Exhaled Breath Analysis for Investigating the Use of Inhaled Corticosteroids and Corticosteroid Responsiveness in Wheezing Preschool Children
Abstract
:1. Introduction
2. Materials and Methods
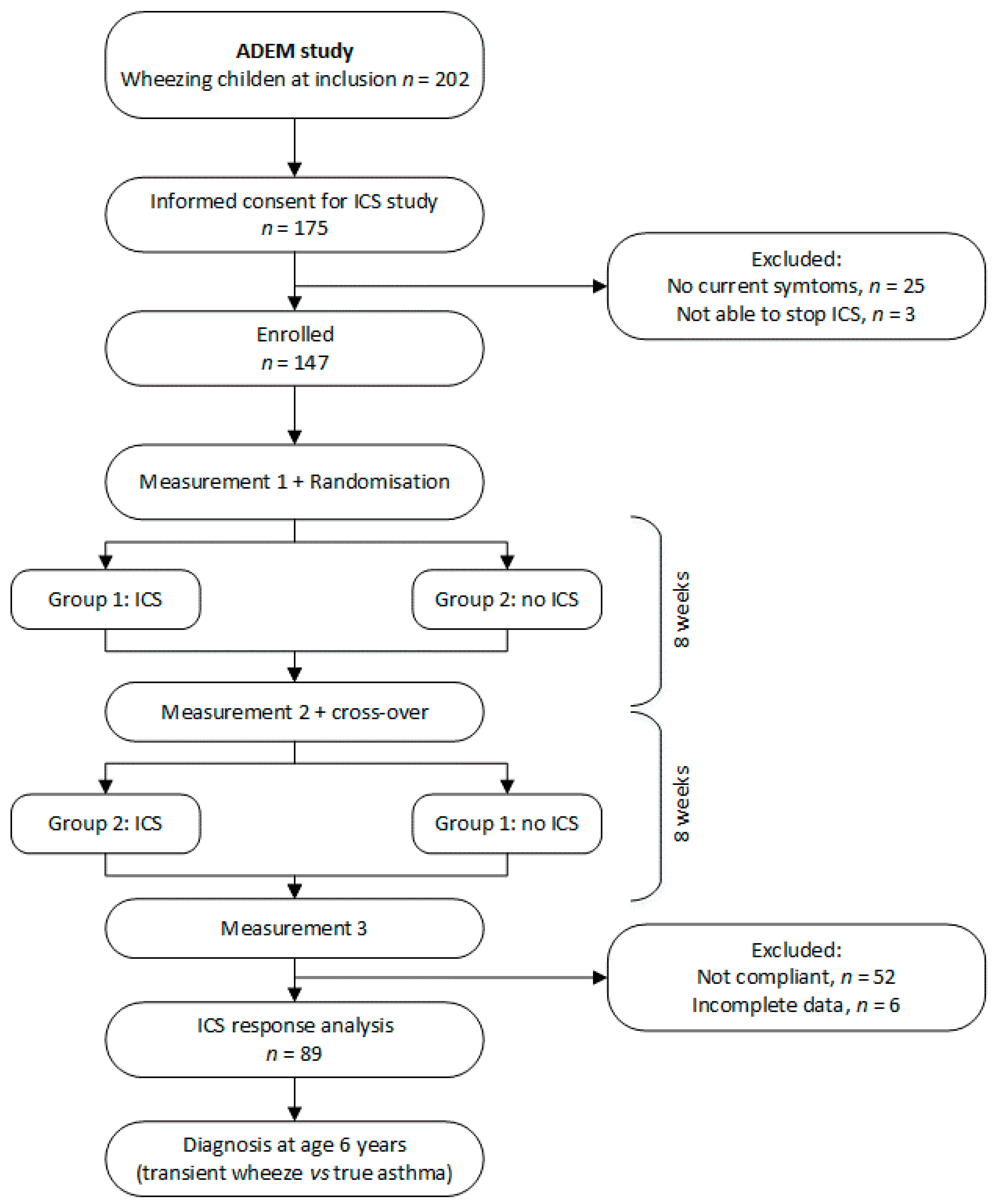
2.1. Study Design
2.2. Response to ICS
2.3. Exhaled Breath Sampling and Measurements
2.4. Data Pre-Processing
3. Results
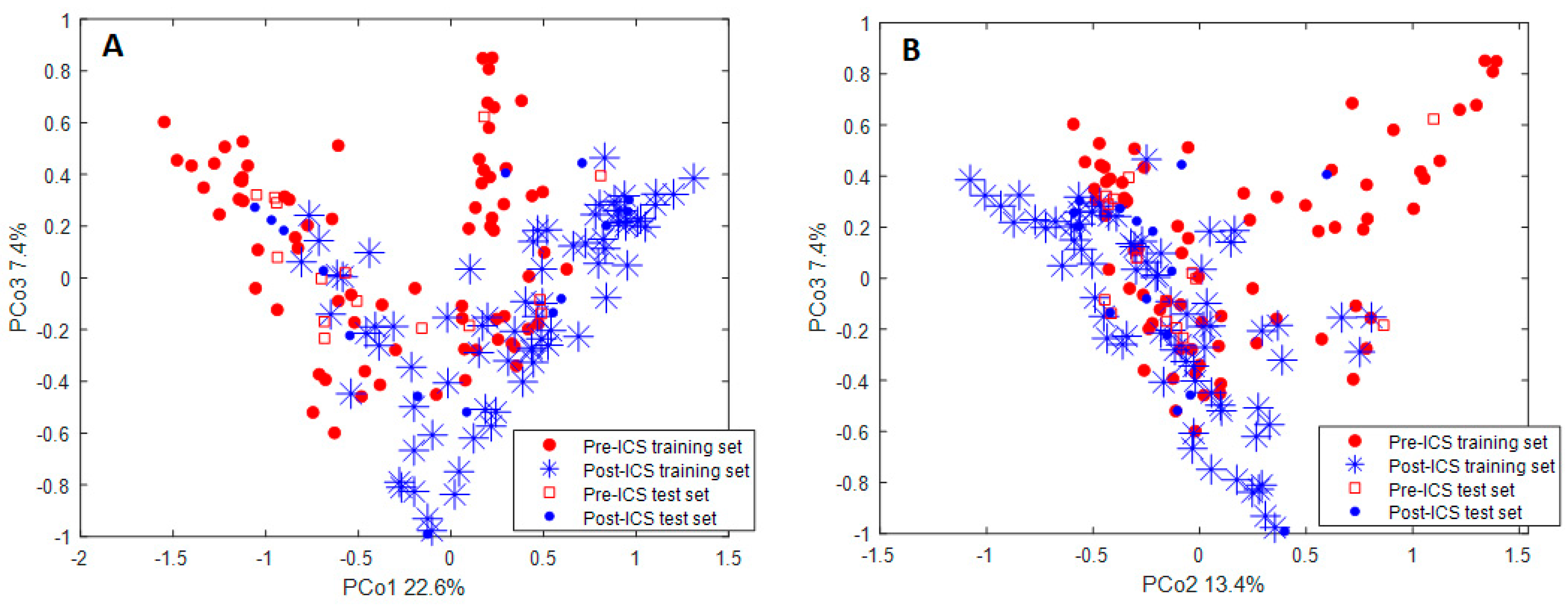
3.1. Influence of ICS on Exhaled VOCs
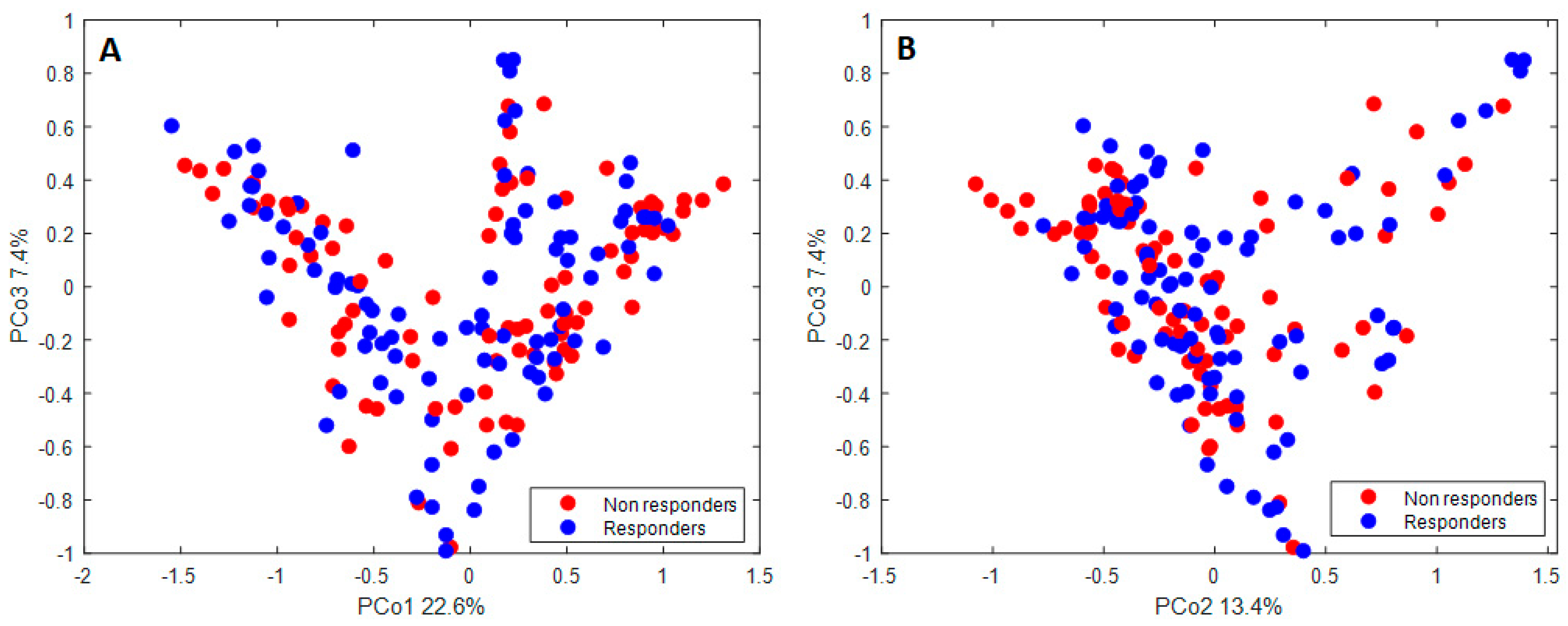
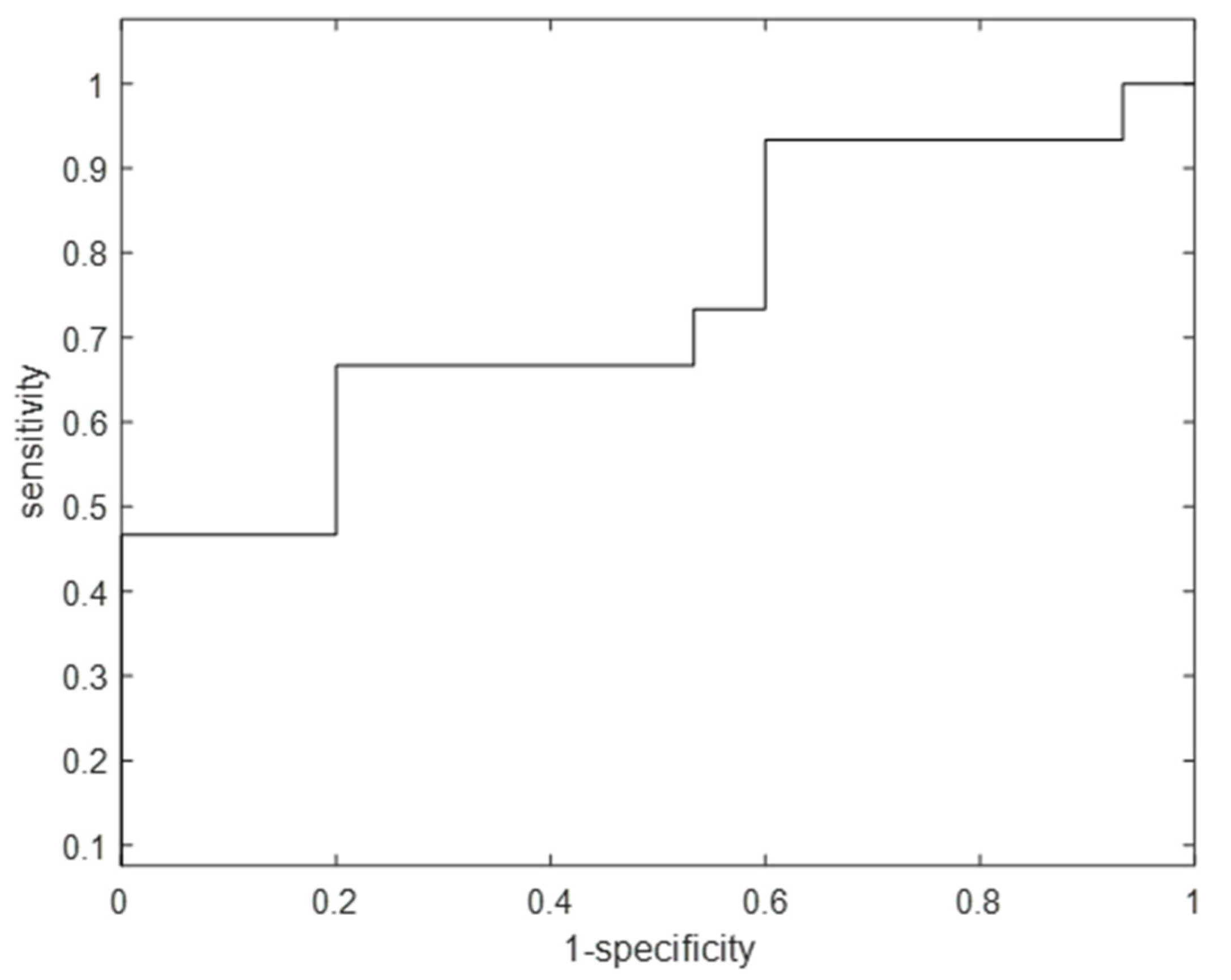
3.2. Exhaled VOCs and Clinical Response to ICS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Ibrahim, W.; Carr, L.; Cordell, R.; Wilde, M.J.; Salman, D.; Monks, P.S.; Thomas, P.; Brightling, C.E.; Siddiqui, S.; Greening, N.J. Breathomics for the clinician: The use of volatile organic compounds in respiratory diseases. Thorax 2021, 76, 514–521. [Google Scholar] [CrossRef]
- Van De Kant, K.D.G.; Van Berkel, J.J.B.N.; Jöbsis, Q.; Passos, V.L.; Klaassen, E.M.M.; Van Der Sande, L.; Van Schayck, O.C.P.; De Jongste, J.C.; Van Schooten, F.J.; Derks, E.; et al. Exhaled breath profiling in diagnosing wheezy preschool children. Eur. Respir. J. 2013, 41, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Dallinga, J.W.; Robroeks, C.M.H.H.T.; Van Berkel, J.J.B.N.; Moonen, E.J.C.; Godschalk, R.W.L.; Jöbsis, Q.; Dompeling, E.; Wouters, E.F.M.; Van Schooten, F.J. Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin. Exp. Allergy 2010, 40, 68–76. [Google Scholar] [CrossRef]
