Evidence of Validity and Measurement Invariance by Gender of the Vaccination Attitudes Examination (VAX) Scale in Colombian University Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Participants
2.3. Variables and Instruments
2.4. Data Analysis
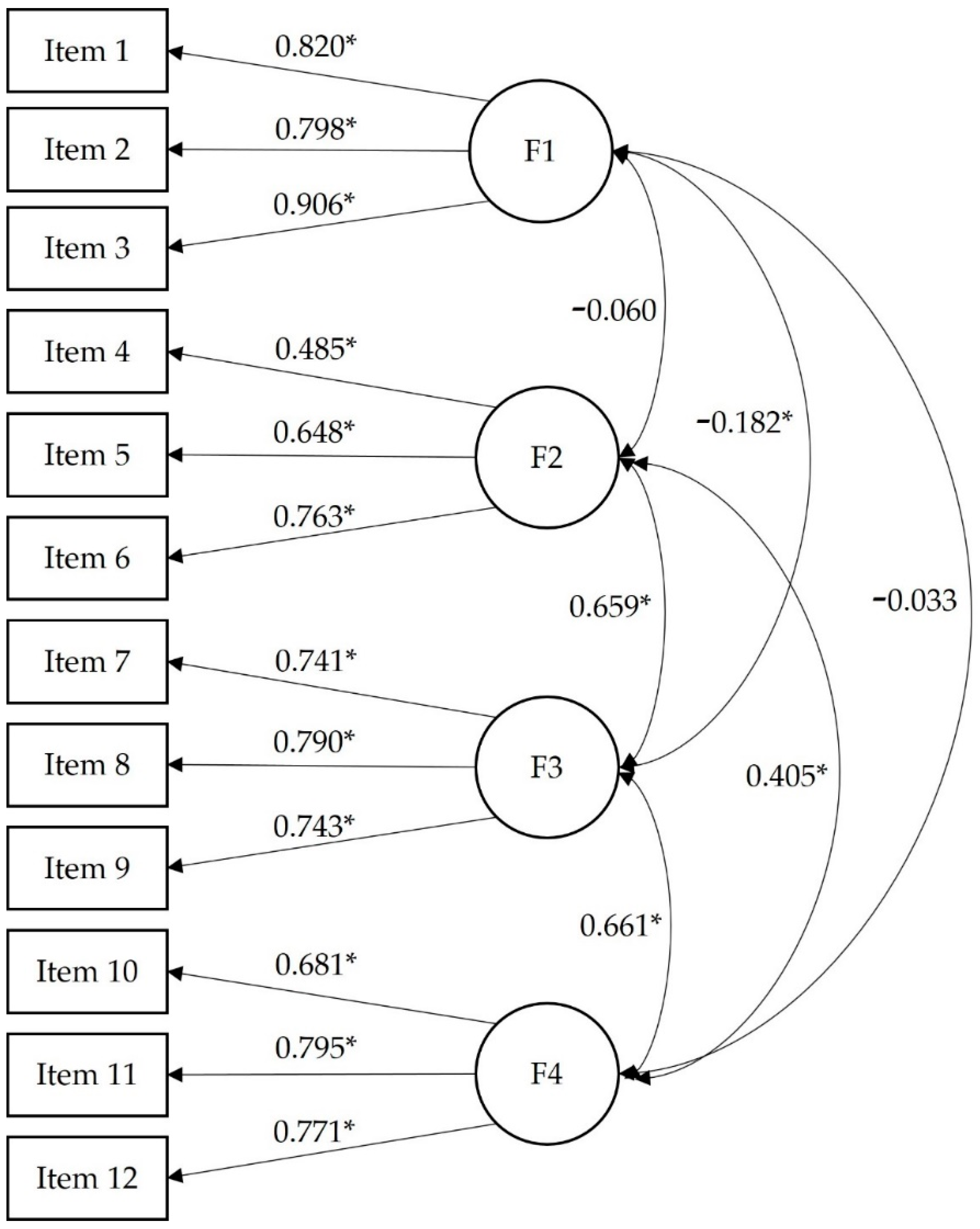
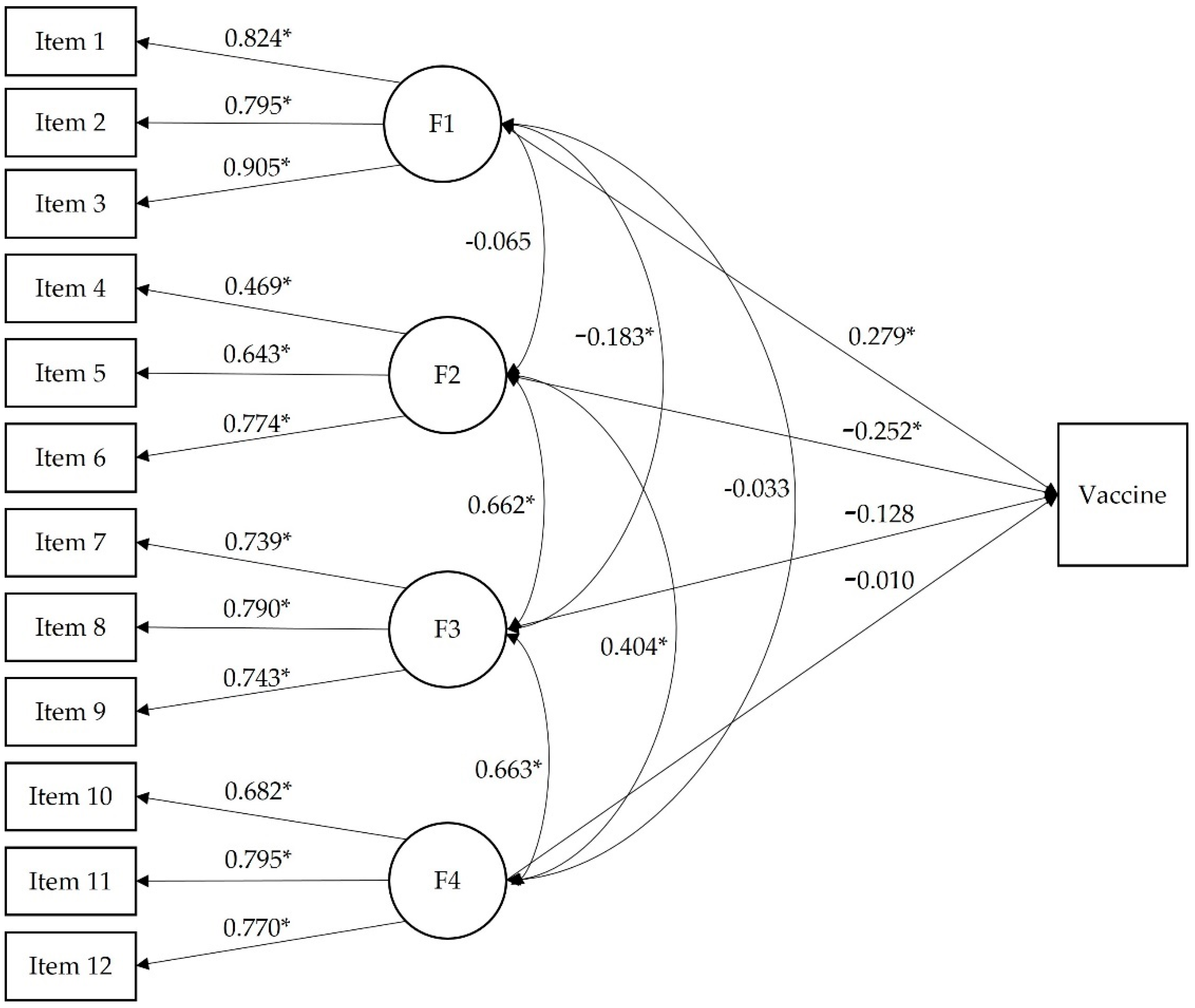
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Me siento seguro (a) después de ser vacunado
- Puedo confiar en las vacunas para detener enfermedades infecciosas graves
- Me siento protegido (a) después de vacunarme
- Aunque la mayoría de las vacunas parecen seguras, puede haber problemas que aún no hemos descubierto
- Las vacunas pueden causar problemas imprevistos en los niños
- Me preocupan los efectos desconocidos de las vacunas en el futuro
- Las vacunas generan mucho dinero para las compañías farmacéuticas, pero no hacen mucho para la gente común
- Las autoridades promueven la vacunación para obtener beneficios económicos, no por la salud de las personas
- Los programas de vacunación son una gran estafa
- La inmunidad natural tiene una duración más larga que una vacuna
- La exposición natural al virus y los gérmenes brinda protección más segura
- Estar expuesto (a) a enfermedades de manera natural es más seguro para el sistema inmunológico que estar expuesto (a) a través de la vacunación
References
- Guedes, G.R.; Coutinho, R.Z.; Marteleto, L.; Pereira, W.H.S.; Duarte, D. Why social perception matters during disease outbreaks: Looking at how individuals understand the zika virus by self-reported history of infection. Cad. Saude Publica 2018, 34, 9–10. [Google Scholar] [CrossRef] [PubMed]
- WHO Europe. Vaccination and Trust; World Health Organization: Copenhaguen, Denmark, 2017. [Google Scholar]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2022, 31, 62–86. [Google Scholar] [CrossRef] [PubMed]
