Abstract
Background: Long-term trends in influenza-related hospitalizations, critical care resource use, and hospital outcomes since the 2009 H1N1 influenza pandemic season have been rarely studied for adult populations. Materials and Methods: Adult patients from the Korean Health Insurance Review and Assessment Service who were hospitalized with influenza over a 10-year period (2009–2019) were analyzed. The incidence rates of hospitalization, critical care resource use, and in-hospital death were calculated using mid-year population census data. Results: In total, 300,152 hospitalized patients with influenza were identified (men, 35.7%; admission to tertiary hospitals, 9.4%). Although the age-adjusted hospitalization rate initially decreased since the 2009 H1N1 pandemic (52.61/100,000 population in 2009/2010), it began to increase again in 2013/2014 and reached a peak of 169.86/100,000 population in 2017/2018 (p < 0.001). The in-hospital mortality rate showed a similar increasing trend as the hospitalization, with a peak of 1.44/100,000 population in 2017/2018 (vs. 0.35/100,000 population in 2009/2010; p < 0.001). The high incidence rates of both hospitalization and in-hospital mortality were mainly attributable to patients aged ≥60 years. The rate of intensive care unit admission and the use of mechanical ventilation, continuous renal replacement therapy and vasopressors have also increased from the 2013/2014 season. The incidence of heart failure was the most frequent complication investigated, with a three-fold increase in the last two seasons since 2009/2010. In multivariate analysis adjusted for covariates, among hospitalized patients, type of hospitals and 2009 H1N1 pandemic season were associated with in-hospital mortality. Conclusions: We confirmed that the rates of hospitalization, critical care resource use, and in-hospital mortality by influenza have increased again in recent years. Therefore, strategies are needed to reduce infections and optimize resource use with a greater focus on older people.
1. Introduction
Influenza, an acute infectious respiratory illness, causes substantial morbidity and mortality, most deaths occurring in adults aged ≥ 65 years. The World Health Organization (WHO) reported that influenza causes about 3~5 million cases of severe illness and 290,000–650,000 deaths annually in the world [1].
Epidemics of influenza and its disease burden vary by different regions [2,3,4,5,6]. Hence, nationwide data from countries with different healthcare systems are needed to establish global strategies and prepare for future epidemics or pandemics. Although influenza cases have decreased for several years after the 2009 H1N1 pandemic season, some Western regions are currently seeing the increasing rates of hospitalizations and hospital deaths by seasonal influenza again [7,8,9]. Hence, given the increased healthcare burden and resource consumption during a surge of infections, an investigation of long-term changes in morbidities or mortalities caused by influenza might be worthwhile in terms of estimating disease burden and guiding future policies.
In Korea, several nationwide studies on influenza, using data from the Korean National Health Insurance Service (NHIS) or the Health Insurance Review & Assessment Service (HIRA), have been conducted [10,11,12,13]. However, trends of influenza-related hospitalizations and hospital outcomes over multiple years have not been well described so far. Besides, it remains unclear how the rates of intensive care unit (ICU) admissions and other critical care resource use have changed since the 2009 H1N1 pandemic season.
Therefore, through a population-based study using HIRA data (from 2009 to 2019), we explored the patterns of changes after 2009 H1N1 pandemic season in the rates of influenza-related hospitalizations, critical care resource use, and hospital outcomes in the Korean adult population.
2. Materials and Methods
2.1. Data Collection
Data were collected from the HIRA database that contains nationwide population-based healthcare reimbursement claims in Korea. The NHIS provides healthcare coverage, using fee-for-service payment system, to about 97% of the population in Korea [14]. The government regulates these fees, and the HIRA reviews the healthcare insurance claims and assess the quality of healthcare services. The claims database holds encrypted personal information including name, age, sex, International Classification of Diseases, the 10th Revision (ICD-10) codes for primary and secondary diagnoses, dates of admission and discharge, type of hospitals, and in-hospital mortality. Records of all medical procedures and prescriptions that are covered by the NHIS are also accumulated in the HIRA database. In this study, we identified adult patients (>18 years) who were hospitalized with influenza from October 2009 to September 2019. In Korea, the influenza season begins as early as October and lasts as late as April or May in next year. However, in the present study, all hospitalized patients with influenza diagnosis were collected year-round.
This study and a waiver of consent were approved by the Hallym University Institutional Review Board (approval No. 2020-05-018).
2.2. Case Definition
All the diagnosis codes for influenza (J09–J11) were extracted from the claims data if the ICD-10 codes for influenza were listed for either the primary or secondary diagnosis. For the analysis, a hospitalization was defined as an admission to a hospital for 24 h or more, and hospital stays separated by <2 days were considered to be the same hospital admission; for patients who were transferred to another hospital, data were combined using resident registration numbers and discharge dates.
