Abstract
Background: Thrombotic conditions triggered by SARS-CoV-2 virus can result in high mortality, especially in pregnant women as they are already in a hypercoagulability state. This thereby leads to excessive inflammation that will increase the risk of thromboembolic (TE) complications. Objective: The aim of this study is to review the prevalence of thromboembolic complications such as deep venous thrombosis, pulmonary embolism, and intervillous thrombosis, and their preventive strategies among pregnant women infected with COVID-19. Method: The articles were retrieved from online databases PubMed and ScienceDirect published from February 2020 to April 2022. Findings: A total of 5249 participants including 5128 pregnant women and 121 placentas from 19 studies were identified for having TE complications after being infected with COVID-19. The types of TE complications that developed within pregnant women were disseminated intravascular coagulation (DIC) (n = 44, 0.86%), unmentioned thromboembolic complications (TE) (n = 14, 0.27%), intervillous thrombosis (IVT) (n = 9, 0.18%), pulmonary embolism (PE) (n = 6, 0.12%), COVID-19 associated coagulopathy (CAC) (n = 5, 0.10%), and deep venous thrombosis (DVT) (n = 2, 0.04%). Whereas the prevalence of TE complications reported from studies focusing on placenta were IVT (n = 27, 22.3%), subchorionic thrombus (SCT) (n = 9, 7.44%), and placental thrombosis (n = 5, 4.13%). Thromboprophylaxis agent used among pregnant women include low molecular weight heparin (LMWH) at prophylactic dose (n = 9). Conclusions: The prevalence of thromboembolic complications among pregnant women infected by COVID-19 is low with DIC being the most common form and placental thrombosis being the least common form of TE complications that occurred within pregnant women infected with COVID-19. Anticoagulation, in particular LMWH (variable dose), is frequently used to prevent TE complications.
1. Introduction
As of December 2019, Coronavirus Disease 2019 (COVID-19) is an infectious disease caused by a new coronavirus, SARS-CoV-2, which was first reported in Wuhan, China. It is a single-stranded RNA virus that infects cells by binding to angiotensin converting enzyme-2 (ACE2) receptors [1,2]. The infection may be asymptomatic or symptomatic with clinical manifestations such as fever, cough, sore throat, and headache, but it might also develop into severe diseases. Despite the fact that COVID-19 was initially thought to be a pulmonary sickness that caused morbidity and mortality in the elderly and those with underlying medical disorders, younger and pregnant patients may also develop moderate to severe symptoms that require hospitalization due to various complications such as thromboembolic (TE) complication.
TE complications are often multifactorial. Venous thromboembolism (VTE) is a disorder in which the blood clots abnormally and is linked to a high rate of morbidity and mortality [3]. VTE can be divided into deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT occurs when clots are developed in the deep veins, primarily in the legs, while PE occurs when a clot in the deep vein lodges loosely and travels to the arteries of the lungs. VTE episodes were shown to be four- to five-folds higher in pregnant women than in non-pregnant women [4,5]. The clinical manifestations of DVT are usually swelling and pain in the extremity or lower leg regions, whereas PE is characterized by symptoms such as dyspnoea, tachypnoea, and chest pain.
Meanwhile, disseminated intravascular coagulation (DIC) is another TE complication, which is characterized by the presence of many micro clots in the vasculature, as well as an increased haemorrhagic predisposition [6]. The signs of DIC are usually bleeding, shortness of breath, and low blood pressure due to constant bleeding. COVID-19 associated coagulopathy (CAC) is also one of the TE complications that develop due to the fact that COVID-19 is highly prothrombotic in which it can cause overstimulation of inflammatory factors resulting in the coagulation cascade to occur.
Meanwhile, other types of TE complications can also develop in the placenta of pregnant women, e.g., (i) intervillous thrombosis (IVT), in which the blood clot is present in the intervillous space; (ii) subchorionic thrombus (SCT), in which the thrombus confined to the subchorionic space; and (iii) placental thrombosis, in which the clots can be found in the fetal circulation. These complications can occur due to multiple aetiologies specifically associated with the Virchow’s triad, involving stasis, endothelial injury, and hypercoagulability [7].
Pregnant women are one of the high-risk categories for COVID-19 infection given their circumstances during and after pregnancy compared to non-pregnant women. This is due to pregnant women experiencing immunologic and physiologic alteration, making them more susceptible to viral respiratory infections [8]. Without COVID-19, they are more likely to develop adverse pregnancy outcomes, e.g., preeclampsia and preterm labor. However, once infected with COVID-19, they are more likely to experience serious complications due to massive inflammation and endothelial damage, thereby triggering the coagulation cascade to be activated and thereby promoting thromboembolic complications.
As cases involving TE events in pregnant women have evolved, practitioners have utilized anticoagulation as the prophylaxis and initial treatment. Low molecular weight heparin (LMWH) is used as a thromboprophylaxis and treatment in pregnant women infected with COVID-19.