- Küçükali, H.; Ataç, Ö.; Palteki, A.S.; Tokaç, A.Z.; Hayran, O. Vaccine Hesitancy and Anti-Vaccination Attitudes during the Start of COVID-19 Vaccination Program: A Content Analysis on Twitter Data. Vaccines 2022, 10, 161. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.R.; Petrie, K.J. Understanding the Dimensions of Anti-Vaccination Attitudes: The Vaccination Attitudes Examination (VAX) Scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Böhm, R.; Betsch, C. Prosocial vaccination. Curr. Opin. Psychol. 2022, 43, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cao, Y. Your pain, my gain: The relationship between self-report and behavioral measures of everyday sadism and COVID-19 vaccination intention. Curr. Psychol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Enea, V.; Eisenbeck, N.; Carreno, D.F.; Douglas, K.M.; Sutton, R.M.; Agostini, M.; Bélanger, J.J.; Gützkow, B.; Kreienkamp, J.; Abakoumkin, G.; et al. Intentions to be Vaccinated Against COVID-19: The Role of Prosociality and Conspiracy Beliefs across 20 Countries. Health Commun. 2022. [Google Scholar] [CrossRef] [PubMed]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Heal. Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef]
- Ruiz-Rodríguez, M.; Vera-Cala, L.M.; López-Barbosa, N. Seguro de salud y cobertura de vacunación en población infantil con y sin experiencia de desplazamiento forzado en Colombia [Health insurance for infants and infant vaccination related to forced-displacement in Colombia]. Rev. Salud Publica 2008, 10, 49–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodríguez-Orejuela, A.; Montes-Mora, C.L.; Osorio-Andrade, C.F. Sentimientos hacia la vacunación contra la COVID-19: Panorama colombiano en Twitter. Palabra Clave 2022, 25, e2514. [Google Scholar] [CrossRef]
- Alvis-Guzmán, N.; Alvis-Zakzuk, J.; Paz-Wilches, J.; Fernandez-Mercado, J.C.; de la Hoz-Restrepo, F. Disposición a recibir la vacuna contra COVID-19 en población de 80 y más años en Colombia 2021 [Willingness to receive the COVID-19 vaccine in the population aged 80 years and older in Colombia 2021]. Vacunas 2021, 22, 138–149. [Google Scholar] [CrossRef]
- Campo-Arias, A.; Caamano-Rocha, L.E.; Pedrozo-Pupo, J.C. Spanish Version of the Attitude Towards COVID-19 Vaccines Scale: Reliability and Validity Assessment. medRxiv 2021. [Google Scholar] [CrossRef]
