Effects of Toxic Lithium Levels on ECG—Findings from the LiSIE Retrospective Cohort Study
Abstract
1. Introduction
Aims and Hypothesis
2. Materials and Methods
2.1. Study Design and Setting
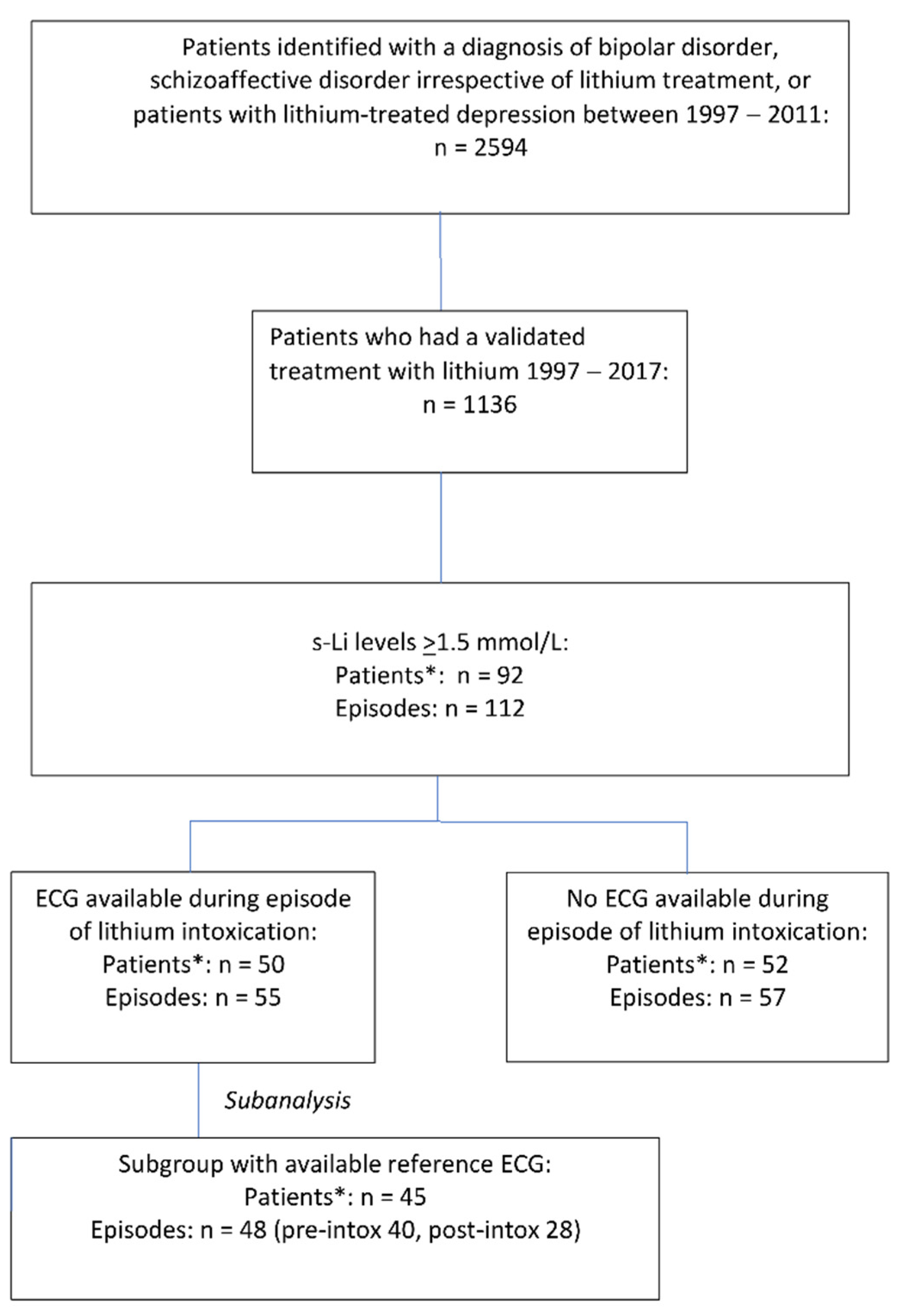
2.2. Participants
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Data Sources/Measurement
2.6. Outcome Variables
ECG Selection
2.7. Exposure Variables
2.7.1. Serum Lithium Concentrations
2.7.2. Concomitant Use of Medicines with Potential QT Prolonging Effect
- Known TdP risk: medicines known to prolong the QT interval with a known risk of TdP, even if taken as recommended.
