Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
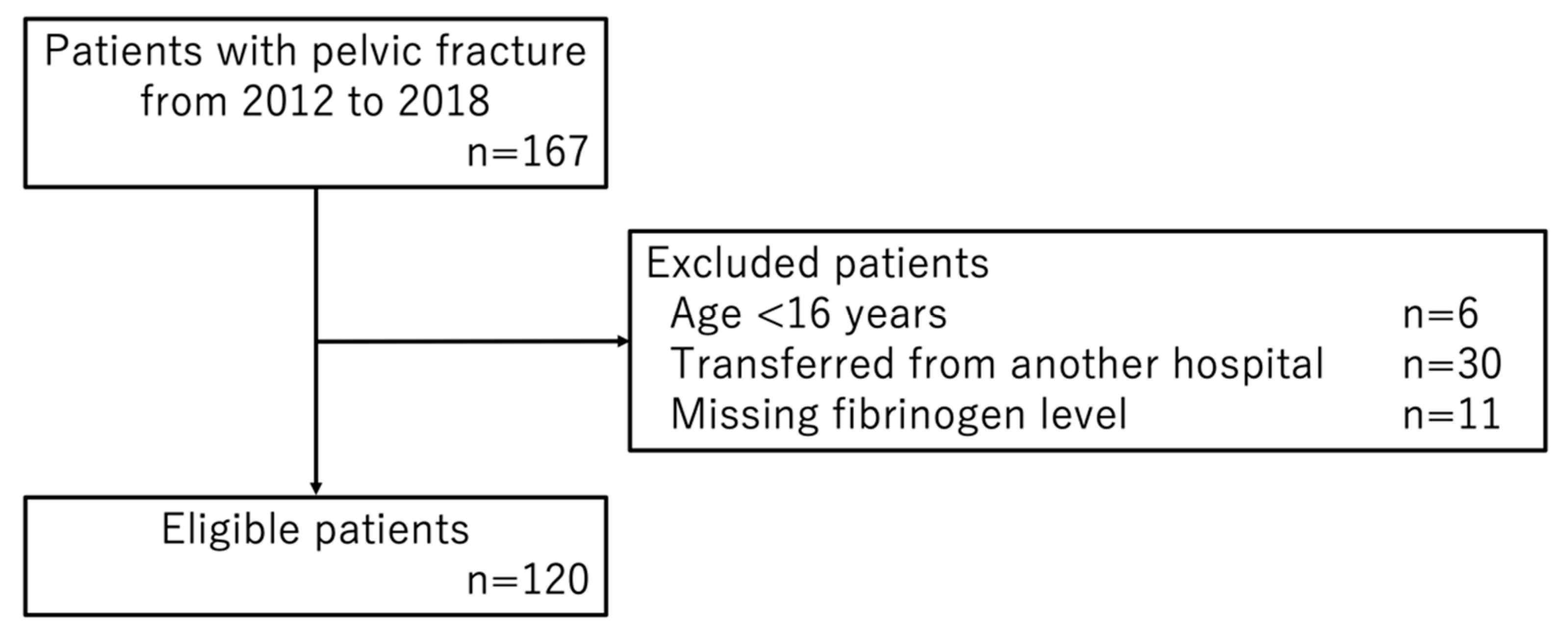
2.3. Participants
2.4. Variables
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. New Publications Show Injuries Kill More Than Five Million People a Year; Road Crashes Account for 1 of 5 Injury-Related Deaths. Available online: https://www.who.int/news/item/12-05-2003-new-publications-show-injuries-kill-more-than-five-million-people-a-year (accessed on 16 March 2022).
