The Analgesic Efficacy of the Single Erector Spinae Plane Block with Intercostal Nerve Block Is Not Inferior to That of the Thoracic Paravertebral Block with Intercostal Nerve Block in Video-Assisted Thoracic Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Perioperative Management
2.3. Paravertebral Block
2.4. Erector Spinae Plane Block
2.5. Intercostal Nerve Block
2.6. Outcome Measures
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, K.; Liu, D.; Chen, J.; Yu, S.; Bai, Y.; Chen, C.; Yao, Y.; Yu, L.; Yan, M. Moderate-severe postoperative pain in patients undergoing video-assisted thoracoscopic surgery: A retrospective study. Sci. Rep. 2020, 10, 795. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Postoperative pain, analgesia, and recovery-bedfellows that cannot be ignored. Pain 2018, 159, S11–S16. [Google Scholar] [CrossRef] [PubMed]
- Bayman, E.O.; Parekh, K.; Keech, J.; Selte, A.; Brennan, T. A Prospective Study of Chronic Pain after Thoracic Surgery. Anesthesiology 2017, 126, 938–951. [Google Scholar] [CrossRef] [PubMed]
- Steinthorsdottir, K.; Wildgaard, L.; Hansen, H.J.; Petersen, R.H.; Wildgaard, K. Regional analgesia for video-assisted thoracic surgery: A systematic review. Eur. J. Cardiothorac. Surg. 2014, 45, 959–966. [Google Scholar] [CrossRef]
- Elsabeeny, W.Y.; Ibrahim, M.A.; Shehab, N.N.; Mohamed, A.; Wadod, M.A. Serratus Anterior Plane Block and Erector Spinae Plane Block Versus Thoracic Epidural Analgesia for Perioperative Thoracotomy Pain Control: A Randomized Controlled Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2928–2936. [Google Scholar] [CrossRef]
- Kot, P.; Rodriguez, P.; Granell, M.; Cano, B.; Rovira, L.; Morales, J.; Broseta, A.; De Andrés, J. The erector spinae plane block: A narrative review. Korean J. Anesthesiol. 2019, 72, 209–220. [Google Scholar] [CrossRef]
- Turhan, O.; Sivrikoz, N.; Sungur, Z.; Duman, S.; Özkan, B.; Şentürk, M. Thoracic Paravertebral Block Achieves Better Pain Control Than Erector Spinae Plane Block and Intercostal Nerve Block in Thoracoscopic Surgery: A Randomized Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2920–2927. [Google Scholar] [CrossRef]
- Guerra-Londono, C.E.; Privorotskiy, A.; Cozowicz, C.; Hicklen, R.S.; Memtsoudis, S.G.; Mariano, E.R.; Cata, J.P. Assessment of Intercostal Nerve Block Analgesia for Thoracic Surgery: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2133394. [Google Scholar] [CrossRef]
- Gürkan, Y.; Aksu, C.; Kuş, A.; Yörükoğlu, U.H. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: A randomized controlled trial. J. Clin. Anesth. 2020, 59, 84–88. [Google Scholar] [CrossRef]
- Gutierrez, J.J.P.; Ben-David, B.; Rest, C.; Grajales, M.T.; Khetarpal, S.K. Quadratus lumborum block type 3 versus lumbar plexus block in hip replacement surgery: A randomized, prospective, non-inferiority study. Reg. Anesth. Pain Med. 2020, 46, 111–117. [Google Scholar] [CrossRef]
