Severe Complications after General Anesthesia versus Sedation during Pediatric Diagnostic Cardiac Catheterization for Ventricular Septal Defect
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Data Source
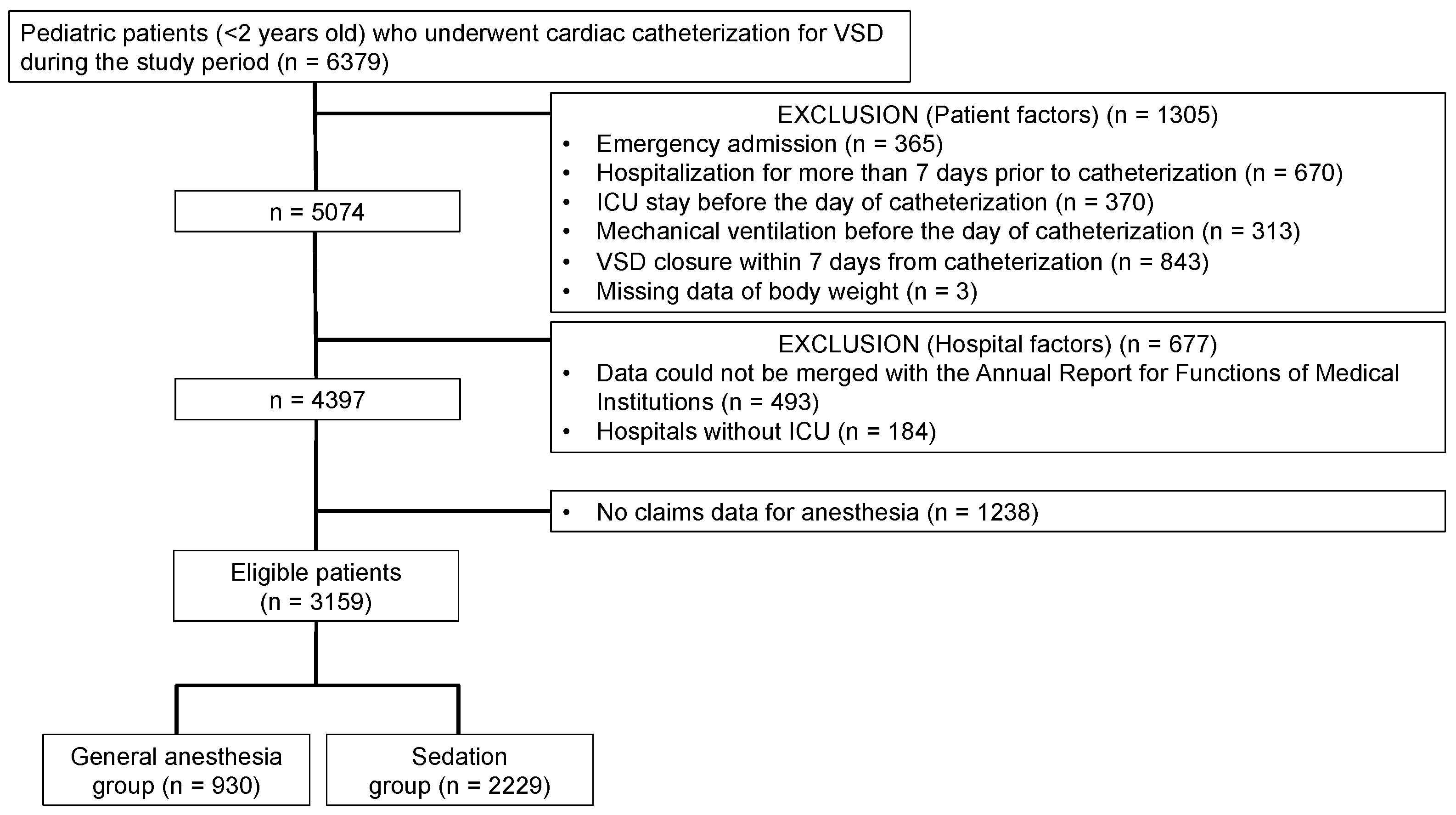
2.3. Patients
2.4. Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bennett, D.; Marcus, R.; Stokes, M. Incidents and Complications During Pediatric Cardiac Catheterization. Paediatr. Anaesth. 2005, 15, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Bergersen, L.; Marshall, A.; Gauvreau, K.; Beekman, R.; Hirsch, R.; Foerster, S.; Balzer, D.; Vincent, J.; Hellenbrand, W.; Holzer, R.; et al. Adverse Event Rates in Congenital Cardiac Catheterization—A Multi-center Experience. Catheter. Cardiovasc. Interv. 2010, 75, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Lam, J.E.; Lin, E.P.; Alexy, R.; Aronson, L.A. Anesthesia and the Pediatric Cardiac Catheterization Suite: A Review. Paediatr. Anaesth. 2015, 25, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Nykanen, D.G.; Forbes, T.J.; Du, W.; Divekar, A.A.; Reeves, J.H.; Hagler, D.J.; Fagan, T.E.; Pedra, C.A.; Fleming, G.A.; Khan, D.M.; et al. CRISP: Catheterization RISk Score for Pediatrics: A Report from the Congenital Cardiac Interventional Study Consortium (CCISC). Catheter. Cardiovasc. Interv. 2016, 87, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Odegard, K.C.; Vincent, R.; Baijal, R.G.; Daves, S.M.; Gray, R.G.; Javois, A.J.; Love, B.A.; Moore, P.; Nykanen, D.; Riegger, L.Q.; et al. SCAI/CCAS/SPA Expert Consensus Statement for Anesthesia and Sedation Practice: Recommendations for Patients Undergoing Diagnostic and Therapeutic Procedures in the Pediatric and Congenital Cardiac Catheterization Laboratory. Anesth. Analg. 2016, 123, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- No authors listed. A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology 2018, 128, 437–479. [Google Scholar] [CrossRef]
- O’Byrne, M.L.; Millenson, M.E.; Steven, J.M.; Gillespie, M.J.; Dori, Y.; Glatz, A.C.; Rome, J.J. Operator-Directed Procedural Sedation in the Congenital Cardiac Catheterization Laboratory. JACC Cardiovasc. Intv. 2019, 12, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Mikus, M.; Welchowski, T.; Schindler, E.; Schneider, M.; Mini, N.; Vergnat, M. Sedation Versus General Anesthesia for Cardiac Catheterization in Infants: A Retrospective, Monocentric, Cohort Evaluation. J. Clin. Med. 2021, 10, 5648. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Desai, S.; Nicolas, R.; Gauvreau, K.; Foerster, S.; Sharma, A.; Armsby, L.; Marshall, A.C.; Odegard, K.; DiNardo, J.; et al. Sedation and Anesthesia in Pediatric and Congenital Cardiac Catheterization: A Prospective Multicenter Experience. Pediatr. Cardiol. 2015, 36, 1363–1375. [Google Scholar] [CrossRef] [PubMed]
