Abstract
Spinal surgeons have not yet considered sleep disturbance an area of concern; thus, a comprehensive study investigating the epidemiology of sleep disturbance in patients with degenerative spinal disease is yet to be conducted. This study aimed to fill this research gap by investigating the epidemiology of sleep disturbance in patients who underwent spinal surgery for degenerative spinal disease and identifying the associated risk factors. This nationwide, population-based, cohort study, used data from January 2016 and December 2018 from the Korea Health Insurance Review and Assessment Service database. This study included 106,837 patients older than 19 years who underwent surgery for degenerative spinal disease. Sleep disorder was initially defined as a diagnosis of a sleep disorder made within one year before the index surgery and identified using the International Classification of Diseases, 10th revision, codes F51 and G47 (main analysis). We also investigated the use of sleep medication within 90 days prior to the index surgery, which was the target outcome of the sensitivity analysis. The prevalence of sleep disturbance was precisely investigated according to various factors, including demographics, comorbidities, and spinal region. Logistic regression analysis was performed to identify the independent factors associated with sleep disturbance. The results of the statistical analysis were validated using sensitivity analysis and bootstrap sampling. The prevalence of sleep disorder was 5.5% (n = 5847) in our cohort. During the 90 days before spinal surgery, sleep medication was used for over four weeks in 5.5% (n = 5864) and over eight weeks in 3.8% (n = 4009) of the cohort. Although the prevalence of sleep disturbance differed according to the spinal region, the spinal region was not a significant risk factor for sleep disorder in multivariable analysis. We also identified four groups of independent risk factors: (1) Age, (2) other demographic factors and general comorbidities, (3) neuropsychiatric disorders, and (4) osteoarthritis of the extremities. Our results, including the prevalence rates of sleep disturbance in the entire patient population and the identified risk factors, provide clinicians with a reasonable reference for evaluating sleep disturbance in patients with degenerative spinal disease and future research.
1. Introduction
Sleep plays an essential role in both cognitive and physiologic function [1,2]. Therefore, sleep disturbance can not only have detrimental effects on quality of life, but also potentially cause mental and physical illness, eventually increasing the risk of mortality [3,4]. Sleep disturbance is prevalent globally, and nationwide studies have revealed that more than 20% of the general population suffers from sleep disturbance [5,6,7].
Chronic pain is one of the major risk factors associated with sleep disturbance [8,9], and sleep disturbance has been reported to be prevalent in patients with degenerative joint diseases of the extremities [10,11]. Recent studies have revealed that sleep disturbance is also prevalent in patients with degenerative spinal disease, with a reported prevalence ranging from 11 to 74% [12,13,14,15]. Interestingly, studies have identified that in patients with degenerative spinal disease, the radiologic severity of degeneration is a stronger predictor of sleep disturbance than overall pain intensity [12,13]. In addition, the radiologic indices associated with sleep disturbance differed according to the spinal regions. For example, in patients with lumbar stenosis, sleep disturbance was more associated with foraminal-type stenosis than central-type stenosis [13]. In contrast, in patients with cervical myelopathy, central-type stenosis was more closely associated with sleep disturbance than foraminal-type stenosis [12]. From these results, the authors deduced that the mechanisms of sleep disturbance may differ according to the spinal regions and that sleep disturbance in patients with cervical myelopathy might be caused by the same factors causing sleep disturbance in patients with spinal cord injury, such as symptoms associated with cord injury, including pain, sleep breathing disorder, and sleep movement disorder, as well as inhibition of the neural pathway for endogenous melatonin production passing through the cervical spinal cord.
Considering that the radiologic degree of spinal degeneration is closely associated with sleep disturbance, sleep disturbance is expected to be particularly prevalent in patients who are considering surgical treatment for degenerative spinal disease, which could have influenced their choice to undergo surgical treatment. However, sleep disturbance has hitherto not been a matter of concern to spinal surgeons, and few studies have investigated the epidemiology of sleep disturbance in patients who underwent spinal surgery. Although several recent studies have been conducted for this purpose, they had the following limitations [12,13,14,16,17]. First, most of these studies are single-center studies with a limited number of patients. Thus, the prevalence rates of sleep disturbance and the estimates for their risk factors can be biased, reflecting the skewness of their study samples. Second, because of the small sample size, a comprehensive epidemiologic analysis including all spinal regions and considering various morbidities that are prevalent in patients with degenerative spinal disease could not be performed. This information would be very useful not only for clinicians, but also for researchers to understand the etiology or mechanisms of sleep disturbance in patients with degenerative spinal disease.
