Complications of Long Head of the Biceps Tenotomy in Association with Arthroscopic Rotator Cuff Repair: Risk Factors and Influence on Outcomes
Abstract
:1. Introduction
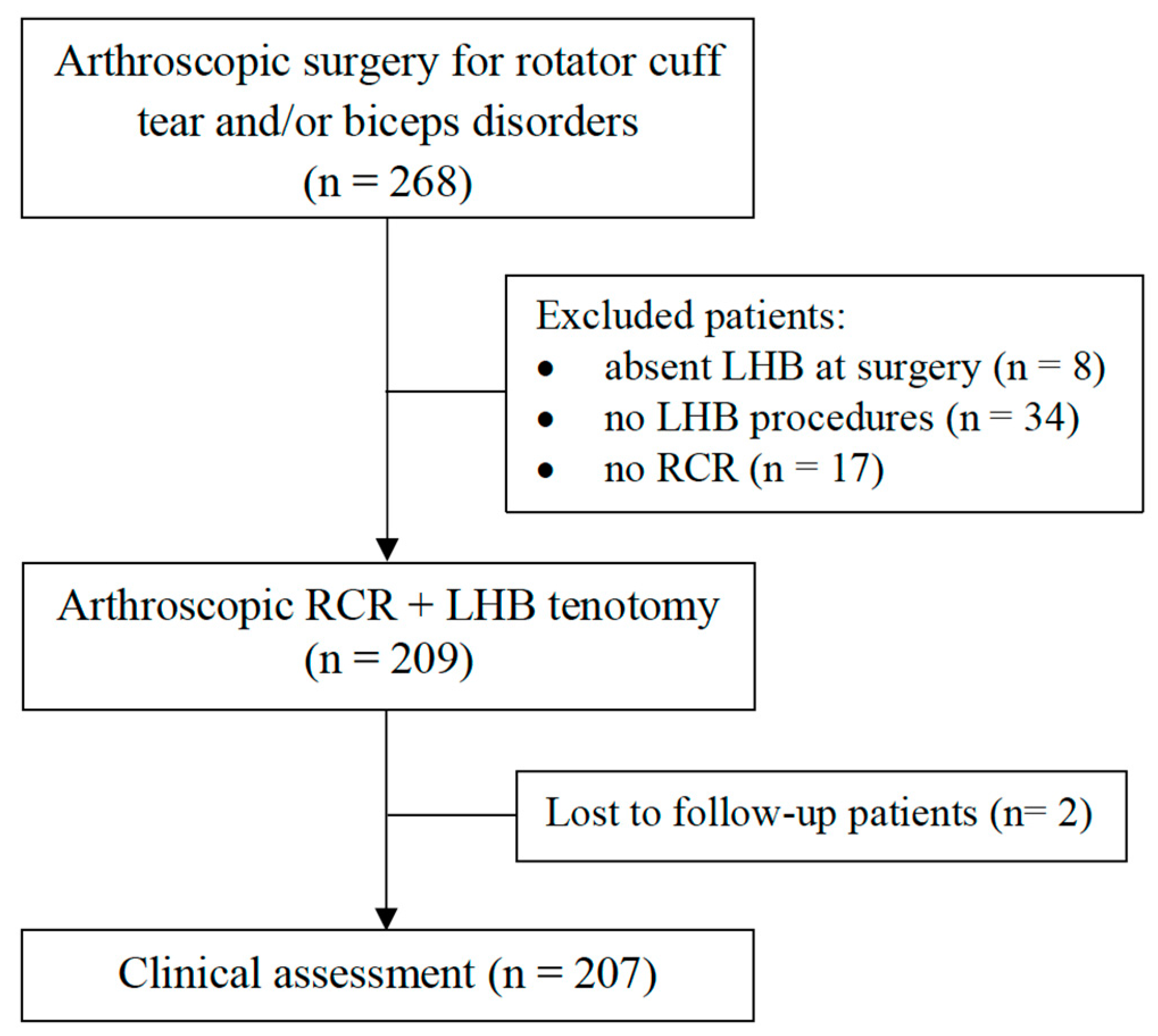
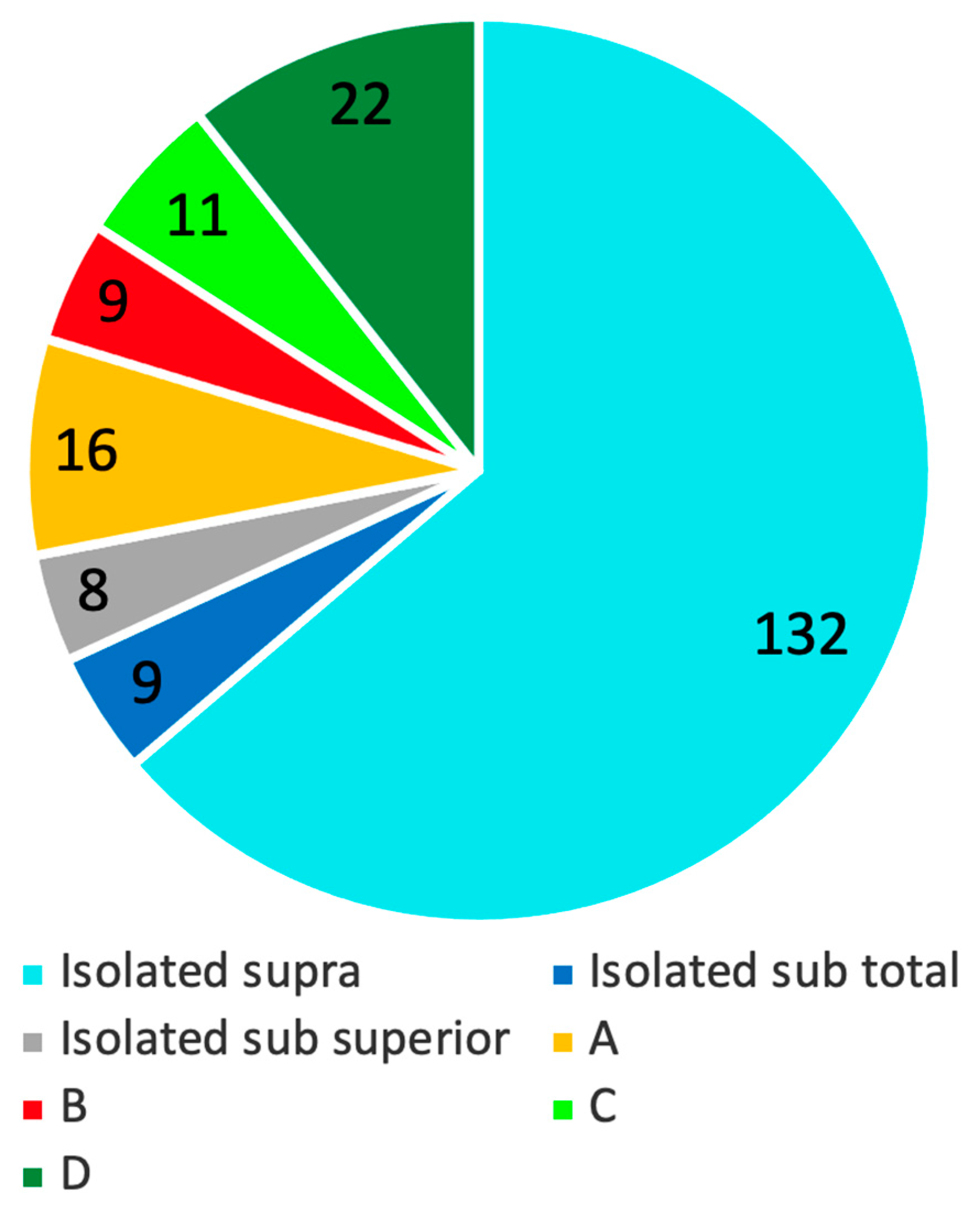
2. Methods
2.1. Surgical Technique
2.2. Clinical Evaluation
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sethi, N.; Wright, R.; Yamaguchi, K. Disorders of the Long Head of the Biceps Tendon. J. Shoulder Elbow Surg. 1999, 8, 644–654. [Google Scholar] [CrossRef]
- Chen, C.-H.; Hsu, K.-Y.; Chen, W.-J.; Shih, C.-H. Incidence and Severity of Biceps Long Head Tendon Lesion in Patients with Complete Rotator Cuff Tears. J. Trauma 2005, 58, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, P.M.; Boileau, P. The Long Head of Biceps and Associated Tendinopathy. J. Bone Joint Surg. Br. 2007, 89, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Desai, S.S.; Mata, H.K. Long Head of Biceps Tendon Pathology and Results of Tenotomy in Full-Thickness Reparable Rotator Cuff Tear. Arthroscopy 2017, 33, 1971–1976. [Google Scholar] [CrossRef]
- Godenèche, A.; Nové-Josserand, L.; Audebert, S.; Toussaint, B.; Denard, P.J.; French Society for Arthroscopy (SFA); Lädermann, A. Relationship between Subscapularis Tears and Injuries to the Biceps Pulley. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2114–2120. [Google Scholar] [CrossRef]
- Walch, G.; Edwards, T.B.; Boulahia, A.; Nové-Josserand, L.; Neyton, L.; Szabo, I. Arthroscopic Tenotomy of the Long Head of the Biceps in the Treatment of Rotator Cuff Tears: Clinical and Radiographic Results of 307 Cases. J. Shoulder Elbow Surg. 2005, 14, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.J.; McIrvin, E.; Mair, S.D.; Hawkins, R.J. Results of Biceps Tenotomy for Treatment of Pathology of the Long Head of the Biceps Brachii. J. Shoulder Elbow Surg. 2001, 10, 247–249. [Google Scholar] [CrossRef]
- Godenèche, A.; Kempf, J.-F.; Nové-Josserand, L.; Michelet, A.; Saffarini, M.; Hannink, G.; Collin, P. Tenodesis Renders Better Results than Tenotomy in Repairs of Isolated Supraspinatus Tears with Pathologic Biceps. J. Shoulder Elbow Surg. 2018, 27, 1939–1945. [Google Scholar] [CrossRef] [PubMed]
