Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review
Abstract
:1. Introduction
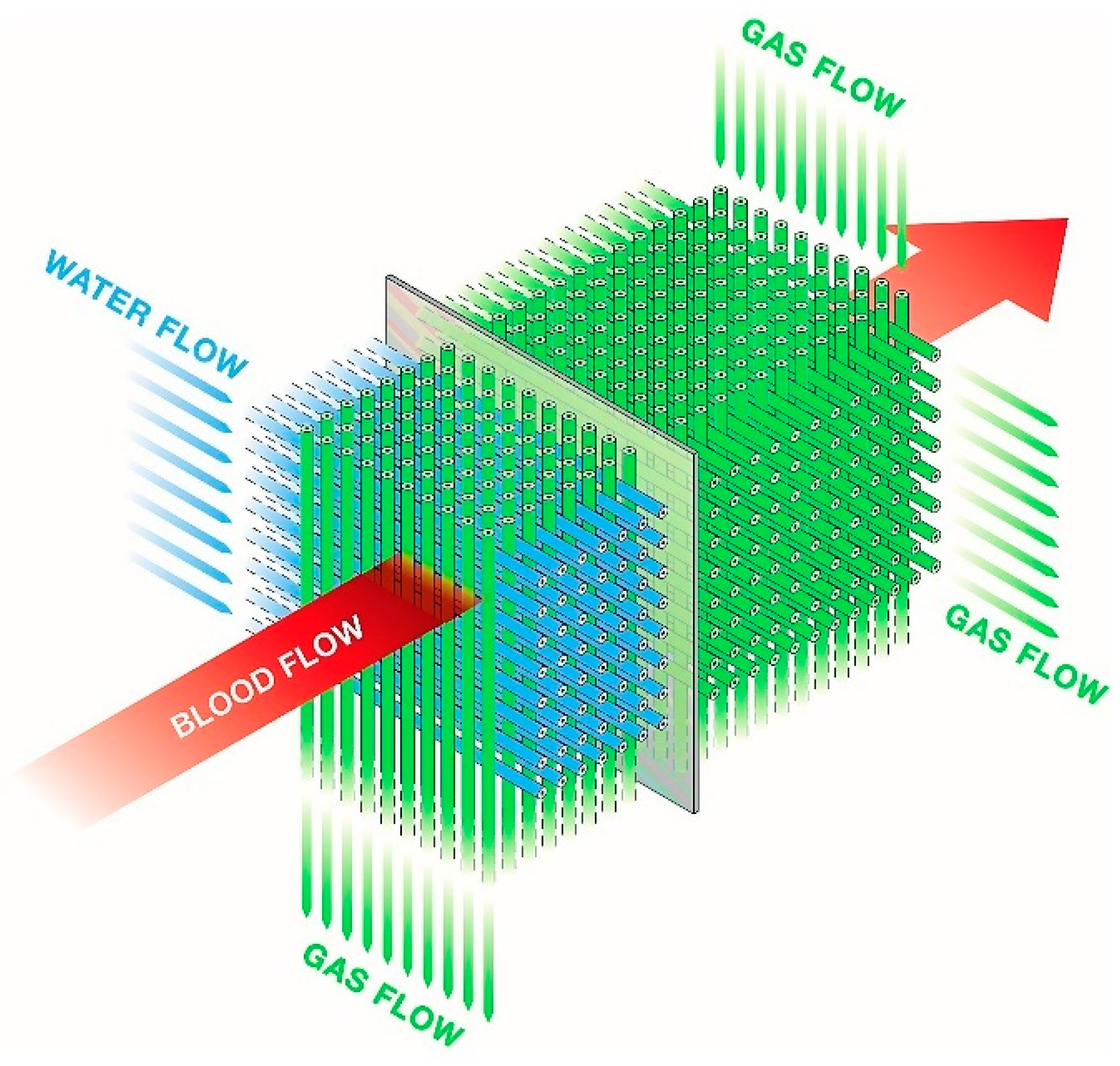
2. ECMO Configurations and Circuits
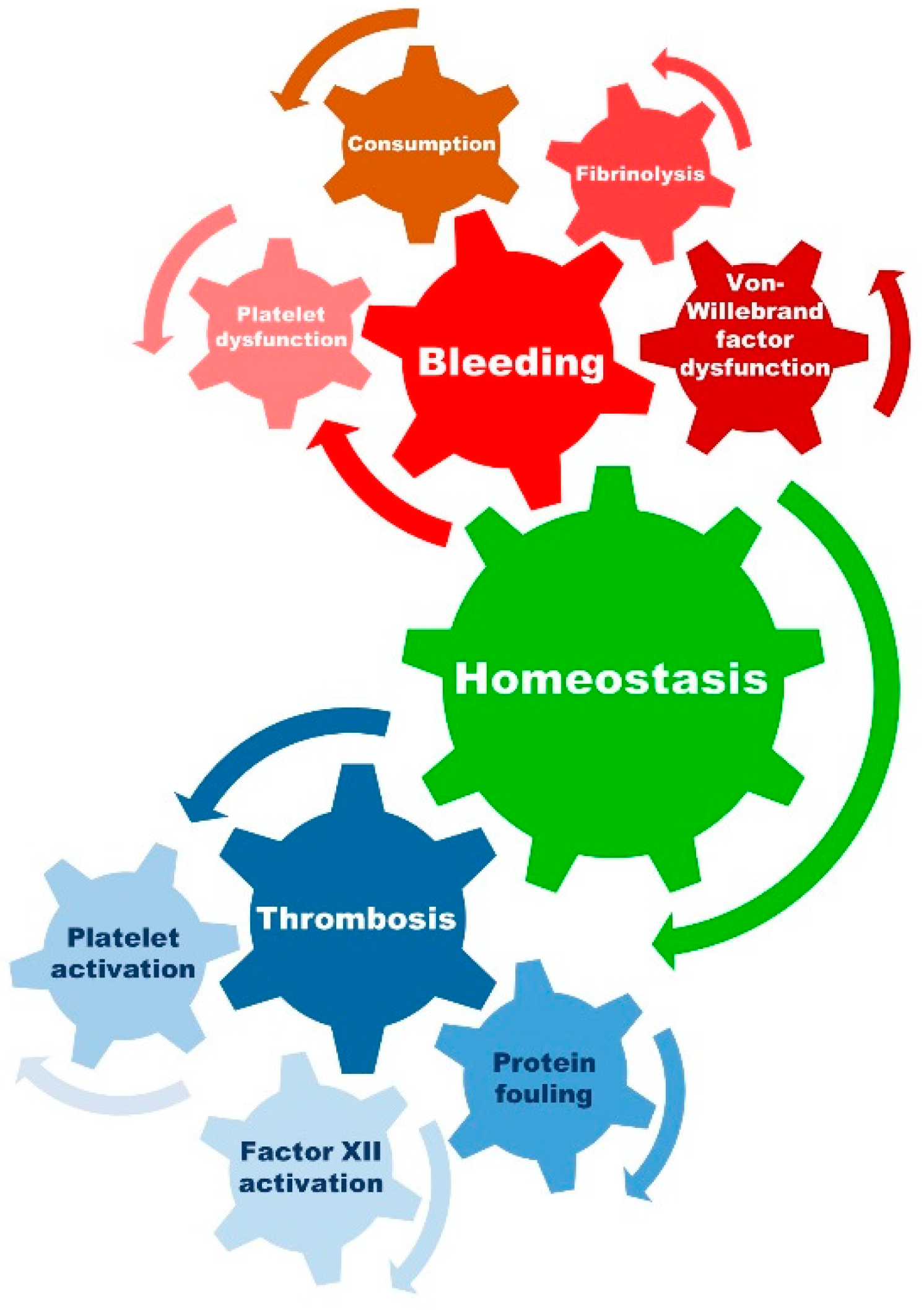
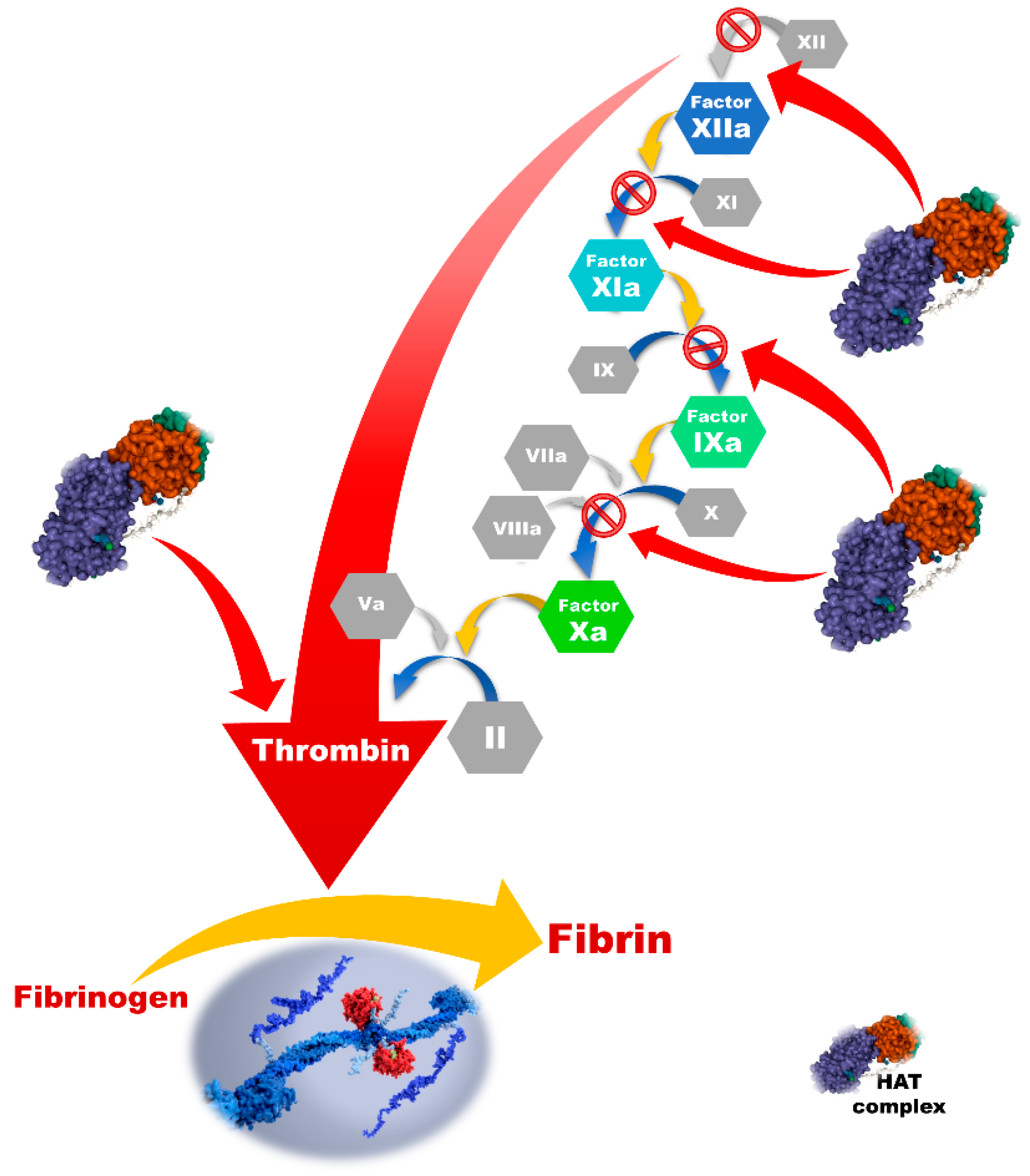
3. Inflammation, Coagulation, and ECMO
4. Anticoagulation Strategies
4.1. Heparin Products
4.1.1. Unfractionated Heparin (UFH)
4.1.2. Low-Molecular-Weight Heparins (LMWH)
4.1.3. Heparin-Coated ECMO Circuits
4.1.4. Heparin Resistance and Antithrombin Deficiency
4.1.5. Heparin-Induced Thrombocytopenia
4.2. Direct Thrombin Inhibitors (DTI)
4.3. Direct and Indirect Factor Xa Inhibitors
4.4. Heparinoids
4.5. Factor XIIa Inhibitors, Nitric Oxide, and Circuit Releasing Compounds
4.6. Citrate
4.7. Antiaggregant Therapy during ECMO Support
4.8. Anticoagulation Free ECMO Support
| Anticoagulant | Mechanism of Action | Monitoring * | Characteristics |
|---|---|---|---|
| Heparin products | |||
| Unfractionated heparin (UFH) | Predominantly inactivating thrombin | aPTT ACT anti-Xa | Half-life: 60–90 min Metabolism: Reticuloendothelial system and the kidneys Antidote: Protamine Advantages: low costs; does not destabilize already existing clots; point-of-care testing possible Disadvantages: Antithrombin dependent; binds to other plasma proteins; heparin resistance and heparin-induced thrombocytopenia |
| Low-molecular-weight heparins (LMWH) | Predominantly inactivating factor Xa | Anti-Xa | Half-life: 3–6 h Metabolism/elimination: Kidneys Antidote: Protamine (only partially effective) Advantages: low costs; does not destabilize already existing clots; binds less to other plasma proteins; no need for monitoring in selected patient groups Disadvantages: Antithrombin dependent; kidney dysfunction |
| Direct thrombin inhibitors (DTI) | |||
| Argatroban | Direct thrombin inhibitor | aPTT ACT Blood drug levels | Half-life: 45 min Metabolism: Liver-dependent Antidote: None Advantages: Independent of antithrombin Disadvantages: Potential destabilization of already existing clots; liver dysfunction; higher costs |
| Bivalirudin | Direct thrombin inhibitor | aPTT ACT | Half-life: 25 min Metabolism: proteolytic degeneration and partial renal excretion Antidote: None Advantages: Independent of antithrombin Disadvantages: Potential destabilization of already existing clots; kidney dysfunction; higher costs |
| Direct factor Xa inhibitors (Rivaroxaban, edoxaban, apixaban) | Inhibition of factor Xa | anti-Xa | Half-life: 5–12 h Metabolism: Oxidative degradation and hydrolysis Antidote: Andexanet alfa Advantages: Independent of antithrombin Disadvantages: Only case reports available for ECMO patients; formulation for oral application available |
| Indirect factor Xa inhibitor (Fondaparinux) | Indirect inhibition of factor Xa | anti-Xa | Half-life: 13–21 h Metabolism: Kidney Antidote: None Advantages: Safe in HIT Disadvantages: Antithrombin dependent; only case reports available for ECMO patients |
| Heparinoids (Danaparoid) | Factor Xa and IIa inhibition | anti-Xa | Half-life: 25 h Metabolism: Kidney Antidote: None Advantages: Safe in HIT Disadvantages: Antithrombin dependent; only case reports available for ECMO patients |
5. Anticoagulation Monitoring
5.1. Activated Clotting Time (ACT)
5.2. Activated Partial Thromboplastin Time (aPTT)
5.3. Anti-Factor Xa Activity Levels (Anti-Xa)
5.4. Viscoelastic Testing
5.5. Antithrombin Monitoring and Substitution
6. Cost of Anticoagulation
7. Future Perspectives and Conclusions
| Surface Modification | Representative (Manufacturer) | Mechanism of Action and Main Characteristics |
|---|---|---|
| Biopassive coatings | ||
| Albumin and recombinant human albumin | X-EED (Xenios), Safeline (Maquet) | Passivation as the main mechanism of action. One of the first proteins used for coating; increases the hydrophilicity; reduces platelets and fibrinogen concentration on the surface; has potential to reduce complement activation |
| Poly-2-methoxyethylacrylate (PMEA) | X-coating (Terumo) | Reduced platelet adhesion and protein denaturation as the main mechanism of action. Inferior hemocompatibility compared to Bioline, Phisio, and Trillium; causes transient leukopenia; reduction in platelet and leukocyte activation and adhesion, reduced coagulation and complement activation, reduced inflammation markers. Compared to other coatings, observed increase in ventilator time and chest tube output |
| Polyethylene glycol | E8 (Nipro) | Hydrophilicity as the main mechanism of action. Reduction in aggregation and reduction in inflammatory response |
| Phosphorylcholine | AGILE (Eurosets), Phisio (Sorin) | Cell membrane mimic as the main mechanism of action. Nonthrombogenic; reduced platelet and fibrinogen binding through GPIIb receptor; reduced complement activation; antifouling properties; reduction in other inflammatory markers; may increase immune cell response (T-cells) |
