Heart Donation and Preservation: Historical Perspectives, Current Technologies, and Future Directions
Abstract
:1. Introduction
2. Historical Aspects of Cardiac Donation
3. Current Methods of Heart Preservation
3.1. Static Cold Storage
3.2. Paragonyx SherpaPak
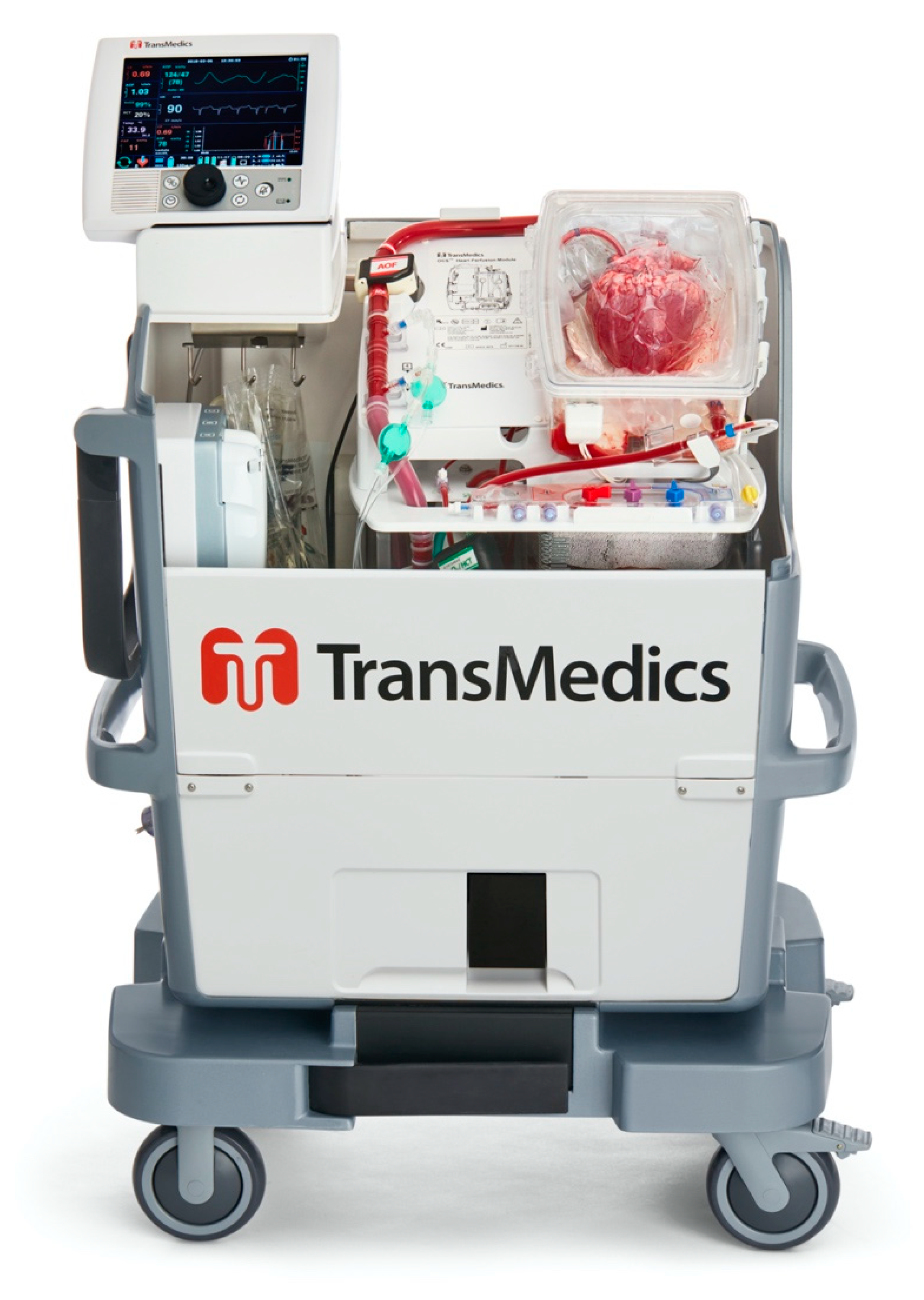
3.3. Transmedics Organ Care System
3.3.1. Setup of the OCS [58,59]
3.3.2. Clinical Usage and Applications
3.4. XVIVO Non-Ischemic Heart Preservation
3.4.1. Device Setup
3.4.2. Clinical Usage and Applications
4. Donation after Circulatory Death
5. Ex Vivo Therapeutic Interventions
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability
Conflicts of Interest
References
- Khush, K.K.; Potena, L.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D.; Hsich, E.; Sadavarte, A.; Singh, T.P.; Zuckermann, A.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult heart transplantation report—2021; Focus on recipient characteristics. J. Heart Lung Transplant. 2021, 40, 1035–1049. [Google Scholar] [CrossRef] [PubMed]
- del Maria Javier, M.F.; Delmo, E.M.J.; Hetzer, R. Evolution of heart transplantation since Barnard’s first. Cardiovasc. Diagn. Ther. 2021, 11, 171. [Google Scholar] [CrossRef] [PubMed]
- UNOS. Organ Transplant Trends. More Transplants than Ever. Available online: https://unos.org/data/transplant-trends/ (accessed on 2 September 2021).