- Kauvar, D.S.; Lefering, R.; Wade, C.E. Impact of Hemorrhage on Trauma Outcome: An Overview of Epidemiology, Clinical Presentations, and Therapeutic Considerations. J. Trauma Inj. Infect. Crit. Care 2006, 60, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holcomb, J.B.; Jenkins, D.; Rhee, P.; Johannigman, J.; Mahoney, P.; Mehta, S.; Cox, E.D.; Gehrke, M.J.; Beilman, G.J.; Schreiber, M.; et al. Damage Control Resuscitation: Directly Addressing the Early Coagulopathy of Trauma. J. Trauma Inj. Infect. Crit. Care 2007, 62, 307–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brohi, K.; Singh, J.; Heron, M.; Coats, T. Acute Traumatic Coagulopathy. J. Trauma 2003, 54, 1127–1130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maegele, M.; Lefering, R.; Yucel, N.; Tjardes, T.; Rixen, D.; Paffrath, T.; Simanski, C.; Neugebauer, E.; Bouillon, B. Early Coagulopathy in Multiple Injury: An Analysis from the German Trauma Registry on 8724 Patients. Injury 2007, 38, 298–304. [Google Scholar] [CrossRef]
- Floccard, B.; Rugeri, L.; Faure, A.; Saint Denis, M.; Boyle, E.M.; Peguet, O.; Levrat, A.; Guillaume, C.; Marcotte, G.; Vulliez, A.; et al. Early Coagulopathy in Trauma Patients: An on-Scene and Hospital Admission Study. Injury 2012, 43, 26–32. [Google Scholar] [CrossRef]
- MacLeod, J.B.A.; Lynn, M.; McKenney, M.G.; Cohn, S.M.; Murtha, M. Early Coagulopathy Predicts Mortality in Trauma. J. Trauma 2003, 55, 39–44. [Google Scholar] [CrossRef]
- Demetriades, D.; Karaiskakis, M.; Toutouzas, K.; Alo, K.; Velmahos, G.; Chan, L. Pelvic Fractures: Epidemiology and Predictors of Associated Abdominal Injuries and Outcomes. J. Am. Coll. Surg. 2002, 195, 1–10. [Google Scholar] [CrossRef]
- Wu, Y.T.; Cheng, C.T.; Tee, Y.S.; Fu, C.Y.; Liao, C.H.; Hsieh, C.H. Pelvic Injury Prognosis Is More Closely Related to Vascular Injury Severity than Anatomical Fracture Complexity: The WSES Classification for Pelvic Trauma Makes Sense. World J. Emerg. Surg. 2020, 15, 1–9. [Google Scholar] [CrossRef]
- Smith, W.; Williams, A.; Agudelo, J.; Shannon, M.; Morgan, S.; Stahel, P.; Moore, E. Early Predictors of Mortality in Hemodynamically Unstable Pelvis Fractures. J. Orthop. Trauma 2007, 21, 31–37. [Google Scholar] [CrossRef]
- Osterhoff, G.; Scheyerer, M.J.; Fritz, Y.; Bouaicha, S.; Wanner, G.A.; Simmen, H.P.; Werner, C.M.L. Comparing the Predictive Value of the Pelvic Ring Injury Classification Systems by Tile and by Young and Burgess. Injury 2014, 45, 742–747. [Google Scholar] [CrossRef]
- Kim, M.J.; Lee, J.G.; Lee, S.H. Factors predicting the need for hemorrhage control intervention in patients with blunt pelvic trauma: A retrospective study. BMC Surg. 2018, 18, 101. [Google Scholar] [CrossRef] [Green Version]
- Hayakawa, M. Dynamics of fibrinogen in acute phases of trauma. J. Intensive Care 2017, 5, 3. [Google Scholar] [CrossRef] [Green Version]
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J. The European Guideline on Management of Major Bleeding and Coagulopathy Following Trauma: Fifth Edition. Crit. Care 2019, 23, 1–74. [Google Scholar] [CrossRef] [Green Version]
- Inaba, K.; Karamanos, E.; Lustenberger, T.; Schöchl, H.; Shulman, I.; Nelson, J.; Rhee, P.; Talving, P.; Lam, L.; Demetriades, D. Impact of Fibrinogen Levels on Outcomes after Acute Injury in Patients Requiring a Massive Transfusion. J. Am. Coll. Surg. 2013, 216, 290–297. [Google Scholar] [CrossRef]
- Hagemo, J.S.; Stanworth, S.; Juffermans, N.P.; Brohi, K.; Cohen, M.J.; Johansson, P.I.; Røislien, J.; Eken, T.; Næss, P.A.; Gaarder, C. Prevalence, Predictors and Outcome of Hypofibrinogenaemia in Trauma: A Multicentre Observational Study. Crit. Care 2014, 18, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Japanese Association for the Surgery of Trauma Japan Expert Trauma Evaluation and Care (JETECTM) Guideline, 2nd ed.; Herusu Shuppan: Tokyo, Japan, 2018.