- Belk, J.W.; Kraeutler, M.J.; Houck, D.A.; Chrisman, A.N.; Scillia, A.J.; McCarty, E.C. Biceps Tenodesis versus Tenotomy: A Systematic Review and Meta-Analysis of Level I Randomized Controlled Trials. J. Shoulder Elbow Surg. 2020, 30, 951–960. [Google Scholar] [CrossRef]
- Delle Rose, G.; Borroni, M.; Silvestro, A.; Garofalo, R.; Conti, M.; De Nittis, P.; Castagna, A. The Long Head of Biceps as a Source of Pain in Active Population: Tenotomy or Tenodesis? A Comparison of 2 Case Series with Isolated Lesions. Musculoskelet. Surg. 2012, 96 (Suppl. 1), S47–S52. [Google Scholar] [CrossRef]
- Shank, J.R.; Singleton, S.B.; Braun, S.; Kissenberth, M.J.; Ramappa, A.; Ellis, H.; Decker, M.J.; Hawkins, R.J.; Torry, M.R. A Comparison of Forearm Supination and Elbow Flexion Strength in Patients with Long Head of the Biceps Tenotomy or Tenodesis. Arthroscopy 2011, 27, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Duff, S.J.; Campbell, P.T. Patient Acceptance of Long Head of Biceps Brachii Tenotomy. J. Shoulder Elbow Surg. 2012, 21, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Mirzayan, R.; McCrum, C.; Butler, R.K.; Alluri, R.K. Risk Factors and Complications Following Arthroscopic Tenotomy of the Long Head of the Biceps Tendon. Orthop. J. Sports Med. 2020, 8, 2325967120904361. [Google Scholar] [CrossRef]
- Lim, T.K.; Moon, E.S.; Koh, K.H.; Yoo, J.C. Patient-Related Factors and Complications after Arthroscopic Tenotomy of the Long Head of the Biceps Tendon. Am. J. Sports Med. 2011, 39, 783–789. [Google Scholar] [CrossRef]
- Mariani, E.M.; Cofield, R.H.; Askew, L.J.; Li, G.P.; Chao, E.Y. Rupture of the Tendon of the Long Head of the Biceps Brachii. Surgical versus Nonsurgical Treatment. Clin. Orthop. Relat. Res. 1988, 228, 233–239. [Google Scholar] [CrossRef]
- Pouliquen, L.; Berhouet, J.; Istvan, M.; Thomazeau, H.; Ropars, M.; Collin, P. Popeye Sign: Frequency and Functional Impact. Orthop. Traumatol. Surg. Res. 2018, 104, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.-H.; Lin, Y.-C.; Chen, P.; Chao-Yu Chen, A.; Chan, Y.-S.; Hsu, K.-Y.; Lädermann, A. Adhesion of the Long Head of the Biceps Tendon: A Case Series. Arthrosc. Sports Med. Rehabil. 2021, 3, e79–e87. [Google Scholar] [CrossRef]
