State-of-the-Art Multimodality Imaging in Sudden Cardiac Arrest with Focus on Idiopathic Ventricular Fibrillation: A Review
Abstract
1. Introduction
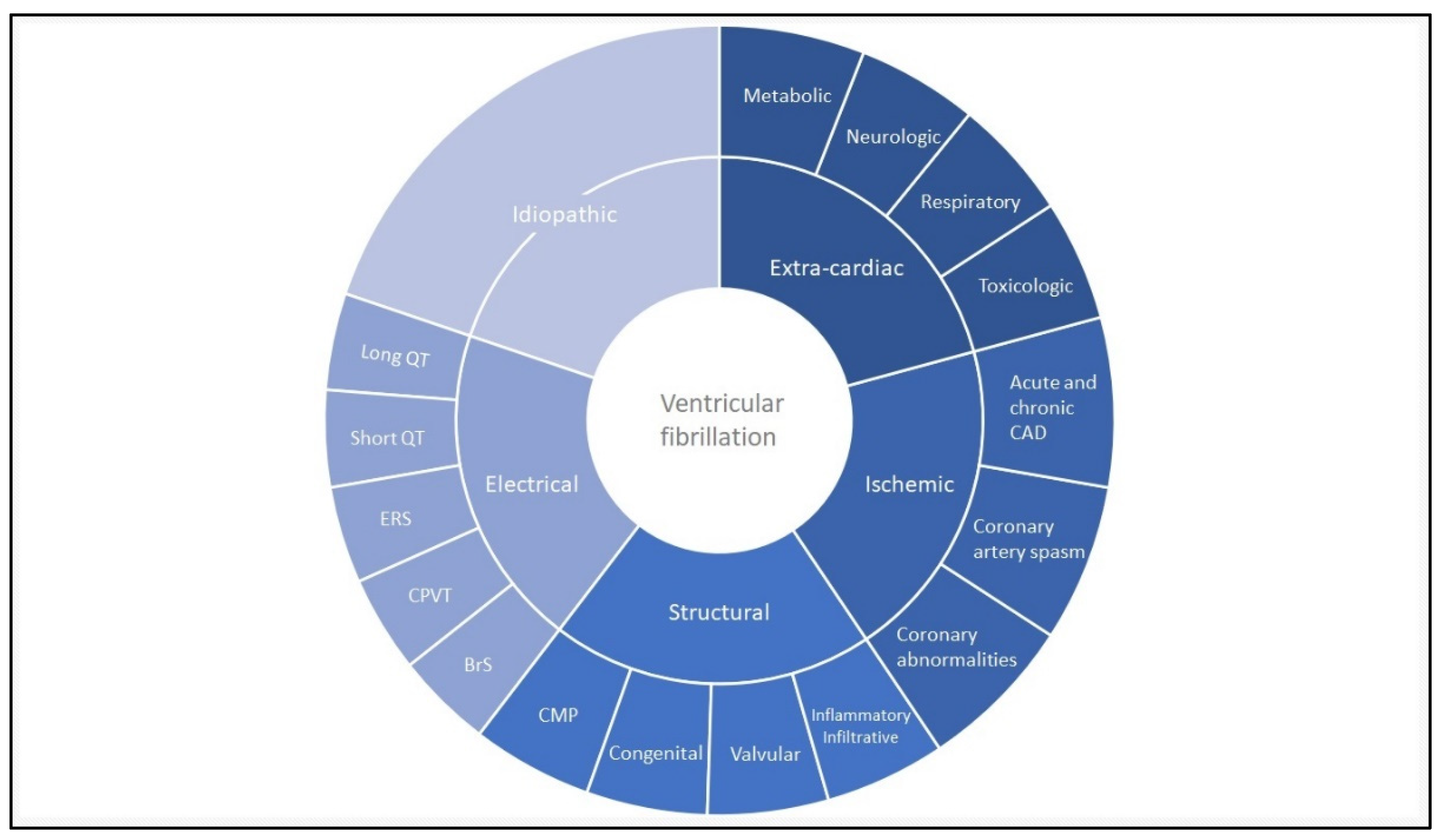
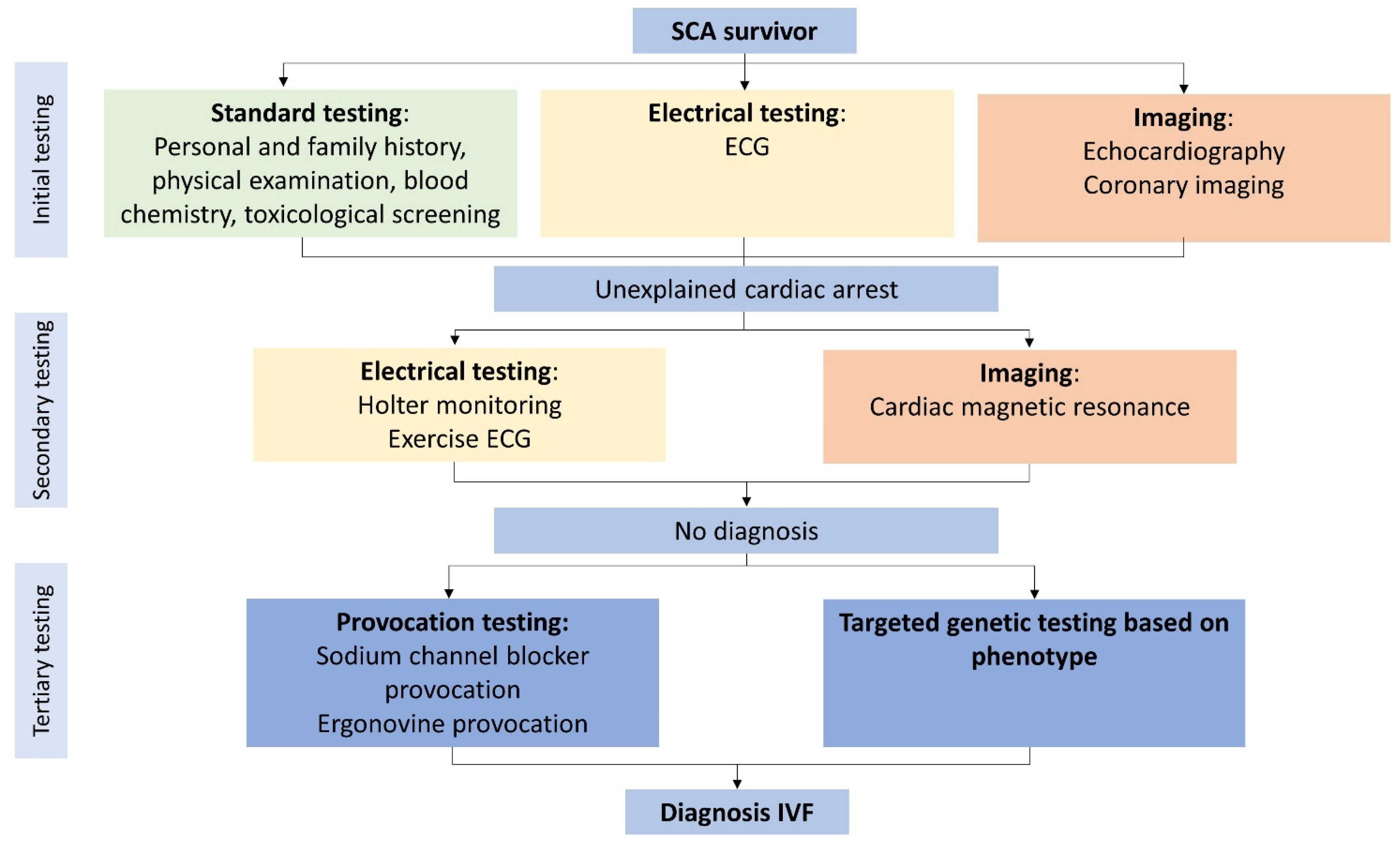
2. Defining Idiopathic Ventricular Fibrillation
2.1. Background
2.2. Clinical Evaluation
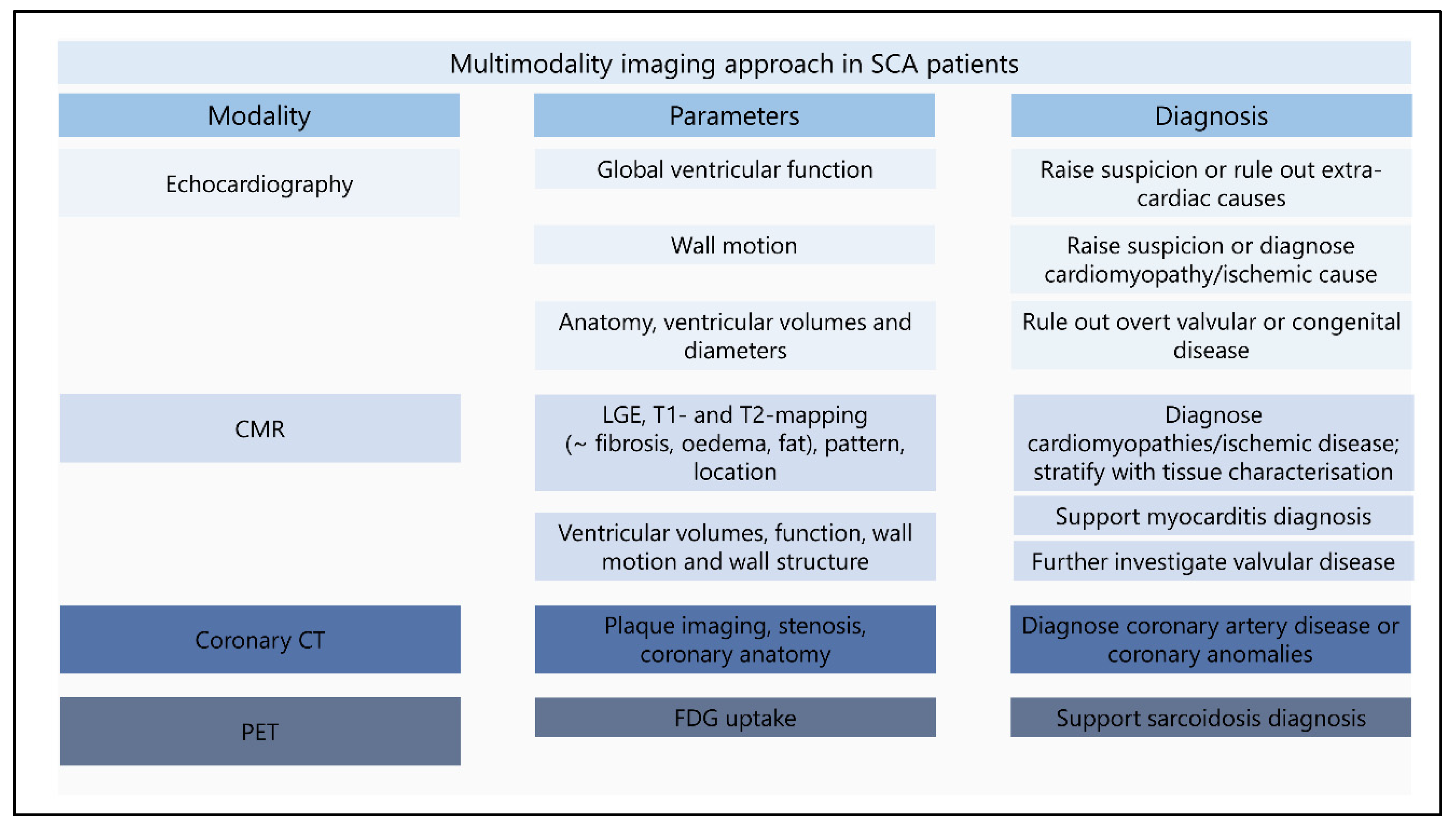
3. The Use of Multiple Imaging Modalities
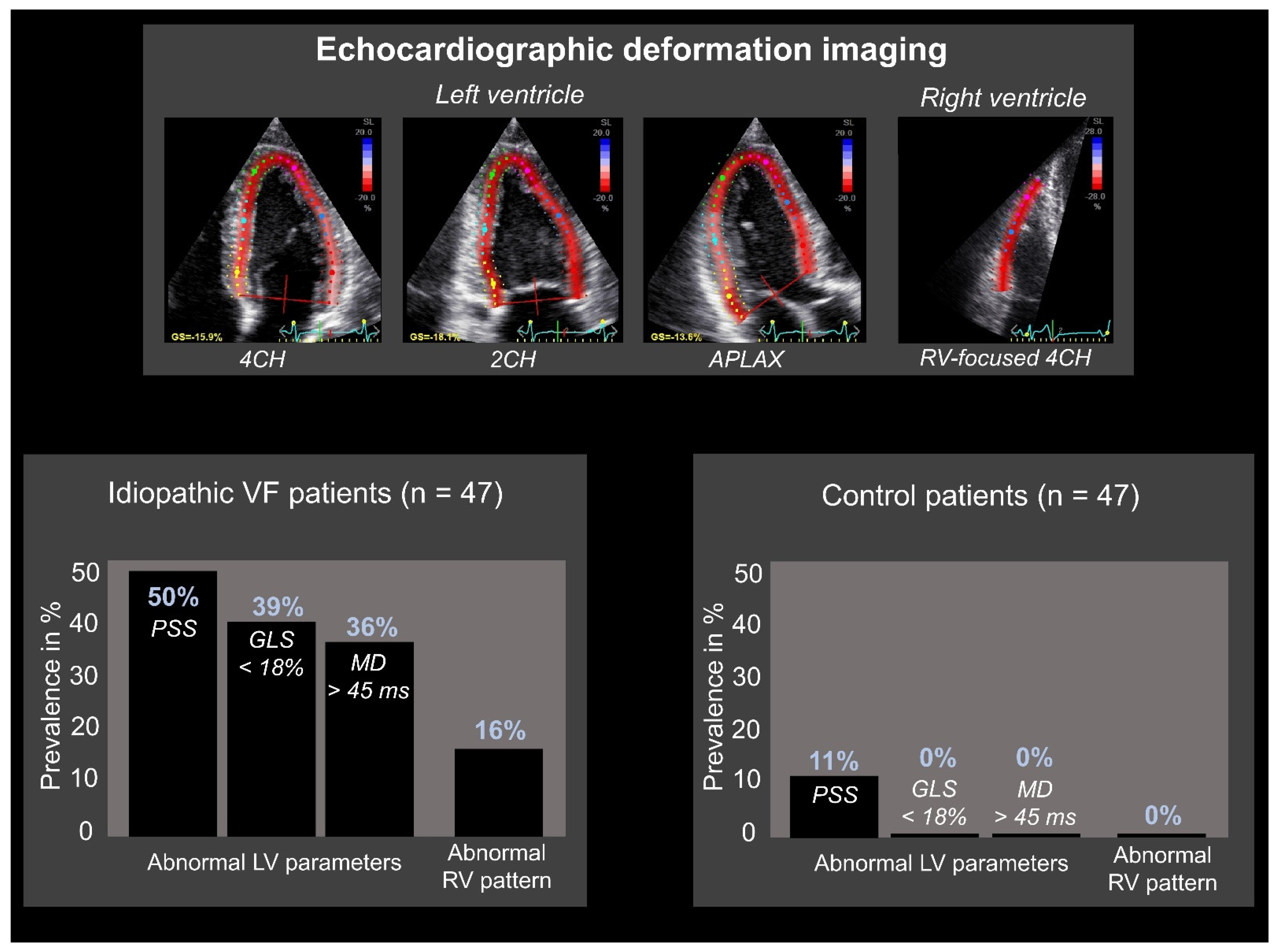
3.1. Echocardiography
Focus on Idiopathic Ventricular Fibrillation
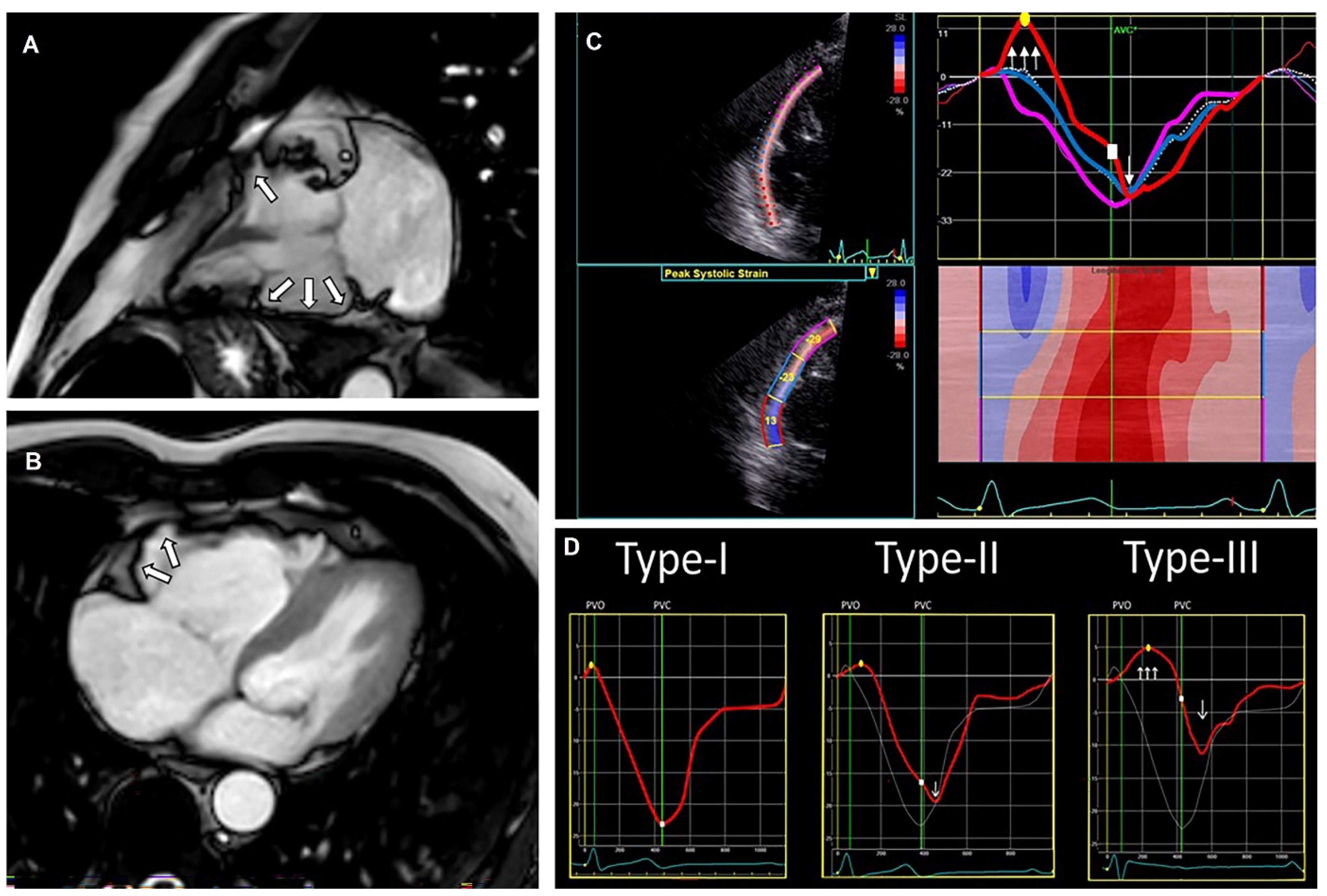
3.2. Cardiac Magnetic Resonance
Focus on Idiopathic Ventricular Fibrillation
3.3. Computed and Positron Emission Tomography
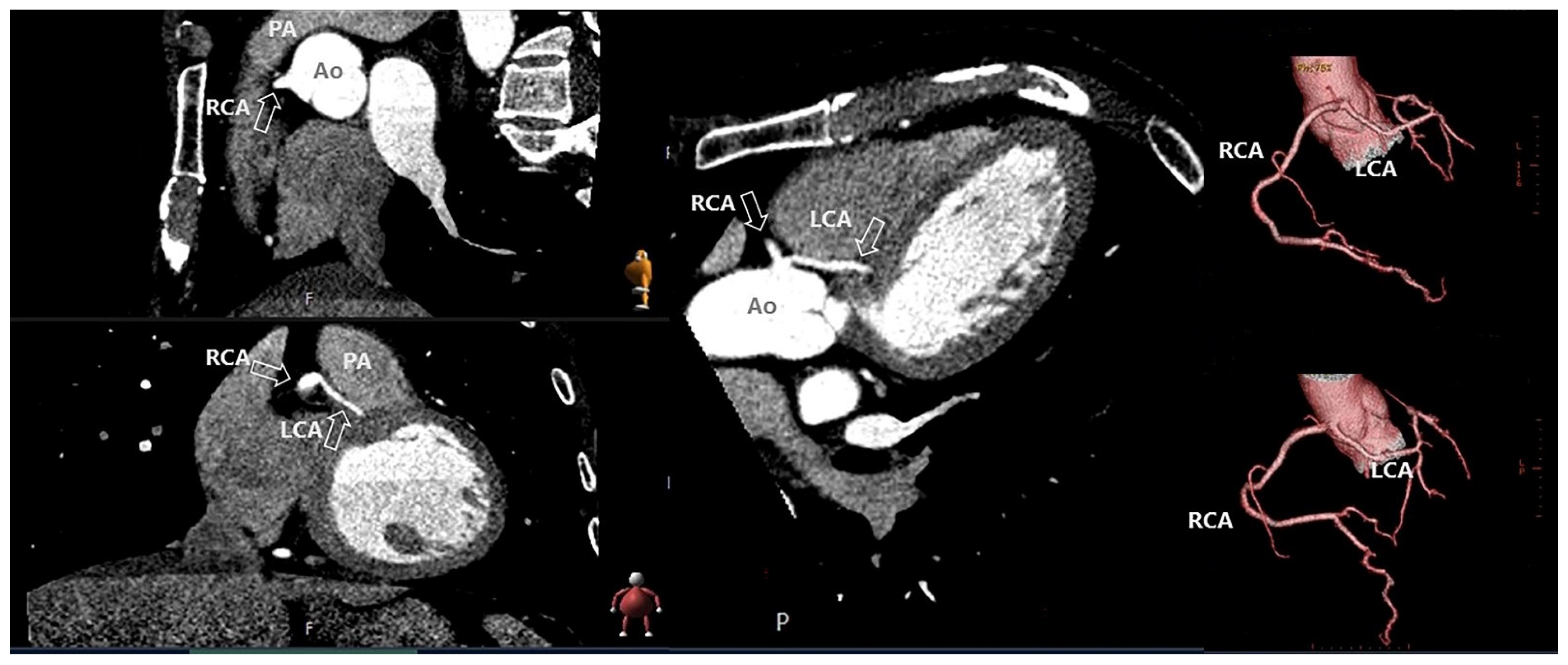
3.3.1. Cardiac Computed Tomography
3.3.2. Positron Emission Tomography
3.3.3. Focus on Idiopathic Ventricular Fibrillation
3.4. Reconstruction of Cardiac Electrical Activity
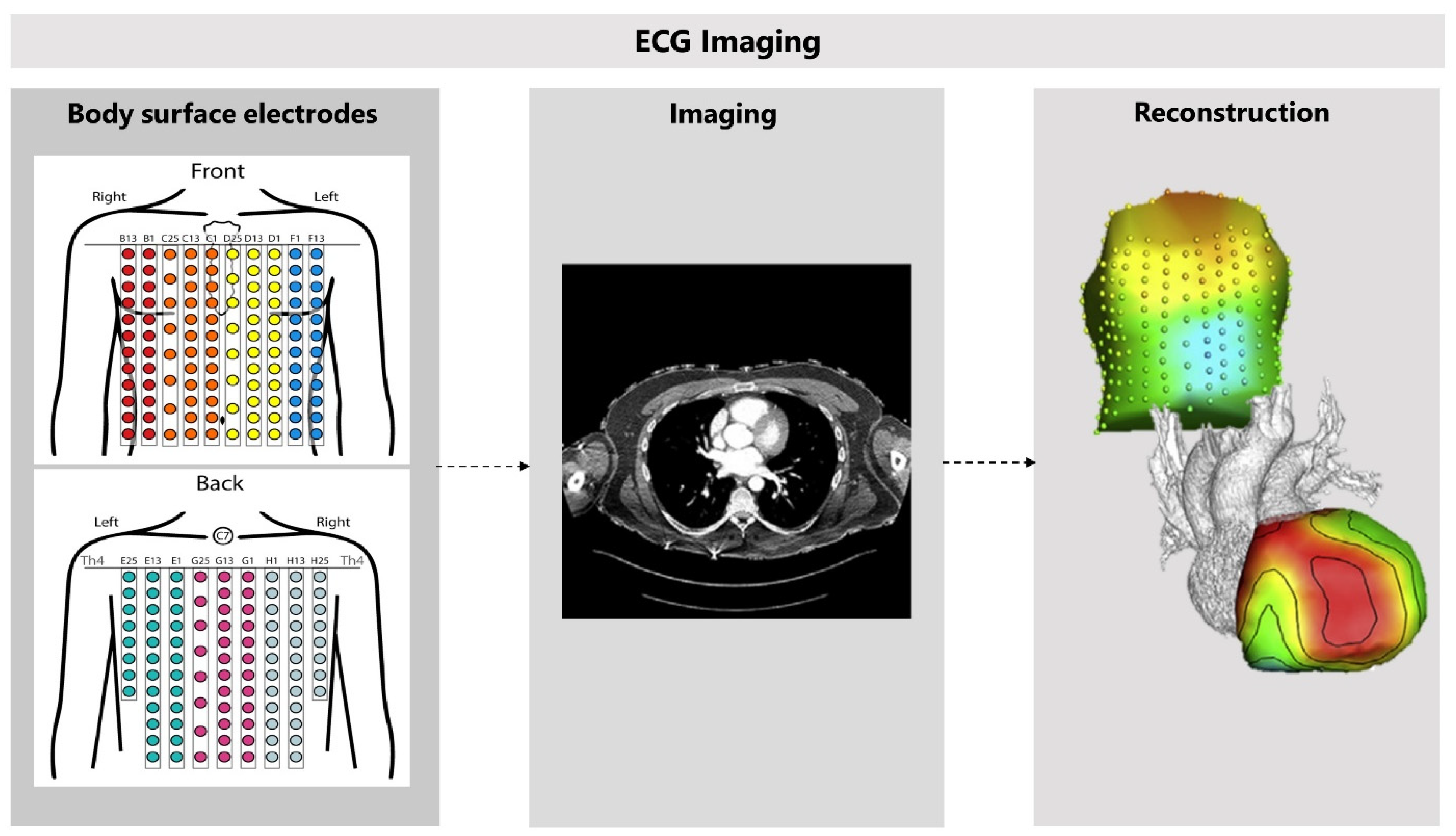
3.4.1. Non-Invasive Reconstruction: ECG-Imaging
3.4.2. Clinical Validation and Application
3.4.3. Finding Pro-Arrhythmic Factors in Idiopathic Ventricular Fibrillation Patients
4. Multimodality Imaging Approach and Future Perspectives
5. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Hayashi, M.; Shimizu, W.; Albert, C.M. The Spectrum of Epidemiology Underlying Sudden Cardiac Death. Circ. Res. 2015, 116, 1887–1906. [Google Scholar] [CrossRef] [PubMed]
- Zipes, D.P.; Camm, A.J.; Borggrefe, M.; Buxton, A.E.; Chaitman, B.; Fromer, M.; Gregoratos, G.; Klein, G.; Moss, A.J.; Myerburg, R.J.; et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Circulation 2006, 114, e385–e484. [Google Scholar] [CrossRef] [PubMed]
- Visser, M.; van der Heijden, J.F.; Doevendans, P.A.; Loh, P.; Wilde, A.A.; Hassink, R.J. Idiopathic Ventricular Fibrillation. Circ. Arrhythmia Electrophysiol. 2016, 9, e003817. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, V.; Bougouin, W.; Karam, N.; Dumas, F.; Sharifzadehgan, A.; Gandjbakhch, E.; Algalarrondo, V.; Narayanan, K.; Zhao, A.; Amet, D.; et al. Characteristics and Clinical Assessment of Unexplained Sudden Cardiac Arrest in the Real-World Setting: Focus on Idiopathic Ventricular Fibrillation. Eur. Heart J. 2018, 39, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Conte, G.; Belhassen, B.; Lambiase, P.; Ciconte, G.; De Asmundis, C.; Arbelo, E.; Schaer, B.; Frontera, A.; Burri, H.; Calo, L.; et al. Out-of-Hospital Cardiac Arrest Due to Idiopathic Ventricular Fibrillation in Patients with Normal Electrocardiograms: Results from a Multicentre Long-Term Registry. Europace 2019, 21, 1670–1677. [Google Scholar] [CrossRef]
- Dock, W. Transitory Ventricular Fibrillation as a Cause of Syncope and Its Prevention by Quinidine Sulphate. With Case Report and Discussion of Diagnostic Criteria for Ventricular Fibrillation. Am. Heart J. 1929, 4, 709–714. [Google Scholar] [CrossRef]
- Offerhaus, J.A.; Bezzina, C.R.; Wilde, A.A.M. Epidemiology of Inherited Arrhythmias. Nat. Rev. Cardiol. 2020, 17, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Viskin, S.; Belhassen, B. Idiopathic Ventricular Fibrillation. Am. Heart J. 1990, 120, 661–671. [Google Scholar] [CrossRef]
- McKenna, W.J.; Maron, B.J.; Thiene, G. Classification, Epidemiology, and Global Burden of Cardiomyopathies. Circ. Res. 2017, 121, 722–730. [Google Scholar] [CrossRef]
- Priori, S.G.; Wilde, A.A.; Horie, M.; Cho, Y.; Behr, E.R.; Berul, C.; Blom, N.; Brugada, J.; Chiang, C.E.; Huikuri, H.; et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013, 10, 1932–1963. [Google Scholar] [CrossRef]
