Expression Profiles of AQP3 and AQP4 in Lung Adenocarcinoma Samples Generated via Bronchoscopic Biopsies
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Characteristics
2.2. Immunohistochemistry
2.3. Scoring System for Immunohistochemistry Results
2.4. Statistical Analysis
3. Results
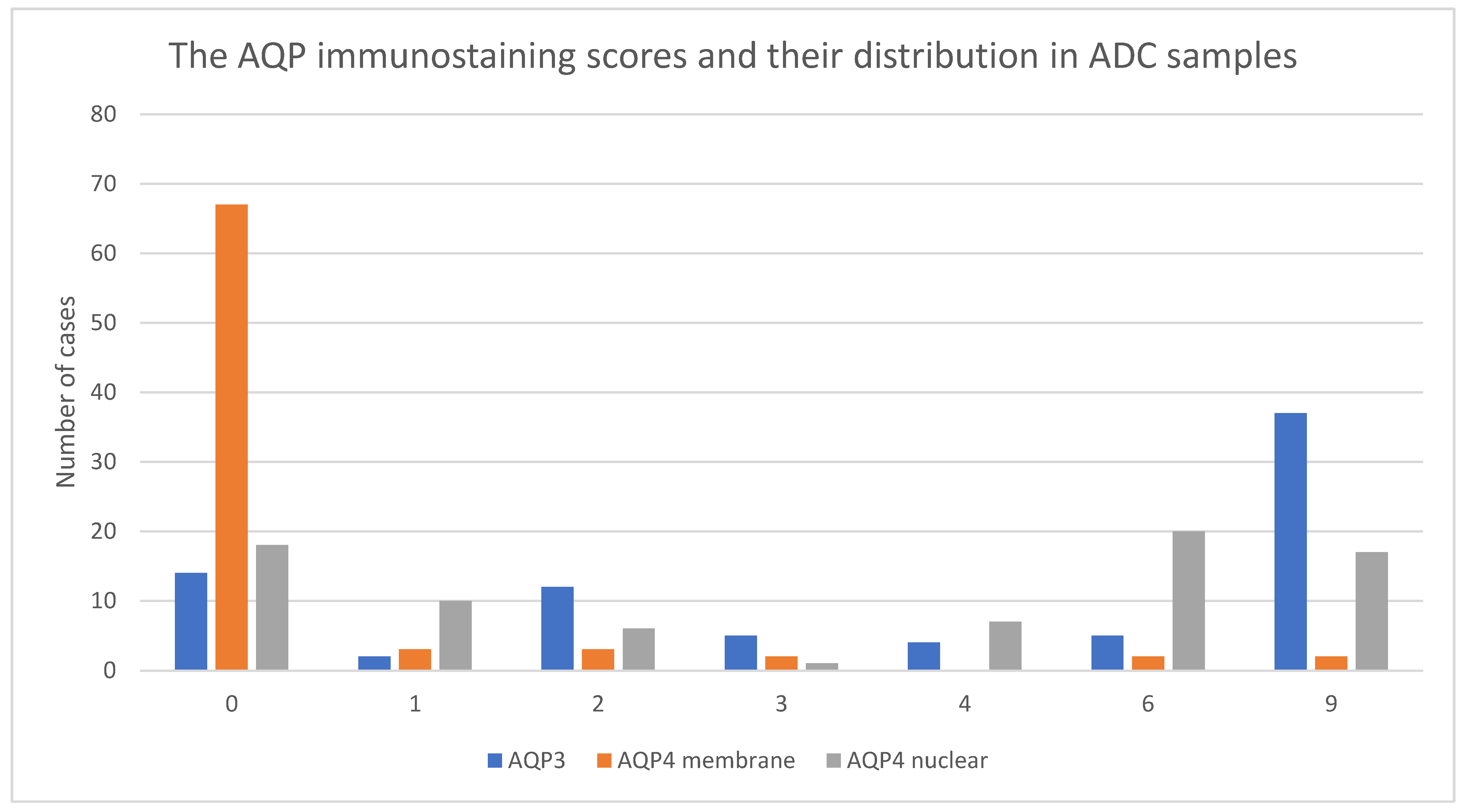
3.1. Immunohistochemistry Results for AQP3 and AQP4
3.2. Correlation among AQPs Expression, Outcome and Clinical Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agre, P.; Sasaki, S.; Chrispeels, M.J. Aquaporins: A family of water channel proteins. Am. J. Physiol. Physiol. 1993, 265, F461. [Google Scholar] [CrossRef]
- Gomes, D.; Agasse, A.; Thiébaud, P.; Delrot, S.; Gerós, H.; Chaumont, F. Aquaporins are multifunctional water and solute transporters highly divergent in living organisms. Biochim. Biophys. Acta BBA Biomembr. 2009, 1788, 1213–1228. [Google Scholar] [CrossRef] [PubMed]
- Agre, P.; King, L.S.; Yasui, M.; Guggino, W.B.; Ottersen, O.P.; Fujiyoshi, Y.; Engel, A.; Nielsen, S. Aquaporin water channels—From atomic structure to clinical medicine. J. Physiol. 2002, 542, 3–16. [Google Scholar] [CrossRef] [PubMed]
- King, L.S.; Agre, P. Pathophysiology of the Aquaporin Water Channels. Annu. Rev. Physiol. 1996, 58, 619–648. [Google Scholar] [CrossRef] [PubMed]
- King, L.S.; Yasui, M. Aquaporins and disease: Lessons from mice to humans. Trends Endocrinol. Metab. 2002, 13, 355–360. [Google Scholar] [CrossRef]