- Robroeks, C.M.; van Berkel, J.J.; Jöbsis, Q.; van Schooten, F.-J.; Dallinga, J.W.; Wouters, E.F.; Dompeling, E. Exhaled volatile organic compounds predict exacerbations of childhood asthma in a 1-year prospective study. Eur. Respir. J. 2013, 42, 98–106. [Google Scholar] [CrossRef]
- Van Vliet, D.; Smolinska, A.; Jöbsis, Q.; Rosias, P.; Muris, J.; Dallinga, J.; Dompeling, E.; Van Schooten, F.-J. Can exhaled volatile organic compounds predict asthma exacerbations in children? J. Breath Res. 2017, 11, 16016. [Google Scholar] [CrossRef]
- Klaassen, E.M.M.; van de Kant, K.D.G.; Jöbsis, Q.; van Schayck, O.C.P.; Smolinska, A.; Dallinga, J.W.; van Schooten, F.J.; den Hartog, G.J.M.; de Jongste, J.C.; Rijkers, G.T.; et al. Exhaled Biomarkers and Gene Expression at Preschool Age Improve Asthma Prediction at 6 Years of Age. Am. J. Respir. Crit. Care Med. 2015, 191, 201–207. [Google Scholar] [CrossRef]
- Horvath, I.; Barnes, P.J.; Loukides, S.; Sterk, P.J.; Hogman, M.; Olin, A.C.; Amann, A.; Antus, B.; Baraldi, E.; Bikov, A.; et al. A European Respiratory Society technical standard: Exhaled biomarkers in lung disease. Eur. Respir. J. 2017, 49, 1600965. [Google Scholar] [CrossRef]
- van der Schee, M.P.; Palmay, R.; Cowan, J.O.; Taylor, D.R. Predicting steroid responsiveness in patients with asthma using exhaled breath profiling. Clin. Exp. Allergy 2013, 43, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, P.; Van De Pol, M.A.; Gerritsen, M.G.; Bos, L.; Dekker, T.; Smids, B.S.; Sinha, A.; Majoor, C.; Sneeboer, M.M.; Knobel, H.H.; et al. Exhaled breath profiles in the monitoring of loss of control and clinical recovery in asthma. Clin. Exp. Allergy 2017, 47, 1159–1169. [Google Scholar] [CrossRef]