Since COVID-19 has created a serious threat to human health resulting in significant increases in morbidity and mortality worldwide, the scenario becomes considerably more serious when the virus infects pregnant mothers since they are already in a hypercoagulable state causing substantial inflammation and coagulation leading to the thromboembolic complications. These TE complications have been reported in many pregnant women with the outcomes being either survival or death. Therefore, the purpose of this study is to review the prevalence of TE events among pregnant women who are infected with COVID-19 as well as their preventive strategies.
2. Materials and Methods
A comprehensive structured literature search was performed based on the scientific online databases PubMed and ScienceDirect published from February 2020 to April 2022. The search included research papers, case series, and case reports with the following keywords: COVID-19, thromboembolic complications, pregnancy, prevalence, venous thromboembolism, pulmonary embolism, deep venous thrombosis, disseminated intravascular coagulation, and intervillous thrombosis. A search filter was used to only include articles published in the English language. The articles were screened by assessing the title and abstract for the inclusion and exclusion criteria. The inclusion criteria included research publications, original articles, case reports, and case series. General review, irrelevant research regarding thrombocytopenia, placenta as the subjects without details of the mothers, physician as the subjects instead of pregnant women, and fetal vessels were all excluded. The gathered articles were assessed for eligibility in which only studies with reported prevalence of TE events were included. The final gathered studies (n = 19) were then extracted into Microsoft Excel software for the data analysis.
The prevalence of TE complications among positive COVID-19 pregnant women was calculated by dividing the number of women who experience thromboembolism by the entire population of pregnant women involved in collected studies. Whereas the prevalence of TE complications reported from studies focusing on placenta were calculated by dividing the total number of those who develop placental thromboembolism by the total number of placentas from the collected studies.
3. Results
The search identified 150 articles, which after the screening of titles, abstracts, and assessing for eligibility, only 19 studies were included (Figure 1). From the 19 studies, most [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26] of them were (n = 5) case series [16,17,18,19,20] and case reports (n = 6) [21,22,23,24,25,26]. Seven studies [8,10,11,12,13,14,15] were performed retrospectively and one [9] was a systematic review. The studies were mostly conducted from 2018 until May 2021. These 19 studies involving 5249 participants included 5128 pregnancies and 121 placentas being examined for TE complications caused by SARS-CoV-2 virus.
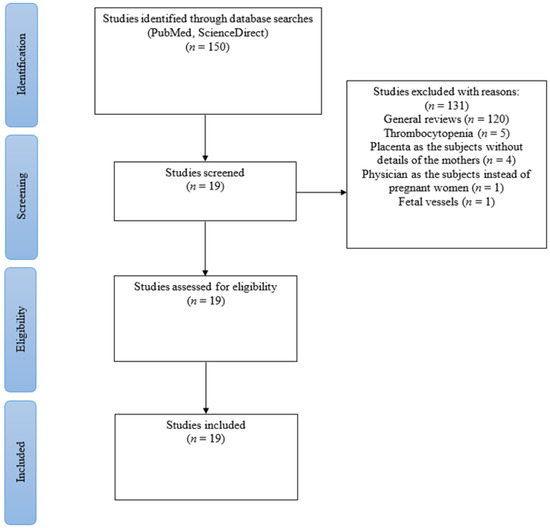
Figure 1.
PRISMA chart.
According to Table 1 and Table 2, from the 19 studies included, 7 studies were conducted in North America [10,12,13,14,15,18,20], 6 in Europe [11,17,19,23,24,26], 1 in the Middle East [21], and others were each conducted in South Asia [22], East Asia [8], and South America [25], and one was a multicentre study [16]. Most studies were performed in adults (mean/median age ranging from 17 to 47 years). The majority (n = 4012) of the patients included were Hispanic (44.9%) and Non-Hispanic White (31.1%) with the mean/median age ranging from 28.9 to 30 years, while the remaining were Non-Hispanic Black (14.5%), Asian (1.37%), African-American (0.72%), and others (7.45%) [10,12,14,15,25].

Table 1.
Demographic characteristics of case reports/case series reporting thromboembolic (TE) complications among pregnant women infected with COVID-19.

Table 2.
Demographics characteristics of retrospective/prospective/cohort studies reporting thromboembolic (TE) complications among pregnant women infected with COVID-19.
Based on the 19 studies included, pregnant mothers have many comorbidities, e.g., diabetes mellitus type 1 and type 2 [13,15,23,24], gestational diabetes [15], hypothyroidism [13,17], hypertension [13,15], preeclampsia [13,23], and asthma [13,15,24] (Table 1 and Table 2). One case report [21] recorded in Iran presented a patient with clinical manifestations of loss of consciousness, double mydriasis, and tonic-clonic seizures (Table 1).