- Denard, P.J.; Lädermann, A.; Burkhart, S.S. Arthroscopic Management of Subscapularis Tears. Sports Med. Arthrosc. Rev. 2011, 19, 333–341. [Google Scholar] [CrossRef]
- Collin, P.; McCoubrey, G.; Lädermann, A. Posterosuperior Rotator Cuff Repair by an Independent Double-Row Technique. Technical Note and Radiological and Clinical Results. Orthop. Traumatol. Surg. Res. 2016, 102, 405–408. [Google Scholar] [CrossRef]
- Collin, P.; Matsumura, N.; Lädermann, A.; Denard, P.J.; Walch, G. Relationship between Massive Chronic Rotator Cuff Tear Pattern and Loss of Active Shoulder Range of Motion. J. Shoulder Elbow Surg. 2014, 23, 1195–1202. [Google Scholar] [CrossRef]
- Lädermann, A.; Denard, P.J.; Collin, P. Massive Rotator Cuff Tears: Definition and Treatment. Int. Orthop. 2015, 39, 2403–2414. [Google Scholar] [CrossRef]
- Liotard, J.-P. Rééducation d’une épaule douloureuse: Comment faire simple. Revue Rhum. Monogr. 2010, 77, 239–245. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A Clinical Method of Functional Assessment of the Shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Gilbart, M.K.; Gerber, C. Comparison of the Subjective Shoulder Value and the Constant Score. J. Shoulder Elbow Surg. 2007, 16, 717–721. [Google Scholar] [CrossRef]
- Collin, P.; Yoshida, M.; Delarue, A.; Lucas, C.; Jossaume, T.; Lädermann, A. French Society for Shoulder and Elbow (SOFEC) Evaluating Postoperative Rotator Cuff Healing: Prospective Comparison of MRI and Ultrasound. Orthop. Traumatol. Surg. Res. 2015, 101, S265–S268. [Google Scholar] [CrossRef]
- Sugaya, H.; Maeda, K.; Matsuki, K.; Moriishi, J. Repair Integrity and Functional Outcome after Arthroscopic Double-Row Rotator Cuff Repair. A Prospective Outcome Study. J. Bone Joint Surg. Am. 2007, 89, 953–960. [Google Scholar] [CrossRef]
- Van Deurzen, D.F.P.; Garssen, F.L.; Wessel, R.N.; Kerkhoffs, G.M.M.J.; van den Bekerom, M.P.J.; van Wier, M.F. The Popeye Sign: A Doctor’s and Not a Patient’s Problem. J. Shoulder Elbow Surg. 2021, 30, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.M.; Drakos, M.C.; Fealy, S.; Taylor, S.A.; O’Brien, S.J. Arthroscopic Release of the Long Head of the Biceps Tendon: Functional Outcome and Clinical Results. Am. J. Sports Med. 2005, 33, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Baqué, F.; Valerio, L.; Ahrens, P.; Chuinard, C.; Trojani, C. Isolated