Our study has two distinct research purposes. First, by using a nationwide database that included the entire population, we aimed to investigate the epidemiology of sleep disturbance in patients who underwent spinal surgery for degenerative spinal disease. Based on the large dataset, the epidemiology of sleep disturbance was precisely investigated according to various clinical profiles, including demographics, various comorbidities, and spinal regions. We particularly focused on investigating the prevalence of sleep disturbance according to spinal regions, which has not been reported in previous studies due to the limited number of cases. Second, using this information, we attempted to identify independent risk factors for their sleep disturbance.
2. Patients and Methods
2.1. Database
In this nationwide population-based cohort study, data were obtained from the Korea Health Insurance Review and Assessment Service (HIRA) database. The HIRA database contains all inpatient and outpatient data from hospitals and community clinics in Korea, allowing for a nationwide cohort study that includes the entire population. Diagnostic codes were assigned according to the modified version of the 10th revision of the International Classification of Diseases (ICD-10) and the seventh revision of the Korean Classification of Diseases. Drug use under diagnosis was identified using anatomical therapeutic chemical (ATC) codes and the HIRA general name codes. This study was approved by the Institutional Review Board of our hospital (IRB No. 2020-03-009-001).
2.2. Study Patients
We included patients aged >19 years who underwent surgical treatment (index surgery) for degenerative spinal disease between 1 January 2016 and 31 December 2018 (Figure 1). Degenerative spinal diseases were identified using the following codes: Spinal stenosis (M48.0), spondylolisthesis (M43.1), spondylolysis (M43.0), other spondylosis (M47.1 and M47.2), and cervical disc disorder (M50).
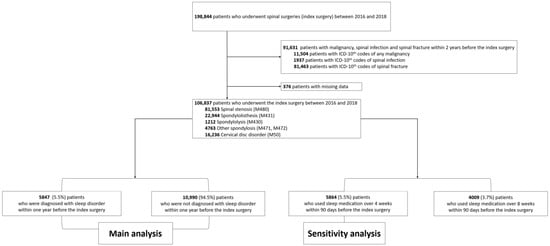
Figure 1.
Enrollment of study patients.
The spinal region of surgical treatment was identified using the following electronic data interchange codes: Cervical surgery including cervical decompressive (N2491, N2492, N0491, N1491, N1497, N2497) and fusion (N2461, N0464, N2463, N2467, N2468, N0467, N2469) surgery; thoracic surgery including thoracic decompressive (N1492, N1498, N2498) and fusion surgery (N0465, N2464, N2465, N2466, N0468), and lumbar surgery including lumbar decompressive (N0492, N1493, N1499, N2499) and fusion (N0466, N1466, N0469, N1460, N1469, N2470) surgery. We excluded patients who were treated under the ICD-10 codes of spinal infection (A18.00, M46, M49, G06, and T814), spine fractures (S1, S2, S3, T02.0, T02.1, T02.7, T08, T09, T91, M48.3, M48.4, and M48.5), or malignancy (C) within two years before the index surgery (Figure 1).
2.3. Definitions of Sleep Disturbance
Sleep disturbance in the cohort was identified using the following two methods (Figure 2). First, sleep disturbance was primarily defined as a diagnosis of sleep disorder within one year before the index surgery. Preoperative sleep disorder was identified using the following diagnostic codes: Nonorganic sleep disorders (F51), and sleep disorders (G47). This was then used as the target outcome in the main analysis. Second, in the sensitivity analysis performed to internally validate our results, sleep disturbance was additionally defined by the use of sleep medication during the 90 days before the index surgery. Sleep medication was defined as drugs currently available for insomnia approved by the Korean Food and Drug Administration, including flurazepam, triazolam, flunitrazepam, brotizolam, zolpidem, eszopiclone, doxepin, doxylamine, and diphenhydramine [18]. Among them, antihistamines, including doxylamine and diphenhydramine, were excluded. The ATC and HIRA general name codes for sleep medication are presented in Supplementary Table S1. Data regarding preoperative sleep medication were used as the target outcome in the sensitivity analysis.
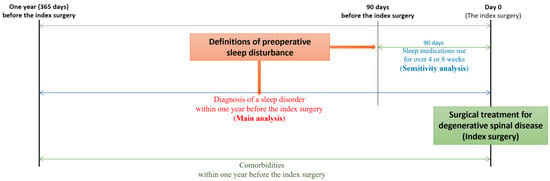
Figure 2.