Laboratory findings (Table 3, Table 4 and Table 5) that were associated with TE events include D-dimer, fibrinogen and C-reactive protein (CRP) levels, as well as radiological imaging. Eight studies [9,11,16,17,22,23,25,26] showed elevated D-dimer level (1.8 to 34.47 mg/L) (Normal range (NR): 0.1–1.7 mg/L), five studies [8,11,16,23,26] for elevated CRP level ranging from 14 to 60 mg/L (NR: 1–10 mg/L), and four studies [16,21,25,26] for elevated fibrinogen ranging from 5.43 to 3530 g/L (NR: 1.5–4.2 g/L). In addition, seven studies [12,18,21,22,24,25,26] included radiological imaging and histopathology examination to confirm the diagnosis of TE complications. For instance, routine histopathology and complement staining for placental thrombosis, echocardiography, computerized tomography pulmonary angiogram (CTPA) and chest CT scan for PE, as well as fetal-placental magnetic resonance imaging, anatomopathological examination of placenta, and placenta pathology for IVT.

Table 3.
Laboratory findings, Prevalence, and Outcomes of case reports/case series reporting thromboembolic (TE) complications among pregnant women infected with COVID-19.

Table 4.
Laboratory findings, Prevalence, and Outcomes of retrospective/prospective/cohort studies reporting thromboembolic (TE) complications among pregnant women infected with COVID-19.

Table 5.
Systematic review reporting thromboembolic (TE) complications among pregnant women infected with COVID-19.
The most common TE complications within pregnant women (n = 5128) were DIC (n = 44, 0.86%), TE (n = 14, 0.27%), IVT (n = 9, 0.18%), PE (n = 6, 0.12%), CAC (n = 5, 0.10%), and DVT (n = 2, 0.04%). (Table 3, Table 4 and Table 5). Meanwhile, the prevalence of TE complications reported from studies focusing on placenta (n = 121) were IVT (n = 27, 22.3%), SCT (n = 9, 7.44%), and placental thrombosis (n = 5, 4.13%) (Table 3 and Table 4). TE complications that occur during pregnancy were DIC (n = 37, 33.3%), TE (n = 13, 11.7%), CAC (n = 3, 2.7%), and PE (n = 2, 1.8%), whereas cases that occur during the postpartum period were IVT (n = 36, 32.4%), SCT (n = 9, 8.1%), placenta thrombosis (n = 5, 4.5%), DVT (n = 2, 1.8%), PE (n = 2, 1.8%), and CAC (n = 2, 1.8%) (Table 1 and Table 2). From the 19 studies included, seven mothers [9,15,21,24] and two neonates died [21,25], whereas the others were discharged well [8,15,16,17,18,22,23,26] (Table 3, Table 4 and Table 5).
Only nine studies [9,11,14,16,17,21,22,24,26] reported thromboprophylaxis strategies among COVID-19 infected pregnant women with TE complications (Table 6). Most studies (n = 9) used anticoagulation, specifically LMWH such as Enoxaparin at prophylactic dose (40–60 mg once daily (OD)). Only one study [9] used therapeutic dose of anticoagulant for the prevention of TE complications.

Table 6.
Thromboprophylaxis used among COVID-19 infected pregnant women with TE complications.
4. Discussion
In this study, we investigate the global prevalence of COVID-19 positive pregnant women who experience TE complications. Findings showed that the prevalence of TE complications among pregnant women infected with COVID-19 is low with the most common form being DIC. LMWH (in variable dose) is frequently used to prevent TE complications in pregnant women.
According to the results obtained, the types of TE complications which developed among pregnant women with COVID-19 were DIC (n = 44, 0.86%), TE (n = 14, 0.27%), IVT (n = 9, 0.18%), PE (n = 6, 0.12%), CAC (n = 5, 0.10%), and DVT (n = 2, 0.04%), whereas complications that developed in the placenta were IVT (n = 27, 22.3%), SCT (n = 9, 7.44%), and placental thrombosis (n = 5, 4.13%). Most of the pregnant women were in the age range of 17 to 47 years old, with underlying comorbidities such as hypertension and diabetes mellitus and presented with TE complications more commonly in the postpartum rather than prepartum period.
Several explanations can be given to the observed findings. Both pregnancy and COVID-19 infection can increase the risk of TE complications. Pregnant women are already known to be in a hypercoagulable state physiologically, so they are more susceptible to COVID-19 due to their physiological alterations. This indirectly can increase the risk of dying due to COVID-19 [9,27]. Pregnant women experience a significant immunocompromised condition generated by the changes in the body’s cell-mediated immune response and inflammatory mechanisms [28]. Pro-inflammatory factors such as von Willebrand factor and fibrinogen are intended to prevent excessive blood loss after birth, but in certain women, this effect is exaggerated causing them to have an elevated risk of thrombosis [1]. Therefore, this hypercoagulable state increased the risk of TE events and morbidity by 4- to 6-fold, with higher risk in the post-partum period [28].
The SARS-CoV-2 virus causes endothelial injury and triggers the innate immune responses by activating the monocytes which are responsible for massive release of proinflammatory cytokines and also platelets activation [29]. Then, the ACE2 receptor on the endothelium surface binds to SARS-CoV-2 virus resulting in conversion of Angiotensin I (ATI) to Angiotensin II (ATII). This ATII pathway causes inflammation by increasing the levels of pro-inflammatory cytokines and chemokines such as Interleukin-6 (IL-6), IL-8, and tumor necrosis factor-α (TNF-α). The cytokines enters the circulation and attract T-lymphocytes and monocytes, causing inflammatory injury to the virally infected cells [30]. Thus, overproduction of ATII will cause the overproduction of cytokines [31].