2.3. Variables for Critical Care Resource Use
ICU admissions were identified using the Korean Classification of Diseases 7th edition codes (KCD-7; AJ001, AJ003, AJ006, AJ007, AJ010, AJ011, AJ020, AJ100, AJ200, AJ300, AC612), which is a modified version of the ICD-10. Multiple ICU admissions during the same hospitalization were considered as a single ICU admission. Comorbidities such as diabetes mellitus, cardiovascular disease, cerebrovascular disease, chronic kidney disease, chronic liver disease, malignancy, rheumatic disease, and acquired immunodeficiency syndrome (AIDS) were identified with the use of ICD-10 codes (Supplementary Table S1), and also summarized using the Charlson Comorbidity Index (CCI) [15,16,17]. Procedures with mechanical ventilation (MV; the Korean NHIS procedure codes: M0850, M0857, M0858, M0860, M5830, M5850, M5857, M5858, M5860, M5890), continuous renal replacement therapy (CRRT; O7031–O7035 and O705–O7055), and extracorporeal membrane oxygenation (ECMO; O1901–O1907) were investigated. Data on the use of vasopressors (i.e., norepinephrine, epinephrine, and dopamine), steroids (i.e., methylprednisolone, prednisone, and hydrocortisone), and oseltamivir were also obtained. Regarding the steroid use, to include patients who received steroids for acute respiratory failures, only doses of ≥40 mg methylprednisolone (or its equivalent doses of other steroids) for ≥5 days were counted, based on a previous study [18].
In addition, hospitals were divided into four types according to their supporting levels, which was based on bed capacity and range of specialties as stipulated by the Korean Health Law [19]. A ‘hospital’ was defined as a healthcare facility with >30 beds. A ‘general hospital’ is one with both >100 beds and >7 specialty departments, where the inclusion of Internal Medicine, Pediatrics, Surgery, Obstetrics and Gynecology, Pathology, Anesthesiology, and Laboratory Medicine is mandatory. A ‘tertiary hospital’ is defined as one with >20 specialty departments and serves as a teaching hospital. When a healthcare facility did not fall into any of the three types (e.g., nursing hospitals, hospitals for oriental medicine, etc.), it was categorized as ‘others’.
2.4. Variables for Outcomes
For hospital outcomes, the incidence of complications (myocarditis, acute myocardial infarct, heart failure, cerebral infarct and hemorrhage, and liver failure) that occurred during the hospitalization was investigated using ICD-10 codes (Supplementary Table S2). In-hospital deaths, as well as ICU deaths, were also investigated for all hospitalized patients.
2.5. Data Analysis
Descriptive analyses were used to summarize characteristics of the hospitalized patients with influenza. Data are presented as means ± standard deviations or median (interquartile ranges, 25th–75th percentiles) for continuous data and as frequency (percentage) for categorical data. To compare the hospitalization rates between years, the age-adjusted rates of hospitalization were calculated, using the annual mid-year population census (the Korea Statistical Information Service) as the standard [20]. We investigated the longitudinal trends over 10 years (2009–2019) in the use of critical care resources, such as ICU admission, vasopressors, MV, CRRT, and ECMO, as well as in-hospital mortality rate. For these data, Cochran–Armitage trend test was used to detect yearly trends. Lengths of hospital and ICU stay were compared using the Kruskal–Wallis test because these variables were not normally distributed. Logistic regression analysis was performed to see the effects of type of hospitals and the seasons on in-hospital mortality, adjusted for age, gender, CCI, and the use of ICU resources. All statistical analyses were performed using R version 4.0.5 (R Foundation Inc.; https://www.r-project.org/, accessed on 28 February 2022). For all analyses, p < 0.05 was considered to indicate statistical significance.
3. Results
3.1. Study Population
In total, 300,152 patients were hospitalized with influenza in South Korea from October 2009 to September 2019 (Supplementary Table S3). The mean age of the included patients was 51.0 ± 18.7 years, and the frequency of men was 35.7%. Diabetes mellitus was the most common underlying comorbidity, followed by chronic obstructive pulmonary disease and liver disease (Supplementary Table S4). Almost half of the patients (48.7%) were treated in general hospitals; only 9.4% of patients were treated in tertiary hospitals (Table 1 and Supplementary Figure S1). Except for the 2009/2010 season, the prescription rate of oseltamivir ranged from 29.4% to 55.1% during the hospitalization (Supplementary Table S3).

Table 1.