Arthroscopic Biceps Tenotomy or Tenodesis Improves Symptoms in Patients with Massive Irreparable Rotator Cuff Tears. J. Bone Joint Surg. Am. 2007, 89, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Osbahr, D.C.; Diamond, A.B.; Speer, K.P. The Cosmetic Appearance of the Biceps Muscle after Long-Head Tenotomy versus Tenodesis. Arthroscopy 2002, 18, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, C.S.; DiSipio, C.; Lester, J.; Gardner, T.R.; Levine, W.N.; Bigliani, L.U. Factors Affecting Dropped Biceps Deformity after Tenotomy of the Long Head of the Biceps Tendon. Arthroscopy 2007, 23, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Szabó, I.; Boileau, P.; Walch, G. The Proximal Biceps as a Pain Generator and Results of Tenotomy. Sports Med. Arthrosc. Rev. 2008, 16, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Kukkonen, J.; Kauko, T.; Vahlberg, T.; Joukainen, A.; Aärimaa, V. Investigating Minimal Clinically Important Difference for Constant Score in Patients Undergoing Rotator Cuff Surgery. J. Shoulder Elbow Surg. 2013, 22, 1650–1655. [Google Scholar] [CrossRef]
- Tashjian, R.Z.; Shin, J.; Broschinsky, K.; Yeh, C.-C.; Martin, B.; Chalmers, P.N.; Greis, P.E.; Burks, R.T.; Zhang, Y. Minimal Clinically Important Differences in the American Shoulder and Elbow Surgeons, Simple Shoulder Test, and Visual Analog Scale Pain Scores after Arthroscopic Rotator Cuff Repair. J. Shoulder Elbow Surg. 2020, 29, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Audigé, L.; Flury, M.; Müller, A.M.; ARCR CES Consensus Panel; Durchholz, H. Complications Associated with Arthroscopic Rotator Cuff Tear Repair: Definition of a Core Event Set by Delphi Consensus Process. J. Shoulder Elbow Surg. 2016, 25, 1907–1917. [Google Scholar] [CrossRef] [PubMed]

| Variable | Mean ± SD or Number of Observations (%) |
|---|---|
| Age (years) | 60.6 ± 8.1 |
| Male/Female | 83 (40.1)/124 (59.9) |
| BMI | 27.4 ± 4.7 |
| Dominant shoulder operated | 151 (73.7)/56 (27.3) |
| Manual work | 84 (40.6)/123 (59.4) |
| LHB Related Complications | 6 Months N. Observation (%) | 1 Year N. Observation (%) | p Value |
|---|---|---|---|
| At least one complication | 75 (36.2) | 41 (19.8) | <0.001 * |