- Survivors of Out-of-Hospital Cardiac Arrest with Apparently Normal Heart: Need for Definition and Standardized Clinical Evaluation. Circulation 1997, 95, 265–272. [CrossRef] [PubMed]
- Stiles, M.K.; Wilde, A.A.M.; Abrams, D.J.; Ackerman, M.J.; Albert, C.M.; Behr, E.R.; Chugh, S.S.; Cornel, M.C.; Gardner, K.; Ingles, J.; et al. 2020 APHRS/HRS Expert Consensus Statement on the Investigation of Decedents with Sudden Unexplained Death and Patients with Sudden Cardiac Arrest, and of Their Families. Heart Rhythm 2021, 18, e1–e50. [Google Scholar] [CrossRef] [PubMed]
- Deif, B.; Roberts, J.D. Diagnostic Evaluation and Arrhythmia Mechanisms in Survivors of Unexplained Cardiac Arrest. PACE—Pacing Clin. Electrophysiol. 2019, 42, 1320–1330. [Google Scholar] [CrossRef] [PubMed]
- Haïssaguerre, M.; Duchateau, J.; Dubois, R.; Hocini, M.; Cheniti, G.; Sacher, F.; Lavergne, T.; Probst, V.; Surget, E.; Vigmond, E.; et al. Idiopathic Ventricular Fibrillation: Role of Purkinje System and Microstructural Myocardial Abnormalities. JACC Clin. Electrophysiol. 2020, 6, 591–608. [Google Scholar] [CrossRef]
- Alqarawi, W.; Dewidar, O.; Tadros, R.; Roberts, J.D.; Steinberg, C.; MacIntyre, C.J.; Laksman, Z.W.M.; Green, M.S.; Nair, G.; Wells, G.; et al. Defining Idiopathic Ventricular Fibrillation: A Systematic Review of Diagnostic Testing Yield in Apparently Unexplained Cardiac Arrest. Heart Rhythm 2021, 18, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Conte, G.; Giudicessi, J.R.; Ackerman, M.J. Idiopathic Ventricular Fibrillation: The Ongoing Quest for Diagnostic Refinement. Europace 2021, 23, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Herman, A.R.M.; Cheung, C.; Gerull, B.; Simpson, C.S.; Birnie, D.H.; Klein, G.J.; Champagne, J.; Healey, J.S.; Gibbs, K.; Talajic, M.; et al. Outcome of Apparently Unexplained Cardiac Arrest: Results from Investigation and Follow-up of the Prospective Cardiac Arrest Survivors with Preserved Ejection Fraction Registry. Circ. Arrhythmia Electrophysiol. 2016, 9, e003619. [Google Scholar] [CrossRef] [PubMed]
- Merghani, A.; Monkhouse, C.; Kirkby, C.; Savvatis, K.; Mohiddin, S.A.; Elliott, P.; O’mahony, C.; Lowe, M.D.; Schilling, R.J.; Lambiase, P.D. Diagnostic Impact of Repeated Expert Review & Long-Term Follow-up in Determining Etiology of Idiopathic Cardiac Arrest. J. Am. Heart Assoc. 2021, 10, e019610. [Google Scholar] [CrossRef] [PubMed]
- White, J.A.; Fine, N.M.; Gula, L.; Yee, R.; Skanes, A.; Klein, G.; Leong-Sit, P.; Warren, H.; Thompson, T.; Drangova, M.; et al. Utility of Cardiovascular Magnetic Resonance in Identifying Substrate for Malignant Ventricular Arrhythmias. Circ. Cardiovasc. Imaging 2012, 5, 12–20. [Google Scholar] [CrossRef]
- Peres, N.; Hourdain, J.; Maille, B.; Arregle, F.; Zabern, M.; Dognin, N.; Koutbi, L.; Franceschi, F.; Deharo, J.C. Comprehensive Assessment of Unexplained Sudden Cardiac Death and Idiopathic Ventricular Fibrillation during the Index Hospitalization: A Systematic Thorough Investigation to Unmask Specific Etiology. Arch. Cardiovasc. Dis. Suppl. 2020, 12, 106–107. [Google Scholar] [CrossRef]