- Fitzpatrick, A.M.; Jackson, D.J.; Mauger, D.T.; Boehmer, S.J.; Phipatanakul, W.; Sheehan, W.J.; Moy, J.N.; Paul, I.M.; Bacharier, L.B.; Cabana, M.D.; et al. Individualized therapy for persistent asthma in young children. J. Allergy Clin. Immunol. 2016, 138, 1608–1618.e12. [Google Scholar] [CrossRef] [Green Version]
- Saglani, S.; Bingham, Y.; Balfour-Lynn, I.; Goldring, S.; Gupta, A.; Banya, W.; Moreiras, J.; Fleming, L.; Bush, A.; Rosenthal, M. Blood eosinophils in managing preschool wheeze: Lessons learnt from a proof-of-concept trial. Pediatr. Allergy Immunol. 2022, 33, e13697. [Google Scholar] [CrossRef] [PubMed]
- Van De Kant, K.D.; Klaassen, E.M.; Jöbsis, Q.; Nijhuis, A.J.; Van Schayck, O.C.; Dompeling, E. Early diagnosis of asthma in young children by using non-invasive biomarkers of airway inflammation and early lung function measurements: Study protocol of a case-control study. BMC Public Health 2009, 9, 210. [Google Scholar] [CrossRef] [PubMed]
- Van De Kant, K.D.G.; Koers, K.; Rijkers, G.T.; Passos, V.L.; Klaassen, E.M.M.; Mommers, M.; Dagnelie, P.C.; Van Schayck, C.P.; Dompeling, E.; Jöbsis, Q. Can exhaled inflammatory markers predict a steroid response in wheezing preschool children? Clin. Exp. Allergy 2011, 41, 1076–1083. [Google Scholar] [CrossRef]
- Smolinska, A.; Klaassen, E.M.M.; Dallinga, J.W.; Van De Kant, K.D.G.; Jobsis, Q.; Moonen, E.J.C.; Van Schayck, O.C.P.; Dompeling, E.; Van Schooten, F.J. Profiling of Volatile Organic Compounds in Exhaled Breath as a Strategy to Find Early Predictive Signatures of Asthma in Children. PLoS ONE 2014, 9, e95668. [Google Scholar] [CrossRef]