Influenza-related hospitalization rates and patients’ characteristics.
3.2. Incidence of Hospitalization
Changes in the annual hospitalization rate per 100,000 people are depicted in Figure 1. The age-adjusted incidence of hospitalizations initially decreased after the 2009 H1N1 pandemic season but increased again in the 2013/2014 season and reached its peak during the 2017/2018 season (169.86/100,000 population), which was almost three times greater than the incidence during the 2009 H1N1 pandemic (52.61/100,000 population: Table 1). This increase was found in all age groups and all regions nationwide (Supplementary Tables S5 and S6). In particular, the rate of increase was higher for older patients than for younger patients (Figure 1); the proportion of women was consistently higher than that of men during the 10-year period (64.3% vs. 35.7%).
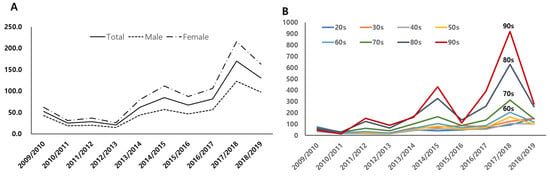
Figure 1.
Age-specific annual hospitalization rates (per 100,000 population). (A) Annual trend of influenza-related hospitalization rates (X axis = years; Y axis = number of patients per 100,000 population). (B) Annual hospitalization rates by age groups (X axis = years; Y axis = number of patients per 100,000 population by age groups).
3.3. Critical Care Resource Use and Complications
The rate of ICU admission decreased initially after the 2009 H1N1 pandemic season, but started to increase again in 2013/2014, with a peak rate during the 2017/2018 season (3.37/100,000 vs. 1.83/100,000 population in 2009/2010, p < 0.001). The rates of MV, CRRT, and vasopressor use also showed a similar increasing trend as the ICU admission rate (1.24/100,000 vs. 0.63/100,000 population for MV, p < 0.001; 0.22/100,000 vs. 0.10/100.000 population for CRRT, p < 0.001; 2.27/100.000 vs. 0.35/100,000 population for vasopressors, p < 0.001; 2017/2018 vs. 2009/2010, respectively) (Figure 2 and Supplementary Table S7). However, a minimal change was detected in the rate of ECMO use. Regarding the complications, heart failure and cerebral infarcts were the most common (Table 2), and their incidences have increased since the 2012/2013 season, with a three-fold increase in the 2017/2018–2018/2019 seasons compared to the 2009/2010 season (p < 0.001 and p < 0.001, respectively; Supplementary Figure S2).
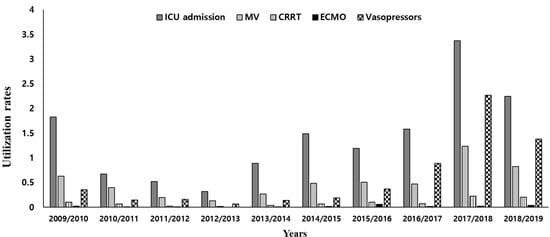
Figure 2.
Rates of critical care resource utilization (per 100,000 population). MV: mechanical ventilation; CRRT: continuous renal replacement therapy; ECMO: extracorporeal membrane oxygenation.

Table 2.
Complications and hospital outcomes (rates per 100,000 population).
3.4. Incidence Rates of ICU and In-Hospital Mortality
The ICU and in-hospital mortality rates showed a similar trend as hospitalization rates during the 10-year period. While mortalities were lowest during the 2012/2013 season (ICU mortality: 0.04/100,000; in-hospital mortality: 0.07/100,000 population), they gradually increased to peak rates in the 2017/2018 season (0.67/100,000 and 1.44/100,000 population, respectively) (Table 2 and Figure 3). In particular, the increased in-hospital mortality rate was primarily driven by patients aged ≥60 years (Figure 3 and Supplementary Table S8). Among the hospitalized patients, a multivariable analysis adjusted for age, gender, comorbidity, steroid, mechanical ventilation, CRRT, and the use of vasopressors demonstrated that type of hospitals (i.e., ‘general’, ‘tertiary’, and ‘others’, compared to ‘hospitals’) and the 2009 H1N1 pandemic season (i.e., 2009/2010–2010/2011, compared to other seasons) were significantly associated with increased in-hospital mortality (Table 3).
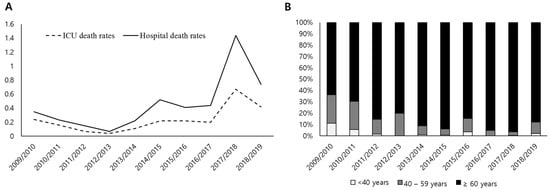
Figure 3.