- Possible TdP risk: medicines known to prolong the QT interval with a current lack of evidence for a risk of TdP if taken as recommended.
- Conditional TdP risk: medicines that may cause TdP if taken (a) in excessive dosage, (b) in conjunction with other medicines that may directly or indirectly contribute to QT prolongation, or (c) by patients with additional risk factors, such as congenital long QT interval, extreme bradycardia, or hypokalaemia.
2.7.3. Concomitant Use of Medicines with Other Cardiac Effects
2.7.4. Cardiovascular Comorbidities and Risk Factors
2.7.5. Potassium Concentrations
2.8. Bias
2.9. Missing Data
2.10. Statistical Methods
3. Results
3.1. Baseline Characteristics
3.2. ECG Changes at Lithium Intoxication
3.3. Heart Rate and Rhythm
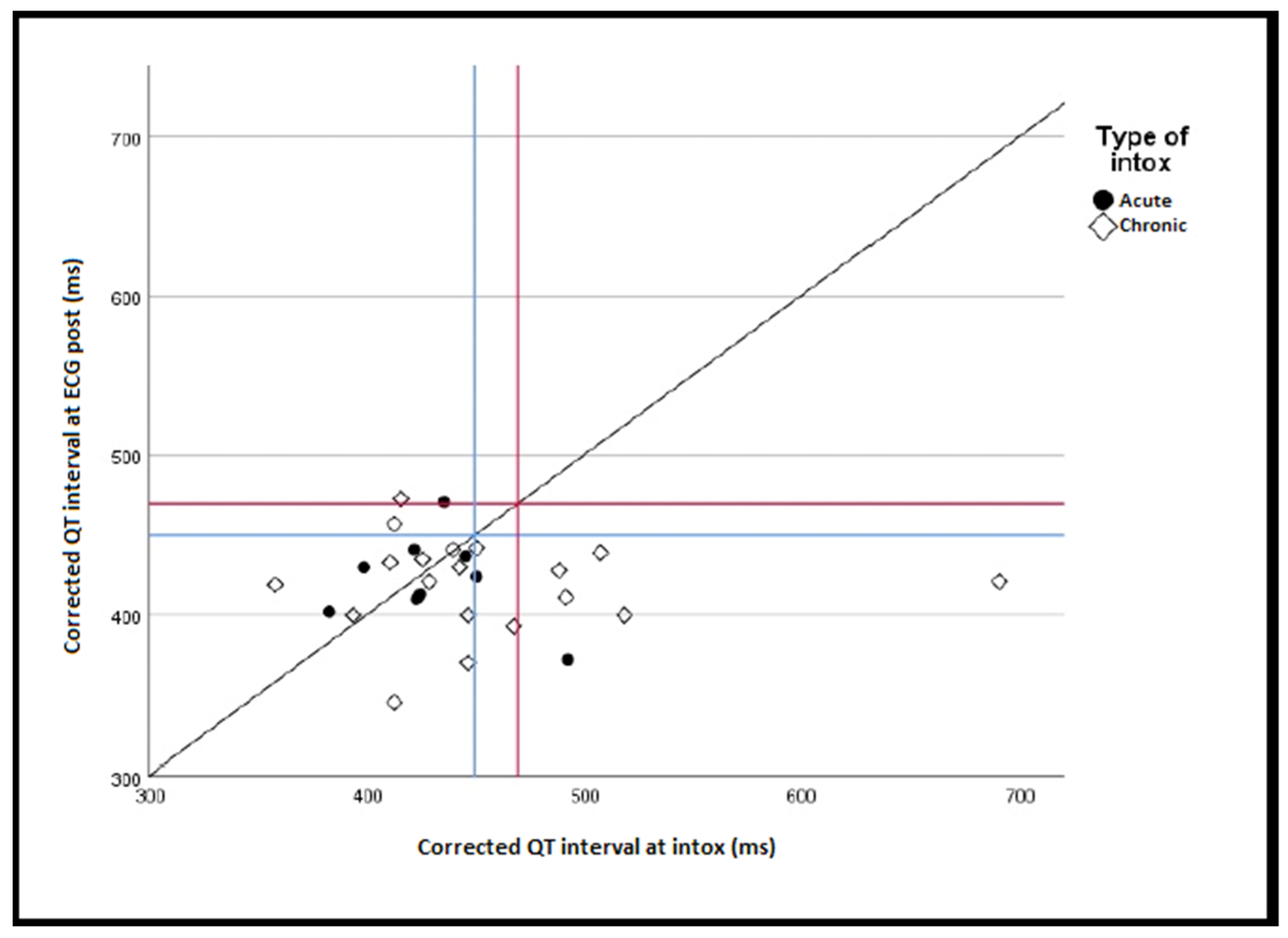
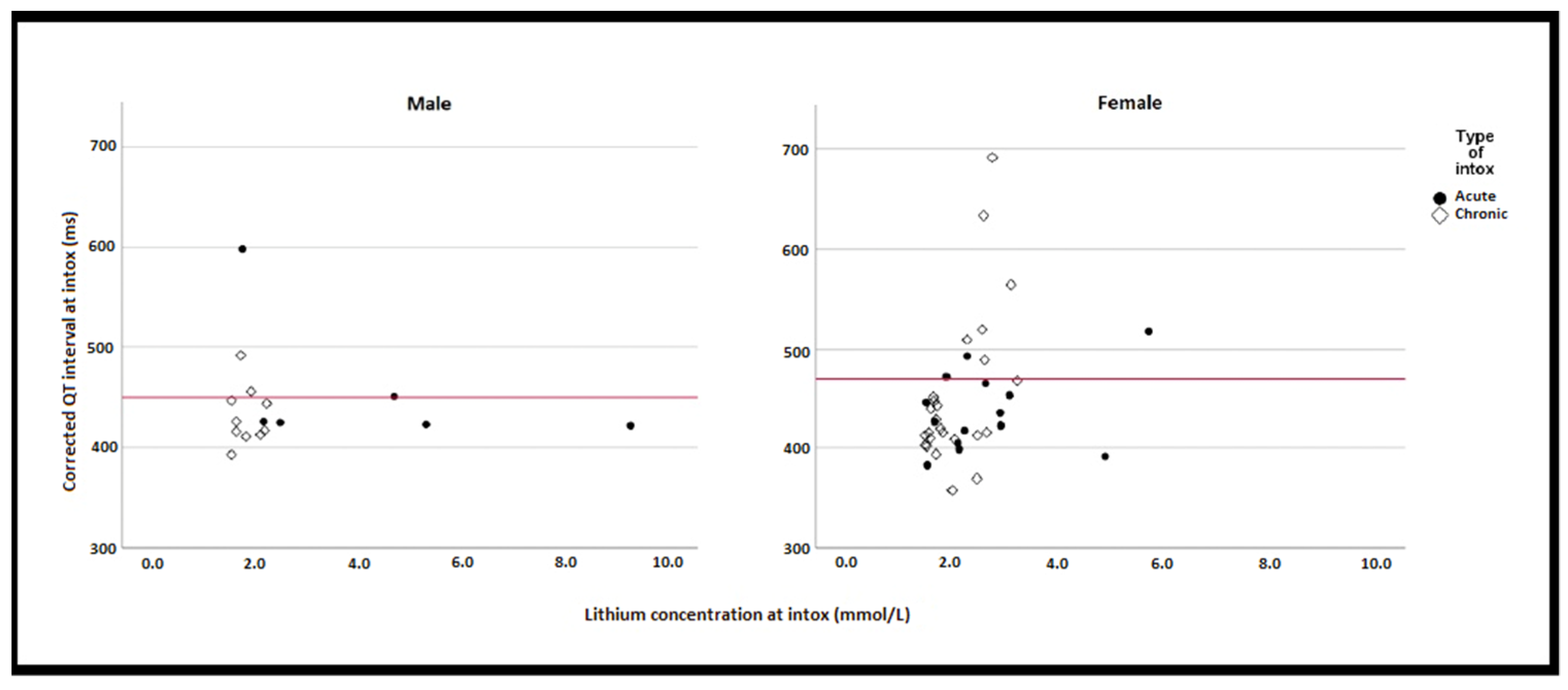
3.4. QT Interval
3.5. T-Wave Inversion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- NICE. Bipolar Disorder: Assessment and Management. Clinical Guideline 185; National Institute for Health and Care Excellence: London, UK, 2014; Available online: https://www.nice.org.uk/guidance/cg185 (accessed on 30 November 2021).