- Yasunaga, H.; Horiguchi, H.; Fushimi, K.; Matsuda, S. Clinical Epidemiology and Health Services Research Using the Diagnosis Procedure Combination Database in Japan. Asian Pac. J. Dis. Manag. 2015, 7, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, H.; Ikegami, N.; Shibuya, K.; Izumida, N.; Noguchi, H.; Yasunaga, H.; Miyata, H.; Acuin, J.M.; Reich, M.R. Cost Containment and Quality of Care in Japan: Is There a Trade-Off? Lancet 2011, 378, 1174–1182. [Google Scholar] [CrossRef]
- Desai, R.J.; Franklin, J.M. Alternative Approaches for Confounding Adjustment in Observational Studies Using Weighting Based on the Propensity Score: A Primer for Practitioners. BMJ 2019, 367, l5657. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.E.; Li, F.; Pencina, M.J. Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial. JAMA 2020, 323, 2417–2418. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Using the Standardized Difference to Compare the Prevalence of a Binary Variable Between Two Groups in Observational Research. Commun. Stat. Simul. Comput. 2009, 38, 1228–1234. [Google Scholar] [CrossRef]
- Odegard, K.C.; Bergersen, L.; Thiagarajan, R.; Clark, L.; Shukla, A.; Wypij, D.; Laussen, P.C. The Frequency of Cardiac Arrests in Patients with Congenital Heart Disease Undergoing Cardiac Catheterization. Anesth. Analg. 2014, 118, 175–182. [Google Scholar] [CrossRef]
- Jayaram, N.; Spertus, J.A.; Kennedy, K.F.; Vincent, R.; Martin, G.R.; Curtis, J.P.; Nykanen, D.; Moore, P.M.; Bergersen, L. Modeling Major Adverse Outcomes of Pediatric and Adult Patients with Congenital Heart Disease Undergoing Cardiac Catheterization: Observations from the NCDR IMPACT Registry (National Cardiovascular Data Registry Improving Pediatric and Adult Congenital Treatment). Circulation 2017, 136, 2009–2019. [Google Scholar] [CrossRef]
- Zeng, X.; Hu, Y.; Shu, L.; Li, J.; Duan, H.; Shu, Q.; Li, H. Explainable Machine-Learning Predictions for Complications After Pediatric Congenital Heart Surgery. Sci. Rep. 2021, 11, 17244. [Google Scholar] [CrossRef] [PubMed]
- Holzer, R.J.; Gauvreau, K.; Kreutzer, J.; Moore, J.W.; McElhinney, D.B.; Bergersen, L. Relationship Between Procedural Adverse Events Associated with Cardiac Catheterization for Congenital Heart Disease and Operator Factors: Results of a Multi-institutional Registry (C3PO). Catheter. Cardiovasc. Interv. 2013, 82, 463–473. [Google Scholar] [CrossRef] [PubMed]
| Variable | General Anesthesia (n = 930) | Sedation (n = 2229) | Standardized Mean Difference % | |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age (months), n (%) | ||||
| <3 | 109 (12) | 338 (15) | −10 | |
| 3–5 | 260 (28) | 674 (30) | −5 | |
| 6–11 | 561 (60) | 1217 (55) | 12 | |
| Male sex, n (%) | 441 (47) | 1133 (51) | −6.8 | |
| Body height (cm), mean (SD) | 65 (10.5) | 64.5 (11) | 4.6 | |