Definitions of sleep disturbance in the main and sensitivity analyses. The term “sleep disorder” has been used when sleep problems were identified using International Classification of Diseases, tenth revision (ICD-10) codes alone. The term “sleep disturbance” has been used when sleep problems were identified using the following two criteria: Diagnosis of a sleep disorder using ICD-10 codes and the use of sleep medication.
2.4. Factors Associated with Sleep Disturbance
Demographic data at the time of surgery were retrieved. Medical conditions diagnosed in the year before the index surgery were identified using ICD-10 codes (Supplementary Table S2) and evaluated using the Charlson comorbidity index (CCI) [19,20,21]. We also investigated neuropsychiatric disorders that were possibly associated with sleep disturbance using ICD-10 codes (Supplementary Table S2). The diagnosis of depression was confirmed using the ATC codes for the use of antidepressants (N06A, Supplementary Table S3).
We also evaluated osteoarthritis of the extremities using a validated method in our database [22]. Patients with osteoarthritis of the extremities were identified using the ICD-10 codes for osteoarthritis (M15 to M19) with corresponding radiographs of the extremities. The HIRA electronic data interchange codes for X-rays of the extremities are presented in Supplementary Table S4.
2.5. Statistical Analysis
Data are reported as the mean ± standard deviation for numerical variables, and as numbers and frequencies (%) for categorical variables. The prevalence of sleep disturbance was precisely presented according to the factors associated with sleep disturbance and the spinal regions. For the main analysis, sleep disturbance, defined as the diagnosis of a sleep disorder within one year before the index surgery, was chosen as the dependent variable. Logistic regression analysis was performed to identify independent factors associated with sleep disturbance, with adjustment for variables identified to be significant in the univariable analysis (p < 0.05).
Our statistical model was validated using the following procedures. First, a sensitivity analysis was performed to validate risk factors. Sleep disturbance was defined according to the use of sleep medication during the 90 days before the index surgery and was used as the dependent variable for the sensitivity analysis. Second, all estimates from the main and sensitivity analyses were validated using the bootstrap method. All estimates were internally validated with relative bias based on 1000 bootstrapped samples. Relative bias was estimated as the difference between the mean bootstrapped regression coefficient estimates and the mean parameter estimates of multivariable model divided by the mean parameter estimates of the multivariable model.
Multicollinearity between covariates was tested using a variance inflation factor. Data extraction and statistical analysis were performed using the SAS Enterprise Guide 6.1 (SAS Institute, Cary, NC, USA).
3. Results
Between 2016 and 2018, 198,844 patients underwent spinal surgery (index surgery) for degenerative spinal disease (Figure 1). Among them, we excluded patients who were treated under the ICD-10 codes of malignancy (n = 11,504), spinal infection (n = 1937), and spinal fracture (n = 81,463) within two years before the index surgery, and those who had missing data (n = 376).
A total of 106,837 patients were included in this study, with a mean age of 62.9 years and 52% (n = 55,595) being women.
3.1. Annual Prevalence of Sleep Disturbance According to the Three Definitions
Among the 106,837 patients, sleep disorders were diagnosed within one year before the index surgery in 5.5% (n = 5847, Table 1). During the 90 days before spinal surgery, sleep medication was used for over four weeks in 5.5% of the cohort (n = 5864) and over eight weeks in 3.8% (n = 4009) of the cohort. During the study period, the number of patients with preoperative sleep disorders and those who used sleep medications continuously increased (Table 1).

Table 1.
Annual prevalence of sleep disturbance according to the three definitions.
3.2. Prevalence of Sleep Disturbance According to the Baseline Characteristics and Comorbidities
Sleep disorders were common in patients of older age, female sex, urban residence, and surgery at a tertiary hospital (Table 2). The difference was most pronounced by age, and patients aged over 80 years had approximately three-fold higher chances of having sleep disturbance than those between 20 and 49 years (8.8% vs. 2.7%).

Table 2.
Prevalence of sleep disturbance according to the baseline characteristics.