- Kirov, G. Lithium plus valproate combination therapy versus monotherapy for relapse prevention in bipolar I disorder (BALANCE): A randomised open-label trial. Lancet 2010, 375, 385–395. [Google Scholar] [CrossRef]
- Antolín-Concha, D.; Lähteenvuo, M.; Vattulainen, P.; Tanskanen, A.; Taipale, H.; Vieta, E.; Tiihonen, J. Suicide mortality and use of psychotropic drugs in patients hospitalized due to bipolar disorder: A Finnish nationwide cohort study. J. Affect. Disord. 2020, 277, 885–892. [Google Scholar] [CrossRef]
- Öhlund, L.; Ott, M.; Bergqvist, M.; Oja, S.; Lundqvist, R.; Sandlund, M.; Renberg, E.S.; Werneke, U. Clinical course and need for hospital admission after lithium discontinuation in patients with bipolar disorder type I or II: Mirror-image study based on the LiSIE retrospective cohort. BJPsych Open 2019, 5, e101. [Google Scholar] [CrossRef] [PubMed]
- Joas, E.; Karanti, A.; Song, J.; Goodwin, G.M.; Lichtenstein, P.; Landén, M. Pharmacological treatment and risk of psychiatric hospital admission in bipolar disorder. Br. J. Psychiatry 2017, 210, 197–202. [Google Scholar] [CrossRef]
- Hayes, J.F.; Marston, L.; Walters, K.; Geddes, J.R.; King, M.; Osborn, D.P. Lithium vs. valproate vs. olanzapine vs. quetiapine as maintenance monotherapy for bipolar disorder: A population-based UK cohort study using electronic health records. World Psychiatry 2016, 15, 53–58. [Google Scholar] [CrossRef]
- Ott, M.; Stegmayr, B.; Renberg, E.S.; Werneke, U. Lithium intoxication: Incidence, clinical course and renal function—A population-based retrospective cohort study. J. Psychopharmacol. 2016, 30, 1008–1019. [Google Scholar] [CrossRef]
- Mehta, N.; Vannozzi, R. Lithium-induced electrocardiographic changes: A complete review. Clin. Cardiol. 2017, 40, 1363–1367. [Google Scholar] [CrossRef]
- Hsu, C.-H.; Liu, P.-Y.; Chen, J.-H.; Yeh, T.-L.; Tsai, H.-Y.; Lin, L.-J. Electrocardiographic Abnormalities as Predictors for Over-Range Lithium Levels. Cardiology 2005, 103, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Mamiya, K.; Sadanaga, T.; Sekita, A.; Nabeyama, Y.; Yao, H.; Yukawa, E. Lithium concentration correlates with QTc in patients with psychosis. J. Electrocardiol. 2005, 38, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Darbar, D.; Yang, T.; Churchwell, K.; Wilde, A.A.M.; Roden, D.M. Unmasking of Brugada Syndrome by Lithium. Circulation 2005, 112, 1527–1531. [Google Scholar] [CrossRef] [PubMed]
- Vodovar, D.; El Balkhi, S.; Curis, E.; Deye, N.; Mégarbane, B. Lithium poisoning in the intensive care unit: Predictive factors of severity and indications for extracorporeal toxin removal to improve outcome. Clin. Toxicol. 2016, 54, 615–623. [Google Scholar] [CrossRef]
- Ström, M. ECG Changes during Lithium Intoxication. 2017. Available online: https://www.diva-portal.org/smash/record.jsf?dswid=-4106&pid=diva2%3A1141514 (accessed on 17 May 2022).