- Stampe, N.K.; Jespersen, C.B.; Glinge, C.; Bundgaard, H.; Tfelt-Hansen, J.; Winkel, B.G. Clinical Characteristics and Risk Factors of Arrhythmia during Follow-up of Patients with Idiopathic Ventricular Fibrillation. J. Cardiovasc. Electrophysiol. 2020, 31, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Stȩpień-Wojno, M.; Ponińska, J.; Rydzanicz, M.; Bilińska, M.; Truszkowska, G.; Baranowski, R.; Lutyńska, A.; Biernacka, E.K.; Stȩpińska, J.; Kowalik, I.; et al. Sudden Cardiac Arrest in Patients without Overt Heart Disease: A Limited Value of next Generation Sequencing. Polish Arch. Intern. Med. 2018, 128, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Blom, L.J.; Visser, M.; Christiaans, I.; Scholten, M.F.; Bootsma, M.; Van Den Berg, M.P.; Yap, S.C.; Van Der Heijden, J.F.; Doevendans, P.A.; Loh, P.; et al. Incidence and Predictors of Implantable Cardioverter-Defibrillator Therapy and Its Complications in Idiopathic Ventricular Fibrillation Patients. Europace 2019, 21, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Conte, G.; Luce Caputo, M.; Regoli, F.; Marcon, S.; Klersy, C.; Adjibodou, B.; Del Bufalo, A.; Moccetti, T.; Auricchio, A. True Idiopathic Ventricular Fibrillation in Out-of-Hospital Cardiac Arrest Survivors in the Swiss Canton Ticino: Prevalence, Clinical Features, and Long-Term Follow-Up. Europace 2017, 19, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, U.; Platonov, P.G.; Rubulis, A.; Bergfeldt, L.; Jensen, S.M.; Lundin, C.; Borgquist, R. Idiopathic Ventricular Fibrillation—Long Term Prognosis in Relation to Clinical Findings and ECG Patterns in a Swedish Cohort. J. Electrocardiol. 2019, 56, 46–51. [Google Scholar] [CrossRef]
- Cunningham, T.; Roston, T.M.; Franciosi, S.; Liu, M.C.; Atallah, J.; Escudero, C.A.; Udupa, S.; Roberts, J.D.; Dhillon, S.; Dallaire, F.; et al. Initially Unexplained Cardiac Arrest in Children and Adolescents: A National Experience from the Canadian Pediatric Heart Rhythm Network. Heart Rhythm 2020, 17, 975–981. [Google Scholar] [CrossRef]
- Frontera, A.; Vlachos, K.; Kitamura, T.; Mahida, S.; Pillois, X.; Fahy, G.; Marquie, C.; Cappato, R.; Stuart, G.; Defaye, P.; et al. Long-Term Follow-Up of Idiopathic Ventricular Fibrillation in a Pediatric Population: Clinical Characteristics, Management, and Complications. J. Am. Heart Assoc. 2019, 8, e011172. [Google Scholar] [CrossRef]
- Jiménez-Jáimez, J.; Peinado, R.; Grima, E.Z.; Segura, F.; Moriña, P.; Sánchez Muñoz, J.J.; Mazuelos, F.; Cózar, R.; Gimeno, J.R.; Heras, R.P.; et al. Diagnostic Approach to Unexplained Cardiac Arrest (from the FIVI-Gen Study). Am. J. Cardiol. 2015, 116, 894–899. [Google Scholar] [CrossRef]
- Price, S.; Uddin, S.; Quinn, T. Echocardiography in Cardiac Arrest. Curr. Opin. Crit. Care 2010, 16, 211–215. [Google Scholar] [CrossRef]
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Bloma, N.; Borggrefe, M.; Camm, J.; Elliott, P.M.; Fitzsimons, D.; Hatala, R.; Hindricks, G.; et al. 2015 ESC Guidelines for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the Europe. Europace 2015, 17, 1601–1687. [Google Scholar] [CrossRef]
- Edvardsen, T.; Asch, F.M.; Davidson, B.; Delgado, V.; DeMaria, A.; Dilsizian, V.; Gaemperli, O.; Garcia, M.J.; Kamp, O.; Lee, D.C.; et al. Non-Invasive Imaging in Coronary Syndromes: Recommendations of the European Association of Cardiovascular Imaging and the American Society of Echocardiography, in Collaboration with the American Society of Nuclear Cardiology, Society of Cardiovascular Com. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e6–e33. [Google Scholar] [CrossRef]
- Lee, S.E.; Uhm, J.S.; Kim, J.Y.; Pak, H.N.; Lee, M.H.; Joung, B. Combined ECG, Echocardiographic, and Biomarker Criteria for Diagnosing Acute Myocardial Infarction in out-of-Hospital Cardiac Arrest Patients. Yonsei Med. J. 2015, 56, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Wand, A.L.; Chrispin, J.; Saad, E.; Mukherjee, M.; Hays, A.G.; Gilotra, N.A. Current State and Future Directions of Multimodality Imaging in Cardiac Sarcoidosis. Front. Cardiovasc. Med. 2022, 8, 785279. [Google Scholar] [CrossRef] [PubMed]