| Body weight (kg), mean (SD) | 6.5 (2.7) | 6.5 (2.7) | 0 | |
| Comorbidities, n (%) | ||||
| Pulmonary hypertension | 216 (23) | 641 (29) | −13 | |
| Heart failure | 319 (34) | 977 (44) | −20 | |
| Trisomy (21, 18, 13) | 183 (20) | 247 (11) | 24 | |
| Fiscal years of admission *, n (%) | ||||
| 2010–2011 | 111 (12) | 418 (19) | −19 | |
| 2012–2013 | 182 (20) | 548 (25) | −12 | |
| 2014–2015 | 249 (27) | 577 (26) | 2 | |
| 2016–2017 | 263 (28) | 483 (22) | 15 | |
| 2018 | 125 (13) | 203 (9.1) | 14 | |
| Hospital characteristics | ||||
| Annual number of all surgeries, n (%) | ||||
| 0–376 | 446 (48) | 978 (44) | 8.2 | |
| >376 | 484 (52) | 1251 (56) | −8.2 | |
| ICU beds, n (%) | ||||
| 0–21 | 257 (28) | 1049 (47) | −41 | |
| >21 | 673 (72) | 1180 (53) | 41 | |
| All beds, n (%) | ||||
| 0–658 | 566 (61) | 1209 (54) | 13 | |
| >658 | 364 (39) | 1020 (46) | −13 | |
| Pediatric beds, n (%) | ||||
| 0 | 16 (1.7) | 218 (9.8) | −35 | |
| 1–48 | 419 (45) | 846 (38) | 14 | |
| >48 | 495 (53) | 1165 (52) | 1.9 | |
| Pediatric-related ICU beds, n (%) | ||||
| 0 | 162 (17) | 185 (8.3) | 27 | |
| 1–9 | 300 (32) | 1021 (46) | −28 | |
| >9 | 468 (50) | 1023 (46) | 8.9 | |
| Hospital category, n (%) | ||||
| Academic hospital | 408 (44) | 1146 (51) | −15 | |
| Nonacademic advanced hospital | 107 (12) | 541 (24) | −34 | |
| Other hospitals | 415 (45) | 542 (24) | 44 | |
| Pediatric inpatient management fee †, n (%) | ||||
| None | 16 (1.7) | 218 (9.8) | −35 | |
| 1 | 454 (49) | 1059 (48) | 2.6 | |
| 2 | 438 (47) | 725 (33) | 30 | |
| 3 | 15 (1.6) | 171 (7.7) | −29 | |
| 4 | 7 (0.8) | 56 (2.5) | −14 | |
| Variable | General Anesthesia | Sedation | Standardized Mean Difference % | |
|---|---|---|---|---|
| Patient characteristics | ||||
| Age (months), % | ||||
| <3 | 13 | 13 | 0 | |
| 3–5 | 30 | 30 | 0 | |
| 6–11 | 57 | 57 | 0 | |
| Male sex, % | 49 | 49 | 0 | |
| Body height (cm), mean (SD) | 64.4 (10.5) | 64.4 (11.6) | 0 | |
| Body weight (kg), mean (SD) | 6.4 (3) | 6.4 (2.2) | 0 | |
| Comorbidities, % | ||||
| Pulmonary hypertension | 25 | 25 | 0 | |
| Heart failure | 38 | 38 | 0 | |
| Trisomy (21, 18, 13) | 18 | 18 | 0 | |
| Fiscal years of admission *, % | ||||
| 2010–2011 | 13 | 12 | 0 | |
| 2012–2013 | 22 | 22 | 0 | |
| 2014–2015 | 28 | 28 | 0 | |
| 2016–2017 | 26 | 26 | 0 | |
| 2018 | 12 | 12 | 0 | |
| Hospital characteristics | ||||
| Annual number of all surgeries, % | ||||
| 0–376 | 43 | 43 | 0 | |
| >376 | 57 | 57 | 0 | |
| ICU beds, % | ||||
| 0–21 | 37 | 37 | 0 | |
| >21 | 63 | 63 | 0 | |
| All beds, % | ||||
| 0–658 | 55 | 55 | 0 | |
| >658 | 45 | 45 | 0 | |
| Pediatric beds, % | ||||
| 0 | 3 | 3 | 0 | |
| 1–48 | 42 | 42 | 0 | |
| >48 | 55 | 55 | 0 | |
| Pediatric-related ICU beds, % | ||||
| 0 | 5.3 | 5.3 | 0 | |
| 1–9 | 37 | 37 | 0 | |
| >9 | 58 | 58 | 0 | |