- Rodríguez, M. Magnitud y causas de oportunidades perdidas en vacunación en población menor de dos años en América. CES Med. 2001, 1, 71–80. [Google Scholar]
- Simas, C.; Munoz, N.; Arregoces, L.; Larson, H.J. HPV vaccine confidence and cases of mass psychogenic illness following immunization in Carmen de Bolivar, Colombia. Hum. Vaccines Immunother. 2019, 15, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Castro, C. What happened in Colombia with the HPV Vaccination program- A story of light and shadows... Happiness and Tears. Cancer Ther. Oncol. Int. J. 2018, 9, 9–10. [Google Scholar] [CrossRef][Green Version]
- Piñeros, M.; Cortés, C.; Trujillo, L.; Wiesner, C. Conocimientos, aceptabilidad y actitudes sobre la vacuna contra el VPH en médicos generales, ginecólogos y pediatras en Colombia [Knowledge, Acceptability and Attitudes Towards the HPV Vaccine among Colombian General Practitioners, Gynecologists and Pedia. Rev. Colomb. Cancerol. 2009, 13, 88–98. [Google Scholar] [CrossRef]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hickler, B.; Guirguis, S.; Obregon, R. Vaccine Special Issue on Vaccine Hesitancy (Editorial). Vaccine 2015, 33, 4155–4156. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.D.; Coronado, G.D.; Williams, R.S.; Glenn, B.; Escoffery, C.; Fernandez, M.; Tuff, R.A.; Wilson, K.M.; Mullen, P.D. A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine 2010, 28, 4027–4037. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Kaufman, J.; Brewer, N.T.; Wiley, K.; Menning, L.; Leask, J.; Abad, N.; Betsch, C.; Bura, V.; Correa, G.; et al. A critical review of measures of childhood vaccine confidence. Curr. Opin. Immunol. 2021, 71, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Marbán-Castro, E.; Villén-Gonzalvo, A.; Enguita-Fernàndez, C.; Romero-Acosta, K.C.; Marín-Cos, A.; Arrieta, G.J.; Mattar, S.; Menéndez, C.; Maixenchs, M.; Bardají, A. Acceptability of a hypothetical zika vaccine among women from Colombia and Spain exposed to zikv: A qualitative study. Vaccines 2020, 8, 580. