Evaluation of the Severity of Malocclusion in Children with Osteogenesis Imperfecta
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Control Samples
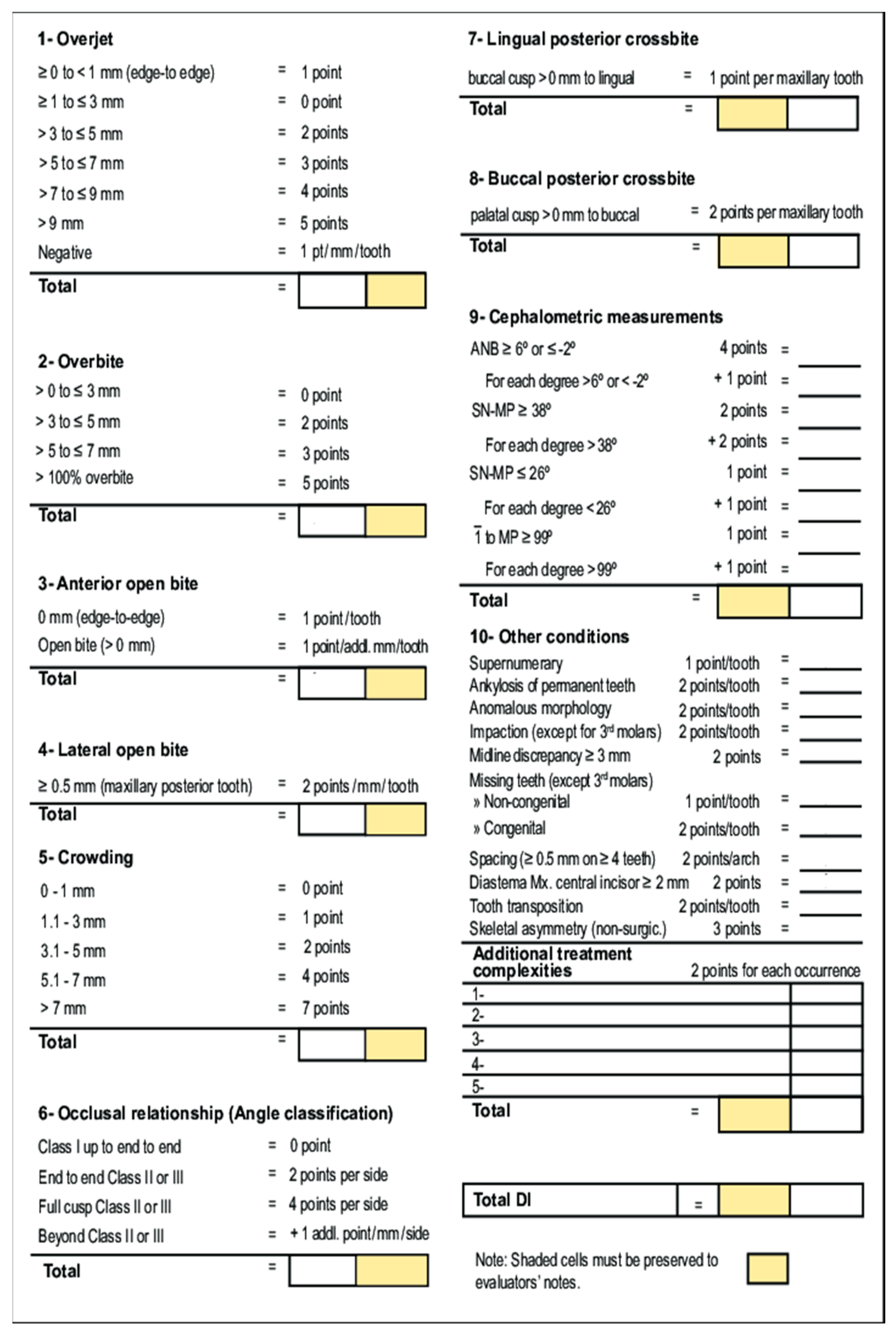
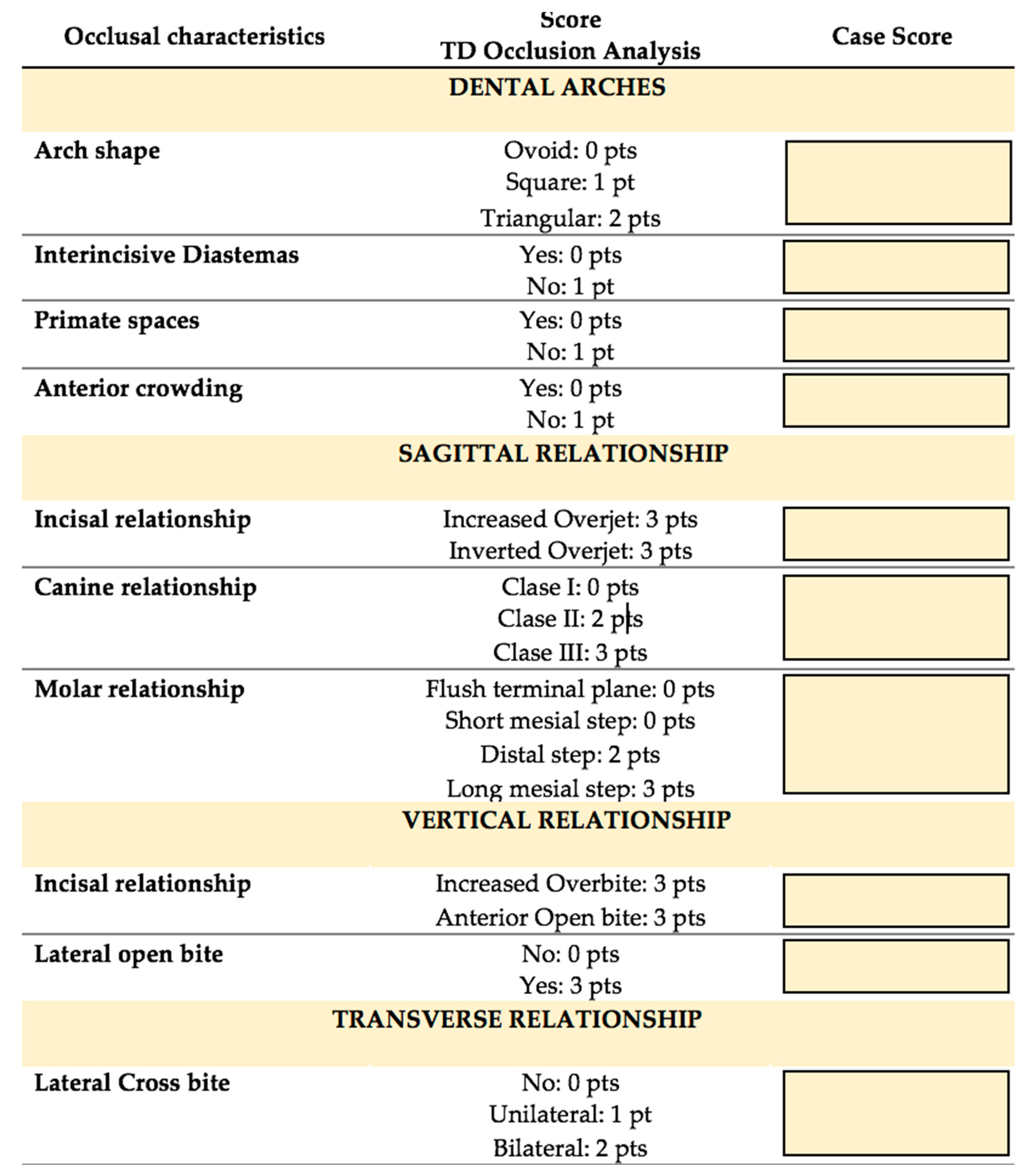
2.3. Method
2.4. Statistical Method
- Non-parametric Kolmogorov–Smirnov test with the Mann–Whitney-Wilcoxon test to compare the measurements of the quantitative variable between the control group and the OI Group.