| Under development | ||
| Tethered liquid perfluorocarbon (omniphobic surfaces) | Tethered liquid perfluorocarbon | Slippery liquid barrier layer is the main mechanism of action. Low adsorption and adhesion of plasma proteins; reduced physico-chemical interactions with the surface; in vitro experiments showed improved prevention of thrombus deposition compared to standard heparin-coated surfaces; data origin from extracorporeal circuits and animal studies |
| Zwitterionic polymers | SB-co-methacrylic acid block copolymer, 2-methacryloyloxyethyl phosphorylcholine, | Hydrophilicity as the main mechanism of action, originally inspired by phosphorylcholine. Decreased bovine serum albumin and fibrinogen absorption and platelet adhesion; prolonged aPTT compared to pristine surfaces under static conditions: data origin from extracorporeal circuits and animal studies |
| Bioactive coatings | ||
| Heparin | Cortiva BioActive Surface (Medtronic), Rheoparin (Xenios), Hepaface (Terumo) | Heparin as anticoagulant. Reduced thrombin production; platelet binding; and D-dimer production; reduced inflammatory response and complement activation; majority of evidence originate from the cardiopulmonary bypass; danger of HIT II; heparin leach; oxygenator swelling and occlusion in case of ionic binding (covalent binding without leaching of heparin) |
| Under development | ||
| Heparin-based coatings | T-NCVC coating | Hydrophobic properties; limited heparin leaching; high antithrombogenicity and long-term durability; data origin from extracorporeal circuits and animal studies |
| Heparin coupled polyethylene glycol grafted polysulfone membranes | Improvement in hemocompatibility (albumin and fibrinogen adsorption and platelet adhesion) compared to noncoated membranes; no studies with comparison to heparin-only coated membranes available | |
| Antithrombin-heparin covalent complex | Higher antithrombotic activity; inhibition of clot-bound thrombin and longer half-life in the circulation compared to heparin | |
| Nitric oxide releasing coatings Combination of nitric oxide and other anticoagulants (argatroban) | Inhibition of platelet and leucocyte activation; inhibition of platelet adhesion; improved endothelial mimetic microenvironment; lower fibrinogen consumption. Improved hemocompatibility in combination with other anticoagulants; data origin from extracorporeal circuits and animal studies; molecule leaching with nitrosamines release in the blood; the nitric oxide storage last for only 4 weeks; no commercial use until now; undergoing studies on endogenous nitric oxide reservoirs (e.g., nanotechnology, metal-organic frameworks, etc.) | |
| Complement inhibitors | C1- esterase inhibitor coating | Improved reduction in factor XIIa activity compared to heparin coatings; C1- esterase inhibitor/heparin coating showed promising results in platelet adhesion and fibrin networks inhibition; data origin from extracorporeal circuits studies |
| Combination | ||
| Heparin and albumin | Bioline (Maquet) | Anticoagulation and passivation as the main mechanism of action. Improved hemocompatibility; reduced complement activation and reduction in other inflammatory markers |
| Polyethylene oxide/sulphate/sulfonate groups with or without heparin | Balance and Trillium Biosurface (Medtronic) | Hydrophilicity, negative charge, and anticoagulant mechanism of action. Reduced protein (both fibrinogen and albumin) and bacterial adhesion; reduction in inflammatory markers; reduction in bleeding events; mimicking endothelium; negative charge dependent platelets repletion and inhibition of thrombin; preserved platelet count; increases the stroke rate in cardiopulmonary bypass; evidence from small and single center studies, missing long-term evaluation |
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Featherstone, P.J.; Ball, C.M. The early history of extracorporeal membrane oxygenation. Anaesth. Intensive Care 2018, 46, 555–557. [Google Scholar] [CrossRef] [PubMed]
- Shekar, K.; Mullany, D.V.; Thomson, B.; Ziegenfuss, M.; Platts, D.G.; Fraser, J.F. Extracorporeal life support devices and strategies for management of acute cardiorespiratory failure in adult patients: A comprehensive review. Crit. Care 2014, 18, 219. [Google Scholar] [CrossRef] [PubMed]
- Schechter, M.A.; Ganapathi, A.M.; Englum, B.R.; Speicher, P.J.; Daneshmand, M.A.; Davis, R.D.; Hartwig, M.G. Spontaneously Breathing Extracorporeal Membrane Oxygenation Support Provides the Optimal Bridge to Lung Transplantation. Transplantation 2016, 100, 2699–2704. [Google Scholar] [CrossRef]