Patients with a sleep disorder had a slightly higher CCI score than those without it (1.56 ± 1.44 vs. 1.12 ± 1.26). However, the prevalence of sleep disorders did not show an increasing trend according to categorized CCI scores (Table 3). Conversely, patients with CCI scores ≥ 6 points had approximately one-half lower chances of having sleep disturbance than those with CCI scores ≤ 2 points (2.9% vs. 6.0%). Patients with specific comorbidity had a higher prevalence of sleep disorder than the overall prevalence (5.5%, Table 3). Sleep disorder was especially frequent in patients with neuropsychiatric comorbidities, including depressive disorder (11.8%), dementia (12.0%), Parkinson’s disease (11.4%), migraine (11.9%), tension-type headache (11.4%), and other-type headache (10.9%). Diagnosis of sleep disorder was also frequent in patients with concurrent osteoarthritis of the extremities, especially in the ankle (9.1%), wrist (8.1%), and shoulder (7.9%).

Table 3.
Prevalence of sleep disturbance according to comorbidities.
3.3. Prevalence of Sleep Disturbance According to Spinal Regions
The prevalence of sleep disorders was 6.9%, 5.7%, and 4.4% in patients with thoracic, lumbar, and cervical spinal lesions, respectively (Figure 3). Prevalence rates of sleep disturbance defined by the use of sleep medication were also concordant with the proportions of those who were diagnosed with a sleep disorder, and the patients who underwent thoracic spine surgery consistently showed the highest prevalence rates according to all three definitions of sleep disturbance (Figure 3).
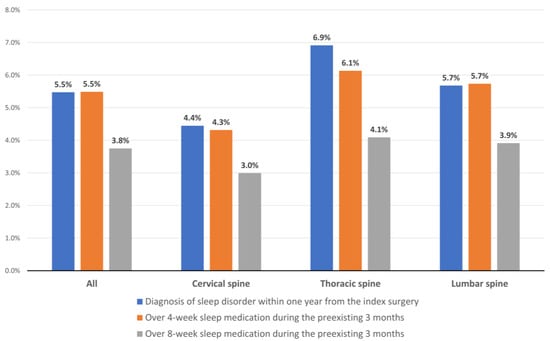
Figure 3.
Prevalence of sleep disturbance by spinal region according to the three definitions.
3.4. Prevalence of Sleep Disturbance According to Concurrent Neuropsychiatric Disorders and Osteoarthritis of Extremities
The two most common types of concurrent neuropsychiatric disorders in our cohort were depressive disorder (21.8%, n = 23,921) and cerebrovascular disease (8.9%, n = 9502; Table 3), which were more common in patients with thoracic or lumbar lesions (Table 4). The prevalence of the three types of sleep disturbance according to the spinal region and concurrent neuropsychiatric disorders are presented in Table 4. The prevalence of sleep disorder in patients with a specific neuropsychiatric disorder was higher in those with a lumbar lesion than in those with a cervical lesion.

Table 4.
Prevalence of sleep disturbance according to spinal regions and concurrent neuropsychiatric disorders.
The three most common regions of concurrent osteoarthritis in our cohort were the knee (22.8%, n = 24,338), shoulder (8.0%, n = 8503), and hip (6.6%, n = 7104; Table 3). Osteoarthritis of the upper extremities was the most common in patients with a cervical lesion, and that of the lower extremities was common in patients with thoracic or lumbar lesions (Table 5). We present the prevalence of three types of sleep disturbance according to spinal region and concurrent osteoarthritis of the extremities in Table 4. The prevalence of sleep disorder in patients with concurrent osteoarthritis of the upper extremities was higher in those with lumbar lesions than in those with cervical lesions.

Table 5.
Prevalence of sleep disturbance according to concurrent osteoarthritis of extremities.
3.5. Risk Factors for Sleep Disorder: Main Analysis
Multivariable analysis identified the following variables as significant risk factors for sleep disturbance in patients who underwent surgical treatment for degenerative spinal diseases: (Table 6): Age of 50–69 years (odds ratio, OR [95% confidence interval] = 1.40 [1.25–1.57]), age of 70–79 years (OR = 1.80 [1.60–2.03]), age over 80 years (OR = 2.22 [1.92–2.58]), female sex (OR = 1.14 [1.07–1.21]), urban residence (OR = 1.18 [1.09–1.27]), surgery at a tertiary hospital (OR = 1.08 [1.00–1.16]), peripheral vascular disease (OR = 1.22 [1.13–1.32]), chronic pulmonary disease (OR = 1.31 [1.23–1.40]), peptic ulcer disease (OR = 1.26 [1.17–1.35]), mild liver disease (OR = 1.27 [1.14–1.41]), depressive disorder (OR = 2.86 [2.70–3.02]), cerebrovascular disease (OR = 1.12 [1.10–1.20]), dementia (OR = 1.49 [1.26–1.78]), Parkinson’s disease’ (OR = 1.51 [1.22–1.88]), migraine (OR = 1.61 [1.44–1.82]), other-type headache (OR = 1.25 [1.03–1.52]), shoulder arthritis (OR = 1.15 [1.06–1.26]), knee arthritis (OR = 1.11 [1.04–1.18]), and ankle arthritis (OR = 1.32 [1.17–1.48]). All the results from the main statistical analysis are presented in Supplementary Table S5.