- Vinson, A.J.; Rose, C.; Kiberd, B.A.; Odutayo, A.; Kim, S.J.; Alwayn, I.; Tennankore, K.K. Factors associated with prolonged warm ischemia time among deceased donor kidney transplant recipients. Transplant. Direct 2018, 4, e342. [Google Scholar] [CrossRef] [PubMed]
- Pan, E.T.; Yoeli, D.; Galvan, N.T.N.; Kueht, M.L.; Cotton, R.T.; O’Mahony, C.A.; Goss, J.A.; Rana, A. Cold ischemia time is an important risk factor for post–liver transplant prolonged length of stay. Liver Transplant. 2018, 24, 762–768. [Google Scholar] [CrossRef]
- Rustad, L.A.; Nytrøen, K.; Andreassen, A.; Geiran, O.; Endresen, K.; Gullestad, L.; Aakhus, S.; Amundsen, B.H. Heart transplant systolic and diastolic function is impaired by prolonged pretransplant graft ischaemic time and high donor age: An echocardiographic study. Eur. J. Cardio-Thorac. Surg. 2013, 44, e97–e104. [Google Scholar] [CrossRef]
- Banner, N.R.; Thomas, H.L.; Curnow, E.; Hussey, J.C.; Rogers, C.A.; Bonser, R.S. The importance of cold and warm cardiac ischemia for survival after heart transplantation. Transplantation 2008, 86, 542–547. [Google Scholar] [CrossRef]
- Stehlik, J.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Christie, J.D.; Dipchand, A.I.; Dobbels, F.; Kirk, R.; Rahmel, A.O.; Hertz, M.I. The registry of the international society for heart and lung transplantation: 29th official adult heart transplant report—2012. J. Heart Lung Transplant. 2012, 31, 1052–1064. [Google Scholar] [CrossRef]
- Hess, N.R.; Seese, L.M.; Sultan, I.; Wang, Y.; Hickey, G.W.; Kilic, A. Geographic Disparities in Heart Transplantation Persist under the New Allocation Policy. Clin. Transplant. 2021, 35, ctr.14459. [Google Scholar] [CrossRef]
- Goff, R.R.; Uccellini, K.; Lindblad, K.; Hall, S.; Davies, R.; Farr, M.; Silvestry, S.; Rogers, J.G. A change of heart: Preliminary results of the US 2018 adult heart allocation revision. Am. J. Transplant. 2020, 20, 2781–2790. [Google Scholar] [CrossRef]
- Khush, K.K.; Potena, L.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D.; Hsich, E.; Sadavarte, A.; Singh, T.P.; Zuckermann, A.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: 37th adult heart transplantation report—2020; focus on deceased donor characteristics. J. Heart Lung Transplant. 2020, 39, 1003–1015. [Google Scholar] [CrossRef]
- John, M.M.; Shih, W.; Estevez, D.; Martens, T.P.; Bailey, L.L.; Razzouk, A.J.; Rabkin, D.G. Interaction Between Ischemic Time and Donor Age on Adult Heart Transplant Outcomes in the Modern Era. Ann. Thorac. Surg. 2019, 108, 744–748. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.J.; Chen, J.M.; Sorabella, R.A.; Martens, T.; Garrido, M.; Davies, R.; George, I.; Cheema, F.H.; Mosca, R.S.; Mital, S.; et al. The effect of ischemic time on survival after heart transplantation varies by donor age: An analysis of the United Network for Organ Sharing database. J. Thorac. Cardiovasc. Surg. 2007, 133, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Qin, G.; Jernryd, V.; Sjöberg, T.; Steen, S.; Nilsson, J. Machine Perfusion for Human Heart Preservation: A Systematic Review. Transpl. Int. 2022, 35, 10258. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; MacGowan, G.A.; Ali, S.; Dark, J.H. Ex situ heart perfusion: The past, the present, and the future. J. Heart Lung Transplant. 2021, 40, 69–86. [Google Scholar] [CrossRef]
- Buchanan, E. The operation: A human cardiac transplant: An interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. Author: C N Barnard. S. Afr. Med. J. 2017, 107, 1041–1044. [Google Scholar]
