Multivalvular Endocarditis: A Rare Condition with Poor Prognosis
Abstract
:1. Introduction
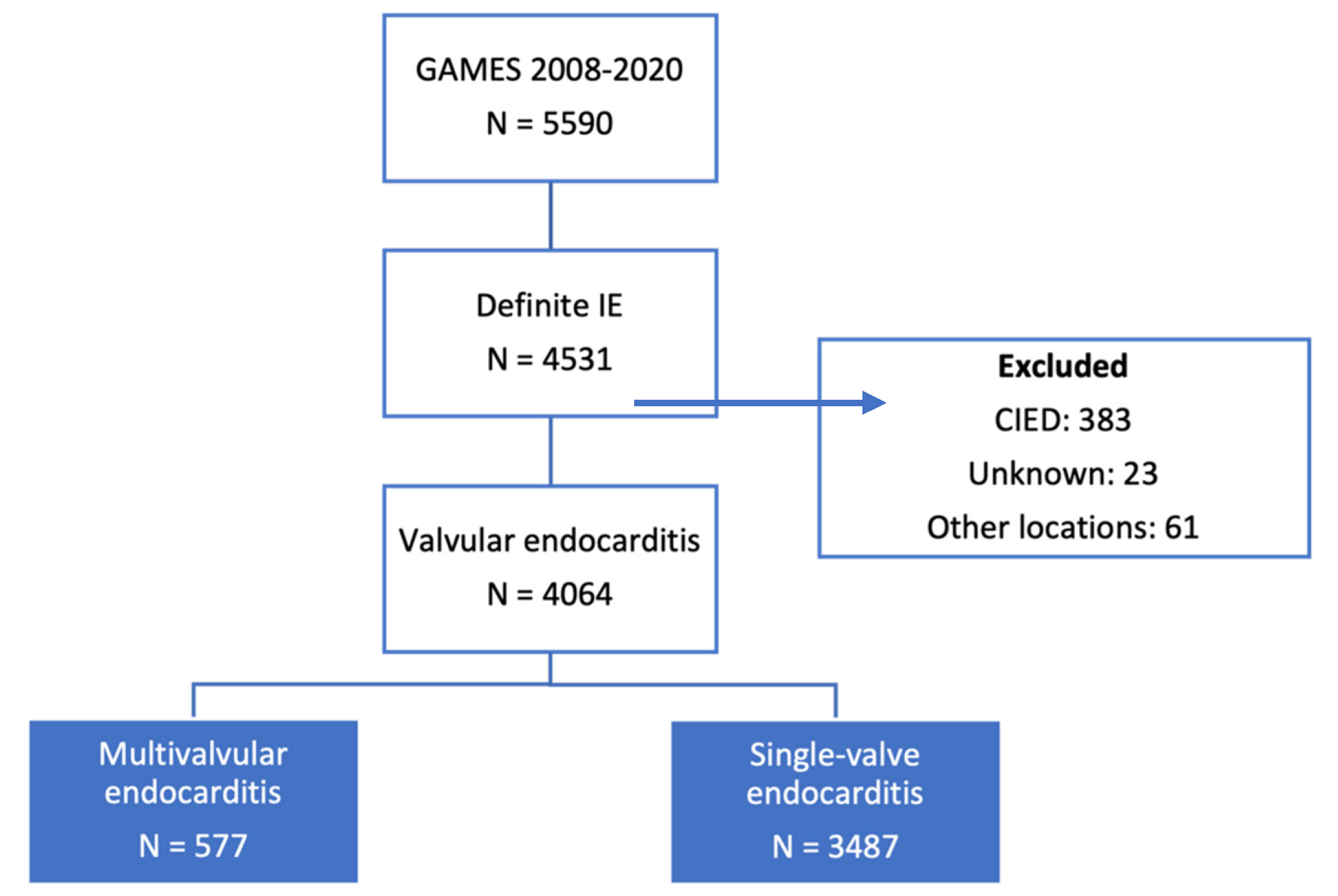
2. Materials and Methods
Statistical Methods
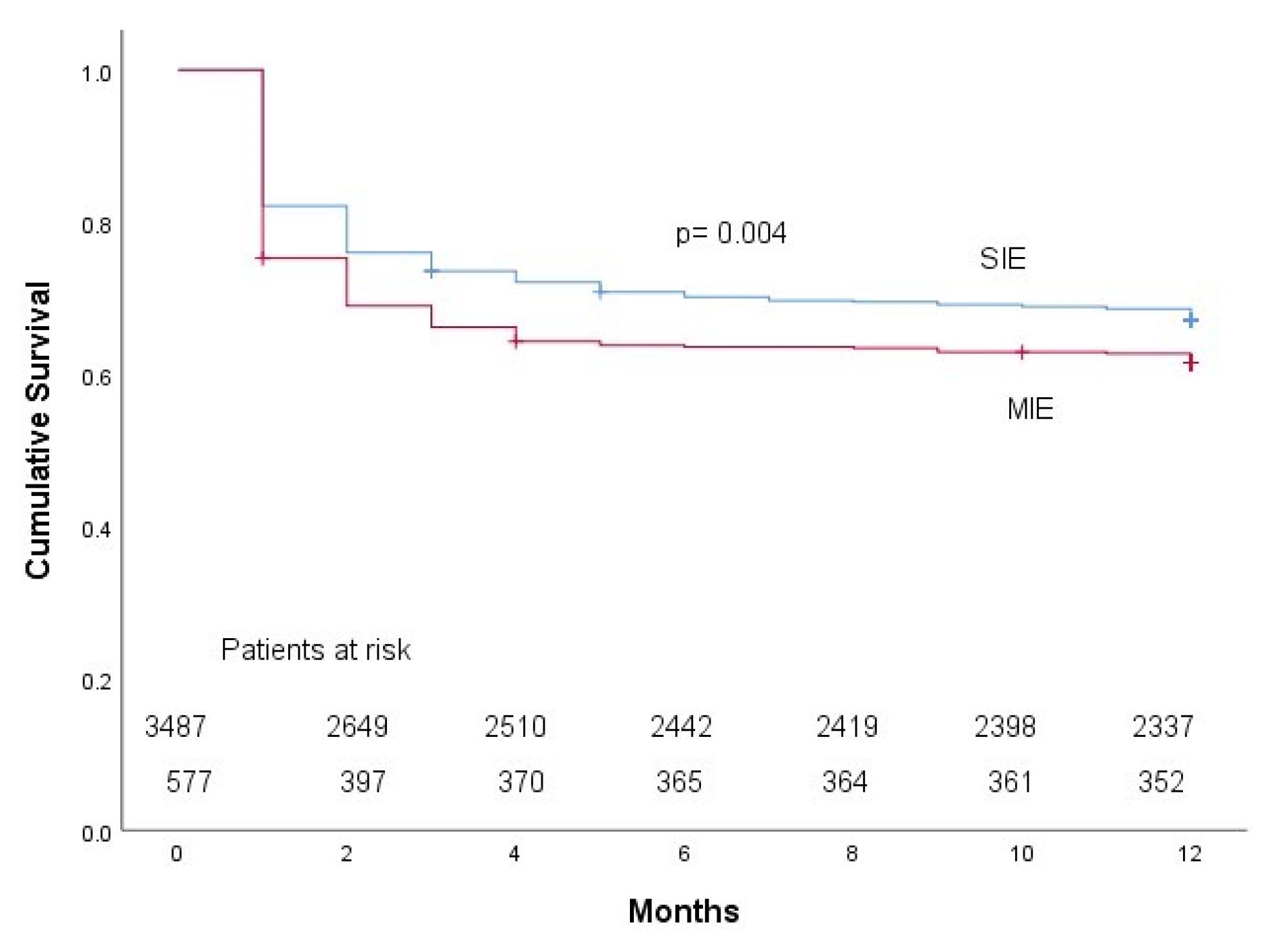
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Habib, G.; Lancellotti, P.; Antunes, M.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3123. [Google Scholar] [CrossRef]
- Kim, N.; Lazar, J.M.; Cunha, B.A.; Liao, W.; Minnaganti, V. Multi-valvular endocarditis. Clin. Microbiol. Infect. 2000, 6, 207–212. [Google Scholar] [CrossRef]
- Yao, F.; Han, L.; Xu, Z.Y.; Huang, S.D.; Wang, Z.N.; Lu, F.L.; Yao, Y.L. Surgical treatment of multivalvular endocarditis: Twenty-one-year single center experience. J. Thorac. Cardiovasc. Surg. 2009, 137, 1475–1480. [Google Scholar] [CrossRef]
- Mihaljevic, T.; Byrne, J.G.; Cohn, L.H.; Aranki, S.F. Long-term results of multivalve surgery for infective multivalve endocarditis. Eur. J. Cardiothorac. Surg. 2001, 20, 842–846. [Google Scholar] [CrossRef]
- López, J.; Revilla, A.; Vilacosta, I.; Sevilla, T.; García, H.; Gómez, I.; Pozo, E.; Sarriá, C.; San Román, J.A. Multiple-valve infective endocarditis: Clinical, microbiologic, echocardiographic, and prognostic profile. Medicine 2011, 90, 231–236. [Google Scholar] [CrossRef]
- Gillinov, A.M.; Diaz, R.; Blackstone, E.H.; Pettersson, G.B.; Sabik, J.F.; Lytle, B.W.; Cosgrove, D.M., 3rd. Double valve endocarditis. Ann. Thorac. Surg. 2001, 71, 1874–1879. [Google Scholar] [CrossRef]
- David, T.E.; Gavra, G.; Feindel, C.M.; Regesta, T.; Armstrong, S.; Maganti, M.D. Surgical treatment of active infective endocarditis: A continued challenge. J. Thorac. Cardiovasc. Surg. 2007, 133, 144–149. [Google Scholar] [CrossRef]
- Sheikh, A.M.; Elhenawy, A.M.; Maganti, M.; Armstrong, S.; David, T.E.; Feindel, C.M. Outcomes of double valve surgery for active infective endocarditis. J. Thorac. Cardiovasc. Surg. 2009, 138, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Ota, T.; Gleason, T.G.; Salizzoni, S.; Wei, L.M.; Toyoda, Y.; Bermudez, C. Midterm surgical outcomes of noncomplicated active native multivalve endocarditis: Single-center experience. Ann. Thorac. Surg. 2011, 91, 1414–1419. [Google Scholar] [CrossRef] [PubMed]