- Birnie, D.H.; Sauer, W.H.; Bogun, F.; Cooper, J.M.; Culver, D.A.; Duvernoy, C.S.; Judson, M.A.; Kron, J.; Mehta, D.; Cosedis Nielsen, J.; et al. HRS Expert Consensus Statement on the Diagnosis and Management of Arrhythmias Associated with Cardiac Sarcoidosis. Heart Rhythm 2014, 11, 1304–1323. [Google Scholar] [CrossRef]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current State of Knowledge on Aetiology, Diagnosis, Management, and Therapy of Myocarditis: A Position Statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef] [PubMed]
- Petek, B.J.; Erley, C.L.; Kudenchuk, P.J.; Carlbom, D.; Strote, J.; Gatewood, M.O.; Shuman, W.P.; Hira, R.S.; Gunn, M.L.; Maynard, C.; et al. Diagnostic Yield of Non-Invasive Imaging in Patients Following Non-Traumatic out-of-Hospital Sudden Cardiac Arrest: A Systematic Review. Resuscitation 2019, 135, 183–190. [Google Scholar] [CrossRef]
- Donal, E.; Delgado, V.; Bucciarelli-Ducci, C.; Galli, E.; Haugaa, K.H.; Charron, P.; Voigt, J.U.; Cardim, N.; Masci, P.G.; Galderisi, M.; et al. Multimodality Imaging in the Diagnosis, Risk Stratification, and Management of Patients with Dilated Cardiomyopathies: An Expert Consensus Document from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1075–1093. [Google Scholar] [CrossRef]
- Cardim, N.; Galderisi, M.; Edvardsen, T.; Plein, S.; Popescu, B.A.; D’Andrea, A.; Bruder, O.; Cosyns, B.; Davin, L.; Donal, E.; et al. Role of Multimodality Cardiac Imaging in the Management of Patients with Hypertrophic Cardiomyopathy: An Expert Consensus of the European Association of Cardiovascular Imaging Endorsed by the Saudi Heart Association. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 280. [Google Scholar] [CrossRef]
- Haugaa, K.H.; Basso, C.; Badano, L.P.; Bucciarelli-Ducci, C.; Cardim, N.; Gaemperli, O.; Galderisi, M.; Habib, G.; Knuuti, J.; Lancellotti, P.; et al. Comprehensive Multi-Modality Imaging Approach in Arrhythmogenic Cardiomyopathy—An Expert Consensus Document of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 237–253. [Google Scholar] [CrossRef]
- Kern, K.B.; Hilwig, R.W.; Rhee, K.H.; Berg, R.A. Myocardial Dysfunction after Resuscitation from Cardiac Arrest: An Example of Global Myocardial Stunning. J. Am. Coll. Cardiol. 1996, 28, 232–240. [Google Scholar] [CrossRef]
- Cha, K.C.; Kim, H., II; Kim, O.H.; Cha, Y.S.; Kim, H.; Lee, K.H.; Hwang, S.O. Echocardiographic Patterns of Postresuscitation Myocardial Dysfunction. Resuscitation 2018, 124, 90–95. [Google Scholar] [CrossRef]
- Isbister, J.C.; Nowak, N.; Butters, A.; Yeates, L.; Gray, B.; Sy, R.W.; Ingles, J.; Bagnall, R.D.; Semsarian, C. “Concealed Cardiomyopathy” as a Cause of Previously Unexplained Sudden Cardiac Arrest. Int. J. Cardiol. 2021, 324, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Blom, L.J.; Te Riele, A.S.J.M.; Vink, A.; Hauer, R.N.W.; Hassink, R.J. Late Evolution of Arrhythmogenic Cardiomyopathy in Patients with Initial Presentation as Idiopathic Ventricular Fibrillation. Heart Case Rep. 2019, 5, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Taha, K.; Kirkels, F.P.; Teske, A.J.; Asselbergs, F.W.; van Tintelen, J.P.; Doevendans, P.A.; Kutty, S.; Haugaa, K.H.; Cramer, M.J. Echocardiographic Deformation Imaging for Early Detection of Genetic Cardiomyopathies: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 594–608. [Google Scholar] [CrossRef]