- Non-parametric test for samples not related to the Kruskal–Wallis test to compare the quantitative variables between the control group and the different subgroups within the OI group (OI type I, OI type III, OI type IV and OI type V).
3. Results
3.1. Mixed and Permanent Dentition
3.2. Subgroup Sample Analysis
3.3. Primary Dentition
4. Discussion
4.1. Permanent and Mixed Dentition
4.2. Primary Dentition
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rauch, F.; Glorieux, F.H. Osteogenesis imperfecta. Lancet 2004, 363, 1377–1385. [Google Scholar] [CrossRef]
- Forlino, A.; Marini, J.C. Osteogenesis imperfecta. Lancet 2016, 387, 1657–1671. [Google Scholar] [CrossRef]
- Morello, R. Osteogenesis imperfecta and therapeutics. Matrix Biol. 2018, 71–72, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Forlino, A.; Cabral, W.A.; Barnes, A.M.; Marini, J.C. New perspectives on osteogenesis imperfecta. Nat. Rev. Endocrinol. 2011, 7, 540–557. [Google Scholar] [CrossRef]
- Bourgeois, A.B.; Aubry-Rozier, B.; Bonafé, L.; Laurent-Applegate, L.; Pioletti, D.P.; Zambelli, P.Y. Osteogenesis imperfecta: From diagnosis and multidisciplinary treatment to future perspectives. Swiss Med. Wkly. 2016, 146, w14322. [Google Scholar]
- Sillence, D.O.; Senn, A.; Danks, D.M. Genetic heterogeneity in osteogenesis imperfecta. J. Med. Genet. 1979, 16, 101–116. [Google Scholar] [CrossRef]
- Van Dijk, F.S.; Sillence, D.O. Osteogenesis imperfecta: Clinical diagnosis, nomenclature and severity assessment. Am. J. Med. Genet. A 2014, 164, 1470–1481. [Google Scholar] [CrossRef]
- Lim, J.; Grafe, I.; Alexander, S.; Lee, B. Genetic Causes and Mechanisms of Osteogenesis Imperfecta. Bone 2017, 102, 40–49. [Google Scholar] [CrossRef]
- Schwartz, S.; Tsipouras, P. Oral findings in osteogenesis imperfecta. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 1984, 57, 161–167. [Google Scholar] [CrossRef]
- O’Connell, A.; Marini, J. Evaluation of oral problems in an osteogenesis imperfecta population. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1999, 87, 189–196. [Google Scholar] [CrossRef]
- Waltimo-Sirén, J.; Tuurala, H.; Säämäki, E.; Holst, P.; Evälahti, M.; Arponen, H. Dental and dentoalveolar dimensions in individuals with osteogenesis imperfecta. Acta Odontol. Scand. 2021, 79, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Rossi, V.; Lee, B.; Marom, R. Osteogenesis imperfecta—Advancements in genetics and treatment. Curr. Opin. Pediatr. 2019, 31, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Retrouvey, J.M.; Taqi, D.; Tamimi, F.; Dagdeviren, D.; Glorieux, F.H.; Lee, B.; Hazboun, R.; Krakow, D.; Sutton, V.R. Oro-dental and cranio-facial characteristics of osteogenesis imperfecta type V. Eur. J. Med. Genet. 2019, 62, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.; Lin, S.; Hsu, K. The craniofacial characteristics of osteogenesis imperfecta patients. Eur. J. Orthod. 2007, 29, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Jensen, B.; Lund, A. Osteogénesis imperfecta: Clinical, cephalometric and biochemical investigations of OI type I, III and IV. J. Craniofac. Genet. Dev. Biol. 1997, 17, 121–132. [Google Scholar]