- Stolf, N.A.G. History of heart transplantation: A hard and glorious journey. Braz. J. Cardiovasc. Surg. 2017, 32, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Beecher, H.K. A Definition of Irreversible Coma: Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA 1968, 205, 337–340. [Google Scholar] [CrossRef]
- Sade, R.M. Brain death, cardiac death, and the dead donor rule. JSC Med. Assoc. 2011, 107, 146–149. [Google Scholar]
- Watson, D.C.; A Reitz, B.; A Baumgartner, W.; A Raney, A.; E Oyer, P.; Stinson, E.B.; E Shumway, N. Distant heart procurement for transplantation. Surgery 1979, 86, 56–59. [Google Scholar] [CrossRef]
- Modry, D.L.; E Oyer, P.; Jamieson, S.W.; Stinson, E.B.; Baldwin, J.C.; A Reitz, B.; Dawkins, K.D.; McGregor, C.G.; A Hunt, S.; Moran, M. Cyclosporine in heart and heart-lung transplantation. Can. J. Surg. 1985, 28, 274–280, 282. [Google Scholar]
- Dhital, K.K.; Iyer, A.; Connellan, M.; Chew, H.C.; Gao, L.; Doyle, A.; Hicks, M.; Kumarasinghe, G.; Soto, C.; Dinale, A.; et al. Adult heart transplantation with distant procurement and ex-vivo preservation of donor hearts after circulatory death: A case series. Lancet 2015, 385, 2585–2591. [Google Scholar] [CrossRef]
- Camp, P.C. Heart transplantation: Donor operation for heart and lung transplantation. Oper. Tech. Thorac. Cardiovasc. Surg. 2010, 15, 125–137. [Google Scholar] [CrossRef]
- Buckberg, G.D. Myocardial temperature management during aortic clamping for cardiac surgery: Protection, preoccupation, and perspective. J. Thorac. Cardiovasc. Surg. 1991, 102, 895–903. [Google Scholar] [CrossRef]
- Jahania, M.S.; Sanchez, J.A.; Narayan, P.; Lasley, R.D.; Mentzer, R.M. Heart preservation for transplantation: Principles and strategies. Ann. Thorac. Surg. 1999, 68, 1983–1987. [Google Scholar] [CrossRef]
- Southard, J.H.; Belzer, F.O. Organ preservation. Annu. Rev. Med. 1995, 46, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Enerson, D.M.; Merola, J. Cellular swelling: 3. Effects of hypothermia and addition of low molecular weight dextran on oxygen consumption and electrolyte composition of isolated tissues. Ann. Surg. 1967, 165, 244. [Google Scholar] [CrossRef]
- Bonventre, J.V.; Cheung, J.Y. Effects of metabolic acidosis on viability of cells exposed to anoxia. Am. J. Physiol. Cell Physiol. 1985, 249, C149–C159. [Google Scholar] [CrossRef]
- Salahudeen, A.K.; Huang, H.; Patel, P.; Jenkins, J.K. Mechanism and prevention of cold storage-induced human renal tubular cell injury. Transplantation 2000, 70, 1424–1431. [Google Scholar] [CrossRef]
- Mühlbacher, F.; Langer, F.; Mittermayer, C. Preservation solutions for transplantation. Transplant. Proc. 1999, 31, 2069–2070. [Google Scholar] [CrossRef]
- Demmy, T.L.; Biddle, J.S.; Bennett, L.E.; Walls, J.T.; Schmaltz, R.A.; Curtis, J.J. Organ preservation solutions in heart transplantation—Patterns of usage and related survival. Transplantation 1997, 63, 262–269. [Google Scholar] [CrossRef]
- Minasian, S.M.; Galagudza, M.M.; Dmitriev, Y.V.; Karpov, A.A.; Vlasov, T.D. Preservation of the donor heart: From basic science to clinical studies. Interact. Cardiovasc. Thorac. Surg. 2015, 20, 510–519. [Google Scholar] [CrossRef] [PubMed]
- Heart Brochure | Custodiol HTK. Available online: http://www.custodiol.com/resources/heart-brochure/ (accessed on 4 October 2021).
- CoStorSolTM. Preservation Solutions. Available online: http://www.preservationsolutions.com/products_costorsol.html (accessed on 4 October 2021).
- CELSIOR®—IGL. Available online: https://groupe-igl.com/celsior/ (accessed on 4 October 2021).