- Öhlund, L.; Ott, M.; Oja, S.; Bergqvist, M.; Lundqvist, R.; Sandlund, M.; Renberg, E.S.; Werneke, U. Reasons for lithium discontinuation in men and women with bipolar disorder: A retrospective cohort study. BMC Psychiatry 2018, 18, 37. [Google Scholar] [CrossRef]
- Lieber, I.; Ott, M.; Öhlund, L.; Lundqvist, R.; Eliasson, M.; Sandlund, M.; Werneke, U. Lithium-associated hypothyroidism and potential for reversibility after lithium discontinuation: Findings from the LiSIE retrospective cohort study. J. Psychopharmacol. 2019, 34, 293–303. [Google Scholar] [CrossRef]
- Bazett, H.C. An analysis of the time-relations of the electrocardiograms. Heart 1920, 7, 353–370. [Google Scholar] [CrossRef]
- Sokolow, M.; Lyon, T.P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Hear. J. 1949, 37, 161–186. [Google Scholar] [CrossRef]
- Sverker, J. Klinisk EKG-DIAGNOSTIK 2.0., 1st ed.; Elander: Mölnlycke, Sweden, 2012; pp. 26–35. [Google Scholar]
- Prineas, R.; Crow, R.; Blackburn, H. The Minnesota Code Manual of Electrocardiographic Findings; John Wright-PSG, Inc.: Littleton, MA, USA, 1982; Available online: http://users.stlcc.edu/departments/fvbio/ECG_MNcode.pdf (accessed on 17 May 2022).
- Chen, K.-P.; Shen, W.W.; Lu, M.-L. Implication of serum concentration monitoring in patients with lithium intoxication. Psychiatry Clin. Neurosci. 2003, 58, 25–29. [Google Scholar] [CrossRef]
- Wood, A.J.; Price, L.H.; Heninger, G.R. Lithium in the Treatment of Mood Disorders. New Engl. J. Med. 1994, 331, 591–598. [Google Scholar] [CrossRef]
- Ott, M.; Stegmayr, B.; Salander Renberg, E.; Werneke, U. Prognosis and outcome of severe lithium poisoning: Authors’ reply. J. Psychopharmacol. 2017, 31, 1275–1277. [Google Scholar]
- Woosley, R.L.; Heise, C.W.; Gallo, T.; Tate, J.; Woosley, D.; Romero, K.A. QTdrugs List [Internet]. Available online: https://crediblemeds.org (accessed on 25 November 2021).
- Danielsson, B.; Collin, J.; Bergman, G.J.; Borg, N.; Salmi, P.; Fastbom, J. Antidepressants and antipsychotics classified with torsades de pointes arrhythmia risk and mortality in older adults—A Swedish nationwide study. Br. J. Clin. Pharmacol. 2016, 81, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, C.; Thalamus, J.; Kristoffersen, D.T.; Svendsen, M.V.; Holla, L.; Heldal, K.; Haugaa, K.; Hysing, J. QT prolongation predicts short-term mortality independent of comorbidity. Europace 2019, 21, 1254–1260. [Google Scholar] [CrossRef] [PubMed]
- Bucht, G.; Smigan, L.; Wahlin, A.; Eriksson, P. ECG Changes during Lithium Therapy. Acta Medica Scand. 2009, 216, 101–104. [Google Scholar] [CrossRef]
- Baird-Gunning, J.; Lea-Henry, T.; Hoegberg, L.C.G.; Gosselin, S.; Roberts, D.M. Lithium Poisoning. J. Intensiv. Care Med. 2016, 32, 249–263. [Google Scholar] [CrossRef]
- Waring, W.S. Delayed Cardiotoxicity in Chronic Lithium Poisoning: Discrepancy between Serum Lithium Concentrations and Clinical Status. Basic Clin. Pharmacol. Toxicol. 2007, 100, 353–355. [Google Scholar] [CrossRef]
- Decker, B.S.; Goldfarb, D.S.; Dargan, P.I.; Friesen, M.; Gosselin, S.; Hoffman, R.S.; Lavergne, V.; Nolin, T.D.; Ghannoum, M.; EXTRIP Workgroup. Extracorporeal Treatment for Lithium Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup. Clin. J. Am. Soc. Nephrol. 2015, 10, 875–887. [Google Scholar] [CrossRef]
| ECG | Criteria |
|---|---|