ICU and in-hospital mortality rates. (A) Annual trends of ICU and hospital mortality rates per 100,000 population (X axis = years; Y axis = number of deaths per 100,000 population). (B) Annual proportions of three age groups who died in hospitals (i.e., in-hospital death; X axis = years; Y axis = proportions of age groups). ICU: intensive care unit.

Table 3.
Univariable and multivariable analyses for in-hospital mortality.
4. Discussion
This population-based study revealed several notable findings. First, since the decline of the 2009 H1N1 pandemic influenza outbreak, the incidence rates of influenza-related hospitalizations and in-hospital mortalities have increased again from the 2013/2014 season, with a more than a two-fold increase during the 2017/2018–2018/2019 seasons, compared with the 2009 H1N1 pandemic season. Notably, the incidence rates of both hospitalization and in-hospital mortality were mainly attributable to patients aged ≥60 years. Second, similar to the changes in hospitalization and in-hospital mortality, the rate of ICU admissions and the use of MV, CRRT, and vasopressors also recently increased. Finally, the incidence of heart failure and cerebral infarct increased by approximately three-fold over the 10-year period.
Influenza with epidemic or pandemic potential can be a huge burden on healthcare services worldwide. Hence, to enable efficient infection control, international surveillance and collaboration systems are important. In many countries, both clinical and laboratory data-based surveillance systems are commonly used [22]. However, to estimate the burden of influenza, detailed data on hospitalization (i.e., severe influenza) should be collected, as in the United States (U.S.) Although the national influenza surveillance system is well organized in South Korea, the data on hospitalized patients are very limited, thus hampering better understanding of the disease burden. In this aspect, our study, highlighting the increasing rates of hospitalization and ICU resource use, is relevant and can add to the current knowledge.
Although the 2009 H1N1 influenza pandemic, which began worldwide in April 2009, was associated with high mortality [23,24], data are limited on how the seasonal influenza epidemics have changed in terms of disease severity and healthcare utilization since the pandemic season. Hence, we conducted this 10-year investigation starting the 2009 pandemic season. In South Korea, cases (of the 2009 H1N1 pandemic) began to increase in late August 2009 and lasted until December 2010 [25]. Therefore, some cases of hospitalization or mortality from the 2009/2010 season may have been missed in our study. However, studies from U.S., the United Kingdom, and China (Shanghai) indicate that since the decline of the 2009 H1N1 pandemic outbreak, the rates of hospitalization have increased again, with a peak during the 2017/2018 season [7,8,9,26]. These data are consistent with our results. Although the rate of hospitalization was higher in females than in males in our study, a previous study using the HIRA data also reported similar results [10]. However, gender difference can vary among different seasons and countries [8,9,10,27].
The current study showed that the rate of in-hospital mortality declined after the 2009/2010 season but increased again in recent years. In the U.S., reports from the Centers for Disease Control and Prevention (CDC) and a surveillance network showed a similar trend, with peak mortality during the 2017/2018 season [7,9]. Although the mortality rate has not changed noticeably in the United Kingdom, the total number of deaths has increased steadily over the past decade [8]; our findings are consistent with that trend. In contrast, among the hospitalized patients, the risk of in-hospital mortality was the highest during the 2009 H1N1 pandemic, compared to other influenza seasons in multivariable analysis. One explanation for this is that different characteristics or disease severities among hospitalized patients over the study period, as well as different circulating virus strains, may have contributed to the different risks for in-hospital mortality. Notably, we found a higher prevalence of admissions to tertiary hospitals during the 2009 H1N1 pandemic season (15.6%) than during any other season. The significant association of type of hospitals with in-hospital mortality may be associated with the fact that patients with comorbidities or high disease severity were more likely to be treated in ‘general’ or ‘tertiary hospitals’ rather than ‘hospitals’, and those who indicated do-not-resuscitation or withholding life-sustaining treatments were also likely to be treated in other type of hospitals (e.g., nursing hospitals).