The pathophysiology of thromboembolism can be aggravated by inflammation [32]. This is because inflammation, particularly at the blood vessel walls, can trigger the activation of the coagulation pathway by inducing the tissue factor (TF). When blood vessels become inflamed, endothelial cells, platelets, and cytokines are generated, triggering the production of TF. By increasing the expression of TF, these mediators can increase the procoagulant state. TNF-α can activate Factor II, causing activation of the extrinsic coagulation cascade [33].
Apart from that, inflammation can increase hypercoagulability by stimulating TF pathways and inducing NETosis [33]. In response to infection, it creates neutrophils extracellular traps (NET), which allows them to trap and destroy the invading virus. The production of NET, which induces fibrin production and deposition in the blood vessels, causes a reaction known as NETosis [32]. As a result, the increased amount of NET promotes synthesis of fibrin, which increases the risk of thrombus and thereby amplifies the hypercoagulable condition state [33].
Overall, SARS-CoV-2 increases NET’s formation, cytokine overproduction, and hyperinflammation, in which all of these will consequently cause coagulopathy [31]. So, once the virus infects pregnant women, it will cause a massive inflammatory reaction since they are already in a hypercoagulable state, and this will further increase the risks of TE complications.
Our findings suggest that DIC is the most common type of TE complication among COVID-19 positive pregnant women (n = 44, 0.86%). This can be due to the fact that DIC is secondary to many clinical conditions such as sepsis and septic shock as well as obstetric conditions such as eclampsia [17]. The term sepsis refers to the body’s severe reaction towards a life-threatening infection, e.g., bacterial infection or pneumonia, and can lead to death [34]. To fight the infection, the immune system goes into overdrive, releasing chemicals into the bloodstream. This sets off a chain reaction resulting in serious inflammatory reaction throughout the body [35]. The SARS-CoV-2 virus can induce pneumonia in individuals which can lead to viral sepsis. As a result, it can trigger concurrent activation of coagulation and fibrinolytic cascade, which leads to coagulopathy [16].
Other than DIC, other complications occurring in pregnancies were TE (n = 14, 0.27%), PE (n = 6, 0.12%), CAC (n = 5, 0.10%), and DVT (n = 2, 0.04%). This is plausible given that pregnant women are at a higher risk of both venous and arterial thrombosis during pregnancy, but the risk of VTE is greater than the risk of arterial thrombosis, which is 4- to 5- folds compared to arterial (3- to 4-fold) [5,36]. From our findings, the risk of TE complications is higher (n = 56) in the postpartum period compared to the prepartum period (n = 55) and studies have shown approximately 2 out of every 1000 births of pregnant women will experience TE events [5]. Since COVID-19 infection is highly prothrombotic and linked to a unique type of coagulopathy, it can cause systemic inflammation and CAC. CAC develops because of overstimulation of the inflammatory cascade, leading to endothelial and platelet activation [37]. Additionally, the presence of a hypercoagulation state triggered by the deep and complex inflammatory response to the virus as well as hypercoagulability state of pregnant women alters the coagulation cascade in the body in a condition also known as ‘thrombo-inflammation’ [38].
Furthermore, there were also TE complications in placenta, which were IVT, SCT, and placental thrombosis. IVT is a specific form of thrombosis that occurs in the placenta and is characterised by the presence of blood clots in the intervillous space, and it is found next to the chorionic plate (subchorionic), in the centre of the parenchymal mass, or adjacent to the basal plate [7]. SCT, on the other hand, occurs due to the deposition of fibrin plaque in the subchorionic space in the placenta, and lastly, placental thrombosis can occur in fetal circulation. These pathological lesions are linked to the Virchow’s triad (venous or circulatory stasis, hypercoagulability, and vein damage). Stasis of maternal blood decreases blood flow in the placenta and enables the accumulation of procoagulant proteases, e.g., thrombin and fibrinogen, which may overcome the local anticoagulant pathways and thereby induce thrombosis [39]. It might also be related to irregular blood flow, which can occur when IVT, SCT, and placental thrombosis develop as a result of direct compression during labour or acute villous oedema, where substantial deformation of the villi creates local stasis and thrombus [7]. Other than that, it might be attributed to maternal hypercoagulability, in which thrombi form spontaneously, most frequently in low-flow regions.
There are several other studies investigating the TE complications among pregnant women infected with COVID-19. According to a case control study by Resta et al. [40], they discovered thrombi in fetal vessels in 16 out of 71 cases of pregnant mothers infected with COVID-19. Moreover, Ko et al. [41] found an adjusted risk ratio of 2.7 for TE complications from 6550 COVID-19 positive pregnancies. Another study by Levitan et al. [42] reported that 15 out of 65 pregnant women infected with COVID-19 developed intervillous thrombosis, whereas 18 of the 74 placentas from pregnant women who tested positive for COVID-19 in a study by Zhang et al. [43] developed thrombosis.