- Engel, J.; Blanchet, L.; Bloemen, B.; van den Heuvel, L.P.; Engelke, U.H.; Wevers, R.A.; Buydens, L.M. Regularized MANOVA (rMANOVA) in untargeted metabolomics. Anal. Chim Acta 2015, 899, 1–12. [Google Scholar] [CrossRef] [PubMed]
- DDaszykowski, M.; Walczak, B.; Massart, D.L. Representative subset selection. Anal. Chim. Acta 2002, 468, 91–103. [Google Scholar] [CrossRef]
- Gaugg, M.T.; Engler, A.; Nussbaumer-Ochsner, Y.; Bregy, L.; Stöberl, A.S.; Gaisl, T.; Bruderer, T.; Zenobi, R.; Kohler, M.; Sinues, P.M.-L. Metabolic effects of inhaled salbutamol determined by exhaled breath analysis. J. Breath Res. 2017, 11, 46004. [Google Scholar] [CrossRef]
- Brinkman, P.; Ahmed, W.M.; Gómez, C.; Knobel, H.H.; Weda, H.; Vink, T.J.; Nijsen, T.M.; Wheelock, C.E.; Dahlen, S.-E.; Montuschi, P.; et al. Exhaled volatile organic compounds as markers for medication use in asthma. Eur. Respir. J. 2020, 55, 1900544. [Google Scholar] [CrossRef]
- Carraro, S.; Giordano, G.; Reniero, F.; Carpi, D.; Stocchero, M.; Sterk, P.; Baraldi, E. Asthma severity in childhood and metabolomic profiling of breath condensate. Allergy 2013, 68, 110–117. [Google Scholar] [CrossRef]
- Ferraro, V.A.; Carraro, S.; Pirillo, P.; Gucciardi, A.; Poloniato, G.; Stocchero, M.; Giordano, G.; Zanconato, S.; Baraldi, E. Breathomics in Asthmatic Children Treated with Inhaled Corticosteroids. Metabolites 2020, 10, 390. [Google Scholar] [CrossRef]
- Rufo, J.C.; Madureira, J.; Fernandes, E.O.; Moreira, A. Volatile organic compounds in asthma diagnosis: A systematic review and meta-analysis. Allergy 2016, 71, 175–188. [Google Scholar] [CrossRef]