Regarding the ICU resource utilization, the frequency of MV, CRRT and ECMO use, as well as the rate of ICU admission, were investigated. Considering the high costs and impacts on morbidity and mortality, these variables seem relevant to answer our research questions. However, the rates of ICU admission in our cohort (0.32~3.37/100,000 population) and the United Kingdom (0.06~0.22/100,000 population) [8] seem to be lower, compared to that in the U.S. (5.7~11.6/100,000 population) or Canada (14.4%) [9,28,29]. This may be explained by the different ICU capacities or triage among hospitals or countries. Besides, the rate of MV use in our cohort (0.4~1.6% among hospitalized patients) seems lower, compared to that of the US (15.6~25.0%), Spain (8.9%), Canada (8.6%) and Germany (3.4~6.7%) [6,9,27,29,30]. This different rate could be linked to different disease severities or proportions of do-not-intubate orders among countries. Particularly, the number of ECMO cases was very low. Although we think all billing claims were processed for all ECMO cases nationwide, a possibility of underestimation of ECMO cases cannot be ruled out. However, of note, recent reports demonstrated that influenza vaccination can reduce the severity of disease in patients with influenza or even COVID-19 [31,32,33]. Hence, the high vaccination rate (>80% in those aged 65 and older) in South Korea might contribute to this lower rate of ICU admission and MV use in our study. However, the Korean national influenza surveillance system reported an increased incidence of influenza-like illness in the 2017/2018 seasons (Supplementary Table S9). The CDC also indicated that the 2017/2018 season had high severity, with unusually high rates of outpatient flu-like illness, hospitalizations, and complications [34]. Increased disease severity or availability of machines may be responsible for the increasing trend of ICU resource use [35].
Regarding complications investigated, a substantial increase in the incidence of heart failure and cerebral infarcts was noted during the past decade, with an almost twofold higher rate compared with respiratory failure (indicated by MV use). It is well known that pneumonia and exacerbation of underlying pulmonary or cardiac diseases are the common complications of influenza. Hence, considering the large effect of these complications on the nation’s healthcare system, we cannot overemphasize the early diagnosis and treatment of influenza. However, the incidence of liver failure in the current study was an unexpected result. Although this is likely to be associated with underlying comorbidity or disease progression, further studies are needed to clarify this association.
As with other studies using administrative database, CCI was used to investigate the frequency of underlying comorbidities in our study, and similar to previous study, COPD, diabetes mellitus, and liver disease were the most common [30,36]. However, despite a thorough review of the HIRA data, we noted that the frequency of comorbidities was lower than anticipated. Previously, the incidence of diabetes mellitus was reported to be 13.8% of Koran adults (>30 years) [37], and a study using the Hospital-based Influenza Morbidity & Mortality Surveillance also reported that the incidence of diabetes mellitus and cardiovascular diseases was 9.8% and 7.2%, respectively [38]. Hence, we cannot exclude a possibility of underestimation of the frequency of comorbidities, which may be inherent when using administrative database. However, from the Korean Statistical Information Service data [20], the prevalence of diabetes mellitus was reported to be 1.3% among the entire hospitalized population in 2018 (unpublished data). Besides, in our study, a high proportion of patients aged <60 years (64.0%) should also be taken into account.
Although we collected data on the prescription of oseltamivir (Supplementary Table S3), many patients could presumably have received oseltamivir before hospitalization, not covered by the NHIS. For these reasons, we did not include the antiviral agent in the multivariate analysis. Regarding the steroid doses, the selection criteria seem arbitrary in our study. Although a dose of 1~2 mg/kg/day methylprednisolone has been frequently used to treat patients with acute respiratory distress syndrome in clinical practice [39], we chose a dose of 40 mg methylprednisolone (or its equivalent doses of other steroids) as the minimum dose. Besides, we also intended to exclude patients receiving long-term treatment for chronic diseases.
This study has some limitations to be considered. First, as with other studies using administrative database, there is a possibility of misclassification. Particularly, although the patients with influenza ICD-10 codes in our study were those with laboratory-confirmed cases, year-to-year heterogeneity of influenza test rates may partially explain the differences in influenza-related hospitalizations. Second, it was not possible to obtain data on influenza virus types (or subtypes) and influenza severity from the billing claims data; in contrary, studies using clinical data may increase the accuracy of diagnoses and severity. Third, although vaccination has been known to decrease the rate of hospitalization and mortality [40,41], this information was not obtainable from the HIRA data because it is not claimed (i.e., non-payment) in Korea. Fourth, to evaluate ICU resource utilizations and disease burden, analysis on the duration (days) of MV, ECMO, or CRRT might have been more informative than just proportions of patients receiving these treatments. Finally, we could not provide long-term mortality data, such as 6- or 12-month mortality rates, because the data were not available for the HIRA database. However, population-based studies like ours are very rare. Additionally, one of our strengths is that we evaluated those data during the 10-year period, facilitating better understanding of long-term trends.