There are a variety of risk factors that might increase the chances of getting thromboembolism. Damage to a vein caused by a fracture, a significant major injury, or major surgery involving the pelvis, hip, or legs can all raise the risk of TE complications. Other factors that might increase the risk of TE include pregnancy, a family history of VTE, birth control pills, and increasing age [44].
Thromboembolism is not age specific. According to the 19 studies included [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], a majority of the studies were performed in adults with mean/median age ranging from 17 to 47 years. However, TE complications frequently occurred among pregnant women in the age range of 29 (five studies) [8,14,15,22,24].
It is widely known that D-dimer levels rise steadily during pregnancy and increased D-dimer concentrations indicate the activation of the coagulation cascade and reflect poor prognosis [11,45]. It was shown that pregnant COVID-19 patients had higher D-dimer levels than pregnant women who were not infected, which suggest increased risk of TE complications [45]. This can also be supported by a study by Wang et al. [45], which found that D-dimer levels in 27 pregnant women with COVID-19 infection ranged from below 3 µg/mL to over 5 µg/mL, all of which were beyond the normal range and indicated a higher risk of TE consequences. From the results obtained, 8 out of 19 studies showed elevated D-dimer levels, with values ranging from >1.8 to 34.37 mg/L. Moreover, CRP, a pentameric protein level, also rises in response to inflammation, and thus enhances the thrombotic response to vascular damage. Elevated CRP appears to be a key mechanistic relationship between inflammation and thrombosis since inflammation upregulates CRP expression. It has also been shown that elevated plasma fibrinogen reflects an inflammatory state and increases the risk of VTE because high fibrinogen indicates enhanced blood clot formation [28,46]. The findings showed that both CRP and fibrinogen values were increased, with values ranging from 14 to 60 mg/L and 5.43 to 3530 g/L, respectively.
From the 19 studies included [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], only 9 [9,11,14,16,17,21,22,24,26] reported the thromboprophylaxis used to prevent TE complications. Most of them used LMWH such as Enoxaparin at prophylactic dose (40 mg OD) [47]. According to The International Society of Thrombosis and Haemostasis (ISTH) and the Scientific and Standardization Committee (SSC) of the ISTH [48,49], a prophylaxis dose of LMWH for VTE is recommended to prevent TE complications in the absence of contraindications. In general, heparin-based drugs are typically the preferred anticoagulants during pregnancy since they do not cross the placenta or penetrate breast milk, hence it is safe to use during pregnancy. Apart from that, they also do not induce any anticoagulant effect in the newborns [3,50,51], hence showing favourable safety profile to this population.
5. Conclusions
The prevalence of TE complications among pregnant women infected with COVID-19 is low (<3%) with DIC and DVT as the most and least common type of TE complications, respectively. LMWH is frequently used as a thromboprophylaxis agent. Further research is required to detect the prevalence of TE complications and optimal management of thromboembolic complications in the future.
Author Contributions
N.S.M.A.: methodology; formal analysis, investigation, data curation, writing—original draft preparation, and project administration; I.A.H.Z.: methodology; writing—original draft; Z.M.N.: writing—original draft; N.S.M.H.: writing—original draft and formal analysis; K.W.G.: funding acquisition; writing—original draft; and formal analysis; L.C.M.: resources, writing—review and editing, and funding acquisition; H.H.Z.: conceptualization; supervision; methodology; formal analysis; investigation; data curation; writing—original draft preparation; and project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