Table 6.
Risk factors for sleep disorder: Main analysis.
3.6. Validation of Risk Factors: Sensitivity Analysis
During the study period, the annual prevalence of sleep disorder in the year before the index surgery (main analysis) was similar to the proportions of patients who used sleep medication for over four weeks during the 90 days before the index surgery (Table 1): 5.3% vs. 5.2% in 2016, 5.4% vs. 5.4% in 2017, and 5.8% vs. 5.8% in 2018. Therefore, the target outcome for the sensitivity analysis was determined as the use of sleep medication for over four weeks during the 90 days before the index surgery. Except for region of residence and other-type headaches, most variables in the main analysis remained significant in the sensitivity analysis (Table 7). In addition, congestive heart failure, uncomplicated diabetes, and renal disease, including end-stage renal disease, were newly identified as significant variables in the sensitivity analysis. All the results from the sensitivity analysis are presented in Supplementary Table S6.

Table 7.
Risk factors for over 4-week sleep medication during the preoperative 90 days: Sensitivity analysis.
3.7. Validation of Estimates: Bootstrap Sampling
In the main analysis, the relative bias of the estimates for the risk factors was very low at between −4.45 and 2.21%, except for that of cerebrovascular disease (−16%). In the sensitivity analysis, the relative bias of the estimates was also very low between −5.13 and 6.99%. Bootstrap-adjusted odds ratios and 95% confidence intervals for the multivariable model are also displayed in Figure 4 (main analysis) and Figure 5 (sensitivity analysis). Multicollinearity among covariates was low, and all variance inflation factors were less than 1.9.
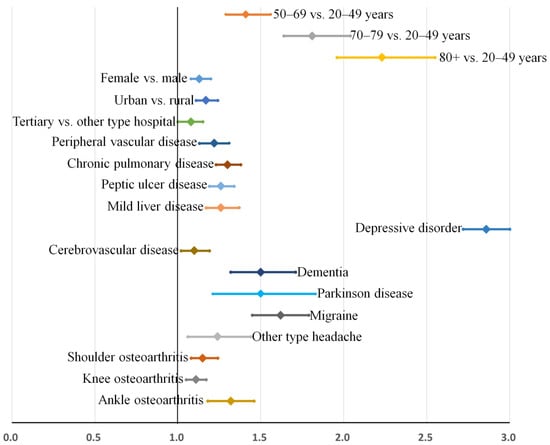
Figure 4.
Risk factors for sleep disorder (main analysis). Bootstrap-adjusted odds ratios and their 95% confidence intervals have been presented. Risk factors can be categorized into four groups: (1) Age, (2) other demographic factors and general comorbidities, (3) neuropsychiatric disorders, and (4) osteoarthritis of the extremities.
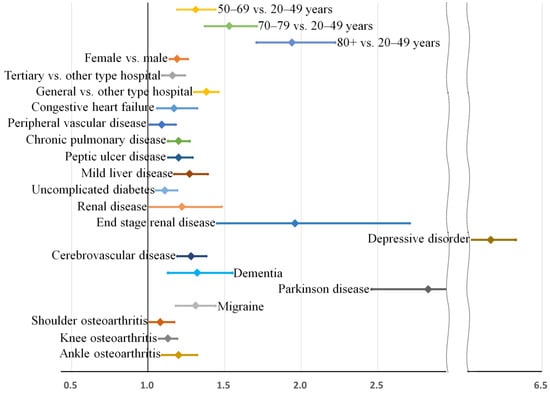
Figure 5.
Risk factors for sleep medication use for over 8 weeks during the preoperative 90 days (subgroup analysis). Bootstrap-adjusted odds ratios and their 95% confidence intervals have been presented. Risk factors can be categorized into four groups: (1) Age, (2) other demographic factors and general comorbidities, (3) neuropsychiatric disorders, and (4) osteoarthritis of the extremities.