- Musci, M.; Siniawski, H.; Pasic, M.; Grauhan, O.; Weng, Y.; Meyer, R.; Yankah, C.A.; Hetzer, R. Surgical treatment of rightsided active infective endocarditis with or without involvement of the left heart: 20-year single center experience. Eur. J. Cardiothorac. Surg. 2007, 32, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Selton-Suty, C.; Doco-Lecompte, T.; Bernard, Y.; Duval, X.; Letranchant, L.; Delahaye, F.; Célard, M.; Alla, F.; Carteaux, J.P.; Hoen, B.; et al. Clinical and microbiologic features of multivalvular endocarditis. Curr. Infect. Dis. Rep. 2010, 12, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Casabé, J.H.; Deschle, H.; Cortés, C.; Stutzbach, P.; Hershson, A.; Nagel, C.; Guevara, E.; Torino, A.; Raffaelli, H.; Favaloro, R.R.; et al. Predictores de mortalidad hospitalaria en 186 episodios de endocarditis infecciosa activa en un centro de tercer nivel (1992–2001) [Predictors of hospital mortality in 186 cases of active infective endocarditis treated in a tertiary medical center (1992–2001)]. Rev. Esp. Cardiol. 2003, 56, 578–585. [Google Scholar] [CrossRef]
- Meszaros, K.; Nujic, S.; Sodeck, G.H.; Englberger, L.; König, T.; Schönhoff, F.; Reineke, D.; Roost-Krähenbühl, E.; Schmidli, J.; Czerny, M.; et al. Long-term results after operations for active infective endocarditis in native and prosthetic valves. Ann. Thorac. Surg. 2012, 94, 1204–1210. [Google Scholar] [CrossRef]
- Scheggi, V.; Merilli, I.; Marcucci, R.; Del Pace, S.; Olivotto, I.; Zoppetti, N.; Ceschia, N.; Andrei, V.; Alterini, B.; Stefàno, P.L.; et al. Predictors of mortality and adverse events in patients with infective endocarditis: A retrospective real world study in a surgical centre. BMC Cardiovasc. Disord. 2021, 21, 28. [Google Scholar] [CrossRef] [PubMed]
- Grover, F.L.; Cohen, D.J.; Oprian, C.; Henderson, W.G.; Sethi, G.; Hammermeister, K.E. Determinants of the occurrence of and survival from prosthetic valve endocarditis. Experience of the veterans affairs cooperative study on valvular heart disease. J. Thorac. Cardiovasc. Surg. 1994, 108, 207–214. [Google Scholar] [CrossRef]