- Kim, H.; Cho, Y.H. Role of extracorporeal cardiopulmonary resuscitation in adults. Acute Crit. Care 2020, 35, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, L.; Qin, T.; Xi, Z.; Sun, L.; Wu, H.; Li, D. Extracorporeal membrane oxygenation in trauma patients: A systematic review. World J. Emerg. Surg. 2020, 15, 51. [Google Scholar] [CrossRef]
- Morley, D.; Yamane, K.; O’Malley, R.; Cavarocchi, N.C.; Hirose, H. Rewarming for accidental hypothermia in an urban medical center using extracorporeal membrane oxygenation. Am. J. Case Rep. 2013, 14, 6–9. [Google Scholar] [CrossRef]
- Bougouin, W.; Dumas, F.; Lamhaut, L.; Marijon, E.; Carli, P.; Combes, A.; Pirracchio, R.; Aissaoui, N.; Karam, N.; Deye, N.; et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: A registry study. Eur. Heart J. 2020, 41, 1961–1971. [Google Scholar] [CrossRef]
- Inoue, A.; Hifumi, T.; Sakamoto, T.; Kuroda, Y. Extracorporeal Cardiopulmonary Resuscitation for Out-of-Hospital Cardiac Arrest in Adult Patients. J. Am. Heart Assoc. 2020, 9, e015291. [Google Scholar] [CrossRef]
- Scquizzato, T.; Bonaccorso, A.; Consonni, M.; Scandroglio, A.M.; Swol, J.; Landoni, G.; Zangrillo, A. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: A systematic review and meta-analysis of randomized and propensity score-matched studies. Artif. Organs 2022, 46, 755–762. [Google Scholar] [CrossRef]
- Downing, J.; Al Falasi, R.; Cardona, S.; Fairchild, M.; Lowie, B.; Chan, C.; Powell, E.; Pourmand, A.; Tran, Q.K. How effective is extracorporeal cardiopulmonary resuscitation (ECPR) for out-of-hospital cardiac arrest? A systematic review and meta-analysis. Am. J. Emerg. Med. 2022, 51, 127–138. [Google Scholar] [CrossRef]
- Extracorporeal Life Support Organization (ELSO). Registry Report on Extracorporeal Life Support, International Summary. Available online: https://www.elso.org/Registry/InternationalSummaryandReports/InternationalSummary.aspx (accessed on 8 July 2022).
- Millar, J.E.; Fanning, J.P.; McDonald, C.I.; McAuley, D.F.; Fraser, J.F. The inflammatory response to extracorporeal membrane oxygenation (ECMO): A review of the pathophysiology. Crit. Care 2016, 20, 387. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Oezpeker, U.C.; Bukumirić, Z.; Dobesberger, M.; Treml, B. The Role of Excessive Anticoagulation and Missing Hyperinflammation in ECMO-Associated Bleeding. J. Clin. Med. 2022, 11, 2314. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, J.; Anand, S.S.; Halperin, J.L.; Fuster, V. Mechanism of action and pharmacology of unfractionated heparin. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 1094–1096. [Google Scholar] [CrossRef]
- Aubron, C.; DePuydt, J.; Belon, F.; Bailey, M.; Schmidt, M.; Sheldrake, J.; Murphy, D.; Scheinkestel, C.; Cooper, D.J.; Capellier, G.; et al. Predictive factors of bleeding events in adults undergoing extracorporeal membrane oxygenation. Ann. Intensive Care 2016, 6, 97. [Google Scholar] [CrossRef]
- Treml, B.; Breitkopf, R.; Bukumirić, Z.; Bachler, M.; Boesch, J.; Rajsic, S. ECMO Predictors of Mortality: A 10-Year Referral Centre Experience. J. Clin. Med. 2022, 11, 1224. [Google Scholar] [CrossRef]
- Levy, J.H.; Staudinger, T.; Steiner, M.E. How to manage anticoagulation during extracorporeal membrane oxygenation. Intensive Care Med. 2022, 48, 1076–1079. [Google Scholar] [CrossRef] [PubMed]
- Abruzzo, A.; Gorantla, V.; Thomas, S.E. Venous thromboembolic events in the setting of extracorporeal membrane oxygenation support in adults: A systematic review. Thromb. Res. 2022, 212, 58–71. [Google Scholar] [CrossRef]
- Deshpande, S.R.; Hastings, S.; Wagoner, S.; Ku, D.; Maher, K. New Insights into Thrombosis in ECMO: Circuits: Where, How and Why? J. Heart Lung Transplant. 2015, 34, S87–S88. [Google Scholar] [CrossRef]
- Brasseur, A.; Scolletta, S.; Lorusso, R.; Taccone, F.S. Hybrid extracorporeal membrane oxygenation. J. Thorac. Dis. 2018, 10, S707–S715. [Google Scholar] [CrossRef]
- Brogan, T.V.; Lequier, L.; Lorusso, R.; MacLaren, G.; Peek, G.J. Extracorporeal Life Support: The ELSO Red Book, 5th ed.; Extracorporeal Life Support Organization: Ann Arbor, MI, USA, 2017; p. 831. [Google Scholar]
- Khan, S.; Vasavada, R.; Qiu, F.; Kunselman, A.; Undar, A. Extracorporeal life support systems: Alternative vs. conventional circuits. Perfusion 2011, 26, 191–198. [Google Scholar] [CrossRef]
- Palanzo, D.; Qiu, F.; Baer, L.; Clark, J.B.; Myers, J.L.; Undar, A. Evolution of the extracorporeal life support circuitry. Artif. Organs 2010, 34, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Iwahashi, H.; Yuri, K.; Nosé, Y. Development of the oxygenator: Past, present, and future. J. Artif. Organs 2004, 7, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Diehl, A.; Pellegrino, V.; Sheldrake, J. ECMO Guideline. Available online: https://ecmo.icu/#menuRoot (accessed on 9 July 2022).