- Groeneveld, S.A.; van der Ree, M.H.; Taha, K.; de Bruin-Bon, R.H.A.; Cramer, M.J.; Teske, A.J.; Bouma, B.J.; Amin, A.S.; Wilde, A.A.M.; Postema, P.G.; et al. Echocardiographic Deformation Imaging Unmasks Global and Regional Mechanical Dysfunction in Patients with Idiopathic Ventricular Fibrillation: A Multicenter Case-Control Study. Heart Rhythm 2021, 18, 1666–1672. [Google Scholar] [CrossRef]
- Voigt, J.U.; Pedrizzetti, G.; Lysyansky, P.; Marwick, T.H.; Houle, H.; Baumann, R.; Pedri, S.; Ito, Y.; Abe, Y.; Metz, S.; et al. Definitions for a Common Standard for 2D Speckle Tracking Echocardiography: Consensus Document of the EACVI/ASE/Industry Task Force to Standardize Deformation Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Mast, T.P.; Teske, A.J.; Walmsley, J.; van der Heijden, J.F.; van Es, R.; Prinzen, F.W.; Delhaas, T.; van Veen, T.A.; Loh, P.; Doevendans, P.A.; et al. Right Ventricular Imaging and Computer Simulation for Electromechanical Substrate Characterization in Arrhythmogenic Right Ventricular Cardiomyopathy. J. Am. Coll. Cardiol. 2016, 68, 2185–2197. [Google Scholar] [CrossRef] [PubMed]
- Zareba, W.; Zareba, K.M. Cardiac Magnetic Resonance in Sudden Cardiac Arrest Survivors. Circ. Cardiovasc. Imaging 2017, 10, e007290. [Google Scholar] [CrossRef][Green Version]
- Patel, A.R.; Kramer, C.M. Role of Cardiac Magnetic Resonance in the Diagnosis and Prognosis of Nonischemic Cardiomyopathy. JACC Cardiovasc. Imaging 2017, 10, 1180–1193. [Google Scholar] [CrossRef]
- Neilan, T.G.; Farhad, H.; Mayrhofer, T.; Shah, R.V.; Dodson, J.A.; Abbasi, S.A.; Danik, S.B.; Verdini, D.J.; Tokuda, M.; Tedrow, U.B.; et al. Late Gadolinium Enhancement among Survivors of Sudden Cardiac Arrest. JACC Cardiovasc. Imaging 2015, 8, 414–423. [Google Scholar] [CrossRef]
- Zorzi, A.; Mattesi, G.; Baldi, E.; Toniolo, M.; Guerra, F.; Cauti, F.M.; Cipriani, A.; De Lazzari, M.; Muser, D.; Stronati, G.; et al. Prognostic Role of Myocardial Edema as Evidenced by Early Cardiac Magnetic Resonance in Survivors of Out-of-Hospital Cardiac Arrest: A Multicenter Study. J. Am. Heart Assoc. 2021, 10, e021861. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, P.; Joshi, A.; Williams, H.; Westwood, M.; Petersen, S.E.; Zemrak, F.; Schilling, R.J.; Kirkby, C.; Wragg, A.; Manisty, C.; et al. Diagnosis and Prognosis in Sudden Cardiac Arrest Survivors Without Coronary Artery Disease: Utility of a Clinical Approach Using Cardiac Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2017, 10, e006709. [Google Scholar] [CrossRef] [PubMed]
- Zorzi, A.; Susana, A.; De Lazzari, M.; Migliore, F.; Vescovo, G.; Scarpa, D.; Baritussio, A.; Tarantini, G.; Cacciavillani, L.; Giorgi, B.; et al. Diagnostic Value and Prognostic Implications of Early Cardiac Magnetic Resonance in Survivors of Out-of-Hospital Cardiac Arrest. Heart Rhythm 2018, 15, 1031–1041. [Google Scholar] [CrossRef]
- Baritussio, A.; Zorzi, A.; Ghosh Dastidar, A.; Susana, A.; Mattesi, G.; Rodrigues, J.C.L.; Biglino, G.; Scatteia, A.; De Garate, E.; Strange, J.; et al. Out of Hospital Cardiac Arrest Survivors with Inconclusive Coronary Angiogram: Impact of Cardiovascular Magnetic Resonance on Clinical Management and Decision-Making. Resuscitation 2017, 116, 91–97. [Google Scholar] [CrossRef][Green Version]
- Kim, S.M.; Youn, C.S.; Lee, G.T.; Shin, T.G.; Kim, J.S.; Kim, Y.J.; Kim, W.Y. Cardiac Magnetic Resonance Imaging for Nonischemic Cardiac Disease in Out-of-Hospital Cardiac Arrest Survivors Treated with Targeted Temperature Management: A Multicenter Retrospective Analysis. J. Clin. Med. 2021, 10, 794. [Google Scholar] [CrossRef] [PubMed]