All data have been included in this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Daru, J.; White, K.; Hunt, B.J. COVID-19, thrombosis and pregnancy. Thromb Update 2021, 5, 100077. [Google Scholar] [CrossRef]
- He, M.; Skaria, P.; Kreutz, K.; Chen, L.; Hagemann, I.S.; Carter, E.B.; Mysorekar, I.U.; Nelson, D.M.; Pfeifer, J.; Dehner, L.P. Histopathology of Third Trimester Placenta from SARS-CoV-2-Positive Women. Fetal Pediatr. Pathol. 2020, 41, 403–412. [Google Scholar] [CrossRef]
- Bain, E.; Wilson, A.; Tooher, R.; Gates, S.; Davis, L.J.; Middleton, P. Prophylaxis for venous thromboembolic disease in pregnancy and the early postnatal period. Cochrane Database Syst. Rev. 2014, 2, Cd001689. [Google Scholar] [CrossRef]
- Gabrieli, D.; Cahen-Peretz, A.; Shimonovitz, T.; Marks-Garber, K.; Amsalem, H.; Kalish, Y.; Lavy, Y.; Walfisch, A. Thromboembolic events in pregnant and puerperal women after COVID-19 lockdowns: A retrospective cohort study. Int. J. Gynaecol. Obs. 2021, 155, 95–100. [Google Scholar] [CrossRef]
- James, A.H. Pregnancy-associated thrombosis. Hematology 2009, 2009, 277–285. [Google Scholar] [CrossRef]
- Levi, M.; Sivapalaratnam, S. Disseminated intravascular coagulation: An update on pathogenesis and diagnosis. Expert Rev. Hematol. 2018, 11, 663–672. [Google Scholar] [CrossRef]
- Morgen, E.K.; Fitzgerald, B.; Keating, S. Intervillous Thrombosis. In Pathology of the Placenta: A Practical Guide; Khong, T.Y., Mooney, E.E., Nikkels, P.G.J., Morgan, T.K., Gordijn, S.J., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 67–76. [Google Scholar] [CrossRef]
- Wu, Y.T.; Liu, J.; Xu, J.J.; Chen, Y.F.; Yang, W.; Chen, Y.; Li, C.; Wang, Y.; Liu, H.; Zhang, C.; et al. Neonatal outcome in 29 pregnant women with COVID-19: A retrospective study in Wuhan, China. PLoS Med. 2020, 17, e1003195. [Google Scholar] [CrossRef]
- Servante, J.; Swallow, G.; Thornton, J.G.; Myers, B.; Munireddy, S.; Malinowski, A.K.; Othman, M.; Li, W.; O’Donoghue, K.; Walker, K.F. Haemostatic and thrombo-embolic complications in pregnant women with COVID-19: A systematic review and critical analysis. BMC Pregnancy Childbirth 2021, 21, 108. [Google Scholar] [CrossRef]
- Gulersen, M.; Prasannan, L.; Tam Tam, H.; Metz, C.N.; Rochelson, B.; Meirowitz, N.; Shan, W.; Edelman, M.; Millington, K.A. Histopathologic evaluation of placentas after diagnosis of maternal severe acute respiratory syndrome coronavirus 2 infection. Am. J. Obs. Gynecol. MFM 2020, 2, 100211. [Google Scholar] [CrossRef]
- Pereira, A.; Cruz-Melguizo, S.; Adrien, M.; Fuentes, L.; Marin, E.; Perez-Medina, T. Clinical course of coronavirus disease-2019 in pregnancy. Acta Obs. Gynecol. Scand 2020, 99, 839–847. [Google Scholar] [CrossRef]
- Jani, S.; Jacques, S.M.; Qureshi, F.; Natarajan, G.; Bajaj, S.; Velumula, P.; Agu, C.; Bajaj, M. Clinical Characteristics of Mother–Infant Dyad and Placental Pathology in COVID-19 Cases in Predominantly African American Population. Am. J. Perinatol. Rep. 2021, 11, e15–e20. [Google Scholar] [CrossRef]
- Smithgall, M.C.; Liu-Jarin, X.; Hamele-Bena, D.; Cimic, A.; Mourad, M.; Debelenko, L.; Chen, X. Third-trimester placentas of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive women: Histomorphology, including viral immunohistochemistry and in-situ hybridization. Histopathology 2020, 77, 994–999. [Google Scholar] [CrossRef]
- Metz, T.D.; Clifton, R.G.; Hughes, B.L.; Sandoval, G.; Saade, G.R.; Grobman, W.A.; Manuck, T.A.; Miodovnik, M.; Sowles, A.; Clark, K.; et al. Disease Severity and Perinatal Outcomes of Pregnant Patients With Coronavirus Disease 2019 (COVID-19). Obs. Gynecol. 2021, 137, 571–580. [Google Scholar] [CrossRef]
- Litman, E.A.; Yin, Y.; Nelson, S.J.; Capbarat, E.; Kerchner, D.; Ahmadzia, H.K. Adverse perinatal outcomes in a large United States birth cohort during the COVID-19 pandemic. Am. J. Obstet. Gynecol. MFM 2022, 4, 100577. [Google Scholar] [CrossRef]
- Koumoutsea, E.V.; Vivanti, A.J.; Shehata, N.; Benachi, A.; Le Gouez, A.; Desconclois, C.; Whittle, W.; Snelgrove, J.; Malinowski, A.K. COVID-19 and acute coagulopathy in pregnancy. J. Thromb Haemost 2020, 18, 1648–1652. [Google Scholar] [CrossRef]