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Smith, M.; Miller, C.B.; O’Carroll, R.E. The Internal Consistency and Validity of the Vaccination Attitudes Examination Scale: A Replication Study. Ann. Behav. Med. 2019, 53, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Huza, G. The Psychometric Properties of a Romanian Version of the Vaccination Attitudes Examination (VAX) Scale. Int. J. HIV/AIDS Prev. Educ. Behav. Sci. 2020, 6, 25–31. [Google Scholar] [CrossRef]
- Yildiz, E.; Gungormus, Z.; Dayapoglu, N. Assessment of Validity and Reliability of the Turkish Version of the Vaccination Attitudes Examination (VAX) Scale. Int. J. Caring Sci. 2021, 14, 261–268. [Google Scholar]
- Paredes, B.; Cárdaba, M.Á.; Cuesta, U.; Martinez, L. Validity of the spanish version of the vaccination attitudes examination scale. Vaccines 2021, 9, 1237. [Google Scholar] [CrossRef] [PubMed]
- López-Gómez, M.; Cáceres, M.P.; Montoro, M.A. Estudio sobre Liderazgo Estudiantil desde un Enfoque Socio-político en la Universidad Santo Tomás de Bucaramanga (Colombia) [Study on Leadership Student at the University of Santo Tomas Bucaramanga (Colombia)]. Int. J. Educ. Leadersh. Manag. 2017, 5, 178–197. [Google Scholar] [CrossRef][Green Version]
- Winter, K.; Pummerer, L.; Hornsey, M.J.; Sassenberg, K. Pro-vaccination subjective norms moderate the relationship between conspiracy mentality and vaccination intentions. Br. J. Health Psychol. 2022, 27, 390–405. [Google Scholar] [CrossRef] [PubMed]
- Graupensperger, S.; Abdallah, D.A.; Lee, C.M. Social norms and vaccine uptake: College students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine 2021, 39, 2060–2067. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- LaCour, M.; Davis, T. Vaccine skepticism reflects basic cognitive differences in mortality-related event frequency estimation. Vaccine 2020, 38, 3790–3799. [Google Scholar] [CrossRef] [PubMed]
- de Angelis, T. How APA Is Helping COVID’s Overlooked Populations. Consider Joining One of the 10 Working Groups Tasked with Culling Resources to Aid Clinicians in Working with Underserved Groups during the Pandemic 2020. Available online: https://www.apaservices.org/practice/news/covid-19-overlooked-populations (accessed on 5 May 2022).