- Denis, F.; Davis, S.; Comfort, T. Sacral fractures: An important problem: Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar] [CrossRef]
- Coccolini, F.; Stahel, P.F.; Montori, G.; Biffl, W.; Horer, T.M.; Catena, F.; Kluger, Y.; Moore, E.E.; Peitzman, A.B.; Ivatury, R.; et al. Pelvic Trauma: WSES Classification and Guidelines. World J. Emerg. Surg. 2017, 12, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Ohmori, T.; Kitamura, T.; Tanaka, K.; Saisaka, Y.; Ishihara, J.; Onishi, H.; Nojima, T.; Yamamoto, K.; Matusmoto, T.; Tokioka, T. Admission Fibrinogen Levels in Severe Trauma Patients: A Comparison of Elderly and Younger Patients. Injury 2015, 46, 1779–1783. [Google Scholar] [CrossRef]
- Brohi, K.; Cohen, M.J.; Ganter, M.T.; Schultz, M.J.; Levi, M.; Mackersie, R.C.; Pittet, J.F. Acute Coagulopathy of Trauma: Hypoperfusion Induces Systemic Anticoagulation and Hyperfibrinolysis. J. Trauma Inj. Infect. Crit. Care 2008, 64, 1211–1217. [Google Scholar] [CrossRef] [Green Version]
- Aoki, M.; Ogura, T.; Hagiwara, S.; Nakamura, M.; Oshima, K. Prediction of Arterial Extravasation in Pelvic Fracture Patients with Stable Hemodynamics Using Coagulation Biomarkers. World J. Emerg. Surg. 2019, 14, 1–8. [Google Scholar] [CrossRef]
- Cullinane, D.C.; Schiller, H.J.; Zielinski, M.D.; Bilaniuk, J.W.; Collier, B.R.; Como, J.; Holevar, M.; Sabater, E.A.; Sems, S.A.; Vassy, W.M.; et al. Eastern Association for the Surgery of Trauma Practice Management Guidelines for Hemorrhage in Pelvic Fracture-Update and Systematic Review. J. Trauma Inj. Infect. Crit. Care 2011, 71, 1850–1868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, J.F.; Shih, L.Y.; Wong, Y.C.; Lin, B.C.; Hsu, Y.P. Repeat Transcatheter Arterial Embolization for the Management of Pelvic Arterial Hemorrhage. J. Trauma Inj. Infect. Crit. Care 2009, 66, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Frevert, S.; Dahl, B.; Lönn, L. Update on the Roles of Angiography and Embolisation in Pelvic Fracture. Injury 2008, 39, 1290–1294. [Google Scholar] [CrossRef] [PubMed]
- Durkin, A.; Sagi, H.C.; Durham, R.; Flint, L. Contemporary Management of Pelvic Fractures. Am. J. Surg. 2006, 192, 211–223. [Google Scholar] [CrossRef]
- Dyer, G.S.M.; Vrahas, M.S. Review of the Pathophysiology and Acute Management of Haemorrhage in Pelvic Fracture. Injury 2006, 37, 602–613. [Google Scholar] [CrossRef]
- Rodrigues-Pinto, R.; Kurd, M.F.; Schroeder, G.D.; Kepler, C.K.; Krieg, J.C.; Holstein, J.H.; Bellabarba, C.; Firoozabadi, R.; Oner, F.C.; Kandziora, F.; et al. Sacral Fractures and Associated Injuries. Glob. Spine J. 2017, 7, 609–616. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.T.; Feng, C.C.; Wu, C.C.; Hsiao, C.W.; Weng, P.W.; Jao, S.W. The Use of Table Fixation Staples to Control Massive Presacral Hemorrhage: A Successful Alternative Treatment. Report of a Case. Dis. Colon Rectum 2009, 52, 159–161. [Google Scholar] [CrossRef]