5. Conclusions
This study highlights that after the big wave of 2009 H1N1 pandemic influenza, the rates of hospitalizations and mortality by seasonal influenza have risen again in recent years, both of which were mostly driven by those 60 years of age and older. Furthermore, increasing trends of critical care resource use and the incidence of complications were also noted. Therefore, strategies are needed to reduce infections and optimize critical care resource use with greater focus on older people.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11164911/s1, Table S1: ICD-10 codes for Charlson comorbidity index; Table S2: Codes for ICU admissions, treatments, and complications; Table S3: Age, Charlson comorbidity index, treatments, and hospital outcomes; Table S4: Underlying comorbidities of enrolled patients; Table S5: Annual numbers and rates of hospitalization by age groups; Table S6: Numbers of hospitalizations by regions across South Korea; Table S7: Critical care resource utilization; Table S8: Annual numbers and rates of in-hospital deaths; Table S9: Annual incidence of ILI visits per 1000 patients and influenza virus isolates by subtypes; Figure S1: Distribution of hospital types; Figure S2: Incidence of complications per 100,000 population.
Author Contributions
Conceptualization, T.H.H. and S.P.; Data curation, H.S.L., N.-E.K. and K.J.L.; Formal analysis, H.S.L., N.-E.K., J.-H.K. and S.P.; Funding acquisition, S.P.; Investigation, K.J.L., J.N.A. and H.W.K.; Methodology, N.-E.K., Y.K.K. and S.P.; Project administration, T.H.H.; Software, K.J.L.; Supervision, Y.K.K., J.N.A., J.-H.K. and H.W.K.; Validation, Y.K.K., J.-H.K., H.W.K. and S.P.; Visualization, J.N.A. and J.-H.K.; Writing—original draft, T.H.H. and S.P.; Writing—review and editing, T.H.H., H.S.L., N.-E.K., K.J.L., Y.K.K., J.N.A., J.-H.K., H.W.K. and S.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant from the Hallym University Medical Center Research Fund (HURF-2020-62).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Hallym University Institutional Review Board (approval No. 2020-05-018).
Informed Consent Statement
Written informed consent was waived because of the retrospective nature of the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We would like to thank Hyunseung Nam for assistance with formatting of the text, tables, and figures in this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Global Influenza Strategy 2019–2030. Available online: https://www.who.int/publications/i/item/9789241515320 (accessed on 5 December 2021).
- Gordon, A.; Reingold, A. The Burden of Influenza: A Complex Problem. Curr. Epidemiol. Rep. 2018, 5, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Park, J.Y.; Song, Y.; How, S.H.; Jung, K.S. Emerging respiratory infections threatening public health in the Asia-Pacific region: A position paper of the Asian Pacific Society of Respirology. Respirology 2019, 24, 590–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, T.W.; Rubinson, L.; Uyeki, T.M.; Vaughn, F.L.; John, B.B.; Miller, R.R.; Higgs, E.; Randolph, A.; Smoot, B.E.; Thompson, B.T. Critical illness from 2009 pandemic influenza A virus and bacterial coinfection in the United States. Crit. Care Med. 2012, 40, 487–498. [Google Scholar] [CrossRef] [Green Version]
- Timmers, P.; Kerssens, J.J.; Minton, J.; Grant, I.; Wilson, J.F.; Campbell, H.; Fischbacher, C.M.; Joshi, P.K. Trends in disease incidence and survival and their effect on mortality in Scotland: Nationwide cohort study of linked hospital admission and death records 2001–2016. BMJ Open 2020, 10, e034299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, J.C.; Lee, I.K.; Huang, W.C.; Chen, Y.C.; Tsai, C.Y. Clinical Characteristics and Predictors of Mortality in Critically Ill Influenza Adult Patients. J. Clin. Med. 2020, 9, 1073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Disease Burden of Influenza. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/about/burden/index.html (accessed on 21 December 2021).
- Public Health England. Flu Annual Report: Winter 2019 to 2020. Available online: https://www.gov.uk/government/statistics/annual-flu-reports (accessed on 22 December 2021).