- Kreda, S.M.; Gynn, M.C.; Fenstermacher, D.A.; Boucher, R.C.; Gabriel, S.E. Expression and Localization of Epithelial Aquaporins in the Adult Human Lung. Am. J. Respir. Cell Mol. Biol. 2001, 24, 224–234. [Google Scholar] [CrossRef] [PubMed]
- King, L.S.; Nielsen, S.; Agre, P.; Brown, R.H. Decreased pulmonary vascular permeability in aquaporin-1-null humans. Proc. Natl. Acad. Sci. USA 2002, 99, 1059–1063. [Google Scholar] [CrossRef]
- Verkman, A. Role of aquaporins in lung liquid physiology. Respir. Physiol. Neurobiol. 2007, 159, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Vogelstein, B.; Kinzler, K.W. Cancer genes and the pathways they control. Nat. Med. 2004, 10, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Verkman, A.S.; Hara-Chikuma, M.; Papadopoulos, M.C. Aquaporins—New players in cancer biology. J. Mol. Med. 2008, 86, 523–529. [Google Scholar] [CrossRef]
- Ribatti, D.; Ranieri, G.; Annese, T.; Nico, B. Aquaporins in cancer. Biochim. Biophys. Acta BBA Gen. Subj. 2014, 1840, 1550–1553. [Google Scholar] [CrossRef]
- Papadopoulos, M.C.; Saadoun, S. Key roles of aquaporins in tumor biology. Biochim. Biophysica. Acta BBA Biomembr. 2015, 1848, 2576–2583. [Google Scholar] [CrossRef] [PubMed]
- Dajani, S.; Saripalli, A.; Sharma-Walia, N. Water transport proteins-aquaporins (AQPs) in cancer biology. Oncotarget 2018, 9, 36392–36405. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- SEER Cancer Stat Facts: Cancer of Any Site; National Cancer Institute: Bethesda, MD, USA. Available online: https://seer.cancer.gov/statfacts/html/all.html (accessed on 22 February 2022).