- Rivera, R. The Research Initiatives Working Group at the APA Interdivisional Task Force on the Pandemic. How to Advance Multidimensional COVID-19 Scholarship from a Global International Perspective. Int. Psychol. Bull. 2021, 25. Available online: https://div52.net/ipb-2021-25-3/#collaborations (accessed on 5 May 2022).
- Gallant, A.J.; Brown Nicholls, L.A.; Rasmussen, S.; Cogan, N.; Young, D.; Williams, L. Changes in attitudes to vaccination as a result of the COVID-19 pandemic: A longitudinal study of older adults in the UK. PLoS ONE 2021, 16, e0261844. [Google Scholar] [CrossRef] [PubMed]
- Muñiz, J.; Elosúa, P.; Padilla, J.L.; Hambleton, R.K. Test adaptation standards for cross-lingual assessment. In Educational Measurement. From Foundations to Future; Wells, C.S., Faulkner-Bond, M., Eds.; Guilford Press: New York, NY, USA, 2016; pp. 291–304. [Google Scholar]
- Raykov, T. Scale construction and development using structural equation modeling. In Handbook of Structural Equation Modeling; Hoyle, R.H., Ed.; The Guilford Press: New York, NY, USA, 2012; pp. 472–492. [Google Scholar]
- Rigdon, E.E.; Schumacker, R.E.; Wothke, W. A comparative review of interaction and nonlinear modeling. In Interaction and Nonlinear Effects in Structural Equation Modeling; Schumacker, R.E., Marcoulides, G.A., Eds.; Modern Methods for Business Research; Lawrence Erlbaum: Mahwah, NJ, USA, 2017; pp. 251–294. [Google Scholar]
- Raykov, T. Scale validity evaluation with congeneric measures in hierarchical designs. Br. J. Math. Stat. Psychol. 2011, 64, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Raykov, T.; Marcoulides, G.A. Introduction to Psychometric Theory; Routledge Ltd.: New York, NY, USA, 2011; ISBN 0415878225. [Google Scholar]
- Jöreskog, K.G. On the estimation of polychoric correlations and their asymptotic covariance matrix. Psychometrika 1994, 59, 381–389. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Bedford, H.; Attwell, K.; Danchin, M.; Marshall, H.; Corben, P.; Leask, J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine 2018, 36, 6556–6558. [Google Scholar] [CrossRef] [PubMed]
- Valentini, F.; Damásio, B.F. Average Variance Extracted and Composite Reliability: Reliability Coefficients. Psicol. Teor. E Pesqui. 2016, 32, 1–7. [Google Scholar] [CrossRef]
- Yeh, Y.C.; Chen, I.H.; Ahorsu, D.K.; Ko, N.Y.; Chen, K.L.; Li, P.C.; Yen, C.F.; Lin, C.Y.; Griffiths, M.D.; Pakpour, A.H. Measurement invariance of the drivers of COVID-19 vaccination acceptance scale: Comparison between taiwanese and mainland chinese-speaking populations. Vaccines 2021, 9, 297. [Google Scholar] [CrossRef]