- Latchana, N.; Peck, J.R.; Whitson, B.; Black, S.M. Preservation solutions for cardiac and pulmonary donor grafts: A review of the current literature. J. Thorac. Dis. 2014, 6, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Vega, J.D.; Ochsner, J.L.; Jeevanandam, V.; McGiffin, D.C.; McCurry, K.R.; Mentzer, R.M.; Stringham, J.C.; Pierson, R.N.; Frazier, O.; Menkis, A.H.; et al. A multicenter, randomized, controlled trial of celsior for flush and hypothermic storage of cardiac allografts. Ann. Thorac. Surg. 2001, 71, 1442–1447. [Google Scholar] [CrossRef]
- Cannata, A.; Botta, L.; Colombo, T.; Russo, C.F.; Taglieri, C.; Bruschi, G.; Merlanti, B.; Frigerio, M.; Martinelli, L. Does the cardioplegic solution have an effect on early outcomes following heart transplantation? Eur. J. Cardio-Thorac. Surg. 2012, 41, e48–e53. [Google Scholar] [CrossRef] [PubMed]
- Kofler, S.; Bigdeli, A.K.; Kaczmarek, I.; Kellerer, D.; Müller, T.; Schmoeckel, M.; Steinbeck, G.; Überfuhr, P.; Reichart, B.; Meiser, B. Long-term outcomes after 1000 heart transplantations in six different eras of innovation in a single center. Transpl. Int. 2009, 22, 1140–1150. [Google Scholar] [CrossRef] [PubMed]
- George, T.J.; Arnaoutakis, G.J.; Beaty, C.A.; Shah, A.S.; Conte, J.V.; Halushka, M.K. A novel method of measuring cardiac preservation injury demonstrates University of Wisconsin solution is associated with less ischemic necrosis than Celsior in early cardiac allograft biopsy specimens. J. Heart Lung Transplant. 2012, 31, 410–418. [Google Scholar] [CrossRef]
- George, T.J.; Arnaoutakis, G.J.; Baumgartner, W.A.; Shah, A.S.; Conte, J.V. Organ storage with University of Wisconsin solution is associated with improved outcomes after orthotopic heart transplantation. J. Heart Lung Transplant. 2011, 30, 1033–1043. [Google Scholar] [CrossRef]
- Hicks, M.; Hing, A.; Gao, L.; Ryan, J.; Macdonald, P.S. Organ preservation. Methods Mol. Biol. 2006, 333, 331–374. [Google Scholar] [CrossRef]
- Segovia, J.; Cosío, M.D.G.; Barceló, J.M.; Bueno, M.G.; Pavía, P.G.; Burgos, R.; Serrano-Fiz, S.; García-Montero, C.; Castedo, E.; Ugarte, J.; et al. RADIAL: A novel primary graft failure risk score in heart transplantation. J. Heart Lung Transplant. 2011, 30, 644–651. [Google Scholar] [CrossRef]
- Russo, M.J.; Iribarne, A.; Hong, K.N.; Ramlawi, B.; Chen, J.M.; Takayama, H.; Mancini, D.M.; Naka, Y. Factors associated with primary graft failure after heart transplantation. Transplantation 2010, 90, 444–450. [Google Scholar] [CrossRef]
- Mitropoulos, F.A.; Odim, J.; Marelli, D.; Karandikar, K.; Gjertson, D.; Ardehali, A.; Kobashigawa, J.; Laks, H. Outcome of hearts with cold ischemic time greater than 300 minutes. A case-matched study. Eur. J. Cardio-Thorac. Surg. 2005, 28, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; O’Brien, K.; Dardas, T.; Fishbein, D.; Verrier, E.; Stempien-Otero, A.; Cheng, R.; Masri, S.; Buchter, C.; Aldea, G.; et al. Excellent Long-Term Survival with Extended Ischemic Time in Orthotopic Heart Transplantation. J. Heart Lung Transplant. 2014, 33, S117–S118. [Google Scholar] [CrossRef]
- Bernard, M.; Cartoux, C.; Caus, T.; Sciaky, M.; Cozzone, P.J. The Influence of Temperature on Metabolic and Cellular Protection of the Heart during Long-Term Ischemia: A Study Using P-31 Magnetic Resonance Spectroscopy and Biochemical Analyses. Cryobiology 1998, 37, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Tian, G.; Smith, K.E.; Biro, G.P.; Butler, K.W.; Haas, N.; Scott, J.; Anderson, R.; Deslauriers, R. A comparison of UW cold storage solution and St. Thomas’ solution II: A 31P NMR and functional study of isolated porcine hearts. J. Heart Lung Transplant. 1991, 10, 975–985. [Google Scholar] [PubMed]
- Keon, W.J.; Hendry, P.J.; Taichman, G.C.; Mainwood, G.W. Cardiac Transplantation: The Ideal Myocardial Temperature for Graft Transport. Ann. Thorac. Surg. 1988, 46, 337–341. [Google Scholar] [CrossRef]