- Armiñanzas, C.; Fariñas-Alvarez, C.; Zarauza, J.; Muñoz, P.; González Ramallo, V.; Martínez-Sellés, M.; Miró, J.M.; Pericás, J.M.; Goenaga, M.A.; Ojeda, G. Role of age and comorbidities in mortality of patients with infective endocarditis. Eur. J. Intern. Med. 2019, 64, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sellés, M.; Munoz, P.; Arnáiz, A.; Moreno, M.; Gálvez, J.; Rodriguez-Roda, J.; de Alarcón, A.; García, E.; Fariñas, M.; Miró, J.M.; et al. Valve surgery in active infective endocarditis: A simple score to predict in-hospital prognosis. Int. J. Cardiol. 2014, 175, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Mateos, R.; Boix-Palop, L.; Muñoz, P.; Mestres, C.A.; Marín, M.; Pedraz, A.; de Alarcón, A.; Gutiérrez, E.; Hernández, M.; Goenaga, M.A. Infective endocarditis in patients with cardiac implantable electronic devices: A nationwide study. Europace 2020, 22, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- Biezma, M.I.; Muñoz, P.; De la Villa, S.; Fariñas-Álvarez, M.C.; Arnáiz de Las Revillas, F.; Gutierrez-Carretero, E.; De Alarcón, A.; Rodríguez-García, R.; Llopis, J.; Goenaga, M.Á.; et al. Infective endocarditis in diabetic patients: A different profile with prognostic consequences. J. Clin. Med. 2022, 11, 2651. [Google Scholar] [CrossRef]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Moreillon, P.; Que, Y.A. Infective endocarditis. Lancet 2004, 363, 139–149. [Google Scholar] [CrossRef]
- Mueller, X.M.; Tevaearai, H.T.; Stumpe, F.; Fischer, A.P.; Hurni, M.; Ruchat, P.; von Segesser, L.K. Multivalvular surgery for infective endocarditis. Cardiovasc. Surg. 1999, 7, 402–408. [Google Scholar] [CrossRef]
- Piper, C.; Hetzer, R.; Korfer, R.; Bergemann, R.; Horstkotte, D. The importance of secondary mitral valve involvement in primary aortic valve endocarditis; the mitral kissing vegetation. Eur. Heart J. 2002, 23, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.S.; Na, C.Y.; Oh, S.S.; Kim, J.H.; Yie, G.S.; Han, J.W.; Chae, M.C. Single and multiple valve surgery in native valve infective endocarditis. Korean J. Thorac. Cardiovasc. Surg. 2013, 46, 256–264. [Google Scholar] [CrossRef]