- Fischer, R.; Karl, J.A. Predicting Behavioral Intentions to Prevent or Mitigate COVID-19: A Cross-Cultural Meta-Analysis of Attitudes, Norms, and Perceived Behavioral Control Effects. Soc. Psychol. Personal. Sci. 2022, 13, 264–276. [Google Scholar] [CrossRef]
| n | % | ||
|---|---|---|---|
| Gender | Male | 388 | 32.4 |
| Female | 791 | 66.8 | |
| Non-binary | 3 | 0.3 | |
| Prefer not to answer | 7 | 0.6 | |
| Student condition | Full-time student | 707 | 59.1 |
| Work and study | 490 | 40.9 | |
| Socioeconomic level | High | 9 | 0.8 |
| Medium-high | 93 | 7.8 | |
| Medium | 435 | 36.3 | |
| Medium-low | 412 | 34.4 | |
| Low | 248 | 20.7 | |
| Provincial department where the studies were carried out | Amazonas | 1 | 0.1 |
| Antioquia | 80 | 6.7 | |
| Arauca | 2 | 0.2 | |
| Atlántico | 61 | 5.1 | |
| Bolívar | 14 | 1.2 | |
| Boyacá | 3 | 0.3 | |
| Casanare | 1 | 0.1 | |
| Cauca | 12 | 1.0 | |
| César | 22 | 1.8 | |
| Córdoba | 34 | 2.8 | |
| Guainía | 1 | 0.1 | |
| La Guajira | 13 | 1.1 | |
| Magdalena | 572 | 47.8 | |
| Meta | 4 | 0.3 | |
| Norte de Santander | 18 | 1.5 | |
| Santander | 16 | 1.3 | |
| Sucre | 338 | 28.2 | |
| Tolima | 1 | 0.1 | |
| Valle del Cauca | 4 | 0.3 | |
| Degree being studied | Psychology | 339 | 28.3 |
| Social work | 82 | 6.9 | |
| Architecture | 149 | 12.4 | |
| Medicine | 22 | 1.8 | |
| Law | 79 | 6.6 | |
| Nursing | 52 | 4.3 | |
| Engineering | 88 | 7.4 | |
| Veterinary | 2 | 0.2 | |
| Other | 384 | 32.1 | |
| How the participants were conducting their studies | Online | 624 | 52.1 |
| Face-to-face | 219 | 18.3 | |
| Combined (online/face-to-face) | 354 | 29.6 | |
| Participants infected with coronavirus | Yes | 353 | 29.5 |
| No | 555 | 46.4 | |
| Not sure | 246 | 20.6 | |
| Missing values | 43 | 3.6 | |
| Participants vaccinated against the coronavirus | Yes | 874 | 73.0 |
| No | 323 | 27.0 |
| Mean | Standard Deviation | Skewness | Kurtosis | Corrected Item-Total Polyserial Correlations | SE for the Corrected Item-Total Polyserial Correlations | |
|---|---|---|---|---|---|---|
| Item 1 | 3.57 | 1.01 | −0.59 | 0.14 | 0.779 | 0.006 |
| Item 2 | 3.65 | 0.99 | −0.67 | 0.26 | 0.763 | 0.007 |
| Item 3 | 3.54 | 0.95 | −0.46 | 0.11 | 0.829 | 0.005 |
| Item 4 | 3.71 | 0.85 | −0.71 | 0.83 | 0.441 | 0.018 |
| Item 5 | 3.16 | 0.83 | −0.11 | 0.40 | 0.515 | 0.016 |
| Item 6 | 3.43 | 1.02 | −0.42 | −0.26 | 0.569 | 0.014 |
| Item 7 | 3.21 | 0.95 | −0.12 | −0.08 | 0.656 | 0.011 |
| Item 8 | 3.02 | 0.99 | 0.01 | −0.18 | 0.725 | 0.008 |
| Item 9 | 2.69 | 0.95 | 0.20 | 0.13 | 0.642 | 0.011 |
| Item 10 | 2.91 | 0.91 | 0.04 | 0.23 | 0.593 | 0.012 |
| Item 11 | 2.73 | 0.96 | 0.10 | −0.11 | 0.706 | 0.009 |
| Item 12 | 2.75 | 0.95 | 0.05 | −0.07 | 0.668 | 0.009 |
| χ2 | df | Δχ2 | Δdf | CFI | RMSEA | SRMR | ΔCFI | ΔRMSEA | ΔSRMR | |