| ECGINTOX | Acute intoxication: ECG within 24 h from detected s-Li ≥ 1.5 mmol/L Chronic intoxication: ECG within four days from detected s-Li ≥ 1.5 mmol/L |
| ECGPRE-INTOX | ECG taken at least one day before lithium intoxication |
| ECGPOST-INTOX | ECG taken later than four days after lithium intoxication |
| ECG Changes | Criteria |
|---|---|
| PQ interval | Prolonged if >220 ms |
| Heart rate | Bradycardia < 50 b/min Tachycardia > 100 b/min |
| QT prolongation | QTc > 470 ms for females, QTc > 450 ms for males f a U-wave was present, the QT interval was measured from the beginning of the Q-wave to the nadir on the U-wave. |
| ST segment elevation | If present in two adjacent leads with ≥2 mm for males and ≥1.5 mm for females in V2-V3, or ≥1 mm in other leads. |
| ST segment depression | If present with ≥1 mm in two adjacent leads |
| T-wave changes | If inverted |
| U-wave | If present |
| Age, mean (SD) | 55.2 (18.5) years |
| Age, median (min-max) | 56.0 (22–86) years |
| Sex, n (%) Male Female | 16 (29) 39 (71) |
| Type of intoxication, n (%) Acute Chronic | 20 (36) 35 (64) |
| Lithium concentration at time of intoxication, mean (SD) | 2.4 (1.3) mmol/L |
| Lithium concentration at time of intoxication, median (min-max) | 2.1 (1.5–9.3) mmol/L |
| Severity of intoxication, n (%) Severe (>2.5 mmol/L) Moderate (≤2.5 mmol/L) | 16 (29) 39 (71) |
| Dialysis treatment, n (%) | 11 (20) |
| Lithium concentration in episodes treated with dialysis, median (min-max) | 2.7 (1.9–9.3) mmol/L |
| Lithium concentration in episodes treated without dialysis, median (min-max) | 1.8 (1.5–5.3) mmol/L |
| Time between lithium serum concentration measurement and ECG, mean (SD) | 1.0 (8.0) h |
| Pre-existing cardiac and vascular comorbidities at time of intoxication, n (%) Total Cerebral stroke/TIA Ischemic heart disease Heart failure Angina pectoris Atrial fibrillation Bradycardia Hypertension Pace-maker use | 28 (51) 5 (9) 3 (5) 6 (11) 2 (4) 3 (5) 1 (2) 25 (45) 1 (2) |
| Cardiac risk factors at time of intoxication, n (%) Diabetes mellitus type 1 Diabetes mellitus type 2 Hyperlipidaemia | 3 (5) 7 (13) 8 (15) |
| Presence of medications with known risk of TdP, n (%) a | 12 (22) |
| Presence of antiarrhythmic medication including beta blockers, n (%) a | 13 (24) |
| Presence of antihypertensive medication excluding beta-blockers, n (%) a | 23 (42) |
| Potassium at time of intoxication, mean (SD) b | 4.3 (0.8) mmol/L |
| Potassium concentration at time of intoxication, median (min-max) b | 4.2 (2.8–7.3) mmol/L |
| Hypokalaemia b,c, n (%) | 8 (15) |
| Hyperkalaemia b,d, n (%) | 13 (24) |
| Heart rate, n (%) Bradycardia Tachycardia | 3 (5) 3 (5) |
| Rhythm, n (%) Sinus rhythm
Atrial fibrillation Pacemaker rhythm | 48 (87) 1 (2) 2 (4) 4 (7) 1 (2) |
| PQ interval, n (%) Prolongation a
| 2 (4) 2 (4) |
| Branch block, n (%) LBBB RBBB | 1 (2) 2 (4) |
| QT prolongation, n (%) | 13 (24) |
| ST segment elevation, n (%) b | 0 (0) |
| ST segment depression, n (%) b | 2 (4) |
| T-wave inversion, n (%) c | 23 (42) |
| U-waves, n (%) | 4 (7) |
| Episode (n = 13) | Type of Intoxication | s-Li (mmol/L) | s-K (mmol/L) | QTc at Intoxication (s) | QTc in Reference ECG (s) | Other ECG Findings | Drugs with Known or Possible Risk of TdP | Drugs with Conditional Risk of TdP | Cardiac Comorbidity |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Chronic | 2.78 | 2.90 | 0.691 | Pre: 0.433 Post: 0.421 | Aripiprazole | Bendroflumethiazide Furosemide | Hypertension Angina pectoris | |