| Cramps | 16 (7.7) | 17 (8.2) | 0.856 |
| Cosmetic deformity ^ | 38 (18.4) | 18 (8.7) | 0.004 * |
| Biceps discomfort | 52 (25.1) | 24 (11.6) | <0.001 * |
| Cramps | Popeye | Discomfort | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk Factors | OR | 95% CI | p Value ^ | OR | 95% CI | p Value ^ | OR | 95% CI | p Value ^ |
| Age 6 months 1 year | 0.88 | 0.81–0.96 | <0.001 * | 0.95 | 0.95–1.03 | 0.660 | 0.94 | 0.90–0.98 | 0.007 * |
| 54.5 ± 5.9 vs. 61.1 ± 8.0 | 60.3 ± 8.3 vs. 60.6 ± 8.0 | 57.8 ± 7.3 vs. 61.5 ± 8.1 | |||||||
| 0.98 | 0.92–1.05 | 0.412 | 1.02 | 0.96–1.1 | 0.610 | 0.96 | 0.90–1.01 | 0.159 | |
| 59.4 ± 8.2 vs. 60.7 ± 8.1 | 61.7 ± 8.5 vs. 60.4 ± 8 | 58.2 ± 7.5 vs. 60.9 ± 8.1 | |||||||
| BMI 6 months 1 year | 1.1 | 1.02–1.23 | 0.025 * | 0.98 | 0.9–1.1 | 0.912 | 1.1 | 0.98–1.1 | 0.190 |
| 30 ± 5.2 vs. 27.2 ± 4.7 | 27 ± 3.3 vs. 27.5 ± 4.5 | 28.2 ± 5.2 vs. 27.1 ± 4.6 | |||||||
| 0.97 | 0.9–1.1 | 0.529 | 1.00 | 0.9–1.1 | 0.849 | 0.99 | 0.9–1.1 | 0.920 | |
| 26.7 ± 4.7 vs. 27.5 ± 4.8 | 27.5 ± 4.2 vs. 27.4 ± 4.8 | 27.2 ± 4.1 vs. 27.4 ± 4.8 | |||||||
| Male sex | |||||||||
| 6 months | 0.9 | 0.3–2.5 | 0.825 | 6.9 | 3.0–15.5 | <0.001 * | 0.9 | 0.5–1.7 | 0.781 |
| 1 year | 0.6 | 0.2–1.8 | 0.491 | 1.6 | 0.6–4.1 | 0.370 | 0.7 | 0.3–1.8 | 0.472 |
| DA operated | |||||||||
| 6 months | 0.5 | 0.2–1.3 | 0.145 | 0.8 | 0.4–1.7 | 0.589 | 0.9 | 0.5–1.9 | 0.878 |
| 1 year | 1.2 | 0.4–4.0 | 0.714 | 0.7 | 0.3–2.0 | 0.549 | 2.0 | 0.7–6.1 | 0.305 |
| Manual work | |||||||||
| 6 months | 5.0 | 1.5–16.0 | 0.009 * | 1.4 | 0.7–2.9 | 0.346 | 2.3 | 1.2–4.3 | 0.010 * |
| 1 year | 2.9 | 1.1–8.3 | 0.034 * | 1.9 | 0.7–5.1 | 0.176 | 2.8 | 1.1–6.6 | 0.020 * |
| STT vs MCT | |||||||||
| 6 months | -° | -° | 0.0168 * | 0.8 | 0.4–1.7 | 0.589 | 1.9 | 0.9–4.1 | 0.103 |
| 1 year | 3.1 | 0.7–14.1 | 0.120 | 1.0 | 0.3–3.0 | 0.981 | 4.9 | 1.1–21.3 | 0.037 * |
| Healed tendon | |||||||||
| 6 months | 0.5 | 0.1–2.5 | 0.608 | 1.5 | 0.7–3.5 | 0.307 | 0.5 | 0.2–1.3 | 0.157 |
| 1 year | 1.2 | 0.4–4.0 | 0.485 | 0.2 | 0.03–1.6 | 0.165 | 0.8 | 0.2–2.4 | 0.836 |
| Popeye | |||||||||
| 6 months | 2.2 | 0.7–6.7 | 0.065 | - | - | - | 2.3 | 1.1–4.9 | 0.024 * |
| 1 year | 2.5 | 0.6–9.7 | 0.173 | - | - | - | 3.4 | 1.1–10.7 | 0.003 * |
| No LHB Complications | ≥1 LHB Complications | p Value | |