- Lou, Z.; Zhang, W.; Meng, R.G.; Fu, C.G. Massive Presacral Bleeding during Rectal Surgery: From Anatomy to Clinical Practice. World J. Gastroenterol. 2013, 19, 4039–4044. [Google Scholar] [CrossRef]
- Naude, G.P.; Bongard, F.S. Gunshot Injuries of the Sacrum. J. Trauma 1996, 40, 1–8. [Google Scholar] [CrossRef]
- Heetveld, M.J.; Harris, I.; Schlaphoff, G.; Balogh, Z.; D’Amours, S.K.; Sugrue, M. Hemodynamically Unstable Pelvic Fractures: Recent Care and New Guidelines. World J. Surg. 2004, 28, 904–909. [Google Scholar] [CrossRef]
- Gando, S.; Shiraishi, A.; Wada, T.; Yamakawa, K.; Fujishima, S.; Saitoh, D.; Kushimoto, S.; Ogura, H.; Abe, T.; Otomo, Y. A Multicenter Prospective Validation Study on Disseminated Intravascular Coagulation in Trauma-Induced Coagulopathy. J. Thromb. Haemost. 2020, 18, 2232–2244. [Google Scholar] [CrossRef]
| Characteristics | n = 120 | |
|---|---|---|
| Age, years, mean (SD) | 47.3 | (20.1) |
| Male sex, n (%) | 69 | (57.5) |
| Mechanism, n (%) | ||
| Traffic collision | 67 | (55.8) |
| Car crash | 8 | (6.7) |
| Motorcycle crash | 34 | (28.3) |
| Bicycle crash | 8 | (6.7) |
| Pedestrian | 17 | (14.2) |
| Fall from height | 49 | (40.8) |
| Others | 4 | (3.3) |
| ISS, median (IQR) | 24 | (13–41) |
| Shock on arrival, n (%) | 24 | (20.0) |
| Pelvic fracture site, n (%) | ||
| Ilium | 39 | (32.5) |
| Unilateral | 37 | (30.8) |
| Bilateral | 2 | (1.7) |
| Pubis | 67 | (55.8) |
| Unilateral | 48 | (40.0) |
| Bilateral | 19 | (15.8) |
| Ischium | 53 | (44.2) |
| Unilateral | 40 | (33.3) |
| Bilateral | 13 | (10.8) |
| Acetabulum | 49 | (40.8) |
| Unilateral | 43 | (35.8) |
| Bilateral | 6 | (5.0) |
| Sacrum | 53 | (44.2) |
| Unilateral | 38 | (31.7) |
| Zone I | 11 | (9.2) |
| Zone II | 21 | (17.5) |
| Zone III | 6 | (5.0) |
| Bilateral | 15 | (12.5) |
| Zone I | 1 | (0.8) |
| Zone II | 4 | (3.3) |
| Zone III | 10 | (8.3) |
| Sacroiliac joint disruption, n (%) | 18 | (15.0) |
| Unilateral | 14 | (11.7) |
| Bilateral | 4 | (3.3) |
| Pubic symphysis diastasis, n (%) | 3 | (2.5) |
| Young−Burgees classification, n (%) | ||
| APC 3 | 6 | (5.0) |
| LC 1 | 51 | (42.5) |
| LC2 | 41 | (34.1) |
| LC 3 | 5 | (4.1) |
| vs. and CM | 17 | (14.2) |
| WSES classification | ||
| Grade I | 46 | (38.3) |
| Grade II | 38 | (31.7) |
| Grade III | 12 | (10.0) |
| Grade IV | 24 | (20.0) |
| Concomitant injury, n (%) | ||
| Head | 47 | (39.2) |
| Thorax | 65 | (54.2) |
| Abdomen | 30 | (25.0) |
| Extravasation on contrast-enhanced CT, n (%) | 34 | (28.3) |
| Angiography, n (%) | 38 | (31.7) |
| Transcatheter arterial embolization, n (%) | 34 | (28.3) |
| Pelvic gauze packing, n (%) | 8 | (6.7) |
| Length of hospital stay, days, median (IQR) | 22 | (5.75–39) |
| In-hospital mortality, n (%) | 13 | (10.8) |
| n = 120 | ||
|---|---|---|
| Minimum fibrinogen level within 24 h of arrival (mg/dL), mean (SD) | 171.4 | (88.9) |