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef]
- Sher, T.; Dy, G.K.; Adjei, A.A. Small Cell Lung Cancer. Mayo Clin. Proc. 2008, 83, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Zappa, C.; Mousa, S.A. Non-small cell lung cancer: Current treatment and future advances. Transl. Lung Cancer Res. 2016, 5, 288–300. [Google Scholar] [CrossRef]
- Janssen-Heijnen, M. The changing epidemiology of lung cancer in Europe. Lung Cancer 2003, 41, 245–258. [Google Scholar] [CrossRef]
- Perez-Moreno, P.; Brambilla, E.; Thomas, R.; Soria, J.-C. Squamous Cell Carcinoma of the Lung: Molecular Subtypes and Therapeutic Opportunities. Clin. Cancer Res. 2012, 18, 2443–2451. [Google Scholar] [CrossRef] [PubMed]
- Khuder, S.A. Effect of cigarette smoking on major histological types of lung cancer: A meta-analysis. Lung Cancer 2001, 31, 139–148. [Google Scholar] [CrossRef]
- Cardarella, S.; Johnson, B.E. The Impact of Genomic Changes on Treatment of Lung Cancer. Am. J. Respir. Crit. Care Med. 2013, 188, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Rekhtman, N.; Tafe, L.J.; Chaft, J.; Wang, L.; Arcila, M.E.; Colanta, A.; Moreira, A.L.; Zakowski, M.F.; Travis, W.D.; Sima, C.S.; et al. Distinct profile of driver mutations and clinical features in immunomarker-defined subsets of pulmonary large-cell carcinoma. Mod. Pathol. 2013, 26, 511–522. [Google Scholar] [CrossRef]
- Zhang, Z.-Q.; Zhu, Z.-X.; Bai, C.-X.; Chen, Z.-H. Aquaporin 5 expression increases mucin production in lung adenocarcinoma. Oncol. Rep. 2011, 25, 1645–1650. [Google Scholar] [CrossRef]
- Hoque, M.O.; Soria, J.-C.; Woo, J.; Lee, T.; Lee, J.; Jang, S.J.; Upadhyay, S.; Trink, B.; Monitto, C.; Desmaze, C.; et al. Aquaporin 1 Is Overexpressed in Lung Cancer and Stimulates NIH-3T3 Cell Proliferation and Anchorage-Independent Growth. Am. J. Pathol. 2006, 168, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Ben, Y.; Chen, J.; Zhu, R.; Gao, L.; Bai, C. Upregulation of AQP3 and AQP5 induced by dexamethasone and ambroxol in A549 cells. Respir. Physiol. Neurobiol. 2008, 161, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Dong, J. Aquaporin 1 promotes the proliferation and migration of lung cancer cell in vitro. Oncol. Rep. 2015, 34, 1440–1448. [Google Scholar] [CrossRef]
- Klein, M.; Picard, E.; Vignaud, J.M.; Marie, B.; Bresler, L.; Toussaint, B.; Weryha, G.; Duprez, A.; LeClere, J. Vascular endothelial growth factor gene and protein: Strong expression in thyroiditis and thyroid carcinoma. J. Endocrinol. 1999, 161, 41–49. [Google Scholar] [CrossRef]
