Prevalence and Determinants of Chronic Pain Post-COVID; Cross-Sectional Study
Abstract
1. Introduction
2. Material and Methods
2.1. Procedure and Participants
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Study Population
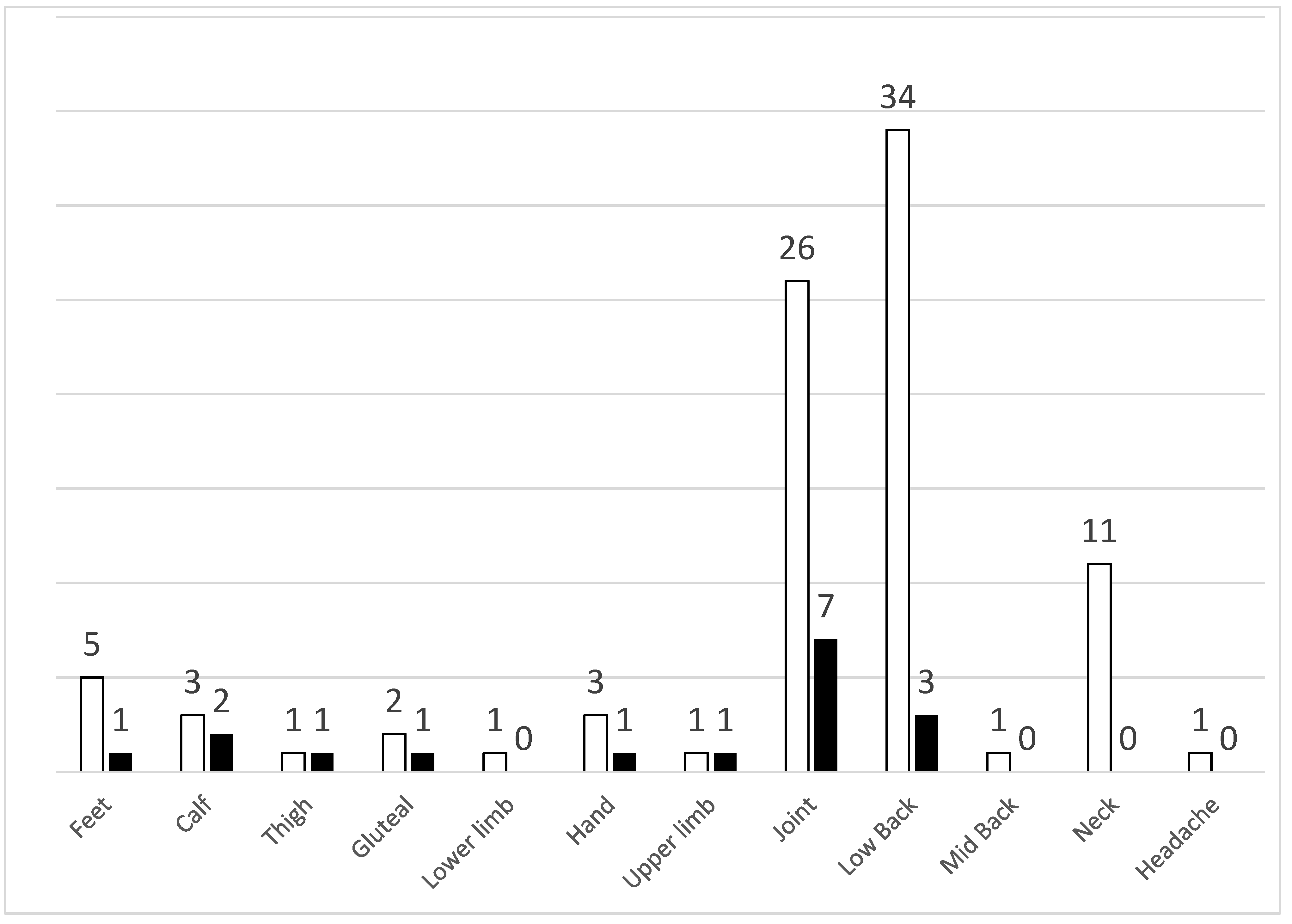
3.2. Prevalence and Determinants of Chronic Pain
3.3. Prevalence and Determinants of Neuropathic Pain
3.4. Prevalence and Determinants of New-Onset Pain Post COVID-19
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Izquierdo-Dominguez, A.; Rojas-Lechuga, M.J.; Mullol, J.; Alobid, I. Olfactory dysfunction in the COVID-19 outbreak. J. Investig. Allergol. Clin. Immunol. 2020, 30, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Ellul, M.A.; Benjamin, L.; Singh, B.; Lant, S.; Michael, B.D.; Easton, A.; Kneen, R.; Defres, S.; Sejvar, J.; Solomon, T. Neurological associations of COVID-19. Lancet Neurol. 2020, 19, 767–783. [Google Scholar] [CrossRef]
- Raveendran, A.V.; Jayadevan, R.; Sashidharan, S. Long COVID: An overview. Diabetes Metab Syndr. 2021, 15, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D. Neuropathic pain: Definition, assessment and epidemiology. Rev. Neurol. 2019, 175, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Freynhagen, R.; Baron, R.; Gockel, U.; Tölle, T.R. painDETECT: A new screening questionnaire to identify neuropathic components in patients with back pain. Curr. Med. Res. Opin. 2006, 22, 1911–1920. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Sykioti, P.; Zis, P.; Vadalouca, A.; Siafaka, I.; Argyra, E.; Bouhassira, D.; Stavropoulou, E.; Karandreas, N. Validation of the Greek version of the DN4 diagnostic questionnaire for neuropathic pain. Pain Pract. 2015, 15, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Wollan, P.C.; Weingarten, T.N.; Watson, J.C.; Hooten, W.M.; Melton, L.J., 3rd. The prevalence of neuropathic pain: Clinical evaluation compared with screening tools in a community population. Pain Med. 2009, 10, 586–593. [Google Scholar] [CrossRef] [PubMed]