- Imperatori, A.; Rotolo, N.; Gatti, M.; Nardecchia, E.; De Monte, L.; Conti, V.; Dominioni, L. Peri-operative complications of video-assisted thoracoscopic surgery (VATS). Int. J. Surg. 2008, 6, S78–S81. [Google Scholar] [CrossRef]
- Gerner, P. Postthoracotomy Pain Management Problems. Anesthesiol. Clin. 2008, 26, 355–367. [Google Scholar] [CrossRef]
- Kirby, T.J.; Mack, M.J.; Landreneau, R.J.; Rice, T.W. Lobectomy—Video-assisted thoracic surgery versus muscle-sparing thoracotomy: A randomized trial. J. Thorac. Cardiovasc. Surg. 1995, 109, 997–1001; discussion 1001–1002. [Google Scholar] [CrossRef]
- Horlocker, T.T.; Vandermeuelen, E.; Kopp, S.L.; Gogarten, W.; Leffert, L.R.; Benzon, H.T. Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg. Anesth. Pain Med. 2018, 43, 263–309. [Google Scholar] [CrossRef]
- Yeung, J.; Gates, S.; Naidu, B.V.; Wilson, M.J.A.; Smith, F.G. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst. Rev. 2016, 2, CD009121. [Google Scholar] [CrossRef]
- Ardon, A.E.; Lee, J.; Franco, C.D.; Riutort, K.T.; Greengrass, R.A. Paravertebral block: Anatomy and relevant safety issues. Korean J. Anesthesiol. 2020, 73, 394–400. [Google Scholar] [CrossRef]
- Chin, K.J. Thoracic wall blocks: From paravertebral to retrolaminar to serratus to erector spinae and back again—A review of evidence. Best Pract. Res. Clin. Anaesthesiol. 2019, 33, 67–77. [Google Scholar] [CrossRef]
- Kim, H.K. Video-Assisted Thoracic Surgery Lobectomy. J. Chest Surg. 2021, 54, 239–245. [Google Scholar] [CrossRef]
- Chin, K.J.; Versyck, B.; Pawa, A. Ultrasound-guided fascial plane blocks of the chest wall: A state-of-the-art review. Anaesthesia 2021, 76, 110–126. [Google Scholar] [CrossRef]
- Chin, K.J.; Pawa, A.; Forero, M.; Adhikary, S. Ultrasound-Guided Fascial Plane Blocks of the Thorax: Pectoral I and II, Serratus Anterior Plane, and Erector Spinae Plane Blocks. Adv. Anesth. 2019, 37, 187–205. [Google Scholar] [CrossRef]
- Chin, K.J.; El-Boghdadly, K. Mechanisms of action of the erector spinae plane (ESP) block: A narrative review. Can. J. Anaesth. 2021, 68, 387–408. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.; Park, S.; Oh, C.; Pak, Y.; Jeong, K.; Yun, S.; Noh, C.; Chung, W.; Kim, Y.-H.; Ko, Y.K.; et al. Regional analgesia techniques for video-assisted thoracic surgery: A frequentist network meta-analysis. Korean J. Anesthesiol. 2022, 75, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Liao, Y.; Gong, C.; Yu, L.; Gao, F.; Yu, J.; Chen, J.; Chen, X.; Zheng, T.; Zheng, X. Regional Analgesia in Video-Assisted Thoracic Surgery: A Bayesian Network Meta-Analysis. Front. Med. 2022, 9, 842332. [Google Scholar] [CrossRef] [PubMed]