| Hospital category, % | ||||
| Academic hospital | 51 | 51 | 0 | |
| Nonacademic advanced hospital | 17 | 17 | 0 | |
| Other hospitals | 32 | 32 | 0 | |
| Pediatric inpatient management fee †, % | ||||
| None | 3.0 | 3.0 | 0 | |
| 1 | 58 | 58 | 0 | |
| 2 | 35 | 35 | 0 | |
| 3 | 2.7 | 2.7 | 0 | |
| 4 | 1.1 | 1.1 | 0 | |
| Analysis | General Anesthesia % (n) | Sedation % (n) | Risk Difference | 95% Confidence Interval | p-Value |
|---|---|---|---|---|---|
| Before adjustment | 2.6% (24/930) | 0.8% (17/2229) | 1.8% | 0.7−2.9% | 0.001 |
| After adjustment | 2.4% (38/1580) | 0.6% (10/1580) | 1.8% | 0.9−2.6% | <0.001 |
| Type of Severe Complication | Before Adjustment, % (n) | After Adjustment, % | ||
|---|---|---|---|---|
| General Anesthesia | Sedation | General Anesthesia | Sedation | |
| Death | 0 (0) | 0 (0) | 0 | 0 |
| Surgery for cardiac tamponade | 0 (0) | 0 (0) | 0 | 0 |
| ECMO management | 0 (0) | 0 (0) | 0 | 0 |
| Electrical cardioversion | 0 (0) | 0.09 (2) | 0 | 0.1 |
| Catecholamine use | 2.2 (20) | 0.6 (13) | 1.9 | 0.4 |
| Pericardiocentesis | 0 (0) | 0 (0) | 0 | 0 |
| ICU admission | 1.9 (18) | 0.6 (14) | 0.7 | 0.3 |
| Cardiopulmonary resuscitation | 0 (0) | 0 (0) | 0 | 0 |
| Composite outcome | 2.6 (24) | 0.8 (17) | 2.4 | 0.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ogawa, Y.; Yamana, H.; Noda, T.; Kishimoto, M.; Yoshihara, S.; Kanaoka, K.; Matsui, H.; Fushimi, K.; Yasunaga, H.; Kawaguchi, M.; et al. Severe Complications after General Anesthesia versus Sedation during Pediatric Diagnostic Cardiac Catheterization for Ventricular Septal Defect. J. Clin. Med. 2022, 11, 5165. https://doi.org/10.3390/jcm11175165
Ogawa Y, Yamana H, Noda T, Kishimoto M, Yoshihara S, Kanaoka K, Matsui H, Fushimi K, Yasunaga H, Kawaguchi M, et al. Severe Complications after General Anesthesia versus Sedation during Pediatric Diagnostic Cardiac Catheterization for Ventricular Septal Defect. Journal of Clinical Medicine. 2022; 11(17):5165. https://doi.org/10.3390/jcm11175165
Chicago/Turabian StyleOgawa, Yuki, Hayato Yamana, Tatsuya Noda, Miwa Kishimoto, Shingo Yoshihara, Koshiro Kanaoka, Hiroki Matsui, Kiyohide Fushimi, Hideo Yasunaga, Masahiko Kawaguchi, and et al. 2022. "Severe Complications after General Anesthesia versus Sedation during Pediatric Diagnostic Cardiac Catheterization for Ventricular Septal Defect" Journal of Clinical Medicine 11, no. 17: 5165. https://doi.org/10.3390/jcm11175165
APA StyleOgawa, Y., Yamana, H., Noda, T., Kishimoto, M., Yoshihara, S., Kanaoka, K., Matsui, H., Fushimi, K., Yasunaga, H., Kawaguchi, M., & Imamura, T. (2022). Severe Complications after General Anesthesia versus Sedation during Pediatric Diagnostic Cardiac Catheterization for Ventricular Septal Defect. Journal of Clinical Medicine, 11(17), 5165. https://doi.org/10.3390/jcm11175165