- Warren, O.J.; Smith, A.J.; Alexiou, C.; Rogers, P.L.; Jawad, N.; Vincent, C.; Darzi, A.W.; Athanasiou, T. The inflammatory response to cardiopulmonary bypass: Part 1—Mechanisms of pathogenesis. J. Cardiothorac. Vasc. Anesth. 2009, 23, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Warren, O.J.; Watret, A.L.; de Wit, K.L.; Alexiou, C.; Vincent, C.; Darzi, A.W.; Athanasiou, T. The inflammatory response to cardiopulmonary bypass: Part 2—Anti-inflammatory therapeutic strategies. J. Cardiothorac. Vasc. Anesth. 2009, 23, 384–393. [Google Scholar] [CrossRef]
- Landis, R.C.; Brown, J.R.; Fitzgerald, D.; Likosky, D.S.; Shore-Lesserson, L.; Baker, R.A.; Hammon, J.W. Attenuating the Systemic Inflammatory Response to Adult Cardiopulmonary Bypass: A Critical Review of the Evidence Base. J. Extra-Corpor. Technol. 2014, 46, 197–211. [Google Scholar]
- Paparella, D.; Yau, T.M.; Young, E. Cardiopulmonary bypass induced inflammation: Pathophysiology and treatment. An update. Eur. J. Cardio-Thorac. Surg. 2002, 21, 232–244. [Google Scholar] [CrossRef]
- Warltier, D.C.; Laffey, J.G.; Boylan, J.F.; Cheng, D.C.H. The Systemic Inflammatory Response to Cardiac Surgery: Implications for the Anesthesiologist. Anesthesiology 2002, 97, 215–252. [Google Scholar] [CrossRef]
- Conway, E.M. Thrombomodulin and its role in inflammation. Semin. Immunopathol. 2012, 34, 107–125. [Google Scholar] [CrossRef]
- Moore, K.L.; Esmon, C.T.; Esmon, N.L. Tumor necrosis factor leads to the internalization and degradation of thrombomodulin from the surface of bovine aortic endothelial cells in culture. Blood 1989, 73, 159–165. [Google Scholar] [CrossRef]
- Lindmark, E.; Tenno, T.; Siegbahn, A. Role of platelet P-selectin and CD40 ligand in the induction of monocytic tissue factor expression. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 2322–2328. [Google Scholar] [CrossRef]
- Van de Wouwer, M.; Collen, D.; Conway, E.M. Thrombomodulin-protein C-EPCR system: Integrated to regulate coagulation and inflammation. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1374–1383. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Xu, D.Y.; Jialal, I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: Implications for the metabolic syndrome and atherothrombosis. Circulation 2003, 107, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Wolbink, G.J.; Bossink, A.W.; Groeneveld, A.B.; de Groot, M.C.; Thijs, L.G.; Hack, C.E. Complement activation in patients with sepsis is in part mediated by C-reactive protein. J. Infect. Dis. 1998, 177, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Han, K.H.; Hong, K.H.; Park, J.H.; Ko, J.; Kang, D.H.; Choi, K.J.; Hong, M.K.; Park, S.W.; Park, S.J. C-reactive protein promotes monocyte chemoattractant protein-1--mediated chemotaxis through upregulating CC chemokine receptor 2 expression in human monocytes. Circulation 2004, 109, 2566–2571. [Google Scholar] [CrossRef] [PubMed]
- Cheung, P.Y.; Sawicki, G.; Salas, E.; Etches, P.C.; Schulz, R.; Radomski, M.W. The mechanisms of platelet dysfunction during extracorporeal membrane oxygenation in critically ill neonates. Crit. Care Med. 2000, 28, 2584–2590. [Google Scholar] [CrossRef]
- Hamad, O.A.; Bäck, J.; Nilsson, P.H.; Nilsson, B.; Ekdahl, K.N. Platelets, complement, and contact activation: Partners in inflammation and thrombosis. Adv. Exp. Med. Biol. 2012, 946, 185–205. [Google Scholar] [CrossRef]
- Whiteheart, S.W. Platelet granules: Surprise packages. Blood 2011, 118, 1190–1191. [Google Scholar] [CrossRef]
- Kraft, F.; Schmidt, C.; Van Aken, H.; Zarbock, A. Inflammatory response and extracorporeal circulation. Best Pract. Research. Clin. Anaesthesiol. 2015, 29, 113–123. [Google Scholar] [CrossRef]
- Esmon, C.T. The interactions between inflammation and coagulation. Br. J. Haematol. 2005, 131, 417–430. [Google Scholar] [CrossRef]
- Mulloy, B.; Hogwood, J.; Gray, E.; Lever, R.; Page, C.P. Pharmacology of Heparin and Related Drugs. Pharmacol. Rev. 2016, 68, 76–141. [Google Scholar] [CrossRef]
- Levy, J.H.; Connors, J.M. Heparin Resistance-Clinical Perspectives and Management Strategies. N. Engl. J. Med. 2021, 385, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Doyle, A.J.; Hunt, B.J. Current Understanding of How Extracorporeal Membrane Oxygenators Activate Haemostasis and Other Blood Components. Front. Med. 2018, 5, 352. [Google Scholar] [CrossRef] [PubMed]
- Malhotra Kapoor, P.; Karanjkar, A.; Bhardwaj, V. Evaluation of coagulopathy on veno-arterial ECMO (VA) extracorporeal membrane oxygenation using platelet aggregometry and standard tests: A narrative review. Egypt. J. Crit. Care Med. 2018, 6, 73–78. [Google Scholar] [CrossRef]
- Cartwright, B.; Bruce, H.M.; Kershaw, G.; Cai, N.; Othman, J.; Gattas, D.; Robson, J.L.; Hayes, S.; Alicajic, H.; Hines, A.; et al. Hemostasis, coagulation and thrombin in venoarterial and venovenous extracorporeal membrane oxygenation: The HECTIC study. Sci. Rep. 2021, 11, 7975. [Google Scholar] [CrossRef]
- Ki, K.K.; Passmore, M.R.; Chan, C.H.H.; Malfertheiner, M.V.; Fanning, J.P.; Bouquet, M.; Millar, J.E.; Fraser, J.F.; Suen, J.Y. Low flow rate alters haemostatic parameters in an ex-vivo extracorporeal membrane oxygenation circuit. Intensive Care Med. Exp. 2019, 7, 51. [Google Scholar] [CrossRef]
- Wendel, H.P.; Scheule, A.M.; Eckstein, F.S.; Ziemer, G. Haemocompatibility of paediatric membrane oxygenators with heparin-coated surfaces. Perfusion 1999, 14, 21–28. [Google Scholar] [CrossRef]
- Rodell, T.C.; Naidoo, Y.; Bhoola, K.D. Role of Kinins in Inflammatory Responses. Clin. Immunother. 1995, 3, 352–361. [Google Scholar] [CrossRef]
- Wachtfogel, Y.T.; Hack, C.E.; Nuijens, J.H.; Kettner, C.; Reilly, T.M.; Knabb, R.M.; Bischoff, R.; Tschesche, H.; Wenzel, H.; Kucich, U.; et al. Selective kallikrein inhibitors alter human neutrophil elastase release during extracorporeal circulation. Am. J. Physiol. 1995, 268, H1352–H1357. [Google Scholar] [CrossRef]
- Larsson, M.; Rayzman, V.; Nolte, M.W.; Nickel, K.F.; Björkqvist, J.; Jämsä, A.; Hardy, M.P.; Fries, M.; Schmidbauer, S.; Hedenqvist, P.; et al. A factor XIIa inhibitory antibody provides thromboprotection in extracorporeal circulation without increasing bleeding risk. Sci. Transl. Med. 2014, 6, 222ra217. [Google Scholar] [CrossRef]
- Wallisch, M.; Lorentz, C.U.; Lakshmanan, H.H.S.; Johnson, J.; Carris, M.R.; Puy, C.; Gailani, D.; Hinds, M.T.; McCarty, O.J.T.; Gruber, A.; et al. Antibody inhibition of contact factor XII reduces platelet deposition in a model of extracorporeal membrane oxygenator perfusion in nonhuman primates. Res. Pract. Thromb. Haemost. 2020, 4, 205–216. [Google Scholar] [CrossRef]