- Sertcakacilar, G.; Pektas, Y.; Yildiz, G.O.; Isgorucu, O.; Kose, S. Efficacy of ultrasound-guided erector spinae plane block versus paravertebral block for postoperative analgesia in single-port video-assisted thoracoscopic surgery: A retrospective study. Ann. Palliat. Med. 2022, 11, 1981–1989. [Google Scholar] [CrossRef]
- Zhang, J.; He, Y.; Wang, S.; Chen, Z.; Zhang, Y.; Gao, Y.; Wang, Q.; Xia, Y.; Papadimos, T.J.; Zhou, R. The erector spinae plane block causes only cutaneous sensory loss on ipsilateral posterior thorax: A prospective observational volunteer study. BMC Anesthesiol. 2020, 20, 88. [Google Scholar] [CrossRef]
- Dautzenberg, K.H.W.; Zegers, M.J.; Bleeker, C.P.; Tan, E.C.T.H.; Vissers, K.C.P.; van Geffen, G.-J.; van der Wal, S.E.I. Unpredictable Injectate Spread of the Erector Spinae Plane Block in Human Cadavers. Anesth. Analg. 2019, 129, e163–e166. [Google Scholar] [CrossRef]
- Huan, S.; Deng, Y.; Wang, J.; Ji, Y.; Yin, G. Efficacy and safety of paravertebral block versus intercostal nerve block in thoracic surgery and breast surgery: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0237363. [Google Scholar] [CrossRef]
- Borys, M.; Gawęda, B.; Horeczy, B.; Kolowca, M.; Olszówka, P.; Czuczwar, M.; Woloszczuk-Gebicka, B.; Widenka, K. Erector spinae-plane block as an analgesic alternative in patients undergoing mitral and/or tricuspid valve repair through a right mini-thoracotomy—An observational cohort study. Wideochir Inne Tech Maloinwazyjne 2020, 15, 208–214. [Google Scholar] [CrossRef]
- Liu, L.; Ni, X.-X.; Zhang, L.-W.; Zhao, K.; Xie, H.; Zhu, J. Effects of ultrasound-guided erector spinae plane block on postoperative analgesia and plasma cytokine levels after uniportal VATS: A prospective randomized controlled trial. J. Anesth. 2021, 35, 3–9. [Google Scholar] [CrossRef]
- Bendixen, M.; Jørgensen, O.D.; Kronborg, C.; Andersen, C.; Licht, P.B. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: A randomised controlled trial. Lancet Oncol. 2016, 17, 836–844. [Google Scholar] [CrossRef]
- Bayman, E.O.; Parekh, K.R.; Keech, J.; Larson, N.; Weg, M.V.; Brennan, T.J. Preoperative Patient Expectations of Postoperative Pain Are Associated with Moderate to Severe Acute Pain After VATS. Pain Med. 2019, 20, 543–554. [Google Scholar] [CrossRef]

| PVB-ICNB (n = 26) | ESPB-ICNB (n = 26) | p-Value | |
|---|---|---|---|
| Female (%) | 9 (34.6) | 13 (50.0) | |
| Age | 62.42 ± 13.11 | 60.31 ± 15.43 | 0.597 |
| Height | 161.09 ± 11.33 | 161.01 ± 10.14 | 0.978 |
| Weight | 62.34 ± 10.43 | 60.18 ± 10.72 | 0.464 |
| BSA | 1.66 ± 0.18 | 1.63 ± 0.17 | 0.591 |
| Diabetes mellitus | 11 (42.3) | 6 (23.1) | 0.143 |
| Preoperative analgesics | 3 (11.5) | 3 (11.5) | 1.000 |
| Operation Type | |||
| Lobectomy | 12 (46.2) | 13 (50.0) | |
| Segmentectomy | 3 (11.5) | 0 (0.0) | |
| Wedge resection | 10 (38.5) | 13 (50.0) | |
| Mediastinal mass | 1 (3.8) | 0 (0.0) | |
| OP time (min) | 85.96 ± 48.48 | 97.69 ± 55.38 | 0.420 |