- Hill, E.E.; Herijgers, P.; Herregods, M.C.; Peetermans, W.E. Evolving trends in infective endocarditis. Clin. Microbiol. Infect. 2006, 12, 5–12. [Google Scholar] [CrossRef]
- Holland, D.J.; Simos, P.A.; Yoon, J.; Sivabalan, P.; Ramnarain, J.; Runnegar, N.J. Infective Endocarditis: A Contemporary Study of Microbiology, Echocardiography and Associated Clinical Outcomes at a Major Tertiary Referral Centre. Heart Lung Circ. 2020, 29, 840–850. [Google Scholar] [CrossRef]
| SIE (3487) | MIE (577) | p | |
|---|---|---|---|
| Age, mean (IQR 1) | 69 (57–77) | 67 (57–76) | 0.273 |
| Sex (Men) | 2341 (67.1%) | 421 (72.9%) | 0.005 |
| Location | |||
| Aortic | 1827 (52.4%) | 550 (95.3%) | <0.001 |
| Mitral | 1428 (41.0%) | 552 (95.7%) | <0.001 |
| Tricuspid | 177 (5.1%) | 57 (9.9%) | <0.001 |
| Pulmonary | 50 (1.4%) | 18 (3.1%) | 0.003 |
| Native IE | 2326 (66.7%) | 450 (78.0%) | <0.001 |
| Prosthetic IE | 1169 (33.5%) | 194 (33.6%) | 0.963 |
| Etiology | |||
| Staphylococcus aureus | 842 (24.1%) | 113 (19.6%) | 0.017 |
| Coagulase-negative staphylococci | 618 (17.7%) | 94 (16.3%) | 0.402 |
| Enterococcus | 541 (15.5%) | 109 (18.9%) | 0.040 |
| Streptococcus | 999 (28.6%) | 192 (33.3%) | 0.024 |
| Candida | 50 (1.4%) | 7 (1.2%) | 0.676 |
| Clinical course | |||
| Vegetation present | 2759 (79.1%) | 493 (85.4%) | <0.001 |
| Intracardiac complications | 1261 (36.2%) | 291 (50.4%) | <0.001 |
| Perforation or rupture | 533 (15.2%) | 150 (25.9%) | <0.001 |
| Pseudoaneurysm | 242 (6.9%) | 56 (9.7%) | 0.018 |
| Abscess | 682 (19.5%) | 151 (26.1%) | 0.001 |
| Intracardiac fistula | 98 (2.8%) | 26 (4.5%) | 0.028 |
| Vascular phenomenon | 378 (10.8%) | 60 (10.4%) | 0.751 |
| New heart murmur | 1261 (36.2%) | 263 (45.6%) | <0.001 |
| Heart failure | 1489 (42.7%) | 305 (52.9%) | <0.001 |
| Persistent bacteriemia | 404 (11.6%) | 69 (12.0%) | 0.796 |
| Central nervous system involvement | 777 (22.3%) | 140 (24.3%) | 0.292 |
| Embolization | 834 (23.9%) | 153 (26.5%) | 0.177 |
| Renal failure | 1278 (36.7%) | 220 (38.1%) | 0.495 |
| Septic shock | 465 (13.3%) | 94 (16.3%) | 0.056 |