- Hayes, D., Jr.; Preston, T.J.; Kirkby, S.; Nicol, K.K. Human leukocyte antigen sensitization in lung transplant candidates supported by extracorporeal membrane oxygenation. Am. J. Respir. Crit. Care Med. 2013, 188, 627–628. [Google Scholar] [CrossRef]
- Ranucci, M.; Ballotta, A.; Di Dedda, U.; Baryshnikova, E.; Dei Poli, M.; Resta, M.; Falco, M.; Albano, G.; Menicanti, L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J. Thromb. Haemost. JTH 2020, 18, 1747–1751. [Google Scholar] [CrossRef]
- Lim, M.S.; McRae, S. COVID-19 and immunothrombosis: Pathophysiology and therapeutic implications. Crit. Rev. Oncol./Hematol. 2021, 168, 103529. [Google Scholar] [CrossRef] [PubMed]
- Ontaneda, A.; Annich, G.M. Novel Surfaces in Extracorporeal Membrane Oxygenation Circuits. Front. Med. 2018, 5, 321. [Google Scholar] [CrossRef] [PubMed]
- Laurance Lequier, G.A.; Omar Al-Ibrahim, M.B.; Dan Brodie, T.B.; Shannon Buckvold, L.C.; Steve Conrad, D.C.; Heidi Dalton, J.F.; Bill Harris, R.M.; Paden, M.; Natalie Rintoul, L.R.; Phil Spinella, J.T.; et al. ELSO Anticoagulation Guideline; ELSO: Ann Arbor, MI, USA, 2014. [Google Scholar]
- Olson, S.R.; Murphree, C.R.; Zonies, D.; Meyer, A.D.; McCarty, O.J.T.; Deloughery, T.G.; Shatzel, J.J. Thrombosis and Bleeding in Extracorporeal Membrane Oxygenation (ECMO) without Anticoagulation: A Systematic Review. ASAIO J. 2021, 67, 290–296. [Google Scholar] [CrossRef] [PubMed]
- McLean, J. The thromboplastic action of cephalin. Am. J. Physiol. Content 1916, 41, 250–257. [Google Scholar] [CrossRef]
- Mclean, J. The Discovery of Heparin. Circulation 1959, 19, 75–78. [Google Scholar] [CrossRef]
- Linhardt, R.J.; Gunay, N.S. Production and chemical processing of low molecular weight heparins. Semin. Thromb. Hemost. 1999, 25 (Suppl. 3), 5–16. [Google Scholar] [PubMed]
- Wolf, H. Low-molecular-weight heparin. Med. Clin. N. Am. 1994, 78, 733–743. [Google Scholar] [CrossRef]
- Rosenberg, R.; Bauer, K. The heparin-antithrombin system: A natural anticoagulant mechanism. In Hemostasis and Thrombosis: Basic Principles and Clinical Practice; Colman, R.W., Hirsh, J., Marder, V.J., Salzman, E.W., Eds.; J.B. Lippincott & Co.: Philadelphia, PA, USA, 1994; Volume 3, pp. 837–860. [Google Scholar]
- Lam, L.H.; Silbert, J.E.; Rosenberg, R.D. The separation of active and inactive forms of heparin. Biochem. Biophys. Res. Commun. 1976, 69, 570–577. [Google Scholar] [CrossRef]
- Andersson, L.O.; Barrowcliffe, T.W.; Holmer, E.; Johnson, E.A.; Sims, G.E. Anticoagulant properties of heparin fractionated by affinity chromatography on matrix-bound antithrombin iii and by gel filtration. Thromb. Res. 1976, 9, 575–583. [Google Scholar] [CrossRef]
- Hirsh, J.; Raschke, R.; Warkentin, T.E.; Dalen, J.E.; Deykin, D.; Poller, L. Heparin: Mechanism of action, pharmacokinetics, dosing considerations, monitoring, efficacy, and safety. Chest 1995, 108, 258s–275s. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.O.; Barrowcliffe, T.W.; Holmer, E.; Johnson, E.A.; Söderström, G. Molecular weight dependency of the heparin potentiated inhibition of thrombin and activated factor X. Effect of heparin neutralization in plasma. Thromb. Res. 1979, 15, 531–541. [Google Scholar] [CrossRef]
- Hirsh, J.; Warkentin, T.E.; Shaughnessy, S.G.; Anand, S.S.; Halperin, J.L.; Raschke, R.; Granger, C.; Ohman, E.M.; Dalen, J.E. Heparin and low-molecular-weight heparin: Mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest 2001, 119, 64s–94s. [Google Scholar] [CrossRef]
- Bembea, M.M.; Annich, G.; Rycus, P.; Oldenburg, G.; Berkowitz, I.; Pronovost, P. Variability in anticoagulation management of patients on extracorporeal membrane oxygenation: An international survey. Pediatr. Crit. Care Med. 2013, 14, e77–e84. [Google Scholar] [CrossRef] [PubMed]
- Kato, C.; Oakes, M.; Kim, M.; Desai, A.; Olson, S.R.; Raghunathan, V.; Shatzel, J.J. Anticoagulation strategies in extracorporeal circulatory devices in adult populations. Eur. J. Haematol. 2021, 106, 19–31. [Google Scholar] [CrossRef]
- Sklar, M.C.; Sy, E.; Lequier, L.; Fan, E.; Kanji, H.D. Anticoagulation Practices during Venovenous Extracorporeal Membrane Oxygenation for Respiratory Failure. A Systematic Review. Ann. Am. Thorac. Soc. 2016, 13, 2242–2250. [Google Scholar] [CrossRef]
- Goligher, E.C.; Bradbury, C.A.; McVerry, B.J.; Lawler, P.R.; Berger, J.S.; Gong, M.N.; Carrier, M.; Reynolds, H.R.; Kumar, A.; Turgeon, A.F.; et al. Therapeutic Anticoagulation with Heparin in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 777–789. [Google Scholar] [CrossRef]
- Geerts, W.H.; Bergqvist, D.; Pineo, G.F.; Heit, J.A.; Samama, C.M.; Lassen, M.R.; Colwell, C.W. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008, 133, 381s–453s. [Google Scholar] [CrossRef]
- Krueger, K.; Schmutz, A.; Zieger, B.; Kalbhenn, J. Venovenous Extracorporeal Membrane Oxygenation with Prophylactic Subcutaneous Anticoagulation Only: An Observational Study in More Than 60 Patients. Artif. Organs 2017, 41, 186–192. [Google Scholar] [CrossRef]
- Prat, N.J.; Meyer, A.D.; Langer, T.; Montgomery, R.K.; Parida, B.K.; Batchinsky, A.I.; Cap, A.P. Low-Dose Heparin Anticoagulation During Extracorporeal Life Support for Acute Respiratory Distress Syndrome in Conscious Sheep. Shock 2015, 44, 560–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gratz, J.; Pausch, A.; Schaden, E.; Baierl, A.; Jaksch, P.; Erhart, F.; Hoetzenecker, K.; Wiegele, M. Low molecular weight heparin versus unfractioned heparin for anticoagulation during perioperative extracorporeal membrane oxygenation: A single center experience in 102 lung transplant patients. Artif. Organs 2020, 44, 638–646. [Google Scholar] [CrossRef]
- Wiegele, M.; Laxar, D.; Schaden, E.; Baierl, A.; Maleczek, M.; Knöbl, P.; Hermann, M.; Hermann, A.; Zauner, C.; Gratz, J. Subcutaneous Enoxaparin for Systemic Anticoagulation of COVID-19 Patients During Extracorporeal Life Support. Front. Med. 2022, 9, 879425. [Google Scholar] [CrossRef] [PubMed]
- Rastan, A.J.; Lachmann, N.; Walther, T.; Doll, N.; Gradistanac, T.; Gommert, J.F.; Lehmann, S.; Wittekind, C.; Mohr, F.W. Autopsy findings in patients on postcardiotomy extracorporeal membrane oxygenation (ECMO). Int. J. Artif. Organs 2006, 29, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Larm, O.; Larsson, R.; Olsson, P. A new non-thrombogenic surface prepared by selective covalent binding of heparin via a modified reducing terminal residue. Biomater. Med. Devices Artif. Organs 1983, 11, 161–173. [Google Scholar] [CrossRef]