- Waltimo-Sirén, J.; Kolkka, M.; Pynnönen, S.; Kuurila, K.; Kaitila, I.; Outi Kovero, O. Craniofacial Features in Osteogenesis Imperfecta: A Cephalometric Study. Am. J. Med. Genet. 2005, 133A, 142–150. [Google Scholar] [CrossRef]
- Thuesen, K.; Gjørup, H.; Hald, J.D.; Schmidt, M.; Harsløf, T.; Langdahl, B.; Haubek, D. The dental perspective on osteogenesis imperfecta in a Danish adult population. BMC Oral Health 2018, 18, 175. [Google Scholar] [CrossRef]
- Najirad, M.; Madathil, S.A.; Rauch, F.; Sutton, V.R.; Lee, B.; Retrouvey, J.M.; Members of the Brittle Bone Diseases Consortium; Esfandiari, S. Malocclusion traits and oral health-related quality of life in children with osteogenesis imperfecta: A cross-sectional study. J. Am. Dent. Assoc. 2020, 151, 480–490.e2. [Google Scholar] [CrossRef] [PubMed]
- Jabbour, Z.; Al-Khateeb, A.; Eimar, H.; Retrouvey, J.M.; Glorieux, F.H.; Rauch, F.; Tamimi, F. Genotype and malocclusion in patients with osteogenesis imperfecta. Orthod. Craniofac. Res. 2018, 21, 71–77. [Google Scholar] [CrossRef]
- Rousseau, M.; Retrouvey, J.M.; Members of the Brittle Bone Disease Consortium. Osteogenesis imperfecta: Potential therapeutic approaches. Peer J. 2018, 6, e5464. [Google Scholar] [CrossRef]
- Rizkallah, J.; Schwartz, S.; Rauch, F.; Glorieux, F.; Vu, D.D.; Muller, K.; Retrouvey, J.M. Evaluation of the severity of malocclusions in children affected by osteogenesis imperfecta with the peer assessment rating and discrepancy indexes. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.S.; Binh, H.D.; Nguyen, K.M.; Maasalu, K.; Köks, S.; Märtson, A.; Saag, M.; Jagomägi, T. Occlusal features and need for orthodontic treatment in persons with osteogenesis imperfecta. Clin. Exp. Dent. Res. 2017, 3, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Assunção, Z.L. Class II malocclusion nonextraction treatment with growth control. Dent. Press J. Orthod. 2014, 19, 113–122. [Google Scholar] [CrossRef] [PubMed][Green Version]


| Type of OI * | n | Female | Male | Mean Age | Dental Phases | Subgroup 1 | |
|---|---|---|---|---|---|---|---|
| Mixed and Permanent | Primary | ||||||
| I | 18 | 10 | 8 | 8.67 | 13 | 5 | 10 |
| III | 19 | 11 | 8 | 12.11 | 18 | 1 | 9 |
| IV | 10 | 3 | 7 | 12.10 | 8 | 2 | 6 |
| V | 2 | 1 | 1 | 7.5 | 2 | 0 | 0 |
| Total | 49 | 25 | 24 | 11.6 | 41 | 8 | 25 |
| OI (I) | OI (III) | OI (IV) | OI Total | Control | |
|---|---|---|---|---|---|
| Total | 14.69 | 35.5 | 45.2 | 30.56 ** (26.6) | 13.27 ** (11.04) |
| Overjet | 3.23 | 8.67 | 2.75 | 5.59 * (9.4) | 2.32 * (3.1) |
| Overbite | 0.4 | 0.6 | 0.8 | 0.61 (1.2) | 0.34 (0.7) |
| Anterior open bite | 2.23 | 3.72 | 2.31 | 3.56 (6.7) | 1.66 (4.3) |
| Lateral open bite | 2.46 | 11.22 ** | 27.75 ** | 11.12 * (20.2) | 0.83 * (2.2) |