- Skalska-Świstek, M.; Huras, H.; Jaworowski, A.P.; Świstek, R.; Kołak, M. COVID-19 Infection Complicated by Disseminated Intravascular Coagulation during Pregnancy-Two Cases Report. Diagnostics 2022, 12, 655. [Google Scholar] [CrossRef]
- Mulvey, J.J.; Magro, C.M.; Ma, L.X.; Nuovo, G.J.; Baergen, R.N. Analysis of complement deposition and viral RNA in placentas of COVID-19 patients. Ann. Diagn. Pathol. 2020, 46, 151530. [Google Scholar] [CrossRef]
- Menter, T.; Mertz, K.D.; Jiang, S.; Chen, H.; Monod, C.; Tzankov, A.; Waldvogel, S.; Schulzke, S.M.; Hösli, I.; Bruder, E. Placental Pathology Findings during and after SARS-CoV-2 Infection: Features of Villitis and Malperfusion. Pathobiology 2021, 88, 69–77. [Google Scholar] [CrossRef]
- Shanes, E.D.; Mithal, L.B.; Otero, S.; Azad, H.A.; Miller, E.S.; Goldstein, J.A. Placental Pathology in COVID-19. Am. J. Clin. Pathol. 2020, 154, 23–32. [Google Scholar] [CrossRef]
- Goudarzi, S.; Firouzabadi, F.D.; Mahmoudzadeh, F.; Aminimoghaddam, S. Pulmonary embolism in pregnancy with COVID-19 infection: A case report. Clin. Case Rep. 2021, 9, 1882–1886. [Google Scholar] [CrossRef]
- Kripalani, Y.; Parulekar, L. Pulmonary Embolism in a COVID-19-Positive Primigravida After Caesarean Section Despite Prophylaxis. Eur. J. Case Rep. Intern. Med. 2021, 8, 002684. [Google Scholar] [CrossRef]
- Mongula, J.E.; Frenken, M.W.E.; van Lijnschoten, G.; Arents, N.L.A.; de Wit-Zuurendonk, L.D.; Schimmel-de Kok, A.P.A.; van Runnard Heimel, P.J.; Porath, M.M.; Goossens, S. COVID-19 during pregnancy: Non-reassuring fetal heart rate, placental pathology and coagulopathy. Ultrasound Obs. Gynecol. 2020, 56, 773–776. [Google Scholar] [CrossRef]
- Ahmed, I.; Azhar, A.; Eltaweel, N.; Tan, B.K. First COVID-19 maternal mortality in the UK associated with thrombotic complications. Br. J. Haematol. 2020, 190, e37–e38. [Google Scholar] [CrossRef]
- Marinho, P.S.; da Cunha, A.J.L.A.; Chimelli, L.; Avvad-Portari, E.; Andreiuolo, F.d.M.; de Oliveira-Szejnfeld, P.S.; Mendes, M.A.; Gomes, I.C.; Souza, L.R.Q.; Guimarães, M.Z.; et al. Case Report: SARS-CoV-2 Mother-to-Child Transmission and Fetal Death Associated With Severe Placental Thromboembolism. Front. Med. 2021, 8, 1315. [Google Scholar] [CrossRef]
- Martinelli, I.; Ferrazzi, E.; Ciavarella, A.; Erra, R.; Iurlaro, E.; Ossola, M.; Lombardi, A.; Blasi, F.; Mosca, F.; Peyvandi, F. Pulmonary embolism in a young pregnant woman with COVID-19. Thromb Res. 2020, 191, 36–37. [Google Scholar] [CrossRef]
- Wastnedge, E.A.N.; Reynolds, R.M.; van Boeckel, S.R.; Stock, S.J.; Denison, F.C.; Maybin, J.A.; Critchley, H.O.D. Pregnancy and COVID-19. Physiol. Rev. 2021, 101, 303–318. [Google Scholar] [CrossRef]
- Kadir, R.A.; Kobayashi, T.; Iba, T.; Erez, O.; Thachil, J.; Kazi, S.; Malinowski, A.K.; Othman, M. COVID-19 coagulopathy in pregnancy: Critical review, preliminary recommendations, and ISTH registry-Communication from the ISTH SSC for Women’s Health. J. Thromb Haemost 2020, 18, 3086–3098. [Google Scholar] [CrossRef]
- Gąsecka, A.; Borovac, J.A.; Guerreiro, R.A.; Giustozzi, M.; Parker, W.; Caldeira, D.; Chiva-Blanch, G. Thrombotic Complications in Patients with COVID-19: Pathophysiological Mechanisms, Diagnosis, and Treatment. Cardiovasc. Drugs 2021, 35, 215–229. [Google Scholar] [CrossRef]
- Arnett, S. What We Know about COVID-19 and the Inflammatory Response. 2021. Available online: https://www.drugtargetreview.com/article/85765/what-we-know-about-covid-19-and-the-inflammatory-response/ (accessed on 1 October 2022).
- Lee, C.; Choi, W.J. Overview of COVID-19 inflammatory pathogenesis from the therapeutic perspective. Arch. Pharmacal Res. 2021, 44, 99–116. [Google Scholar] [CrossRef]
- Branchford, B.R.; Carpenter, S.L. The Role of Inflammation in Venous Thromboembolism. Front. Pediatr. 2018, 6, 142. [Google Scholar] [CrossRef]
- Page, E.M.; Ariëns, R.A.S. Mechanisms of thrombosis and cardiovascular complications in COVID-19. Thromb Res. 2021, 200, 1–8. [Google Scholar] [CrossRef]
- What Is Sepsis? Available online: https://www.cdc.gov/sepsis/what-is-sepsis.html#:~:text=Sepsis%20is%20the%20body’s%20extreme,%2C%20skin%2C%20or%20gastrointestinal%20tract (accessed on 1 October 2022).