- Ingemansson, R.; Budrikis, A.; Bolys, R.; Sjöberg, T.; Steen, S. Effect of temperature in long-term preservation of vascular endothelial and smooth muscle function. Ann. Thorac. Surg. 1996, 61, 1413–1417. [Google Scholar] [CrossRef]
- Mankad, P.S.; Slavik, Z.; Yacoub, M. Endothelial dysfunction caused by University of Wisconsin preservation solution in the rat heart: The importance of temperature. J. Thorac. Cardiovasc. Surg. 1992, 104, 1618–1624. [Google Scholar] [CrossRef]
- Horch, D.F.; Mehlitz, T.; Laurich, O.; Abel, A.; Reuter, S.; Pratschke, H.; Neuhaus, P.; Wesslau, C. Organ transport temperature box: Multicenter study on transport temperature of organs. Transplant. Proc. 2002, 34, 2320. [Google Scholar] [CrossRef]
- Naito, N.; Funamoto, M.; Pierson, R.N.; D’Alessandro, D.A. First clinical use of a novel hypothermic storage system for a long-distance donor heart procurement. J. Thorac. Cardiovasc. Surg. 2020, 159, e121–e123. [Google Scholar] [CrossRef]
- Michel, S.G.; LaMuraglia Ii, G.M.; Madariaga, M.L.L.; Anderson, L.M. Innovative cold storage of donor organs using the Paragonix Sherpa PakTM devices. Heart Lung Vessel 2015, 7, 246–255. [Google Scholar]
- Radakovic, D.; Karimli, S.; Penov, K.; Schade, I.; Hamouda, K.; Bening, C.; Leyh, R.G.; Aleksic, I. First clinical experience with the novel cold storage SherpaPakTM system for donor heart transportation. J. Thorac. Dis. 2020, 12, 7227–7235. [Google Scholar] [CrossRef]
- Jacobs, J.; Schroder, J.; Boston, U.; Zuckermann, A. First Report of Pediatric Outcomes from the GUARDIAN Registry: Multi-Center Analysis of Advanced Organ Preservation for Pediatric Recipients. J. Heart Lung Transplant. 2022, 41, S477. [Google Scholar] [CrossRef]
- Hardesty, R.L.; Griffith, B.P. Autoperfusion of the heart and lungs for preservation during distant procurement. J. Thorac. Cardiovasc. Surg. 1987, 93, 11–18. [Google Scholar] [CrossRef]
- Sáez, D.G.; Zych, B.; Sabashnikov, A.; Bowles, C.T.; De Robertis, F.; Mohite, P.N.; Popov, A.-F.; Maunz, O.; Patil, N.P.; Weymann, A.; et al. Evaluation of the organ care system in heart transplantation with an adverse donor/recipient profile. Ann. Thorac. Surg. 2014, 98, 2099–2106. [Google Scholar] [CrossRef]
- Messer, S.; Ardehali, A.; Tsui, S. Normothermic donor heart perfusion: Current clinical experience and the future. Transpl. Int. 2015, 28, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Hamed, A.; Tsui, S.; Huber, J.; Lin, R.; Poggio, E.C.; Ardehali, A. 19: Serum Lactate Is a Highly Sensitive and Specific Predictor of Post Cardiac Transplant Outcomes Using the Organ Care System. J. Heart Lung Transplant. 2009, 28, S71. [Google Scholar] [CrossRef]
- Koerner, M.M.; Ghodsizad, A.; Schulz, U.; Banayosy AEl Koerfer, R.; Tenderich, G. Normothermic ex vivo allograft blood perfusion in clinical heart transplantation. Heart Surg. Forum 2014, 17, 141–145. [Google Scholar] [CrossRef]
- Ardehali, A.; Esmailian, F.; Deng, M.; Soltesz, E.; Hsich, E.; Naka, Y.; Mancini, D.; Camacho, M.; Zucker, M.; Leprince, P.; et al. Ex-vivo perfusion of donor hearts for human heart transplantation (PROCEED II): A prospective, open-label, multicentre, randomised non-inferiority trial. Lancet 2015, 385, 2577–2584. [Google Scholar] [CrossRef]
- Chan, J.L.; Kobashigawa, J.A.; Reich, H.J.; Ramzy, D.; Thottam, M.M.; Yu, Z.; Aintablian, T.L.; Liou, F.; Patel, J.K.; Kittleson, M.M.; et al. Intermediate outcomes with ex-vivo allograft perfusion for heart transplantation. J. Heart Lung Transplant. 2017, 36, 258–263. [Google Scholar] [CrossRef]
- Fleck, T.P.; Ayala, R.; Kroll, J.; Siepe, M.; Schibilsky, D.; Benk, C.; Maier, S.; Reineker, K.; Hoehn, R.; Humburger, F.; et al. Ex Vivo Allograft Perfusion for Complex Pediatric Heart Transplant Recipients. Ann. Thorac. Surg. 2021, 112, 1275–1280. [Google Scholar] [CrossRef]
- Schroder, J.; D’Alessandro, D.; Esmailian, F.; Boeve, T.; Tang, P.; Liao, K.; Wang, I.; Anyanwu, A.; Shah, A.; Mudy, K.; et al. Successful Utilization of Extended Criteria Donor (ECD) Hearts for Transplantation—Results of the OCSTM Heart EXPAND Trial to Evaluate the Effectiveness and Safety of the OCS Heart System to Preserve and Assess ECD Hearts for Transplantation. J. Heart Lung Transplant. 2019, 38, S42. [Google Scholar] [CrossRef]