- Bush, A.; Saglani, S. Medical algorithm: Diagnosis and treatment of preschool asthma. Allergy 2020, 75, 2711–2712. [Google Scholar] [CrossRef]
- Di Cicco, M.; Peroni, D.G.; Ragazzo, V.; Comberiati, P. Application of exhaled nitric oxide (FeNO) in pediatric asthma. Curr. Opin. Allergy Clin. Immunol. 2021, 21, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Rufo, J.C.; Paciencia, I.; Mendes, F.C.; Farraia, M.; Rodolfo, A.; Silva, D.; de Oliveira Fernandes, E.; Delgado, L.; Moreira, A. Exhaled breath condensate volatilome allows sensitive diagnosis of persistent asthma. Allergy 2019, 74, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Klok, T.; Kaptein, A.A.; Brand, P.L.P. Non-adherence in children with asthma reviewed: The need for improvement of asthma care and medical education. Pediatr. Allergy Immunol. 2015, 26, 197–205. [Google Scholar] [CrossRef] [PubMed]
| Responders | Non-Responders | |
|---|---|---|
| Study population (N) | 46 | 43 |
| Age (years), mean (SD) | 3.2 (0.7) | 3.4 (0.6) |
| Sex: male/female, n/n | 20/26 | 25/18 |
| Wheezing episodes, n (IQR) | 8 (3–8) | 8 (3–8) |
| Atopy, n/n (%) | 12/45 (27) | 9/41 (22) |
| Allergic rhinitis, n/n (%) | 3/45 (7) | 3/42 (7) |
| Eczema, n/n (%) | 15/44 (34) | 12/43 (28) |
| Positive API, n (%) | 5/44 (11) | 4/43 (9) |
| Inhaled corticosteroids, n/n (%) | 12/45 (27) | 9/42 (21) |
| Short acting β2-agonists, n/n (%) | 23/46 (50) | 19/42 (45) |
| Long acting β2-agonists, n/n (%) | 1/46 (2) | 0/42 (0) |
| Total symptom score, mean (SD) | 24.7 (5.2) | 26.4 (3.1) |
| Airway resistance (kPa s/L), mean (SD) * | 1.6 (0.4) | 1.4 (0.3) |
| Nr. | Compound Name | Concentration Changes in Post-ICS |