| 2 | Chronic | 2.62 | 3.70 | 0.633 | U-wave Inverted T-wave | None | None | None | |
| 3 | Acute on therapeutic | 1.76 | 3.40 | 0.598 | Tachycardia | Citalopram Haloperidol Chlorprothixene | None | None | |
| 4 | Chronic | 3.13 | 3.60 | 0.564 | Pre: 0.440 | RBBB Inverted T-wave | None | Omeprazole Furosemide | Hypertension |
| 5 | Chronic | 2.59 | 3.70 | 0.519 | Pre: 0.394 Post: 0.400 | Bradycardia | None | Bendroflumethiazide | Hypertension |
| 6 | Acute on therapeutic | 5.73 | 4.70 | 0.517 | Pre: 0.443 | Levomepromazine Promethazine | Clomipramine Loperamide | None | |
| 7 | Chronic | 2.30 | 3.90 | 0.508 | Pre: 0.543 Post: 0.439 | Atrial PM rhythm U-wave | Venlafaxine | Olanzapine | Heart failureSick sinus syndrome (PM) |
| 8 | Acute | 2.30 | 3.10 | 0.493 | Post: 0.372 | None | None | None | |
| 9 | Chronic | 1.73 | 4.80 | 0.492 | Pre: 0.461 Post: 0.411 | LBBB Inverted T-wave AV block I | None | Olanzapine Omeprazole | Hypertension |
| 10 | Chronic | 2.64 | 2.80 | 0.489 | Pre: 0.400 Post: 0.428 | U-wave Inverted T-wave | Citalopram Clozapine | None | None |
| 11 | Acute on therapeutic | 1.91 | 4.30 | 0.472 | Pre: 0.422 | LVH | None | Hydroxyzine Formoterol | Hypertension |
| 12 | Chronic | 1.93 | 3.00 | 0.456 | Pre: 0.468 | Clozapine | Loperamide | Hypertension | |
| 13 | Acute on therapeutic | 4.69 | 4.60 | 0.451 | Post: 0.424 | Tachycardia | None | Clomipramine | None |
| OR [95% CI] | p | |
|---|---|---|
| Lithium concentration (mmol/L) >2.5 mmol/L = Severe ≤2.5 mmol/L = Moderate (baseline) | 4.28 [1.15–15.95] | 0.030 |
| Age ≥65 years <65 (baseline) | 1.25 [0.35–4.53] | 0.734 |
| Sex Female Male (baseline) | 0.90 [0.23–3.49] | 0.879 |
| Type of intoxication Chronic Acute (baseline) | 0.89 [0.25–3.21] | 0.857 |
| Potassium concentration (mmol/L) Hypokalaemia a Hyperkalaemia b Normal (baseline) | 6.67 [1.23–36.06] 0.73 [0.13–4.19] | 0.028 0.722 |
| Co-medication with drugs with known or possible risk for QT prolongation Yes No (baseline) | 0.53 [0.15–1.85] | 0.318 |
| Concomitant use of medicines with other cardiac effects Yes No (baseline) | 1.17 [0.34–4.06] | 0.809 |
| Cardiovascular comorbidities and risk factors Yes No (baseline) | 1.17 [0.34–4.06] | 0.809 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Truedson, P.; Ott, M.; Lindmark, K.; Ström, M.; Maripuu, M.; Lundqvist, R.; Werneke, U. Effects of Toxic Lithium Levels on ECG—Findings from the LiSIE Retrospective Cohort Study. J. Clin. Med. 2022, 11, 5941. https://doi.org/10.3390/jcm11195941
Truedson P, Ott M, Lindmark K, Ström M, Maripuu M, Lundqvist R, Werneke U. Effects of Toxic Lithium Levels on ECG—Findings from the LiSIE Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(19):5941. https://doi.org/10.3390/jcm11195941
Chicago/Turabian StyleTruedson, Petra, Michael Ott, Krister Lindmark, Malin Ström, Martin Maripuu, Robert Lundqvist, and Ursula Werneke. 2022. "Effects of Toxic Lithium Levels on ECG—Findings from the LiSIE Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 19: 5941. https://doi.org/10.3390/jcm11195941
APA StyleTruedson, P., Ott, M., Lindmark, K., Ström, M., Maripuu, M., Lundqvist, R., & Werneke, U. (2022). Effects of Toxic Lithium Levels on ECG—Findings from the LiSIE Retrospective Cohort Study. Journal of Clinical Medicine, 11(19), 5941. https://doi.org/10.3390/jcm11195941