- Klein, M.; Vignaud, J.-M.; Hennequin, V.; Toussaint, B.; Bresler, L.; Plénat, F.; Leclère, J.; Duprez, A.; Weryha, G. Increased Expression of the Vascular Endothelial Growth Factor Is a Pejorative Prognosis Marker in Papillary Thyroid Carcinoma. J. Clin. Endocrinol. Metab. 2001, 86, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Bucciarelli, E.; Sidoni, A.; Bellezza, G.; Cavaliere, A.; Brachelente, G.; Costa, G.; Chaplet, M.; Castronovo, V.; Bellahcène, A. Low dentin matrix protein 1 expression correlates with skeletal metastases development in breast cancer patients and enhances cell migratory capacity in vitro. Breast Cancer Res. Treat. 2007, 105, 95–104. [Google Scholar] [CrossRef]
- Bellezza, G.; Vannucci, J.; Bianconi, F.; Metro, G.; Del Sordo, R.; Andolfi, M.; Ferri, I.; Siccu, P.; Ludovini, V.; Puma, F.; et al. Prognostic implication of aquaporin 1 overexpression in resected lung adenocarcinoma. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Brambilla, E.; Noguchi, M.; Nicholson, A.G.; Geisinger, K.R.; Yatabe, Y.; Beer, D.G.; Powell, C.A.; Riely, G.J.; Van Schil, P.E.; et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society International Multidisciplinary Classification of Lung Adenocarcinoma. J. Thorac. Oncol. 2011, 6, 244–285. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, H.; Huang, B.W. Lung Cancer: Diagnosis, Treatment Principles, and Screening. Am. Fam. Physician 2022, 105, 487–494. [Google Scholar] [PubMed]
- Yung, R.C.W. Tissue diagnosis of suspected lung cancer: Selecting between bronchoscopy, transthoracic needle aspiration, and resectional biopsy. Respir. Care Clin. N. Am. 2003, 9, 51–76. [Google Scholar] [CrossRef]
- Morrissey, J.J.; Kharasch, E.D. The Specificity of Urinary Aquaporin 1 and Perilipin 2 to Screen for Renal Cell Carcinoma. J. Urol. 2013, 189, 1913–1920. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, J.J.; Mobley, J.; Song, J.; Vetter, J.; Luo, J.; Bhayani, S.; Figenshau, R.S.; Kharasch, E.D. Urinary Concentrations of Aquaporin-1 and Perilipin-2 in Patients with Renal Cell Carcinoma Correlate with Tumor Size and Stage but not Grade. Urology 2014, 83, 256.e9–256.e14. [Google Scholar] [CrossRef]
- Nakakoshi, M.; Morishita, Y.; Usui, K.; Ohtsuki, M.; Ishibashi, K. Identification of a keratinocarcinoma cell line expressing AQP3. Biol. Cell 2006, 98, 95–100. [Google Scholar] [CrossRef][Green Version]
- Shen, L.; Zhu, Z.; Huang, Y.; Shu, Y.; Sun, M.; Xu, H.; Zhang, G.; Guo, R.; Wei, W.; Wu, W. Expression profile of multiple aquaporins in human gastric carcinoma and its clinical significance. Biomed. Pharmacother. 2010, 64, 313–318. [Google Scholar] [CrossRef]
- Zhao, H.; Yang, X.; Zhou, Y.; Zhang, W.; Wang, Y.; Wen, J.; Zhang, Z.; Shen, L. Potential role of aquaporin 3 in gastric intestinal metaplasia. Oncotarget 2015, 6, 38926–38933. [Google Scholar] [CrossRef]
- Liu, Y.L.; Matsuzaki, T.; Nakazawa, T.; Murata, S.-I.; Nakamura, N.; Kondo, T.; Iwashina, M.; Mochizuki, K.; Yamane, T.; Takata, K.; et al. Expression of aquaporin 3 (AQP3) in normal and neoplastic lung tissues. Hum. Pathol. 2007, 38, 171–178. [Google Scholar] [CrossRef]