- Sáez, D.G.; Zych, B.; Mohite, P.N.; Sabashnikov, A.; Patil, N.P.; Popov, A.F.; Zeriouh, M.; Bowles, C.T.; Hards, R.; Hedger, M.; et al. LVAD Bridging to Heart Transplantation with Ex Vivo Allograft Preservation Shows Significantly Improved: Outcomes: A New Standard of Care? J. Heart Lung Transplant. 2015, 34, S95. [Google Scholar] [CrossRef]
- Wong, Y.; Maddicks-Law, J.; Raymond, P.; Davidson, M.; Thomson, B.; Sharma, V.; Javorsky, G.; Prabhu, A. Real World Experience with Transmedics Organ Care System in Cardiac Transplantation with Donor Organs Associated with Marginal Risk Factors. J. Heart Lung Transplant. 2021, 40, S195–S196. [Google Scholar] [CrossRef]
- Wicomb, W.N.; Cooper, D.K.C.; Barnard, C.N. Twenty-four-hour preservation of the pig heart by a portable hypothermic perfusion system. Transplantation 1982, 34, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Wicomb, W.N.; Novitzky, D.; Cooper, D.K.C.; Rose, A.G. Forty-eight hours hypothermic perfusion storage of pig and baboon hearts. J. Surg. Res. 1986, 40, 276–284. [Google Scholar] [CrossRef]
- Wicomb, W.N.; Cooper, D.K.C.; Novitzky, D.; Barnard, C.N.; Med, M.; Causa, H. Cardiac Transplantation Followin Storage of the Donor Heart by a Portable Hypo a ermic Perfusion System. Ann. Thorac. Surg. 1984, 37, 243–248. [Google Scholar] [CrossRef]
- Qin, G.; Wohlfart, B.; Zuo, L.; Hu, J.; Sjöberg, T.; Steen, S. Intact coronary and myocardial functions after 24 hours of non-ischemic heart preservation. Scand. Cardiovasc. J. 2020, 54, 59–65. [Google Scholar] [CrossRef]
- Steen, S.; Paskevicius, A.; Liao, Q.; Sjöberg, T. Safe orthotopic transplantation of hearts harvested 24 hours after brain death and preserved for 24 hours. Scand. Cardiovasc. J. 2016, 50, 193–200. [Google Scholar] [CrossRef]
- Längin, M.; Mayr, T.; Reichart, B.; Michel, S.; Buchholz, S.; Guethoff, S.; Dashkevich, A.; Baehr, A.; Egerer, S.; Bauer, A.; et al. Consistent success in life-supporting porcine cardiac xenotransplantation. Nature 2018, 564, 430–433. [Google Scholar] [CrossRef]
- Längin, M.; Reichart, B.; Steen, S.; Sjöberg, T.; Paskevicius, A.; Liao, Q.; Qin, G.; Mokelke, M.; Mayr, T.; Radan, J.; et al. Cold non-ischemic heart preservation with continuous perfusion prevents early graft failure in orthotopic pig-to-baboon xenotransplantation. Xenotransplantation 2021, 28, e12636. [Google Scholar] [CrossRef]
- Nilsson, J.; Jernryd, V.; Qin, G.; Paskevicius, A.; Metzsch, C.; Sjöberg, T.; Steen, S. A nonrandomized open-label phase 2 trial of nonischemic heart preservation for human heart transplantation. Nat. Commun. 2020, 11, 2976. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, P.; Davis, R.; D’Ovidio, F.; Cantu, E.; Weyant, M.; Camp, P.; Griffith, B. The NOVEL Lung Trial One-Year Outcomes. J. Heart Lung Transplant. 2014, 33, S71–S72. [Google Scholar] [CrossRef]
- Denfield, S.W.; Azeka, E.; Das, B.; Guereta, L.G.; Irving, C.; Kemna, M.; Reinhardt, Z.; Thul, J.; Dipchand, A.I.; Kirk, R.; et al. Pediatric cardiac waitlist mortality—Still too high. Pediatr. Transplant. 2020, 24, e13671. [Google Scholar] [CrossRef]
- Vela, M.M.; Sáez, D.G.; Simon, A.R. Current approaches in retrieval and heart preservation. Ann. Cardiothorac. Surg. 2018, 7, 67–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messer, S.; Page, A.; Axell, R.; Berman, M.; Hernández-Sánchez, J.; Colah, S.; Parizkova, B.; Valchanov, K.; Dunning, J.; Pavlushkov, E.; et al. Outcome after heart transplantation from donation after circulatory-determined death donors. J. Heart Lung Transplant. 2017, 36, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Entwistle, J.W.; Drake, D.H.; Fenton, K.N.; Smith, M.A.; Sade, R.M. Normothermic regional perfusion: Ethical issues in thoracic organ donation. J. Thorac. Cardiovasc. Surg. 2022, 164, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Sáez, D.G.; Bowles, C.T.; Mohite, P.N.; Zych, B.; Maunz, O.; Popov, A.F.; Hurtado, A.; Raj, B.; Rahman-Haley, S.; Banner, N.; et al. Heart transplantation after donor circulatory death in patients bridged to transplant with implantable left ventricular assist devices. J. Heart Lung Transplant. 2016, 35, 1255–1260. [Google Scholar] [CrossRef]