| Crowding | 2.12 | 1.06 | 1.44 | 1.54 (3.2) | 1.9 (2.1) |
| Occlusion | 1.38 | 4.44 ** | 3.87 ** | 3.2 (3.2) | 2.1 (2.1) |
| Lingual posterior crossbite | 2.2 | 2.8 | 3.79 | 2.93 (3.2) | 3.68 (6.5) |
| Bucal posterior crossbite | 0.0 | 0.2 | 0.1 | 0.1 (0.4) | 0.0 (0.0) |
| Other | 1.38 | 1.39 | 4.25 ** | 1.93 * (2.9) | 0.44 * (0.9) |
| OI | Control | |
|---|---|---|
| ANB *** Angle | 0.96 (1.7) | 0.32 (1.10) |
| SN-GoGn **** Angle | 3.24 * (3.7) | 0.44 * (1.16) |
| IMPA ** | 0.68 (1.67) | 0.40 (1.38) |
| OI | Control | |
|---|---|---|
| Total | 8.25 | 9.38 |
| Arch shape | 0.63 | 0.50 |
| Interincisive diastemas | 0.50 | 0.13 |
| Primate spaces | 0.25 | 0.25 |
| Incisive Crowding | 0.50 | 0.50 |
| Incisive Relationship | 2.25 | 2.25 |
| Canine Relationship | 1.13 | 1.38 |
| Molar Relationship | 1.25 | 1.88 |
| Lingual posterior crossbite | 0.38 | 0.25 |
| Bucal posterior crossbite | 0.25 | 0.75 |
| Anterior crossbite | 1.13 | 1.50 |
| Study Index | n | Male | Female | Mean Age | OI (I) n (%) | OI (III) n (%) | OI (IV) n (%) | OI (V) n (%) | OI (VI) n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Present study | DI | 41 | 21 | 20 | 11.61 | 13 (31.7) | 18 (43.9) | 8 (19.5) | 2 (4.8) | |
| Rizkallah et al. (2013) [21] | DI and PAR | 49 | 21 | 28 | 10.7 | 8 (16.3) | 11 (22.4) | 26 (53.1) | 2 (4.0) | 2 (4.0) |
| Nguyen et al. (2017) [22] | DAI and IOTN | 26 | 18 | 8 | 5–19 | 7 (26.9) | 10 (38.4) | 9 (34.6) | ||
| Jabbour et al. (2018) [19] | PAR | 49 | 21 | 28 | 10.7 | 7 (14.2) | 11 (22.4) | 27 (55.1) | 2 (4.0) | 2 (4.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Nova-García, M.J.; Bernal-Barroso, F.; Mourelle-Martínez, M.R.; Gallardo-López, N.E.; Diéguez-Pérez, M.; Feijoo-García, G.; Burgueño-Torres, L. Evaluation of the Severity of Malocclusion in Children with Osteogenesis Imperfecta. J. Clin. Med. 2022, 11, 4862. https://doi.org/10.3390/jcm11164862
De Nova-García MJ, Bernal-Barroso F, Mourelle-Martínez MR, Gallardo-López NE, Diéguez-Pérez M, Feijoo-García G, Burgueño-Torres L. Evaluation of the Severity of Malocclusion in Children with Osteogenesis Imperfecta. Journal of Clinical Medicine. 2022; 11(16):4862. https://doi.org/10.3390/jcm11164862
Chicago/Turabian StyleDe Nova-García, Manuel Joaquín, Fabiola Bernal-Barroso, Maria Rosa Mourelle-Martínez, Nuria Esther Gallardo-López, Montserrat Diéguez-Pérez, Gonzalo Feijoo-García, and Laura Burgueño-Torres. 2022. "Evaluation of the Severity of Malocclusion in Children with Osteogenesis Imperfecta" Journal of Clinical Medicine 11, no. 16: 4862. https://doi.org/10.3390/jcm11164862
APA StyleDe Nova-García, M. J., Bernal-Barroso, F., Mourelle-Martínez, M. R., Gallardo-López, N. E., Diéguez-Pérez, M., Feijoo-García, G., & Burgueño-Torres, L. (2022). Evaluation of the Severity of Malocclusion in Children with Osteogenesis Imperfecta. Journal of Clinical Medicine, 11(16), 4862. https://doi.org/10.3390/jcm11164862