4. Discussions
To the best of our knowledge, this is the largest study to investigate the epidemiology of preoperative sleep disturbance in patients who underwent surgery for degenerative spinal disease. Among the 106,837 patients, the prevalence of sleep disorder was 5.5% (n = 5847), and during the 90 days before the spinal surgery, sleep medication was used over four weeks in 5.5% of the cohort (n = 5864) and over eight weeks in 3.8% (n = 4009) of the cohort. The prevalence of sleep disturbance differed according to the spinal regions, and sleep disorder was present in 6.9%, 5.7%, and 4.4% of patients with thoracic, lumbar, and cervical lesions, respectively. However, the spinal region was not a significant risk factor for sleep disorders in the multivariable analysis (Supplementary Tables S5 and S6). The presence of sleep disorder in patients who underwent surgery for degenerative spinal disease was significantly associated with the following factors: Older age; female sex; urban residence; surgery at a tertiary hospital; general comorbidities, including peripheral vascular disease, chronic pulmonary disease, peptic ulcer disease, and mild liver disease; neuropsychiatric disorders, including depressive disorder, cerebrovascular disease, dementia, Parkinson’s disease, migraine, and other-type headache; and arthritis of the shoulder, knee, and ankle joints.
Compared with the prevalence of sleep disturbance in recent studies in the general population (1.6 to 18.6%) [23], and in patients with degenerative spinal disease (11 to 74%) [12,13,14,15,16,17], the prevalence of sleep disturbance in our cohort (3.8 to 5.5%, Table 3) is quite low. This difference results from the different methods used to evaluate sleep disturbance. Most previous studies used self-administered questionnaire-based surveys without objective clinical evidence to evaluate sleep disturbance, and the prevalence could have been overestimated. In contrast, in our study, sleep disturbance was only defined as present when the sleep disorder was diagnosed by doctors after a hospital visit or when sleep medication was prescribed for a sufficient period. Therefore, the prevalence of sleep disturbance in our cohort could have been underestimated.
The core results of our analysis identifying the independent factors associated with sleep disturbance are presented in Figure 4. In Figure 4, the bootstrap-adjusted ORs and 95% confidence intervals of individual factors can be evidently divided into four groups: (1) Age, (2) other demographic factors and general comorbidities, (3) neuropsychiatric disorders, and (4) osteoarthritis of the extremities. While older age is a strong risk factor for sleep disturbance in our cohort, other demographic variables including sex and region of residence, various general comorbidities, and osteoarthritis of the extremities did not show comparable risks for sleep disturbance (all their adjusted ORs are below 1.4). In contrast, most neuropsychiatric disorders showed higher ORs for sleep disturbance than general comorbidities, and depressive disorder was the most prominent risk factor for sleep disturbance (OR = 2.86 [2.72–3.00]).
Interestingly, the prevalence of sleep disturbance differed according to the location of the spinal lesion (Figure 3), and univariable analysis identified significant differences according to spinal regions, especially between the cervical and lumbar regions (p < 0.001, Supplementary Table S5). However, the location of the spinal lesion was not an independent risk factor for sleep disturbance in the multivariable analysis (Table 6 and Table 7). Based on the results of our study, we suggest that regional differences in the prevalence of sleep disturbance in the unadjusted analysis (Figure 3 and Supplementary Table S5) result from regional differences in factors associated with sleep disturbance, such as neuropsychiatric disorders (Table 4) and degenerative joint diseases of the extremities (Table 5).
The major advantage of our study is that we could precisely present the prevalence of sleep disturbance according to four groups of factors (Table 2, Table 3, Table 4 and Table 5). Our database represents the entire Korean population, and these prevalence rates can be used as the base rates for sleep disturbance in patients with specific risk factors. It is well known that the accuracy of prediction by a simple ‘base rate’ of the entire population can be comparable to that obtained from a complex statistical analysis [24]. Although our prediction model (Table 6 and Table 7) for sleep disturbance could be inevitably biased by unknown confounders due to the study’s limitations, our prevalence rates of sleep disturbance presented by four groups of factors can be used as a reasonable source of the base rates.