- Messer, S.; Page, A.; Colah, S.; Axell, R.; Parizkova, B.; Tsui, S.; Large, S. Human heart transplantation from donation after circulatory-determined death donors using normothermic regional perfusion and cold storage. J. Heart Lung Transplant. 2018, 37, 865–869. [Google Scholar] [CrossRef]
- Miñambres, E.; Royo-Villanova, M.; Pérez-Redondo, M.; Coll, E.; Villar-García, S.; Canovas, S.J.; Nistal, J.F.; Garrido, I.P.; Gómez-Bueno, M.; Cobo, M.; et al. Spanish experience with heart transplants from controlled donation after the circulatory determination of death using thoraco-abdominal normothermic regional perfusion and cold storage. Am. J. Transplant. 2021, 21, 1597–1602. [Google Scholar] [CrossRef]
- Sánchez-Cámara, S.; Asensio-López, M.C.; Royo-Villanova, M.; Soler, F.; Jara-Rubio, R.; Garrido-Peñalver, J.F.; Pinar, E.; Hernández-Vicente, Á.; Hurtado, J.A.; Lax, A.; et al. Critical warm ischemia time point for cardiac donation after circulatory death. Am. J. Transplant. 2022, 22, 1321–1328. [Google Scholar] [CrossRef]
- Smith, D.E.; Kon, Z.N.; Carillo, J.A.; Chen, S.; Gidea, C.G.; Piper, G.L.; Reyentovich, A.; Montgomery, R.A.; Galloway, A.C.; Moazami, N. Early experience with donation after circulatory death heart transplantation using normothermic regional perfusion in the United States. J. Thorac. Cardiovasc. Surg. 2021. Published online. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.R.; McMaster, W.G.; Rali, A.S.; Rahaman, Z.; Balsara, K.; Absi, T.; Levack, M.; Brinkley, M.; Menachem, J.; Punnoose, L.; et al. Early US experience with cardiac donation after circulatory death (DCD) using normothermic regional perfusion. J. Heart Lung Transplant. 2021, 40, 1408–1418. [Google Scholar] [CrossRef] [PubMed]
- Messer, S.; Cernic, S.; Page, A.; Berman, M.; Kaul, P.; Colah, S.; Ali, J.; Pavlushkov, E.; Baxter, J.; Quigley, R.; et al. A 5-year single-center early experience of heart transplantation from donation after circulatory-determined death donors. J. Heart Lung Transplant. 2020, 39, 1463–1475. [Google Scholar] [CrossRef] [PubMed]
- Nachum, E.; Laurence, C.; Osman, M.; Hogan, J.; Baxter, J.; Quigley, R.; Messer, S.; Large, S.; Kaul, P.; Forsythe, J.; et al. Pediatric Heart Transplantation Following Donation after Circulatory Death, Distant Procurement and Ex-Situ Perfusion. J. Heart Lung Transplant. 2021, 40, S121. [Google Scholar] [CrossRef]
- Shudo, Y.; Benjamin-Addy, R.; Koyano, T.K.; Hiesinger, W.; Macarthur, J.W.; Woo, Y.J. Donors after circulatory death heart trial. Future Cardiol. 2021, 17, 11–17. [Google Scholar] [CrossRef]
- Suarez-Pierre, A.; Iguidbashian, J.; Stuart, C.; King, R.W.; Cotton, J.; Carroll, A.M.; Cleveland, J.C.; Fullerton, D.A.; Pal, J.D. Appraisal of Donation After Circulatory Death: How Far Could We Expand the Heart Donor Pool? Ann. Thorac. Surg. 2022, 114, 676–682. [Google Scholar] [CrossRef]
- Madan, S.; Saeed, O.; Forest, S.J.; Goldstein, D.J.; Jorde, U.P.; Patel, S.R. Feasibility and Potential Impact of Heart Transplantation from Adult Donors After Circulatory Death. J. Am. Coll. Cardiol. 2022, 79, 148–162. [Google Scholar] [CrossRef]
- Epstein, F.H.; McCord, J.M. Oxygen-derived free radicals in postischemic tissue injury. N. Engl. J. Med. 1985, 312, 159–163. [Google Scholar] [CrossRef]
- Oerlemans, M.I.F.J.; Koudstaal, S.; Chamuleau, S.A.; De Kleijn, D.P.; Doevendans, P.A.; Sluijter, J.P.G. Targeting cell death in the reperfused heart: Pharmacological approaches for cardioprotection. Int. J. Cardiol. 2013, 165, 410–422. [Google Scholar] [CrossRef]