- Zaremba, T.; Brøndberg, A.K.; Jensen, H.K.; Kim, W.Y. Cardiac Magnetic Resonance Characteristics in Young Survivors of Aborted Sudden Cardiac Death. Eur. J. Radiol. 2018, 105, 141–147. [Google Scholar] [CrossRef]
- Marstrand, P.; Axelsson, A.; Thune, J.J.; Vejlstrup, N.; Bundgaard, H.; Theilade, J. Cardiac Magnetic Resonance Imaging After Ventricular Tachyarrhythmias Increases Diagnostic Precision and Reduces the Need for Family Screening for Inherited Cardiac Disease. Europace 2016, 18, 1860–1865. [Google Scholar] [CrossRef]
- Andreini, D.; Dello Russo, A.; Pontone, G.; Mushtaq, S.; Conte, E.; Perchinunno, M.; Guglielmo, M.; Coutinho Santos, A.; Magatelli, M.; Baggiano, A.; et al. CMR for Identifying the Substrate of Ventricular Arrhythmia in Patients with Normal Echocardiography. JACC Cardiovasc. Imaging 2020, 13, 410–421. [Google Scholar] [CrossRef]
- Hennig, A.; Salel, M.; Sacher, F.; Camaioni, C.; Sridi, S.; Denis, A.; Montaudon, M.; Laurent, F.; Jais, P.; Cochet, H. High-Resolution Three-Dimensional Late Gadolinium-Enhanced Cardiac Magnetic Resonance Imaging to Identify the Underlying Substrate of Ventricular Arrhythmia. Europace 2018, 20, f179–f191. [Google Scholar] [CrossRef]
- Marques, J.S.; Pinto, F.J. Clinical Use of Multimodality Imaging in the Assessment of Dilated Cardiomyopathy. Heart 2015, 101, 565–572. [Google Scholar] [CrossRef]
- Cummings, K.W.; Bhalla, S.; Javidan-Nejad, C.; Bierhals, A.J.; Gutierrez, F.R.; Woodard, P.K. A Pattern-Based Approach to Assessment of Delayed Enhancement in Nonischemic Cardiomyopathy at MR Imaging. Radiographics 2009, 29, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Basso, C.; Perazzolo Marra, M.; Rizzo, S.; De Lazzari, M.; Giorgi, B.; Cipriani, A.; Frigo, A.C.; Rigato, I.; Migliore, F.; Pilichou, K.; et al. Arrhythmic Mitral Valve Prolapse and Sudden Cardiac Death. Circulation 2015, 132, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Guglielmo, M.; Fusini, L.; Muscogiuri, G.; Baessato, F.; Loffreno, A.; Cavaliere, A.; Rizzon, G.; Baggiano, A.; Rabbat, M.G.; Muratori, M.; et al. T1 Mapping and Cardiac Magnetic Resonance Feature Tracking in Mitral Valve Prolapse. Eur. Radiol. 2021, 31, 1100–1109. [Google Scholar] [CrossRef] [PubMed]
- Pavon, A.G.; Arangalage, D.; Pascale, P.; Hugelshofer, S.; Rutz, T.; Porretta, A.P.; Le Bloa, M.; Muller, O.; Pruvot, E.; Schwitter, J.; et al. Myocardial Extracellular Volume by T1 Mapping: A New Marker of Arrhythmia in Mitral Valve Prolapse. J. Cardiovasc. Magn. Reson. 2021, 23, 102. [Google Scholar] [CrossRef]
- Kukavica, D.; Guglielmo, M.; Baggiano, A.; Muscogiuri, G.; Fusini, L.; Muratori, M.; Tamborini, G.; Mantegazza, V.; Trancuccio, A.; Arnò, C.; et al. Arrhythmic Mitral Valve Prolapse: Introducing an Era of Multimodality Imaging-Based Diagnosis and Risk Stratification. Diagnostics 2021, 11, 467. [Google Scholar] [CrossRef]
- Moura-Ferreira, S.; Vandenberk, B.; Masci, P.G.; Dresselaers, T.; Garweg, C.; Symons, R.; Willems, R.; Bogaert, J. Left Ventricular Remodelling in Mitral Valve Prolapse Patients: Implications of Apical Papillary Muscle Insertion. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 1119–1128. [Google Scholar] [CrossRef]
- Groeneveld, S.A.; Kirkels, F.P.; Cramer, M.J.; Evertz, R.; Haugaa, K.H.; Postema, P.G.; Prakken, N.H.J.; Teske, A.J.; Wilde, A.A.M.; Velthuis, B.K.; et al. Prevalence of Mitral Annulus Disjunction and Mitral Valve Prolapse in Idiopathic Ventricular Fibrillation Patients. J. Am. Heart Assoc. 2022, 11, e025364. [Google Scholar] [CrossRef]