This study has some limitations. First, the HIRA database is a claims database not originally designed for clinical research. Although we used validated data retrieval methods for the HIRA database, possible discrepancies between the diagnostic codes in the database and the actual diseases may be potential sources of bias. However, the HIRA system is based on our compulsory national health insurance system, and the control policy for high-revenue spinal surgeries has been the object of priority. Therefore, therapeutic information about drug and device use, as well as precise surgical approaches, is thoroughly reviewed by government officials and is thus considered very accurate. Second, information possibly related to sleep disturbance, including the radiologic degree of spinal degeneration such as disc degeneration or canal stenosis, or the degree of neurological impairment, could not be included in the study. In particular, information regarding the radiologic degree or types of degeneration could have influenced our results as a confounder [12,13], although most patients who underwent surgical treatment have an end-stage degenerative spinal disease. To reduce the influence of such unknown confounders, we performed a two-step validation procedure, and the results were consistent. Third, we could not include patients with degenerative spinal deformities because of the limited data capacity for analysis. Finally, we particularly focused on investigating the sleep disturbance according to spinal regions, and multivariable analysis showed that the prevalence of sleep disturbance was not significantly different among spinal regions. However, due to the lack of important information, including the presence of various symptoms or signs depending on spinal regions and their severity, our results could be biased. Previous studies have suggested different mechanisms of sleep disturbance according to spinal regions, and further studies including such important clinical information would be interesting and helpful to understand the actual mechanisms of sleep disturbance in patients with degenerative spinal disease.
In conclusion, our population-based study using a nationwide database identified that the prevalence of sleep disturbance in patients undergoing surgery for degenerative spinal disease was 5.5% (5847 of 106,837 patients). Although the prevalence of sleep disturbance differed according to spinal regions, the spinal region was not a significant risk factor for sleep disorder in the multivariable analysis. In addition, we identified four groups of independent risk factors: (1) Age, (2) other demographic factors and general comorbidities, (3) neuropsychiatric disorders, and (4) osteoarthritis of the extremities. Our results, including the prevalence rates of sleep disturbance based on the entire population and the identified risk factors, provide clinicians with a reasonable reference for evaluating sleep disturbance in patients with degenerative spinal diseases and future research.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11195932/s1, Table S1: Types of the used sleep medication; Table S2. ICD-10 codes for comorbidities including Charlson comorbidities index items and scores; Table S3. ATC and HIRA codes for the used antidepressant; Table S4. HIRA codes for the x-rays of the extremities; Table S5. Risk factors for sleep disorder (main analysis): all the results from statistical analysis; Table S6. Risk factors for over 8-week sleep medication during the preoperative 90 days (sensitivity analysis): all the results from statistical analysis.
Author Contributions
Conceptualization, J.K. and T.-H.K.; Data curation, M.S.K.; Formal analysis, J.K.; Investigation, M.S.K.; Methodology, J.K., M.S.K. and T.-H.K.; Resources, M.S.K.; Software, J.K. and M.S.K.; Validation, T.-H.K.; Visualization, T.-H.K.; Writing—original draft, J.K.; Writing–review & editing, T.-H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of our hospital (IRB No. 2020-03-009-001).
Informed Consent Statement
Patient consent was waived due to the retrospective study design and anonymity of the HIRA database.
Data Availability Statement
The datasets generated for the current study are not publicly available due to Data Protection Laws and Regulations in Korea, but the analyzing results are available from the corresponding authors on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dattilo, M.; Antunes, H.K.; Medeiros, A.; Mônico Neto, M.; Souza, H.S.; Tufik, S.; de Mello, M.T. Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Med. Hypotheses 2011, 77, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Cirelli, C.; Tononi, G. Is sleep essential? PLoS Biol. 2008, 6, e216. [Google Scholar] [CrossRef] [PubMed]