| Initial fibrinogen level (mg/dL), mean (SD) | 211.7 | (73.0) |
| Initial fibrinogen degradation products level (mg/L), mean (SD) | 154.2 | (180.2) |
| Initial D-dimer level (μg/mL), mean (SD) | 42.8 | (48.0) |
| Initial prothrombin time activity (%), mean (SD) | 76.5 | (22.4) |
| Initial activated partial thromboplastin time (s), mean (SD) | 35.2 | (29.0) |
| Patients who underwent blood transfusion, n (%) | 59 | (49.2) |
| Red cell concentrate | 59 | (49.2) |
| Fresh frozen plasma | 47 | (39.2) |
| Platelet concentrate | 27 | (22.5) |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Estimate | SE | p Value | Estimate | SE | p Value | |
| Pelvic fracture site | ||||||
| Ilium | 9.3 | 16.0 | 0.563 | 7.6 | 16.1 | 0.638 |
| Pubis | −23.7 | 11.1 | 0.035 | 0.0 | 13.6 | 0.999 |
| Ischium | −20.3 | 11.8 | 0.088 | −13.9 | 13.3 | 0.299 |
| Acetabulum | −7.7 | 13.8 | 0.577 | −1.4 | 13.0 | 0.913 |
| Sacrum | −37.1 | 11.1 | 0.001 | −34.5 | 12.2 | 0.005 |
| Sacroiliac joint diastasis | −34.0 | 17.2 | 0.051 | −2.7 | 21.8 | 0.902 |
| Pubic symphysis diastasis | −37.7 | 52.1 | 0.470 | 6.3 | 58.7 | 0.915 |
| Concomitant injury | ||||||
| Head | −27.8 | 16.5 | 0.095 | −34.7 | 18.9 | 0.069 |
| Thorax | −45.6 | 15.8 | 0.005 | −20.1 | 16.8 | 0.234 |
| Abdomen | −27.9 | 18.6 | 0.137 | −19.0 | 18.9 | 0.316 |
| Age | 0.0 | 0.4 | 0.997 | 0.0 | 0.4 | 0.977 |
| Shock on arrival | −70.2 | 19.3 | <0.001 | −46.1 | 20.9 | 0.030 |
| Crude OR | 95% CI | p Value | Adjusted OR | 95% CI | p Value | |
|---|---|---|---|---|---|---|
| Ilium | 1.7 | 0.8–3.5 | 0.171 | 2.1 | 0.9–5.1 | 0.101 |
| Pubis | 2.1 | 1.2–3.5 | 0.008 | 1.4 | 0.7–2.8 | 0.317 |
| Ischium | 1.9 | 1.1–3.4 | 0.025 | 1.5 | 0.8–3.0 | 0.236 |
| Acetabulum | 1.0 | 0.5–1.8 | 0.990 | 1.0 | 0.5–2.0 | 0.987 |
| Sacrum | 2.0 | 1.2–3.4 | 0.015 | 1.9 | 1.1–3.6 | 0.031 |
| Sacroiliac joint dissection | 3.0 | 1.3–9.2 | 0.025 | 2.1 | 0.6–8.4 | 0.262 |
| Pubic symphysis dissection | 2.1 | 0.2–46.0 | 0.548 | 0.4 | 0.0–12.1 | 0.532 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunii, M.; Nakao, S.; Nakagawa, Y.; Shimazaki, J.; Ogura, H. Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study. J. Clin. Med. 2022, 11, 4689. https://doi.org/10.3390/jcm11164689
Kunii M, Nakao S, Nakagawa Y, Shimazaki J, Ogura H. Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study. Journal of Clinical Medicine. 2022; 11(16):4689. https://doi.org/10.3390/jcm11164689
Chicago/Turabian StyleKunii, Mayuko, Shunichiro Nakao, Yuko Nakagawa, Junya Shimazaki, and Hiroshi Ogura. 2022. "Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study" Journal of Clinical Medicine 11, no. 16: 4689. https://doi.org/10.3390/jcm11164689
APA StyleKunii, M., Nakao, S., Nakagawa, Y., Shimazaki, J., & Ogura, H. (2022). Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study. Journal of Clinical Medicine, 11(16), 4689. https://doi.org/10.3390/jcm11164689