- Sriram, C.S.; Syed, F.F.; Ferguson, M.E.; Johnson, J.N.; Enriquez-Sarano, M.; Cetta, F.; Cannon, B.C.; Asirvatham, S.J.; Ackerman, M.J. Malignant Bileaflet Mitral Valve Prolapse Syndrome in Patients with Otherwise Idiopathic Out-of-Hospital Cardiac Arrest. J. Am. Coll. Cardiol. 2013, 62, 222–230. [Google Scholar] [CrossRef]
- Dejgaard, L.A.; Skjølsvik, E.T.; Lie, Ø.H.; Ribe, M.; Stokke, M.K.; Hegbom, F.; Scheirlynck, E.S.; Gjertsen, E.; Andresen, K.; Helle-Valle, T.M.; et al. The Mitral Annulus Disjunction Arrhythmic Syndrome. J. Am. Coll. Cardiol. 2018, 72, 1600–1609. [Google Scholar] [CrossRef]
- Pontone, G.; Rossi, A.; Guglielmo, M.; Dweck, M.R.; Gaemperli, O.; Nieman, K.; Pugliese, F.; Maurovich-Horvat, P.; Gimelli, A.; Cosyns, B.; et al. Clinical Applications of Cardiac Computed Tomography: A Consensus Paper of the European Association of Cardiovascular Imaging—Part I. Eur. Heart J. Cardiovasc. Imaging 2022, 23, 299–314. [Google Scholar] [CrossRef]
- Conte, E.; Mushtaq, S.; Muscogiuri, G.; Formenti, A.; Annoni, A.; Mancini, E.; Ricci, F.; Melotti, E.; Gigante, C.; Lorenza, Z.; et al. The Potential Role of Cardiac CT in the Evaluation of Patients With Known or Suspected Cardiomyopathy: From Traditional Indications to Novel Clinical Applications. Front. Cardiovasc. Med. 2021, 8, 709124. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, S.; Jahnke, C.; Loebe, S.; Oebel, S.; Weber, A.; Spampinato, R.; Richter, S.; Doering, M.; Bollmann, A.; Sommer, P.; et al. Cardiovascular Magnetic Resonance Imaging in Patients with Cardiac Implantable Electronic Devices: A Device-Dependent Imaging Strategy for Improved Image Quality. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1051–1061. [Google Scholar] [CrossRef] [PubMed]
- Conte, E.; Mushtaq, S.; Carbucicchio, C.; Piperno, G.; Catto, V.; Mancini, M.E.; Formenti, A.; Annoni, A.; Guglielmo, M.; Baggiano, A.; et al. State of the Art Paper: Cardiovascular CT for Planning Ventricular Tachycardia Ablation Procedures. J. Cardiovasc. Comput. Tomogr. 2021, 15, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Meijboom, W.B.; Meijs, M.F.L.; Schuijf, J.D.; Cramer, M.J.; Mollet, N.R.; van Mieghem, C.A.G.; Nieman, K.; van Werkhoven, J.M.; Pundziute, G.; Weustink, A.C.; et al. Diagnostic Accuracy of 64-Slice Computed Tomography Coronary Angiography. A Prospective, Multicenter, Multivendor Study. J. Am. Coll. Cardiol. 2008, 52, 2135–2144. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; Rossi, A.; Guglielmo, M.; Dweck, M.R.; Gaemperli, O.; Nieman, K.; Pugliese, F.; Maurovich-Horvat, P.; Gimelli, A.; Cosyns, B.; et al. Clinical Applications of Cardiac Computed Tomography: A Consensus Paper of the European Association of Cardiovascular Imaging—Part II. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e136–e161. [Google Scholar] [CrossRef]
- Gräni, C.; Buechel, R.R.; Kaufmann, P.A.; Kwong, R.Y. Multimodality Imaging in Individuals with Anomalous Coronary Arteries. JACC Cardiovasc. Imaging 2017, 10, 471–481. [Google Scholar] [CrossRef]
- Nolan, J.P.; Soar, J.; Cariou, A.; Cronberg, T.; Moulaert, V.R.M.; Deakin, C.D.; Bottiger, B.W.; Friberg, H.; Sunde, K.; Sandroni, C. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-Resuscitation Care 2015. Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015, 95, 202–222. [Google Scholar] [CrossRef]
- Caforio, A.L.P.; Marcolongo, R.; Basso, C.; Iliceto, S. Clinical Presentation and Diagnosis of Myocarditis. Heart 2015, 101, 1332–1344. [Google Scholar] [CrossRef]