- O’Halloran, A.C.; Holstein, R.; Cummings, C.; Kirley, P.D.; Alden, N.B.; Yousey-Hindes, K.; Anderson, E.J.; Ryan, P.; Kim, S.; Lynfield, R.; et al. Rates of Influenza-Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death by Race and Ethnicity in the United States From 2009 to 2019. JAMA Netw. Open 2021, 4, e2121880. [Google Scholar] [CrossRef]
- Byeon, K.H.; Kim, J.; Choi, B.Y.; Kim, J.Y.; Lee, N. Age-Period-Cohort Analysis of Influenza in Koreans: The National Health Insurance Research Database, 2009–2018. J. Korean Med. Sci. 2020, 35, e121. [Google Scholar] [CrossRef]
- Byeon, K.H.; Kim, J.; Choi, B.Y.; Kim, J.Y.; Lee, N. Factors Affecting the Incidence of Hospitalized Pneumonia after Influenza Infection in Korea Using the National Health Insurance Research Database, 2014–2018: Focusing on the Effect of Antiviral Therapy in the 2017 Flu Season. J. Korean Med. Sci. 2020, 35, e318. [Google Scholar] [CrossRef]
- Kim, Y.W.; Yoon, S.J.; Oh, I.H. The economic burden of the 2009 pandemic H1N1 influenza in Korea. Scand. J. Infect. Dis. 2013, 45, 390–396. [Google Scholar] [CrossRef]
- Suh, M.; Kang, D.R.; Lee, D.H.; Choi, Y.J.; Tchoe, B.; Nam, C.M.; Kim, H.J.; Lee, J.K.; Jun, B.Y.; Youm, Y.; et al. Socioeconomic burden of influenza in the Republic of Korea, 2007–2010. PLoS ONE 2013, 8, e84121. [Google Scholar] [CrossRef]
- Lee, Y.H.; Han, K.; Ko, S.H.; Ko, K.S.; Lee, K.U. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes, A. Data Analytic Process of a Nationwide Population-Based Study Using National Health Information Database Established by National Health Insurance Service. Diabetes Metab. J. 2016, 40, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Kim, K.H. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients [article in Korean]. J. Prev. Med. Public Health 2010, 43, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Zhou, Y.; Fu, X.; Liu, X.; Huang, C.; Tian, G.; Ding, C.; Wu, J.; Lan, L.; Yang, S. Use of corticosteroids in influenza-associated acute respiratory distress syndrome and severe pneumonia: A systemic review and meta-analysis. Sci. Rep. 2020, 10, 3044. [Google Scholar] [CrossRef] [Green Version]
- Korea Ministry of Health and Welfare. Korea Health Law. Available online: http://law.go.kr (accessed on 10 November 2021).
- Korean Statistical Information Service. Available online: https://kosis.kr/eng/index/index.do (accessed on 30 December 2021).
- Korea Disease Control and Prevention Agency. Health Statistics. Available online: https://health.kdca.go.kr/healthinfo/biz/pblcVis/details.do?ctgrSn=71 (accessed on 12 August 2022).
- Choi, W.S. The National Influenza Serveillance System of Korea. Infect. Chemother. 2019, 51, 98–106. [Google Scholar] [CrossRef]
- Nguyen, A.M.; Noymer, A. Influenza mortality in the United States, 2009 pandemic: Burden, timing and age distribution. PLoS ONE 2013, 8, e64198. [Google Scholar] [CrossRef]
- Wu, S.; Wei, Z.; Greene, C.M.; Yang, P.; Su, J.; Song, Y.; Iuliano, A.D.; Wang, Q. Mortality burden from seasonal influenza and 2009 H1N1 pandemic influenza in Beijing, China, 2007–2013. Influenza Other Respir. Viruses 2018, 12, 88–97. [Google Scholar] [CrossRef]
- The Korean Disease Control and Prevention Agency. Infectious Disease Surveillance Year Book. 2010. Available online: http://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaView.do?pblctDtaSeAt=1&pblctDtaSn=10 (accessed on 10 December 2021).