| PVB-ICNB (n = 26) | ESPB-ICNB (n = 26) | 95% CI | p-Value | |
|---|---|---|---|---|
| Primary Endpoint | ||||
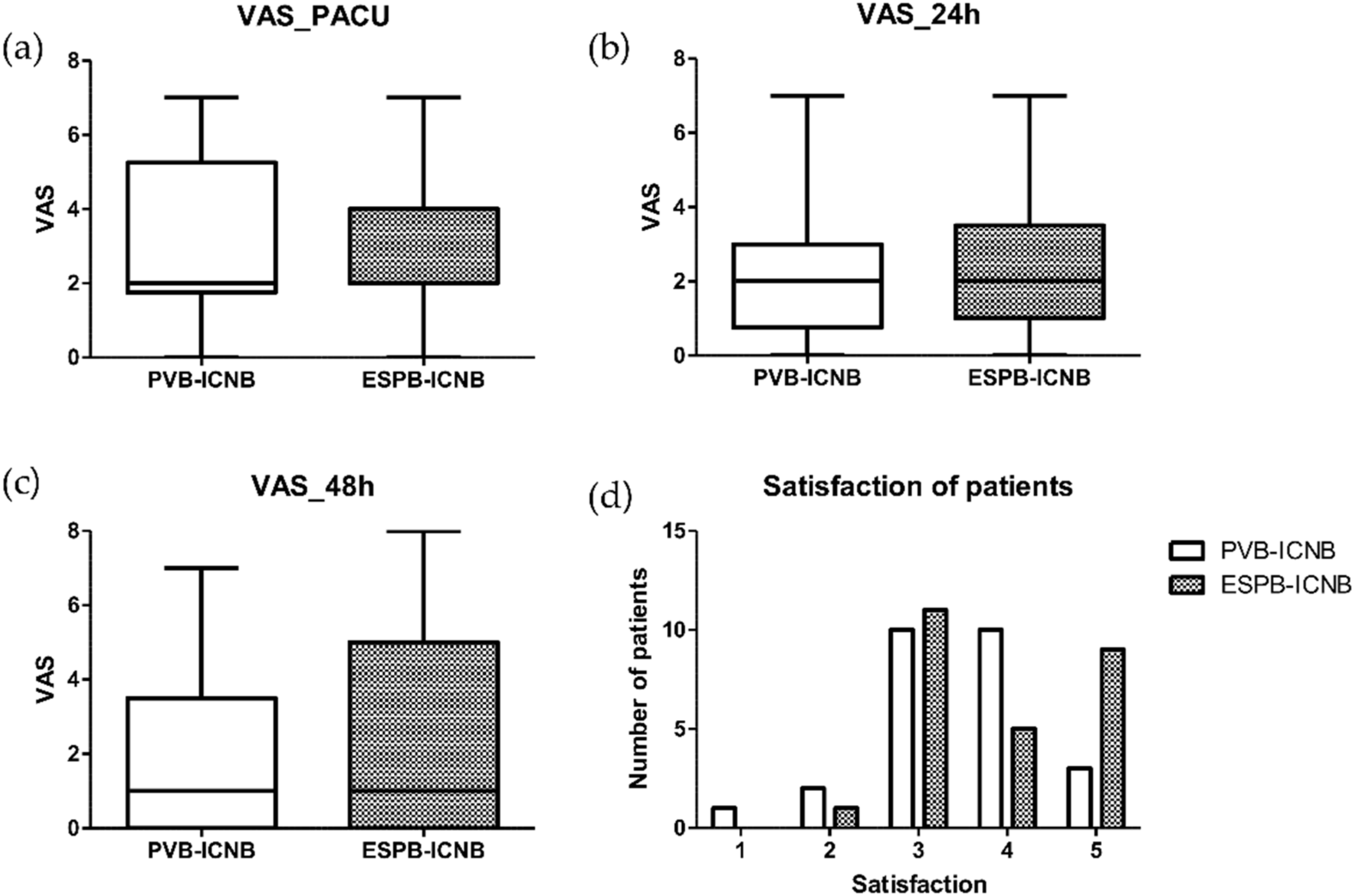
| VAS PACU | 2.0 (1.8, 5.3) | 2.0 (2.0, 4.0) | (−0.890, 1.428) | 0.970 |
| VAS 24 h | 2.0 (0.8, 3.0) | 2.0 (1.0, 3.5) | (−1.283, 1.052) | 0.993 |
| VAS 48 h | 1.0 (0.0, 3.5) | 1.0 (0.0, 5.0) | (−1.637, 1.176) | 0.985 |
| Above Moderate Pain (VAS > 3) | ||||
| VAS PACU | 8 (30.8) | 7 (26.9) | 0.762 | |
| VAS 24 h | 5 (19.2) | 6 (23.1) | 0.737 | |
| VAS 48 h | 6 (23.1) | 8 (30.8) | 0.536 | |
| Above Severe Pain (VAS > 6) | ||||
| VAS PACU | 4 (15.4) | 2 (7.7) | 0.390 | |
| VAS 24 h | 1 (3.8) | 2 (7.7) | 0.556 | |
| VAS 48 h | 1 (3.8) | 2 (7.7) | 0.556 | |
| Secondary Endpoints | ||||
| Rescue Analgesics (MME) | 110.24 ± 103.64 | 118.40 ± 93.52 | 0.767 | |
| Number of Rescue Analgesic Events | 5.88 ± 1.56 | 5.50 ± 1.45 | 0.361 | |
| Satisfaction of Patients | 3.5 (3.0, 4.0) | 4.0 (3.0, 5.0) | 0.227 | |
| Remifentanil (µg) | 511.62 ± 205.51 | 547.42 ± 224.35 | 0.551 | |
| Antiemetics | ||||
| Dose | 1.59 ± 0.63 | 1.44 ± 0.67 | 0.408 | |
| Hypotension | 2 (7.7) | 4 (15.4) | 0.390 | |
| Bradycardia | 0 (0) | 2 (3.8) | 0.153 | |
| Pleural Puncture | 2 (3.8) | 0 (0) | 0.153 | |
| Hospital Day | 9.04 ± 4.20 | 9.27 ± 3.77 | 0.836 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Song, S.W.; Do, H.; Hong, J.; Byun, C.S.; Park, J.-H. The Analgesic Efficacy of the Single Erector Spinae Plane Block with Intercostal Nerve Block Is Not Inferior to That of the Thoracic Paravertebral Block with Intercostal Nerve Block in Video-Assisted Thoracic Surgery. J. Clin. Med. 2022, 11, 5452. https://doi.org/10.3390/jcm11185452
Kim S, Song SW, Do H, Hong J, Byun CS, Park J-H. The Analgesic Efficacy of the Single Erector Spinae Plane Block with Intercostal Nerve Block Is Not Inferior to That of the Thoracic Paravertebral Block with Intercostal Nerve Block in Video-Assisted Thoracic Surgery. Journal of Clinical Medicine. 2022; 11(18):5452. https://doi.org/10.3390/jcm11185452
Chicago/Turabian StyleKim, Sujin, Seung Woo Song, Hyejin Do, Jinwon Hong, Chun Sung Byun, and Ji-Hyoung Park. 2022. "The Analgesic Efficacy of the Single Erector Spinae Plane Block with Intercostal Nerve Block Is Not Inferior to That of the Thoracic Paravertebral Block with Intercostal Nerve Block in Video-Assisted Thoracic Surgery" Journal of Clinical Medicine 11, no. 18: 5452. https://doi.org/10.3390/jcm11185452
APA StyleKim, S., Song, S. W., Do, H., Hong, J., Byun, C. S., & Park, J.-H. (2022). The Analgesic Efficacy of the Single Erector Spinae Plane Block with Intercostal Nerve Block Is Not Inferior to That of the Thoracic Paravertebral Block with Intercostal Nerve Block in Video-Assisted Thoracic Surgery. Journal of Clinical Medicine, 11(18), 5452. https://doi.org/10.3390/jcm11185452