| Sepsis | 648 (18.6%) | 105 (18.2%) | 0.825 |
| Indication for surgery | 2360 (67.7%) | 491 (85.1%) | <0.001 |
| Cardiac surgery | 1616 (46.3%) | 325 (56.3%) | <0.001 |
| Surgery indicated not performed | 772 (22.1%) | 168 (29.1%) | <0.001 |
| Mean hospital stay (IQR) | 36 (22–52) | 38 (22–54) | 0.368 |
| Antibiotic treatment days, mean (IQR) | 40 (28–46) | 38 (21–45) | 0.368 |
| In-hospital mortality | 937 (26.9%) | 198 (34.3%) | <0.001 |
| 1-year mortality | 1146 (32.9%) | 222 (38.5%) | 0.008 |
| IE Recurrence in those alive | 42 (1.6%) | 7 (1.8%) | 0.777 |
| (A) | ||
| OR (95% CI) | p | |
| Male sex | 0.8 (0.7–0.9) | 0.041 |
| Charlson comorbidity index | 1.12 (1.09–1.16) | <0.001 |
| Heart failure | 2.9 (2.5–3.4) | <0.001 |
| Multivalvular IE | 1.3 (1.1–1.7) | 0.004 |
| Severe sepsis | 2.1 (1.8–2.6) | <0.001 |
| S. aureus | 1.7 (1.4–2.1) | <0.001 |
| Nosocomial IE | 1.6 (1.3–1.9) | <0.001 |
| Intracardiac abscess | 1.3 (1.1–1.7) | 0.004 |
| Age (years) | 1.015 (1.008–1.022) | <0.001 |
| (B) | ||
| OR (95% CI) | p | |
| Mitral location | 1.2 (1.0–1.4) | 0.017 |
| Charlson comorbidity index | 1.15 (1.12–1.19) | <0.001 |
| Heart failure | 2.5 (2.2–2.9) | <0.001 |
| Persistent bacteriemia | 1.2 (1.0–1.5) | 0.043 |
| Severe sepsis | 2.0 (1.7–2.4) | <0.001 |
| S. aureus | 1.4 (1.2–1.7) | <0.001 |
| Nosocomial IE | 1.6 (1.3–1.9) | <0.001 |
| Intracardiac abscess | 1.4 (1.1–1.7) | <0.001 |
| Age (years) | 1.015 (1.015–1.009) | <0.001 |
| First Author, Year | N and Cohort Type | MIE | Mean/Median Age (Years) | Main Etiologies | MIE in-Hospital Mortality |
|---|---|---|---|---|---|
| Kim et al., 2000 [2] | 77 | 14 (31%) | 65 | S. aureus 43% S. viridans 36% | 21% overall 29% surgery |
| Mihalhevic et al., 2001 [4] | 63 MIE surgery | All | 49 | S. viridans 28% S. aureus | 16% |
| Gillinov et al., 2001 [6] | 54 MIE surgery | All | 50 | Streptococci 70% Staphylococci 18% | 0% |
| David et al., 2007 [7] | 383 IE surgery | 101 (26%) | 51 | S. aureus 23% S. viridans 18% | 12% |
| Yao et al., 2009 [3] | 388 IE surgery | 48 (12%) | 42 | S. viridans 29% S. aureus 19% | 13% |
| Sheikh et al., 2009 [8] | 90 MIE surgery | All | 53 | S. aureus 16% S. viridans 14% | 15% |