|---|---|---|---|---|---|---|---|---|---|---|
| Men | 168.71 * | 48 | 0.909 | 0.081 | 0.070 | |||||
| Women | 154.26 * | 48 | 0.954 | 0.053 | 0.048 | |||||
| Configural | 322.98 * | 96 | - | - | 0.937 | 0.063 | 0.056 | - | - | - |
| Metric | 332.91 * | 104 | 10.6 | 8 | 0.936 | 0.061 | 0.060 | −0.001 | −0.002 | 0.004 |
| Scalar | 356.93 * | 112 | 20.0 | 8 | 0.932 | 0.061 | 0.062 | −0.004 | 0.000 | 0.002 |
| F1 | F2 | F3 | F4 | ||
|---|---|---|---|---|---|
| N | Valid | 1197 | 1197 | 1196 | 1197 |
| Missing | 0 | 0 | 1 | 0 | |
| Mean | 10.70 | 10.76 | 10.30 | 8.91 | |
| Median | 11 | 11 | 10 | 9 | |
| Mode | 12 | 12 | 9 | 9 | |
| Standard deviation | 2.70 | 2.64 | 2.10 | 2.44 | |
| Variance | 7.00 | 6.99 | 4.41 | 5.97 | |
| Minimum | 3 | 3 | 3 | 3 | |
| Maximum | 15 | 15 | 15 | 15 | |
| Percentiles | 5 | 6 | 7 | 5 | 4 |
| 10 | 7 | 8 | 6 | 6 | |
| 15 | 9 | 8 | 6 | 6 | |
| 20 | 9 | 9 | 7 | 6 | |
| 25 | 9 | 9 | 7 | 7 | |
| 30 | 9 | 9 | 8 | 7 | |
| 35 | 10 | 10 | 8 | 8 | |
| 40 | 10 | 10 | 9 | 8 | |
| 45 | 11 | 10 | 9 | 9 | |
| 50 | 11 | 10 | 9 | 9 | |
| 55 | 12 | 11 | 9 | 9 | |
| 60 | 12 | 11 | 9 | 9 | |
| 65 | 12 | 11 | 10 | 9 | |
| 70 | 12 | 11 | 10 | 9 | |
| 75 | 12 | 12 | 10 | 9 | |
| 80 | 12 | 12 | 11 | 10 | |
| 85 | 13 | 12 | 11 | 10 | |
| 90 | 15 | 13 | 12 | 11 | |
| 95 | 15 | 14 | 13 | 12 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espejo, B.; Martín-Carbonell, M.; Romero-Acosta, K.C.; Fernández-Daza, M.; Paternina, Y. Evidence of Validity and Measurement Invariance by Gender of the Vaccination Attitudes Examination (VAX) Scale in Colombian University Students. J. Clin. Med. 2022, 11, 4682. https://doi.org/10.3390/jcm11164682
Espejo B, Martín-Carbonell M, Romero-Acosta KC, Fernández-Daza M, Paternina Y. Evidence of Validity and Measurement Invariance by Gender of the Vaccination Attitudes Examination (VAX) Scale in Colombian University Students. Journal of Clinical Medicine. 2022; 11(16):4682. https://doi.org/10.3390/jcm11164682
Chicago/Turabian StyleEspejo, Begoña, Marta Martín-Carbonell, Kelly Carolina Romero-Acosta, Martha Fernández-Daza, and Yadid Paternina. 2022. "Evidence of Validity and Measurement Invariance by Gender of the Vaccination Attitudes Examination (VAX) Scale in Colombian University Students" Journal of Clinical Medicine 11, no. 16: 4682. https://doi.org/10.3390/jcm11164682
APA StyleEspejo, B., Martín-Carbonell, M., Romero-Acosta, K. C., Fernández-Daza, M., & Paternina, Y. (2022). Evidence of Validity and Measurement Invariance by Gender of the Vaccination Attitudes Examination (VAX) Scale in Colombian University Students. Journal of Clinical Medicine, 11(16), 4682. https://doi.org/10.3390/jcm11164682