- Marlar, S.; Jensen, H.H.; Login, F.H.; Nejsum, L.N. Aquaporin-3 in Cancer. Int. J. Mol. Sci. 2017, 18, 2106. [Google Scholar] [CrossRef]
- Moosavi, M.-S.; Elham, Y. Aquaporins 1, 3 and 5 in Different Tumors, their Expression, Prognosis Value and Role as New Therapeutic Targets. Pathol. Oncol. Res. 2020, 26, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Bisi, S.; Disanza, A.; Malinverno, C.; Frittoli, E.; Palamidessi, A.; Scita, G. Membrane and actin dynamics interplay at lamellipodia leading edge. Curr. Opin. Cell Biol. 2013, 25, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Hara-Chikuma, M.; Verkman, A.S. Prevention of Skin Tumorigenesis and Impairment of Epidermal Cell Proliferation by Targeted Aquaporin-3 Gene Disruption. Mol. Cell. Biol. 2008, 28, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Hara-Chikuma, M.; Verkman, A.S. Aquaporin-3 facilitates epidermal cell migration and proliferation during wound healing. J. Mol. Med. 2008, 86, 221–231. [Google Scholar] [CrossRef]
- Kusayama, M.; Wada, K.; Nagata, M.; Ishimoto, S.; Takahashi, H.; Yoneda, M.; Nakajima, A.; Okura, M.; Kogo, M.; Kamisaki, Y. Critical role of aquaporin 3 on growth of human esophageal and oral squamous cell carcinoma. Cancer Sci. 2011, 102, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Chen, L.; Lin, L.; Lin, H.; Guo, Z.; Xu, Y.; Hu, C.; Fu, J.; Lin, Q.; Chen, W.; et al. Comprehensive Analysis of Aquaporin Superfamily in Lung Adenocarcinoma. Front. Mol. Biosci. 2021, 8, 873. [Google Scholar] [CrossRef]
- Warth, A.; Muley, T.; Meister, M.; Herpel, E.; Pathil, A.; Hoffmann, H.; Schnabel, P.A.; Bender, C.; Buness, A.; Schirmacher, P.; et al. Loss of aquaporin-4 expression and putative function in non-small cell lung cancer. BMC Cancer 2011, 11, 161. [Google Scholar] [CrossRef]
- Xu, H.; Zhang, Y.; Wei, W.; Shen, L.; Wu, W. Differential expression of aquaporin-4 in human gastric normal and cancer tissues. Gastroenterol. Clin. Biol. 2009, 33, 72–76. [Google Scholar] [CrossRef]
- Li, J.; Wang, L.; He, F.; Li, B.; Han, R. Long noncoding RNA LINC00629 restrains the progression of gastric cancer by upregulating AQP4 through competitively binding to miR-196b-5p. J. Cell. Physiol. 2020, 235, 2973–2985. [Google Scholar] [CrossRef]
- Wu, X.; Wu, G.; Zhang, H.; Peng, X.; Huang, B.; Huang, M.; Ding, J.; Mao, C.; Peng, C. MiR-196b Promotes the Invasion and Migration of Lung Adenocarcinoma Cells by Targeting AQP4. Technol. Cancer Res. Treat. 2021, 20, 1533033820985868. [Google Scholar] [CrossRef]



| Variables | n | (%) | |
|---|---|---|---|
| Total number of patients | 79 | ||
| Mean Age ± SD, years (range) | 61.8 ± 7.7 (47–81) | ||
| Gender | |||
| Female | 27 | (34.2) | |
| Male | 52 | (65.8) | |
| CS | |||
| I | 3 | (3.8) | |
| II | 6 | (7.6) | |
| III | 16 | (20.2) | |
| IV | 54 | (68.4) | |
| T | |||