| Selton et al., 2010 [11] | 300 IE 511 IE | 42 (14%) 88 (17%) | 58 60 | Streptococci 64% S. aureus 14% | 26% 23% |
| López et al., 2011 [15] | 680 IE | 115 (17%) | 58 | S. aureus 22% Coagulase-negative staphylococci 18% | 30% |
| Ota et al., 2011 [9] | 152 native valve IE surgery | 35 (23%) | 47 | S. aureus 22% S. viridans 22% | 9% |
| Kim et al., 2013 [24] | 90 native valve IE surgery | 23 (25%) | 47 | S. viridans 70% | 0% |
| Our cohort | 4064 IE | 577 (14%) | 67 | S. viridans 33% S. aureus 20% | 34% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez-Zaballos, S.; González-Ramallo, V.; Quintana, E.; Muñoz, P.; de la Villa-Martínez, S.; Fariñas, M.C.; Arnáiz-de las Revillas, F.; de Alarcón, A.; Rodríguez-Esteban, M.Á.; Miró, J.M.; et al. Multivalvular Endocarditis: A Rare Condition with Poor Prognosis. J. Clin. Med. 2022, 11, 4736. https://doi.org/10.3390/jcm11164736
Álvarez-Zaballos S, González-Ramallo V, Quintana E, Muñoz P, de la Villa-Martínez S, Fariñas MC, Arnáiz-de las Revillas F, de Alarcón A, Rodríguez-Esteban MÁ, Miró JM, et al. Multivalvular Endocarditis: A Rare Condition with Poor Prognosis. Journal of Clinical Medicine. 2022; 11(16):4736. https://doi.org/10.3390/jcm11164736
Chicago/Turabian StyleÁlvarez-Zaballos, Sara, Victor González-Ramallo, Eduard Quintana, Patricia Muñoz, Sofía de la Villa-Martínez, M. Carmen Fariñas, Francisco Arnáiz-de las Revillas, Arístides de Alarcón, M. Ángeles Rodríguez-Esteban, José M. Miró, and et al. 2022. "Multivalvular Endocarditis: A Rare Condition with Poor Prognosis" Journal of Clinical Medicine 11, no. 16: 4736. https://doi.org/10.3390/jcm11164736
APA StyleÁlvarez-Zaballos, S., González-Ramallo, V., Quintana, E., Muñoz, P., de la Villa-Martínez, S., Fariñas, M. C., Arnáiz-de las Revillas, F., de Alarcón, A., Rodríguez-Esteban, M. Á., Miró, J. M., Goenaga, M. A., Goikoetxea-Agirre, J., García-Vázquez, E., Boix-Palop, L., Martínez-Sellés, M., & on behalf of GAMES. (2022). Multivalvular Endocarditis: A Rare Condition with Poor Prognosis. Journal of Clinical Medicine, 11(16), 4736. https://doi.org/10.3390/jcm11164736