- Li, J.; Wang, C.; Ruan, L.; Jin, S.; Ye, C.; Yu, H.; Zhu, W.; Wang, X. Development of influenza-associated disease burden pyramid in Shanghai, China, 2010-2017: A Bayesian modelling study. BMJ Open 2021, 11, e047526. [Google Scholar] [CrossRef]
- von der Beck, D.; Seeger, W.; Herold, S.; Günther, A.; Löh, B. Characteristics and outcomes of a cohort hospitalized for pandemic and seasonal influenza in Germany based on nationwide inpatient data. PLoS ONE 2017, 12, e0180920. [Google Scholar] [CrossRef] [Green Version]
- Baker, A.W.; Edmond, M.B.; Herwaldt, L.A.; Chen, L.F.; Srikantaswamy, S.; Sexton, D.J. Real-Time Surveillance of Influenza Morbidity: Tracking Intensive Care Unit Resource Utilization. Ann. Am. Thorac. Soc. 2017, 14, 1810–1817. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.; Ye, L.; Noorduyn, S.G.; Hux, M.; Thommes, E.; Goeree, R.; Ambrose, A.; Andrew, M.K.; Hatchette, T.; Boivin, G.; et al. Resource utilization and cost of influenza requiring hospitalization in Canadian adults: A study from the serious outcomes surveillance network of the Canadian Immunization Research Network. Influenza Other Respir. Viruses 2018, 12, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Viasus, D.; Pano-Pardo, J.R.; Pachon, J.; Campins, A.; López-Medrano, F.; Villoslada, A.; Fariñas, M.; Moreno, A.; Rodríguez-Baño, J.; Oteo, J.; et al. Factors associated with severe disease in hospitalized adults with pandemic (H1N1) 2009 in Spain. Clin. Microbiol. Infect. 2011, 17, 738–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferdinands, J.M.; Thompson, M.G.; Blanton, L.; Spencer, S.; Grant, L.; Fry, A.M. Does influenza vaccination attenuate the severity of breakthrough infections?A narrative review and recommendations for further research. Vaccine 2021, 39, 3678–3695. [Google Scholar] [CrossRef]
- Godoy, P.; Romero, A.; Soldevila, N.; Torner, N.; Jané, M.; Martínez, A.; A Caylà, J.; Rius, C.; Domínguez, A. Influenza vaccine effectiveness in reducing severe outcomes over six influenza seasons, a case-case analysis, Spain, 2010/11 to 2015/16. Eurosurveillance 2018, 23, 1700732. [Google Scholar] [CrossRef] [Green Version]
- Marin-Hernandez, D.; Schwartz, R.E.; Nixon, D.F. Epidemiological evidence for association between higher influenza vaccine uptake in the elderly and lower COVID-19 deaths in Italy. J. Med. Virol. 2021, 93, 64–65. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Estimated Flu-Related Illnesses, Medical Visits, Hospitalizations, and Deaths in the United States—2017–2018 Flu Season. Available online: https://www.cdc.gov/flu/about/burden/2017-2018.htm#:~:text=CDC%20estimates%20that%20flu%20burden,from%20flu%20(Table%201) (accessed on 10 July 2022).
- Lane, C.J.; Bhatnagar, M.; Lutrick, K.; Maves, R.C.; Weiner, D.; Olvera, D.R.; Uyeki, T.M.; Cobb, J.P.; Brown, J.C. ICU Resource Limitations During Peak Seasonal Influenza: Results of a 2018 National Feasibility Study. Crit. Care Explor. 2022, 4, e0606. [Google Scholar] [CrossRef]
- Gutierrez-Gonzalez, E.; Cantero-Escribano, J.M.; Redondo-Bravo, L.; San Juan-Sanz, I.; Robustillo-Rodela, A.; Cendejas-Bueno, E.; Influenza Working Group. Effect of vaccination, comorbidities and age on mortality and severe disease associated with influenza during the season 2016-2017 in a Spanish tertiary hospital. J. Infect. Public Health 2019, 12, 486–491. [Google Scholar] [CrossRef]
- Jung, C.H.; Son, J.W.; Kang, S.; Kim, W.J.; Kim, H.-S.; Kim, H.S.; Seo, M.; Shin, H.-J.; Lee, S.-S.; Jeong, S.J.; et al. Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status. Diabetes Metab. J. 2021, 45, 1–10. [Google Scholar] [CrossRef]
- Choi, W.S.; Cowling, B.J.; Noh, J.Y.; Song, J.Y.; Wie, S.-H.; Lee, J.S.; Bin Seo, Y.; Lee, J.; Jeong, H.W.; Kim, Y.K.; et al. Disease burden of 2013-2014 seasonal influenza in adults in Korea. PLoS ONE 2017, 12, e0172012. [Google Scholar] [CrossRef]
- Meduri, G.U.; Golden, E.; Freire, A.X.; Taylor, E.; Zaman, M.; Carson, S.J.; Gibson, M.; Umberger, R. Methylprednisolone infusion in early severe ARDS: Results of a randomized controlled trial. Chest 2007, 131, 954–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muthuri, S.G.; Venkatesan, S.; Myles, P.R.; Leonardi-Bee, J.; A Al Khuwaitir, T.S.; Al Mamun, A.; Anovadiya, A.P.; Azziz-Baumgartner, E.; Báez, C.; Bassetti, M.; et al. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A H1N1pdm09 virus infection: A meta-analysis of individual participant data. Lancet Respir. Med. 2014, 2, 395–404. [Google Scholar] [CrossRef] [Green Version]
- Mulpuru, S.; Li, L.; Ye, L.; Hatchette, T.; Andrew, M.K.; Ambrose, A.; Boivin, G.; Bowie, W.; Chit, A.; Dos Santos, G.; et al. Effectiveness of Influenza Vaccination on Hospitalizations and Risk Factors for Severe Outcomes in Hospitalized Patients With COPD. Chest 2019, 155, 69–78. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).