- Barbara Stepko. Protect Yourself from Sepsis. Available online: https://www.aarp.org/health/conditions-treatments/info-2018/sepsis-prevention-tips.html#:~:text=Sepsis%20is%20a%20complication%20that,bloodstream%20to%20fight%20the%20infection (accessed on 1 October 2022).
- Fabregues, F.; Peñarrubia, J. Assisted reproduction and thromboembolic risk in the COVID-19 pandemic. Reprod. Biomed. Online 2020, 41, 361–364. [Google Scholar] [CrossRef]
- Jevtic, S.D.; Malinowski, A.K.; Othman, M.; Abdul Kadir, R.A. Physician experiences in management of COVID-19-associated coagulopathy in pregnancy: Communication from the ISTH SSC Subcommittee on Women’s Health Issues in Thrombosis and Haemostasis. J. Thromb Haemost 2021, 19, 2539–2545. [Google Scholar] [CrossRef]
- Lorini, F.L.; Di Matteo, M.; Gritti, P.; Grazioli, L.; Benigni, A.; Zacchetti, L.; Bianchi, I.; Fabretti, F.; Longhi, L. Coagulopathy and COVID-19. Eur. Heart J. Suppl. 2021, 23, E95–E98. [Google Scholar] [CrossRef]
- Mackman, N. New insights into the mechanisms of venous thrombosis. J. Clin. Investig. 2012, 122, 2331–2336. [Google Scholar] [CrossRef]
- Resta, L.; Vimercati, A.; Cazzato, G.; Mazzia, G.; Cicinelli, E.; Colagrande, A.; Fanelli, M.; Scarcella, S.V.; Ceci, O.; Rossi, R. SARS-CoV-2 and Placenta: New Insights and Perspectives. Viruses 2021, 13, 723. [Google Scholar] [CrossRef]
- Ko, J.Y.; DeSisto, C.L.; Simeone, R.M.; Ellington, S.; Galang, R.R.; Oduyebo, T.; Gilboa, S.M.; Lavery, A.M.; Gundlapalli, A.V.; Shapiro-Mendoza, C.K. Adverse Pregnancy Outcomes, Maternal Complications, and Severe Illness Among US Delivery Hospitalizations With and Without a Coronavirus Disease 2019 (COVID-19) Diagnosis. Clin. Infect. Dis. 2021, 73, S24–S31. [Google Scholar] [CrossRef]
- Levitan, D.; London, V.; McLaren, R.A.; Mann, J.D.; Cheng, K.; Silver, M.; Balhotra, K.S.; McCalla, S.; Loukeris, K. Histologic and Immunohistochemical Evaluation of 65 Placentas From Women With Polymerase Chain Reaction-Proven Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. Arch. Pathol. Lab. Med. 2021, 145, 648–656. [Google Scholar] [CrossRef]
- Zhang, P.; Salafia, C.; Heyman, T.; Salafia, C.; Lederman, S.; Dygulska, B. Detection of severe acute respiratory syndrome coronavirus 2 in placentas with pathology and vertical transmission. Am. J. Obstet. Gynecol. MFM 2020, 2, 100197. [Google Scholar] [CrossRef]
- What Is Venous Thromboembolism? Available online: https://www.cdc.gov/ncbddd/dvt/facts.html (accessed on 1 October 2022).
- Wang, Y.; Liang, X.; Wang, H.; Li, L.; Xiong, G.; Mi, L. A considerable asymptomatic proportion and thromboembolism risk of pregnant women with COVID-19 infection in Wuhan, China. J. Perinat. Med. 2021, 49, 237–240. [Google Scholar] [CrossRef]
- Klovaite, J.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Benn, M. Elevated fibrinogen levels are associated with risk of pulmonary embolism, but not with deep venous thrombosis. Am. J. Respir. Crit. Care Med. 2013, 187, 286–293. [Google Scholar] [CrossRef]
- VTE Clinical Practice Guideline: Prevention and Treatment of Venous Thromboembolism. 2013. Available online: https://www.moh.gov.my/moh/attachments/9005.pdf (accessed on 1 October 2022).
- Thachil, J.; Tang, N.; Gando, S.; Falanga, A.; Cattaneo, M.; Levi, M.; Clark, C.; Iba, T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb Haemost 2020, 18, 1023–1026. [Google Scholar] [CrossRef]
- Spyropoulos, A.C.; Levy, J.H.; Ageno, W.; Connors, J.M.; Hunt, B.J.; Iba, T.; Levi, M.; Samama, C.M.; Thachil, J.; Giannis, D.; et al. Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J. Thromb Haemost 2020, 18, 1859–1865. [Google Scholar] [CrossRef]
- Simcox, L.E.; Ormesher, L.; Tower, C.; Greer, I.A. Pulmonary thrombo-embolism in pregnancy: Diagnosis and management. Breathe 2015, 11, 282–289. [Google Scholar] [CrossRef]
- Coronavirus Disease 2019 (COVID-19), Treatment Guidelines, National Institutes of Health. 2022. Available online: https://files.covid19treatmentguidelines.nih.gov/guidelines/covid19treatmentguidelines.pdf (accessed on 1 October 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).