|---|---|---|
| 1 | Branched C11H24 | ↓ |
| 2 | Butanal | ↓ |
| 3 | Octanal | ↓ |
| 4 | Acetic acid (ester) | ↑ |
| 5 | Methylated pentane | ↓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bannier, M.A.G.E.; Kienhorst, S.; Jöbsis, Q.; van de Kant, K.D.G.; van Schooten, F.-J.; Smolinska, A.; Dompeling, E. Exhaled Breath Analysis for Investigating the Use of Inhaled Corticosteroids and Corticosteroid Responsiveness in Wheezing Preschool Children. J. Clin. Med. 2022, 11, 5160. https://doi.org/10.3390/jcm11175160
Bannier MAGE, Kienhorst S, Jöbsis Q, van de Kant KDG, van Schooten F-J, Smolinska A, Dompeling E. Exhaled Breath Analysis for Investigating the Use of Inhaled Corticosteroids and Corticosteroid Responsiveness in Wheezing Preschool Children. Journal of Clinical Medicine. 2022; 11(17):5160. https://doi.org/10.3390/jcm11175160
Chicago/Turabian StyleBannier, Michiel A. G. E., Sophie Kienhorst, Quirijn Jöbsis, Kim D. G. van de Kant, Frederik-Jan van Schooten, Agnieszka Smolinska, and Edward Dompeling. 2022. "Exhaled Breath Analysis for Investigating the Use of Inhaled Corticosteroids and Corticosteroid Responsiveness in Wheezing Preschool Children" Journal of Clinical Medicine 11, no. 17: 5160. https://doi.org/10.3390/jcm11175160
APA StyleBannier, M. A. G. E., Kienhorst, S., Jöbsis, Q., van de Kant, K. D. G., van Schooten, F.-J., Smolinska, A., & Dompeling, E. (2022). Exhaled Breath Analysis for Investigating the Use of Inhaled Corticosteroids and Corticosteroid Responsiveness in Wheezing Preschool Children. Journal of Clinical Medicine, 11(17), 5160. https://doi.org/10.3390/jcm11175160