- Wei, J.; Chen, S.; Xue, S.; Zhu, Q.; Liu, S.; Cui, L.; Hua, X.; Wang, Y. Blockade of Inflammation and Apoptosis Pathways by siRNA Prolongs Cold Preservation Time and Protects Donor Hearts in a Porcine Model. Mol. Ther. Nucleic Acids 2017, 9, 428–439. [Google Scholar] [CrossRef]
- Kotani, Y.; Ishino, K.; Osaki, S.; Honjo, O.; Suezawa, T.; Kanki, K.; Yutani, C.; Sano, S. Efficacy of MCI-186, a free-radical scavenger and antioxidant, for resuscitation of nonbeating donor hearts. J. Thorac. Cardiovasc. Surg. 2007, 133, 1626–1632. [Google Scholar] [CrossRef]
- Kung, G.; Konstantinidis, K.; Kitsis, R.N. Programmed Necrosis, Not Apoptosis, in the Heart. Circ. Res. 2011, 108, 1017–1036. [Google Scholar] [CrossRef] [PubMed]
- Qiao, S.; Zhao, W.-J.; Li, H.-Q.; Ao, G.-Z.; An, J.-Z.; Wang, C.; Zhang, H.-L. Necrostatin-1 Analog DIMO Exerts Cardioprotective Effect against Ischemia Reperfusion Injury by Suppressing Necroptosis via Autophagic Pathway in Rats. Pharmacology 2021, 106, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.C.T.; Davidson, S.M.; Lim, S.Y.; Simpkin, J.C.; Hothersall, J.S.; Yellon, D.M. Necrostatin: A potentially novel cardioprotective agent? Cardiovasc. Drugs Ther. 2007, 21, 227–233. [Google Scholar] [CrossRef]
- Yin, R.; Yang, D.; Wu, H.; Huang, K.; Wu, X.; Chen, Y. Intramyocardial injection of vascular endothelial growth factor gene improves cardiac performance and inhibits cardiomyocyte apoptosis. Eur. J. Heart Fail. 2007, 9, 343–351. [Google Scholar] [CrossRef]
- Urayama, K.; Guilini, C.; Messaddeq, N.; Hu, K.; Steenman, M.; Kurose, H.; Ert, G.; Nebigil, C.G. The prokineticin receptor-1 (GPR73) promotes cardiomyocyte survival and angiogenesis. FASEB J. 2007, 21, 2980–2993. [Google Scholar] [CrossRef]
- Hung, S.C.; Pochampally, R.R.; Chen, S.C.; Hsu, S.C.; Prockop, D.J. Angiogenic effects of human multipotent stromal cell conditioned medium activate the PI3K-Akt pathway in hypoxic endothelial cells to inhibit apoptosis, increase survival, and stimulate angiogenesis. Stem Cells 2007, 25, 2363–2370. [Google Scholar] [CrossRef]


| Component (g/L) | UW | Celsior | HTK |
|---|---|---|---|
| Pentafraction | 50 | - | - |
| Lactobionic Acid | 35.83 | 28.664 | - |
| Potassium Phosphate monobasic | 3.4 | - | - |
| Magnesium Sulfate heptahydrate | 1.23 | - | - |
| Raffinose pentahydrate | 17.83 | - | - |
| Adenosine | 1.34 | - | - |
| Allopurinol | 0.136 | - | - |
| Glutathione | 0.922 | 0.921 | - |
| Potassium Hydroxide | 5.61 | - | |
| Mannitol | - | 10.930 | 5.4651 |
| Glutamic Acid | - | 2.942 | - |
| Sodium Hydroxide | Adjust to pH 7.4 | 4.000 | - |
| Calcium chloride dihydrate | - | 0.037 | 0.0022 |
| Potassium chloride | - | 1.118 | 0.6710 |
| Magnesium chloride hexahydrate | - | 2.642 | 0.8132 |
| Histidine | - | 4.650 | 27.9289 |
| Histidine monohydrochloride monohydrate | - | - | 3.7733 |
| Hydrochloric acid | Adjust to pH 7.4 | - | - |
| Sodium chloride | - | - | 0.8766 |
| Potassium hydrogen 2-ketoglutarate | - | - | 0.1842 |
| Tryptophan | - | - | 0.4085 |
| Physical properties | |||
| pH | 7.4 | 7.3 | 7.2 |
| Osmolarity (mosmol/kg) | 320 | 320 | 310 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hess, N.R.; Ziegler, L.A.; Kaczorowski, D.J. Heart Donation and Preservation: Historical Perspectives, Current Technologies, and Future Directions. J. Clin. Med. 2022, 11, 5762. https://doi.org/10.3390/jcm11195762
Hess NR, Ziegler LA, Kaczorowski DJ. Heart Donation and Preservation: Historical Perspectives, Current Technologies, and Future Directions. Journal of Clinical Medicine. 2022; 11(19):5762. https://doi.org/10.3390/jcm11195762
Chicago/Turabian StyleHess, Nicholas R., Luke A. Ziegler, and David J. Kaczorowski. 2022. "Heart Donation and Preservation: Historical Perspectives, Current Technologies, and Future Directions" Journal of Clinical Medicine 11, no. 19: 5762. https://doi.org/10.3390/jcm11195762
APA StyleHess, N. R., Ziegler, L. A., & Kaczorowski, D. J. (2022). Heart Donation and Preservation: Historical Perspectives, Current Technologies, and Future Directions. Journal of Clinical Medicine, 11(19), 5762. https://doi.org/10.3390/jcm11195762