- Luyster, F.S.; Strollo, P.J., Jr.; Zee, P.C.; Walsh, J.K. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- Stranges, S.; Tigbe, W.; Gómez-Olivé, F.X.; Thorogood, M.; Kandala, N.B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef]
- Sutton, D.A.; Moldofsky, H.; Badley, E.M. Insomnia and health problems in Canadians. Sleep 2001, 24, 665–670. [Google Scholar] [CrossRef]
- Hossain, J.L.; Shapiro, C.M. The prevalence, cost implications, and management of sleep disorders: An overview. Sleep Breath 2002, 6, 85–102. [Google Scholar] [CrossRef]
- Burgess, H.J.; Burns, J.W.; Buvanendran, A.; Gupta, R.; Chont, M.; Kennedy, M.; Bruehl, S. Associations between sleep disturbance and chronic pain intensity and function: A test of direct and indirect pathways. Clin. J. Pain 2019, 35, 569–576. [Google Scholar] [CrossRef]
- Onen, S.H.; Onen, F. Chronic medical conditions and sleep in the older adult. Sleep Med. Clin. 2018, 13, 71–79. [Google Scholar] [CrossRef]
- Sasaki, E.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Inoue, R.; Chiba, D.; Okubo, N.; Takahashi, I.; Nakaji, S.; Ishibashi, Y. Nocturnal knee pain increases with the severity of knee osteoarthritis, disturbing patient sleep quality. Arthritis Care Res. 2014, 66, 1027–1032. [Google Scholar] [CrossRef]
- Khazzam, M.S.; Mulligan, E.P.; Brunette-Christiansen, M.; Shirley, Z. Sleep quality in patients with rotator cuff disease. J. Am. Acad. Orthop. Surg. 2018, 26, 215–222. [Google Scholar] [CrossRef]
- Kim, J.; Oh, J.K.; Kim, S.W.; Yee, J.S.; Kim, T.H. Risk factors for sleep disturbance in patients with cervical myelopathy and its clinical significance: A cross-sectional study. Spine J. 2021, 21, 96–104. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.; Kim, S.W.; Oh, J.K.; Park, M.S.; Kim, Y.W.; Kim, T.H. Prevalence of sleep disturbance in patients with lumbar spinal stenosis and analysis of the risk factors. Spine J. 2020, 20, 1239–1247. [Google Scholar] [CrossRef]
- Kim, H.J.; Hong, S.J.; Park, J.H.; Ki, H. Sleep disturbance and its clinical implication in patients with adult spinal deformity: Comparison with lumbar spinal stenosis. Pain Res. Manag. 2020, 2020, 6294151. [Google Scholar] [CrossRef]
- Artner, J.; Cakir, B.; Spiekermann, J.-A.; Kurz, S.; Leucht, F.; Reichel, H.; Lattig, F. Prevalence of sleep deprivation in patients with chronic neck and back pain: A retrospective evaluation of 1016 patients. J. Pain Res. 2013, 6, 1–6. [Google Scholar] [CrossRef]
- Kim, J.; Kim, G.; Kim, S.W.; Oh, J.K.; Park, M.S.; Kim, Y.W.; Kim, T.H. Changes in sleep disturbance in patients with cervical myelopathy: Comparison between surgical treatment and conservative treatment. Spine J. 2021, 21, 586–597. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.H.; Kim, T.H. Improvement of sleep quality after treatment in patients with lumbar spinal stenosis: A prospective comparative study between conservative versus surgical treatment. Sci. Rep. 2020, 10, 14135. [Google Scholar] [CrossRef]
- Choi, H.; Youn, S.; Um, Y.H.; Kim, T.W.; Ju, G.; Lee, H.J.; Lee, C.; Lee, S.D.; Bae, K.; Kim, S.J.; et al. Korean Clinical Practice Guideline for the Diagnosis and Treatment of Insomnia in Adults. Psychiatry Investig. 2020, 17, 1048–1059. [Google Scholar] [CrossRef]
- Kim, J.; Ryu, H.; Kim, T.-H. Early reoperation rates and its risk factors after instrumented spinal fusion surgery for degenerative spinal disease: A nationwide cohort study of 65,355 patients. J. Clin. Med. 2022, 11, 3338. [Google Scholar] [CrossRef]
- Lim, J.S.; Kim, T.-H. Recurrence rates and its associated factors after early spinal instrumentation for pyogenic spondylodiscitis: A nationwide cohort study of 2148 patients. J. Clin. Med. 2022, 11, 3356. [Google Scholar] [CrossRef]
- Kim, J.; Kim, T.-H. Risk factors for postoperative deep infection after instrumented spinal fusion surgeries for degenerative spinal disease: A nationwide cohort study of 194,036 patients. J. Clin. Med. 2022, 11, 778. [Google Scholar] [CrossRef]
- Park, H.-R.; Im, S.; Kim, H.; Jung, S.-Y.; Kim, D.; Jang, E.; Sung, Y.-K.; Cho, S.-K. Validation of algorithms to identify knee osteoarthritis patients in the claims database. Int. J. Rheum. Dis. 2019, 22, 890–896. [Google Scholar] [CrossRef]
- Koyanagi, A.; Stickley, A. The association between sleep problems and psychotic symptoms in the general population: A global perspective. Sleep 2015, 38, 1875–1885. [Google Scholar] [CrossRef]
- Kahneman, D. Thinking, Fast and Slow; Farrar, Straus and Giroux: New York, NY, USA, 2017. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).