- Wendel, H.P.; Ziemer, G. Coating-techniques to improve the hemocompatibility of artificial devices used for extracorporeal circulation. Eur. J. Cardio-Thorac. Surg. 1999, 16, 342–350. [Google Scholar] [CrossRef]
- Steinlechner, B.; Kargl, G.; Schlömmer, C.; Holaubek, C.; Scheriau, G.; Eichinger, S.; Gratz, J.; Rössler, B. Can Heparin-Coated ECMO Cannulas Induce Thrombocytopenia in COVID-19 Patients? Case Rep. Immunol. 2021, 2021, 6624682. [Google Scholar] [CrossRef]
- Anderson, J.A.; Saenko, E.L. Heparin resistance. Br. J. Anaesth. 2002, 88, 467–469. [Google Scholar] [CrossRef]
- Greinacher, A. Heparin-Induced Thrombocytopenia. N. Engl. J. Med. 2015, 373, 252–261. [Google Scholar] [CrossRef]
- Salter, B.S.; Weiner, M.M.; Trinh, M.A.; Heller, J.; Evans, A.S.; Adams, D.H.; Fischer, G.W. Heparin-Induced Thrombocytopenia: A Comprehensive Clinical Review. J. Am. Coll. Cardiol. 2016, 67, 2519–2532. [Google Scholar] [CrossRef]
- Pollak, U. Heparin-induced thrombocytopenia complicating extracorporeal membrane oxygenation support: Review of the literature and alternative anticoagulants. J. Thromb. Haemost. 2019, 17, 1608–1622. [Google Scholar] [CrossRef] [PubMed]
- Arepally, G.M. Heparin-induced thrombocytopenia. Blood 2017, 129, 2864–2872. [Google Scholar] [CrossRef] [PubMed]
- Weitz, J.I.; Hudoba, M.; Massel, D.; Maraganore, J.; Hirsh, J. Clot-bound thrombin is protected from inhibition by heparin-antithrombin III but is susceptible to inactivation by antithrombin III-independent inhibitors. J. Clin. Investig. 1990, 86, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.A.; Bartlett, R.H. Anticoagulation for Extracorporeal Life Support: Direct Thrombin Inhibitors and Heparin. ASAIO J. 2015, 61, 652–655. [Google Scholar] [CrossRef] [PubMed]
- Fisser, C.; Winkler, M.; Malfertheiner, M.V.; Philipp, A.; Foltan, M.; Lunz, D.; Zeman, F.; Maier, L.S.; Lubnow, M.; Müller, T. Argatroban versus heparin in patients without heparin-induced thrombocytopenia during venovenous extracorporeal membrane oxygenation: A propensity-score matched study. Crit. Care 2021, 25, 160. [Google Scholar] [CrossRef]
- Geli, J.; Capoccia, M.; Maybauer, D.M.; Maybauer, M.O. Argatroban Anticoagulation for Adult Extracorporeal Membrane Oxygenation: A Systematic Review. J. Intensive Care Med. 2022, 37, 459–471. [Google Scholar] [CrossRef]
- Ranucci, M.; Ballotta, A.; Kandil, H.; Isgrò, G.; Carlucci, C.; Baryshnikova, E.; Pistuddi, V. Bivalirudin-based versus conventional heparin anticoagulation for postcardiotomy extracorporeal membrane oxygenation. Crit. Care 2011, 15, R275. [Google Scholar] [CrossRef]
- Hirsh, J.; O’Donnell, M.; Weitz, J.I. New anticoagulants. Blood 2005, 105, 453–463. [Google Scholar] [CrossRef]
- Van De Car, D.A.; Rao, S.V.; Ohman, E.M. Bivalirudin: A review of the pharmacology and clinical application. Expert Rev. Cardiovasc. Ther. 2010, 8, 1673–1681. [Google Scholar] [CrossRef]
- Koster, A.; Weng, Y.; Böttcher, W.; Gromann, T.; Kuppe, H.; Hetzer, R. Successful use of bivalirudin as anticoagulant for ECMO in a patient with acute HIT. Ann. Thorac. Surg. 2007, 83, 1865–1867. [Google Scholar] [CrossRef]
- Zhong, H.; Zhu, M.L.; Yu, Y.T.; Li, W.; Xing, S.P.; Zhao, X.Y.; Wang, W.J.; Gu, Z.C.; Gao, Y. Management of Bivalirudin Anticoagulation Therapy for Extracorporeal Membrane Oxygenation in Heparin-Induced Thrombocytopenia: A Case Report and a Systematic Review. Front. Pharmacol. 2020, 11, 565013. [Google Scholar] [CrossRef]
- Ma, M.; Liang, S.; Zhu, J.; Dai, M.; Jia, Z.; Huang, H.; He, Y. The Efficacy and Safety of Bivalirudin Versus Heparin in the Anticoagulation Therapy of Extracorporeal Membrane Oxygenation: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2022, 13, 771563. [Google Scholar] [CrossRef]
- Burstein, B.; Wieruszewski, P.M.; Zhao, Y.J.; Smischney, N. Anticoagulation with direct thrombin inhibitors during extracorporeal membrane oxygenation. World J. Crit. Care Med. 2019, 8, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Beiderlinden, M.; Werner, P.; Bahlmann, A.; Kemper, J.; Brezina, T.; Schäfer, M.; Görlinger, K.; Seidel, H.; Kienbaum, P.; Treschan, T.A. Monitoring of argatroban and lepirudin anticoagulation in critically ill patients by conventional laboratory parameters and rotational thromboelastometry—A prospectively controlled randomized double-blind clinical trial. BMC Anesthesiol. 2018, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- McCarty, D.; Robinson, A. Factor Xa inhibitors: A novel therapeutic class for the treatment of nonvalvular atrial fibrillation. Ther. Adv. Cardiovasc. Dis. 2016, 10, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Phan, X.T.; Nguyen, T.H.; Tran, T.T.; Huynh, T.-H.T.; Hoang, T.-H.T.; Nguyen, V.-C.V.; Pham, T.N.T. Suspected heparin-induced thrombocytopenia in a COVID-19 patient on extracorporeal membrane oxygenation support: A case report. Thromb. J. 2020, 18, 37. [Google Scholar] [CrossRef]
- Parlar, A.I.; Sayar, U.; Cevirme, D.; Yuruk, M.A.; Mataraci, I. Successful use of fondaparinux in a patient with heparin-induced thrombocytopenia while on extracorporeal membrane oxygenation after mitral valve redo surgery. Int. J. Artif. Organs 2014, 37, 344–347. [Google Scholar] [CrossRef]
- Wilde, M.I.; Markham, A. Danaparoid. A review of its pharmacology and clinical use in the management of heparin-induced thrombocytopenia. Drugs 1997, 54, 903–924. [Google Scholar] [CrossRef]
- Bauer, C.; Vichova, Z.; Ffrench, P.; Hercule, C.; Jegaden, O.; Bastien, O.; Lehot, J.J. Extracorporeal membrane oxygenation with danaparoid sodium after massive pulmonary embolism. Anesth. Analg. 2008, 106, 1101–1103. [Google Scholar] [CrossRef]
- Giani, M.; Scaravilli, V.; Stefanini, F.; Valsecchi, G.; Rona, R.; Grasselli, G.; Bellani, G.; Pesenti, A.M.; Foti, G. Continuous Renal Replacement Therapy in Venovenous Extracorporeal Membrane Oxygenation: A Retrospective Study on Regional Citrate Anticoagulation. ASAIO J. 2020, 66, 332–338. [Google Scholar] [CrossRef]
- Shum, H.-P.; Kwan, A.M.-C.; Chan, K.-C.; Yan, W.-W. The Use of Regional Citrate Anticoagulation Continuous Venovenous Hemofiltration in Extracorporeal Membrane Oxygenation. ASAIO J. 2014, 60, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, D.L.; Biever, P.M.; Benk, C.; Ahrens, I.; Bode, C.; Wengenmayer, T. Dual Antiplatelet Therapy (DAPT) versus No Antiplatelet Therapy and Incidence of Major Bleeding in Patients on Venoarterial Extracorporeal Membrane Oxygenation. PLoS ONE 2016, 11, e0159973. [Google Scholar] [CrossRef]