| Tx | 2 | (2.5) | |
| T0 | 1 | (1.3) | |
| T1 | 12 | (15.2) | |
| T2 | 29 | (36.7) | |
| T3 | 4 | (5.1) | |
| T4 | 26 | (32.9) | |
| no data | 5 | (6.3) | |
| N | |||
| N0 | 10 | (12.7) | |
| N1 | 7 | (8.9) | |
| N2 | 38 | (48.1) | |
| N3 | 22 | (27.8) | |
| no data | 2 | (2.5) | |
| M | |||
| M0 | 26 | (32.9) | |
| M1 | 53 | (67.1) | |
| Intention to treat | |||
| radical | 19 | (24.0) | |
| palliative | 59 | (74.7) | |
| no consent | 1 | (1.3) | |
| Radical treatment | operation + adjuvant radiochemotherapy | 8 | (42.1) |
| radiochemotherapy | 7 | (36.8) | |
| operation | 4 | (21.1) | |
| Palliative treatment | palliative chemotherapy | 41 | (69.5) |
| palliative radiotherapy | 5 | (8.5) | |
| molecular targeted therapy | 4 | (6.8) | |
| symptomatic treatment | 3 | (5.1) | |
| no data | 6 | (10.1) |
| AQP3 Score | AQP4 Membrane Score | AQP4 Nuclear Score | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Low | High | p-Value | Low | High | p-Value | Low | High | p-Value | ||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Mean Age ±SD (years) | 64.6 ± 8.9 | 60.3 ± 6.5 | 0.017 | 61.6 ± 7.5 | 64.5 ± 9.9 | 0.38 | 62.6 ± 8.2 | 61.2 ± 7.3 | 0.44 | ||||||
| Gender | |||||||||||||||
| Female | 8 | (29) | 19 | (37) | 0.44 | 24 | (33) | 3 | (50) | 0.40 | 15 | (44) | 12 | (27) | 0.11 |
| Male | 20 | (71) | 32 | (63) | 49 | (67) | 3 | (50) | 19 | (56) | 33 | (73) | |||
| CS | |||||||||||||||
| I–II | 3 | (10) | 6 | (12) | 0.39 | 7 | (10) | 2 | (33) | 0.21 | 6 | (18) | 3 | (7) | 0.31 |
| III | 8 | (29) | 8 | (16) | 15 | (20) | 1 | (17) | 6 | (17) | 10 | (22) | |||
| IV | 17 | (61) | 37 | (72) | 51 | (70) | 3 | (50) | 22 | (65) | 32 | (71) | |||
| T | |||||||||||||||
| T1 | 8 | (32) | 4 | (9) | 0.06 | 10 | (15) | 2 | (50) | 0.20 | 6 | (21) | 6 | (14) | 0.70 |
| T2 | 7 | (28) | 22 | (48) | 27 | (40) | 2 | (50) | 13 | (45) | 16 | (38) | |||
| T3 | 2 | (8) | 2 | (4) | 4 | (6) | 0 | (0) | 1 | (3) | 3 | (7) | |||
| T4 | 8 | (32) | 18 | (39) | 26 | (39) | 0 | (0) | 9 | (31) | 17 | (41) | |||
| N | |||||||||||||||
| N0 | 2 | (7) | 8 | (16) | 0.74 | 8 | (11) | 2 | (33) | 0.046 | 7 | (21) | 3 | (7) | 0.07 |
| N1 | 3 | (11) | 4 | (8) | 5 | (7) | 2 | (33) | 5 | (15) | 2 | (5) | |||
| N2 | 14 | (52) | 24 | (48) | 37 | (52) | 1 | (17) | 14 | (43) | 24 | (54) | |||
| N3 | 8 | (30) | 14 | (28) | 21 | (30) | 1 | (17) | 7 | (21) | 15 | (34) | |||
| M | |||||||||||||||
| M0 | 11 | (39) | 15 | (29) | 0.37 | 22 | (30) | 4 | (67) | 0.07 | 13 | (38) | 13 | (29) | 0.38 |
| M1 | 17 | (61) | 36 | (71) | 51 | (70) | 2 | (33) | 21 | (62) | 32 | (71) | |||
| Intention to treat | |||||||||||||||
| radical | 8 | (30) | 11 | (22) | 0.43 | 16 | (22) | 3 | (50) | 0.13 | 9 | (27) | 10 | (23) | 0.70 |
| palliative | 19 | (70) | 40 | (78) | 56 | (78) | 3 | (50) | 25 | (73) | 34 | (77) | |||
| Univariate OS Analysis | Multivariate OS Analysis | |||||