| Total Population (n = 90) | |
|---|---|
| Demographics | |
| Age, in years (SD) | 47.5 (15.3) |
| Female gender (%) | 56 (62.2) |
| BMI | 26.8 (4.6) |
| COVID-19 neurological symptoms | |
| Anosmia/Hyposmia (%) | 43 (47.8) |
| Ageusia/Hypogeusia (%) | 43 (47.8) |
| Fatigue (%) | 49 (54.4) |
| Headache (%) | 40 (44.4) |
| Dizziness (%) | 11 (12.2) |
| Any neurological symptom (%) | 76 (84.4) |
| Chronic Pain (n = 57) | No Chronic Pain (n = 33) | p | |
|---|---|---|---|
| Demographics | |||
| Age, in years (SD) | 50.5 (15.9) | 42.2 (12.6) | 0.011 |
| Female gender (%) | 41 (71.9) | 15 (45.5) | 0.013 |
| BMI | 27.3 (4.9) | 26.0 (3.7) | 0.205 |
| COVID-19 neurological symptoms | |||
| Anosmia/Hyposmia (%) | 29 (50.9) | 14 (42.4) | 0.439 |
| Ageusia/Hypogeusia (%) | 28 (49.1) | 15 (45.5) | 0.737 |
| Fatigue (%) | 30 (52.6) | 19 (57.6) | 0.650 |
| Headache (%) | 25 (43.9) | 15 (45.5) | 0.883 |
| Dizziness (%) | 7 (12.3) | 4 (12.1) | 0.982 |
| Any neurological symptom (%) | 48 (84.2) | 28 (84.8) | 0.936 |
| Variable | OR * (95% CI) | Wald | p-Value |
|---|---|---|---|
| Age (per year) | 1.044 (1.01–1.079) | 6.358 | 0.012 |
| Female gender | 3.359 (1.308–8.625) | 6.339 | 0.012 |
| Neuropathic Pain (n = 22) | Non-Neuropathic Pain (n = 35) | p | |
|---|---|---|---|
| Demographics | |||
| Age, in years (SD) | 54.1 (12.4) | 48.3 (17.6) | 0.098 |
| Female gender (%) | 17 (77.3) | 24 (68.6) | 0.477 |
| BMI | 26.9 (5.0) | 27.5 (4.9) | 0.550 |
| COVID-19 neurological symptoms | |||
| Anosmia/Hyposmia (%) | 12 (54.5) | 17 (48.6) | 0.661 |
| Ageusia/Hypogeusia (%) | 13 (59.1) | 15 (42.9) | 0.233 |
| Fatigue (%) | 14 (63.6) | 16 (45.7) | 0.187 |
| Headache (%) | 14 (63.6) | 11 (31.4) | 0.017 |
| Dizziness (%) | 3 (13.6) | 4 (11.4) | 0.805 |
| Any neurological symptom (%) | 21 (95.5) | 27 (77.1) | 0.065 |
| Variable | OR * (95% CI) | Wald | p-Value |
