.5%) | 39 (79.6%) | 7 (50%) | <0.01 * |
| Success (N) (%) | 50 (79.4%) | 38 (77.6%) | 5 (35.7%) | <0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-K.; Hsieh, M.-W.; Chang, H.-C.; Chen, Y.-H.; Chien, K.-H. Modified Target Angle as a Predictor of Success in Strabismus Management after Orbital Fracture. J. Clin. Med. 2022, 11, 287. https://doi.org/10.3390/jcm11020287
Hsu C-K, Hsieh M-W, Chang H-C, Chen Y-H, Chien K-H. Modified Target Angle as a Predictor of Success in Strabismus Management after Orbital Fracture. Journal of Clinical Medicine. 2022; 11(2):287. https://doi.org/10.3390/jcm11020287
Chicago/Turabian StyleHsu, Chih-Kang, Meng-Wei Hsieh, Hsu-Chieh Chang, Yi-Hao Chen, and Ke-Hung Chien. 2022. "Modified Target Angle as a Predictor of Success in Strabismus Management after Orbital Fracture" Journal of Clinical Medicine 11, no. 2: 287. https://doi.org/10.3390/jcm11020287
APA StyleHsu, C.-K., Hsieh, M.-W., Chang, H.-C., Chen, Y.-H., & Chien, K.-H. (2022). Modified Target Angle as a Predictor of Success in Strabismus Management after Orbital Fracture. Journal of Clinical Medicine, 11(2), 287. https://doi.org/10.3390/jcm11020287