- Bauer, K.A.; Hawkins, D.W.; Peters, P.C.; Petitou, M.; Herbert, J.M.; van Boeckel, C.A.; Meuleman, D.G. Fondaparinux, a synthetic pentasaccharide: The first in a new class of antithrombotic agents-the selective factor Xa inhibitors. Cardiovasc. Drug Rev. 2002, 20, 37–52. [Google Scholar] [CrossRef] [PubMed]
- Weinz, C.; Schwarz, T.; Kubitza, D.; Mueck, W.; Lang, D. Metabolism and excretion of rivaroxaban, an oral, direct factor Xa inhibitor, in rats, dogs, and humans. Drug Metab. Dispos. Biol. Fate Chem. 2009, 37, 1056–1064. [Google Scholar] [CrossRef]
- de Pont, A.C.; Hofstra, J.J.; Pik, D.R.; Meijers, J.C.; Schultz, M.J. Pharmacokinetics and pharmacodynamics of danaparoid during continuous venovenous hemofiltration: A pilot study. Crit. Care 2007, 11, R102. [Google Scholar] [CrossRef]
- Levi, M.; Hunt, B.J. A critical appraisal of point-of-care coagulation testing in critically ill patients. J. Thromb. Haemost. JTH 2015, 13, 1960–1967. [Google Scholar] [CrossRef]
- Berk, Z.B.K.; Shah, A.; Sun, W.; Griffith, B.P.; Wu, Z.J. An ex vivo comparison of partial thromboplastin time and activated clotting time for heparin anticoagulation in an ovine model. Artif. Organs 2022, 46, 501–505. [Google Scholar] [CrossRef]
- Bolliger, D.; Tanaka, K.A. Point-of-Care Coagulation Testing in Cardiac Surgery. Semin. Thromb. Hemost. 2017, 43, 386–396. [Google Scholar]
- Chlebowski, M.M.; Baltagi, S.; Carlson, M.; Levy, J.H.; Spinella, P.C. Clinical controversies in anticoagulation monitoring and antithrombin supplementation for ECMO. Crit. Care 2020, 24, 19. [Google Scholar] [CrossRef]
- Esper, S.A.; Welsby, I.J.; Subramaniam, K.; John Wallisch, W.; Levy, J.H.; Waters, J.H.; Triulzi, D.J.; Hayanga, J.W.A.; Schears, G.J. Adult extracorporeal membrane oxygenation: An international survey of transfusion and anticoagulation techniques. Vox Sang. 2017, 112, 443–452. [Google Scholar] [CrossRef]
- McMichael, A.B.V.; Ryerson, L.M.; Ratano, D.; Fan, E.; Faraoni, D.; Annich, G.M. 2021 ELSO Adult and Pediatric Anticoagulation Guidelines. ASAIO J. 2022, 68, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Gouin-Thibaut, I.; Martin-Toutain, I.; Peynaud-Debayle, E.; Marion, S.; Napol, P.; Alhenc-Gelas, M. Monitoring unfractionated heparin with APTT: A French collaborative study comparing sensitivity to heparin of 15 APTT reagents. Thromb. Res. 2012, 129, 666–667. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Bachler, M.; Treml, B. Diagnostic Modalities in Critical Care: Point-of-Care Approach. Diagnostics 2021, 11, 2202. [Google Scholar] [CrossRef] [PubMed]
- Delmas, C.; Jacquemin, A.; Vardon-Bounes, F.; Georges, B.; Guerrero, F.; Hernandez, N.; Marcheix, B.; Seguin, T.; Minville, V.; Conil, J.-M.; et al. Anticoagulation Monitoring Under ECMO Support: A Comparative Study Between the Activated Coagulation Time and the Anti-Xa Activity Assay. J. Intensiv. Care Med. 2020, 35, 679–686. [Google Scholar] [CrossRef]
- Descamps, R.; Moussa, M.D.; Besnier, E.; Fischer, M.-O.; Preau, S.; Tamion, F.; Daubin, C.; Cousin, N.; Vincentelli, A.; Goutay, J.; et al. Anti-Xa activity and hemorrhagic events under extracorporeal membrane oxygenation (ECMO): A multicenter cohort study. Crit. Care 2021, 25, 127. [Google Scholar] [CrossRef]
- Ranucci, M.; Cotza, M.; Isgrò, G.; Carboni, G.; Ballotta, A.; Baryshnikova, E. Anti-Factor Xa-Based Anticoagulation during Extracorporeal Membrane Oxygenation: Potential Problems and Possible Solutions. Semin. Thromb. Hemost. 2020, 46, 419–427. [Google Scholar] [CrossRef]
- Willems, A.; Roeleveld, P.P.; Labarinas, S.; Cyrus, J.W.; Muszynski, J.A.; Nellis, M.E.; Karam, O. Anti-Xa versus time-guided anticoagulation strategies in extracorporeal membrane oxygenation: A systematic review and meta-analysis. Perfusion 2021, 36, 501–512. [Google Scholar] [CrossRef]
- Baluwala, I.; Favaloro, E.J.; Pasalic, L. Therapeutic monitoring of unfractionated heparin-trials and tribulations. Expert Rev. Hematol. 2017, 10, 595–605. [Google Scholar] [CrossRef]
- Zhou, X.; Ding, T.; Wang, S.; Wen, L. In vivo real-time monitoring of anti-factor Xa level using a microdialysis-coupled microfluidic device. Talanta Open 2021, 4, 100059. [Google Scholar] [CrossRef]
- Carll, T.; Wool, G.D. Basic principles of viscoelastic testing. Transfusion 2020, 60 (Suppl. 6), S1–S9. [Google Scholar] [CrossRef]
- Giani, M.; Russotto, V.; Pozzi, M.; Forlini, C.; Fornasari, C.; Villa, S.; Avalli, L.; Rona, R.; Foti, G. Thromboelastometry, Thromboelastography, and Conventional Tests to Assess Anticoagulation During Extracorporeal Support: A Prospective Observational Study. ASAIO J. 2021, 67, 196–200. [Google Scholar] [CrossRef]
- Rezaie, A.R.; Giri, H. Anticoagulant and signaling functions of antithrombin. J. Thromb. Haemost. JTH 2020, 18, 3142–3153. [Google Scholar] [CrossRef] [PubMed]
- Protti, A.; Iapichino, G.E.; Di Nardo, M.; Panigada, M.; Gattinoni, L. Anticoagulation Management and Antithrombin Supplementation Practice during Veno-venous Extracorporeal Membrane Oxygenation: A Worldwide Survey. Anesthesiology 2020, 132, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Panigada, M.; Cucino, A.; Spinelli, E.; Occhipinti, G.; Panarello, G.; Novembrino, C.; Consonni, D.; Protti, A.; Lissoni, A.; Arcadipane, A.; et al. A Randomized Controlled Trial of Antithrombin Supplementation During Extracorporeal Membrane Oxygenation. Crit. Care Med. 2020, 48, 1636–1644. [Google Scholar] [CrossRef] [PubMed]
- Hayanga, J.W.A.; Aboagye, J.; Bush, E.; Canner, J.; Hayanga, H.K.; Klingbeil, A.; McCarthy, P.; Fugett, J.; Abbas, G.; Badhwar, V. Contemporary analysis of charges and mortality in the use of extracorporeal membrane oxygenation: A cautionary tale. JTCVS Open 2020, 1, 61–70. [Google Scholar] [CrossRef]
- Bharmal, M.I.; Venturini, J.M.; Chua, R.F.M.; Sharp, W.W.; Beiser, D.G.; Tabit, C.E.; Hirai, T.; Rosenberg, J.R.; Friant, J.; Blair, J.E.A.; et al. Cost-utility of extracorporeal cardiopulmonary resuscitation in patients with cardiac arrest. Resuscitation 2019, 136, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.E.; Jerguson, K.; Peterson, J.; Patel, D.V.; Saberi, A.A. Cost-effectiveness of Argatroban Versus Heparin Anticoagulation in Adult Extracorporeal Membrane Oxygenation Patients. Hosp. Pharm. 2021, 56, 276–281. [Google Scholar] [CrossRef]
- Mangoush, O.; Purkayastha, S.; Haj-Yahia, S.; Kinross, J.; Hayward, M.; Bartolozzi, F.; Darzi, A.; Athanasiou, T. Heparin-bonded circuits versus nonheparin-bonded circuits: An evaluation of their effect on clinical outcomes. Eur. J. Cardio-Thorac. Surg. 2007, 31, 1058–1069. [Google Scholar] [CrossRef]
- Mahoney, C.B. Heparin-bonded circuits: Clinical outcomes and costs. Perfusion 1998, 13, 192–204. [Google Scholar] [CrossRef]