|---|---|---|---|
| Age (per year) | 1.036 (0.997–1.076) | 3.217 | 0.073 |
| Female gender | 1.784 (0.471–6.747) | 0.727 | 0.394 |
| Headache | 4.910 (1.449–16.636) | 6.532 | 0.011 |
| Post COVID Pain (n = 15) | No Pain (n = 33) | p | |
|---|---|---|---|
| Demographics | |||
| Age, in years (SD) | 48.7 (14.3) | 42.2 (12.6) | 0.100 |
| Female gender (%) | 12 (80.0) | 15 (45.5) | 0.025 |
| BMI | 29.2 (6.1) | 26.0 (3.7) | 0.136 |
| COVID-19 neurological symptoms | |||
| Anosmia/Hyposmia (%) | 8 (53.3) | 14 (42.4) | 0.482 |
| Ageusia/Hypogeusia (%) | 8 (53.3) | 15 (45.5) | 0.613 |
| Fatigue (%) | 11 (73.3) | 19 (57.6) | 0.296 |
| Headache (%) | 9 (60.0) | 15 (45.5) | 0.350 |
| Dizziness (%) | 1 (6.7) | 4 (12.1) | 0.566 |
| Any neurological symptom (%) | 13 (86.7) | 28 (84.8) | 0.869 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zis, P.; Ioannou, C.; Artemiadis, A.; Christodoulou, K.; Kalampokini, S.; Hadjigeorgiou, G.M. Prevalence and Determinants of Chronic Pain Post-COVID; Cross-Sectional Study. J. Clin. Med. 2022, 11, 5569. https://doi.org/10.3390/jcm11195569
Zis P, Ioannou C, Artemiadis A, Christodoulou K, Kalampokini S, Hadjigeorgiou GM. Prevalence and Determinants of Chronic Pain Post-COVID; Cross-Sectional Study. Journal of Clinical Medicine. 2022; 11(19):5569. https://doi.org/10.3390/jcm11195569
Chicago/Turabian StyleZis, Panagiotis, Christiana Ioannou, Artemios Artemiadis, Katerina Christodoulou, Stefania Kalampokini, and Georgios M. Hadjigeorgiou. 2022. "Prevalence and Determinants of Chronic Pain Post-COVID; Cross-Sectional Study" Journal of Clinical Medicine 11, no. 19: 5569. https://doi.org/10.3390/jcm11195569
APA StyleZis, P., Ioannou, C., Artemiadis, A., Christodoulou, K., Kalampokini, S., & Hadjigeorgiou, G. M. (2022). Prevalence and Determinants of Chronic Pain Post-COVID; Cross-Sectional Study. Journal of Clinical Medicine, 11(19), 5569. https://doi.org/10.3390/jcm11195569