|---|---|---|---|
| six months | |||
| N ^ cases | 132 | 75 | |
| Isolated tendon/MCT | 92 (69.7%)/40 (30.3%) | 57 (76%)/18 (24%) | 0.332 |
| Healed/non-healed | 105 (79.5%)/27 (20.5%) | 60 (80%)/15 (20%) | 0.938 |
| SS involvement 1 | 101 (76.5%) | 53 (70.7%) | 0.447 |
| AE postop | 154.2 ± 23.7 | 149.1 ± 22.0 | 0.039 * |
| ER postop | 50.3 ± 18.4 | 47.5 ± 16.4 | 0.250 |
| IR postop (median) | T12 | L5/L3 | 0.017 * |
| Constant score postop | 75.3 ± 11.3 | 70.4 ± 13.9 | 0.003 * |
| Pain (VAS) | 0.9 ± 1.3 | 1.9 ± 1.6 | <0.001 * |
| SSV | 80.2 ± 13.2 | 76.4 ± 17.0 | 0.001 * |
| 1 year | |||
| N ^ cases | 166 | 41 | |
| Isolated tendon/MCT | 116 (69.9%)/50 (30.1%) | 33 (80.5%)/8 (19.5%) | 0.244 |
| Healed/non-healed | 130 (78.3%)/36 (21.7%) | 35 (85.4%)/6 (14.6%) | 0.390 |
| Pain (VAS) | 0.6 ± 1.0 | 2.0 ± 2.0 | <0.001 * |
| SSV | 91.1 ± 11.2 | 77.8 ± 15 | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ranieri, R.; Nabergoj, M.; Xu, L.; Coz, P.L.; Mohd Don, A.F.; Lädermann, A.; Collin, P. Complications of Long Head of the Biceps Tenotomy in Association with Arthroscopic Rotator Cuff Repair: Risk Factors and Influence on Outcomes. J. Clin. Med. 2022, 11, 5657. https://doi.org/10.3390/jcm11195657
Ranieri R, Nabergoj M, Xu L, Coz PL, Mohd Don AF, Lädermann A, Collin P. Complications of Long Head of the Biceps Tenotomy in Association with Arthroscopic Rotator Cuff Repair: Risk Factors and Influence on Outcomes. Journal of Clinical Medicine. 2022; 11(19):5657. https://doi.org/10.3390/jcm11195657
Chicago/Turabian StyleRanieri, Riccardo, Marko Nabergoj, Li Xu, Pierre Le Coz, Ahmad Farihan Mohd Don, Alexandre Lädermann, and Philippe Collin. 2022. "Complications of Long Head of the Biceps Tenotomy in Association with Arthroscopic Rotator Cuff Repair: Risk Factors and Influence on Outcomes" Journal of Clinical Medicine 11, no. 19: 5657. https://doi.org/10.3390/jcm11195657
APA StyleRanieri, R., Nabergoj, M., Xu, L., Coz, P. L., Mohd Don, A. F., Lädermann, A., & Collin, P. (2022). Complications of Long Head of the Biceps Tenotomy in Association with Arthroscopic Rotator Cuff Repair: Risk Factors and Influence on Outcomes. Journal of Clinical Medicine, 11(19), 5657. https://doi.org/10.3390/jcm11195657