- Sohn, N.; Marcoux, J.; Mycyk, T.; Krahn, J.; Meng, Q. The impact of different biocompatible coated cardiopulmonary bypass circuits on inflammatory response and oxidative stress. Perfusion 2009, 24, 231–237. [Google Scholar] [CrossRef]
- de Vroege, R.; Huybregts, R.; van Oeveren, W.; van Klarenbosch, J.; Linley, G.; Mutlu, J.; Jansen, E.; Hack, E.; Eijsman, L.; Wildevuur, C. The impact of heparin-coated circuits on hemodynamics during and after cardiopulmonary bypass. Artif. Organs 2005, 29, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Obstals, F.; Vorobii, M.; Riedel, T.; de los Santos Pereira, A.; Bruns, M.; Singh, S.; Rodriguez-Emmenegger, C. Improving Hemocompatibility of Membranes for Extracorporeal Membrane Oxygenators by Grafting Nonthrombogenic Polymer Brushes. Macromol. Biosci. 2018, 18, 1700359. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Pauls, J.P.; Bartnikowski, N.; Haymet, A.B.; Chan, C.H.H.; Suen, J.Y.; Schneider, B.; Ki, K.K.; Whittaker, A.K.; Dargusch, M.S.; et al. Anti-thrombogenic Surface Coatings for Extracorporeal Membrane Oxygenation: A Narrative Review. ACS Biomater. Sci. Eng. 2021, 7, 4402–4419. [Google Scholar] [CrossRef]
- Cornelissen, C.G.; Dietrich, M.; Gromann, K.; Frese, J.; Krueger, S.; Sachweh, J.S.; Jockenhoevel, S. Fibronectin coating of oxygenator membranes enhances endothelial cell attachment. BioMedical Eng. OnLine 2013, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Pflaum, M.; Kühn-Kauffeldt, M.; Schmeckebier, S.; Dipresa, D.; Chauhan, K.; Wiegmann, B.; Haug, R.J.; Schein, J.; Haverich, A.; Korossis, S. Endothelialization and characterization of titanium dioxide-coated gas-exchange membranes for application in the bioartificial lung. Acta Biomater. 2017, 50, 510–521. [Google Scholar] [CrossRef]
- Iizuka, K.; Katagiri, N.; Takewa, Y.; Tsukiya, T.; Mizuno, T.; Itamochi, Y.; Kumano, K.; Tatsumi, E. Evaluation of the Novel Centrifugal Pump, CAPIOX SL, in Chronic Large Animal Experiments. Artif. Organs 2018, 42, 835–841. [Google Scholar] [CrossRef]
- Annich, G.M.; Meinhardt, J.P.; Mowery, K.A.; Ashton, B.A.; Merz, S.I.; Hirschl, R.B.; Meyerhoff, M.E.; Bartlett, R.H. Reduced platelet activation and thrombosis in extracorporeal circuits coated with nitric oxide release polymers. Crit. Care Med. 2000, 28, 915–920. [Google Scholar] [CrossRef]
- Skrzypchak, A.M.; Lafayette, N.G.; Bartlett, R.H.; Zhou, Z.; Frost, M.C.; Meyerhoff, M.E.; Reynolds, M.M.; Annich, G.M. Effect of varying nitric oxide release to prevent platelet consumption and preserve platelet function in an in vivo model of extracorporeal circulation. Perfusion 2007, 22, 193–200. [Google Scholar] [CrossRef]
- El-Ferzli, G.T.; Andukuri, A.; Alexander, G.; Scopel, M.; Ambalavanan, N.; Patel, R.P.; Jun, H.W. A Nitric Oxide-Releasing Self-Assembled Peptide Amphiphile Nanomatrix for Improving the Biocompatibility of Microporous Hollow Fibers. ASAIO J. 2015, 61, 589–595. [Google Scholar] [CrossRef]
- Jacobson, J. Nitric oxide: Platelet protectant properties during cardiopulmonary bypass/ECMO. J. Extra-Corpor. Technol. 2002, 34, 144–147. [Google Scholar]
- Chung, A.; Wildhirt, S.M.; Wang, S.; Koshal, A.; Radomski, M.W. Combined administration of nitric oxide gas and iloprost during cardiopulmonary bypass reduces platelet dysfunction: A pilot clinical study. J. Thorac. Cardiovasc. Surg. 2005, 129, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Gerling, K.; Ölschläger, S.; Avci-Adali, M.; Neumann, B.; Schweizer, E.; Schlensak, C.; Wendel, H.P.; Stoppelkamp, S. A Novel C1-Esterase Inhibitor Oxygenator Coating Prevents FXII Activation in Human Blood. Biomolecules 2020, 10, 1042. [Google Scholar] [CrossRef] [PubMed]
- Roberts, T.R.; Harea, G.T.; Singha, P.; Sieck, K.N.; Beely, B.M.; Wendorff, D.S.; Choi, J.H.; Ande, S.; Handa, H.; Batchinsky, A.I. Heparin-Free Extracorporeal Life Support Using Tethered Liquid Perfluorocarbon: A Feasibility and Efficacy Study. ASAIO J. 2020, 66, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Willers, A.; Arens, J.; Mariani, S.; Pels, H.; Maessen, J.G.; Hackeng, T.M.; Lorusso, R.; Swol, J. New Trends, Advantages and Disadvantages in Anticoagulation and Coating Methods Used in Extracorporeal Life Support Devices. Membranes 2021, 11, 617. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.M.; Annich, G.M. The artificial endothelium. Organogenesis 2011, 7, 42–49. [Google Scholar] [CrossRef]
- Biran, R.; Pond, D. Heparin coatings for improving blood compatibility of medical devices. Adv. Drug Deliv. Rev. 2017, 112, 12–23. [Google Scholar] [CrossRef]
- DeLoughery, E.P.; Olson, S.R.; Puy, C.; McCarty, O.J.T.; Shatzel, J.J. The Safety and Efficacy of Novel Agents Targeting Factors XI and XII in Early Phase Human Trials. Semin. Thromb. Hemost. 2019, 45, 502–508. [Google Scholar] [CrossRef]
- Dobrovolskaia, M.A.; McNeil, S.E.J.A.o.T.M. Safe anticoagulation when heart and lungs are “on vacation”. Ann. Transl. Med. 2015, 2015, 11. [Google Scholar]
- Wilbs, J.; Kong, X.-D.; Middendorp, S.J.; Prince, R.; Cooke, A.; Demarest, C.T.; Abdelhafez, M.M.; Roberts, K.; Umei, N.; Gonschorek, P.; et al. Cyclic peptide FXII inhibitor provides safe anticoagulation in a thrombosis model and in artificial lungs. Nat. Commun. 2020, 11, 3890. [Google Scholar] [CrossRef]
- Lorentz, C.U.; Verbout, N.G.; Wallisch, M.; Hagen, M.W.; Shatzel, J.J.; Olson, S.R.; Puy, C.; Hinds, M.T.; McCarty, O.J.T.; Gailani, D.; et al. Contact Activation Inhibitor and Factor XI Antibody, AB023, Produces Safe, Dose-Dependent Anticoagulation in a Phase 1 First-In-Human Trial. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 799–809. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajsic, S.; Breitkopf, R.; Jadzic, D.; Popovic Krneta, M.; Tauber, H.; Treml, B. Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review. J. Clin. Med. 2022, 11, 5147. https://doi.org/10.3390/jcm11175147
Rajsic S, Breitkopf R, Jadzic D, Popovic Krneta M, Tauber H, Treml B. Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review. Journal of Clinical Medicine. 2022; 11(17):5147. https://doi.org/10.3390/jcm11175147
Chicago/Turabian StyleRajsic, Sasa, Robert Breitkopf, Dragana Jadzic, Marina Popovic Krneta, Helmuth Tauber, and Benedikt Treml. 2022. "Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review" Journal of Clinical Medicine 11, no. 17: 5147. https://doi.org/10.3390/jcm11175147
APA StyleRajsic, S., Breitkopf, R., Jadzic, D., Popovic Krneta, M., Tauber, H., & Treml, B. (2022). Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review. Journal of Clinical Medicine, 11(17), 5147. https://doi.org/10.3390/jcm11175147