|---|---|---|---|---|---|---|
| Variables | HR (95% CI) | p | HR (95% CI) | p | ||
| Age | 1.01 | (0.98–1.04) | 0.54 | |||
| Gender | ||||||
| Female | 1.00 | Reference | ||||
| Male | 1.44 | (0.90–2.30) | 0.13 | |||
| CS | ||||||
| I–II | 1.00 | Reference | 1.00 | Reference | ||
| III | 0.82 | (0.35–1.93) | 0.66 | 0.72 | (0.26–1.99) | 0.53 |
| IV | 2.37 | (1.15–4.86) | 0.02 | - | - | |
| T | ||||||
| T1 | 1.00 | Reference | 1.00 | Reference | ||
| T2 | 1.42 | (0.70–2.87) | 0.33 | 1.48 | (0.69–3.16) | 0.31 |
| T3 | 3.70 | (1.12–12.23) | 0.03 | 2.79 | (0.70–11.14) | 0.15 |
| T4 | 2.04 | (0.99–4.19) | 0.05 | 1.44 | (0.62–3.33) | 0.40 |
| N | ||||||
| N0 | 1.00 | Reference | ||||
| N1 | 1.00 | (0.38–2.64) | 1.00 | |||
| N2 | 1.01 | (0.50–2.04) | 0.99 | |||
| N3 | 1.70 | (0.80–3.63) | 0.17 | |||
| M | ||||||
| M0 | 1.00 | Reference | 1.00 | Reference | ||
| M1 | 2.54 | (1.54–4.19) | <0.001 | 1.48 | (0.42–5.23) | 0.54 |
| Intention to treat | ||||||
| radical | 1.00 | Reference | 1.00 | Reference | ||
| palliative | 2.34 | (1.37–4.01) | <0.001 | 1.27 | (0.51–3.13) | 0.61 |
| AQP 3 | ||||||
| low | 1.00 | Reference | ||||
| high | 1.26 | (0.78–2.01) | 0.34 | |||
| AQP 4 membrane | ||||||
| low | 1.00 | Reference | ||||
| high | 0.57 | (0.24–1.31) | 0.18 | |||
| AQP 4 nuclear | ||||||
| low | 1.00 | Reference | ||||
| high | 1.15 | (0.73–1.80) | 0.54 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaskiewicz, L.; Hejne, K.; Szostak, B.; Osowiecka, K.; Skowronski, M.T.; Lepiarczyk, E.; Doboszynska, A.; Majewska, M.; Kordowitzki, P.; Skowronska, A. Expression Profiles of AQP3 and AQP4 in Lung Adenocarcinoma Samples Generated via Bronchoscopic Biopsies. J. Clin. Med. 2022, 11, 5954. https://doi.org/10.3390/jcm11195954
Jaskiewicz L, Hejne K, Szostak B, Osowiecka K, Skowronski MT, Lepiarczyk E, Doboszynska A, Majewska M, Kordowitzki P, Skowronska A. Expression Profiles of AQP3 and AQP4 in Lung Adenocarcinoma Samples Generated via Bronchoscopic Biopsies. Journal of Clinical Medicine. 2022; 11(19):5954. https://doi.org/10.3390/jcm11195954
Chicago/Turabian StyleJaskiewicz, Lukasz, Karolina Hejne, Blazej Szostak, Karolina Osowiecka, Mariusz T. Skowronski, Ewa Lepiarczyk, Anna Doboszynska, Marta Majewska, Pawel Kordowitzki, and Agnieszka Skowronska. 2022. "Expression Profiles of AQP3 and AQP4 in Lung Adenocarcinoma Samples Generated via Bronchoscopic Biopsies" Journal of Clinical Medicine 11, no. 19: 5954. https://doi.org/10.3390/jcm11195954
APA StyleJaskiewicz, L., Hejne, K., Szostak, B., Osowiecka, K., Skowronski, M. T., Lepiarczyk, E., Doboszynska, A., Majewska, M., Kordowitzki, P., & Skowronska, A. (2022). Expression Profiles of AQP3 and AQP4 in Lung Adenocarcinoma Samples Generated via Bronchoscopic Biopsies. Journal of Clinical Medicine, 11(19), 5954. https://doi.org/10.3390/jcm11195954