- Garcia-Pavia, P.; Rapezzi, C.; Adler, Y.; Arad, M.; Basso, C.; Brucato, A.; Burazor, I.; Caforio, A.L.P.; Damy, T.; Eriksson, U.; et al. Diagnosis and Treatment of Cardiac Amyloidosis: A Position Statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2021, 42, 1554–1568. [Google Scholar] [CrossRef]
- Cluitmans, M.J.M.; Bear, L.R.; Nguyên, U.C.; van Rees, B.; Stoks, J.; ter Bekke, R.M.A.; Mihl, C.; Heijman, J.; Lau, K.D.; Vigmond, E.; et al. Noninvasive Detection of Spatiotemporal Activation-Repolarization Interactions That Prime Idiopathic Ventricular Fibrillation. Sci. Transl. Med. 2021, 13, 1–11. [Google Scholar] [CrossRef]
- Ramanathan, C.; Ghanem, R.N.; Jia, P.; Ryu, K.; Rudy, Y. Noninvasive Electrocardiographic Imaging for Cardiac Electrophysiology and Arrhythmia. Nat. Med. 2004, 10, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Cluitmans, M.; Brooks, D.H.; MacLeod, R.; Dössel, O.; Guillem, M.S.; Van Dam, P.M.; Svehlikova, J.; He, B.; Sapp, J.; Wang, L.; et al. Validation and Opportunities of Electrocardiographic Imaging: From Technical Achievements to Clinical Applications. Front. Physiol. 2018, 9, 01305. [Google Scholar] [CrossRef] [PubMed]
- Pereira, H.; Niederer, S.; Rinaldi, C.A. Electrocardiographic Imaging for Cardiac Arrhythmias and Resynchronization Therapy. Europace 2020, 22, 1447–1462. [Google Scholar] [CrossRef] [PubMed]
- Cluitmans, M.J.M.; Bonizzi, P.; Karel, J.M.H.; Das, M.; Kietselaer, B.L.J.H.; de Jong, M.M.J.; Prinzen, F.W.; Peeters, R.L.M.; Westra, R.L.; Volders, P.G.A. In Vivo Validation of Electrocardiographic Imaging. JACC Clin. Electrophysiol. 2017, 3, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Bear, L.R.; LeGrice, I.J.; Sands, G.B.; Lever, N.A.; Loiselle, D.S.; Paterson, D.J.; Cheng, L.K.; Smaill, B.H. How Accurate Is Inverse Electrocardiographic Mapping? A Systematic In Vivo Evaluation. Circ. Arrhythm. Electrophysiol. 2018, 11, e006108. [Google Scholar] [CrossRef] [PubMed]
- Wiggers, C.J. The Mechanism and Nature of Ventricular Fibrillation. Am. Heart J. 1940, 20, 399–412. [Google Scholar] [CrossRef]
- Rudy, Y. Noninvasive Mapping of Repolarization with Electrocardiographic Imaging. J. Am. Heart Assoc. 2021, 10, 3–6. [Google Scholar] [CrossRef]
- Bear, L.R.; Cluitmans, M.; Abell, E.; Rogier, J.; Labrousse, L.; Cheng, L.K.; Le Grice, I.; Lever, N.; Sands, G.B.; Smaill, B.; et al. Electrocardiographic Imaging of Repolarization Abnormalities. J. Am. Heart Assoc. 2021, 10, e020153. [Google Scholar] [CrossRef]
- Sande, J.N.T.; Postema, P.G.; Boekholdt, S.M.; Tan, H.L.; Van Der Heijden, J.F.; De Groot, N.M.S.; Volders, P.G.A.; Zeppenfeld, K.; Boersma, L.V.A.; Nannenberg, E.A.; et al. Detailed Characterization of Familial Idiopathic Ventricular Fibrillation Linked to the DPP6 Locus. Heart Rhythm 2016, 13, 905–912. [Google Scholar] [CrossRef]
- ter Bekke, R.M.A.; Isaacs, A.; Barysenka, A.; Hoos, M.B.; Jongbloed, J.D.H.; Hoorntje, J.C.A.; Patelski, A.S.M.; Helderman-van den Enden, A.T.J.M.; van den Wijngaard, A.; Stoll, M.; et al. Heritability in a SCN5A-Mutation Founder Population with Increased Female Susceptibility to Non-Nocturnal Ventricular Tachyarrhythmia and Sudden Cardiac Death. Heart Rhythm 2017, 14, 1873–1881. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verheul, L.M.; Groeneveld, S.A.; Kirkels, F.P.; Volders, P.G.A.; Teske, A.J.; Cramer, M.J.; Guglielmo, M.; Hassink, R.J. State-of-the-Art Multimodality Imaging in Sudden Cardiac Arrest with Focus on Idiopathic Ventricular Fibrillation: A Review. J. Clin. Med. 2022, 11, 4680. https://doi.org/10.3390/jcm11164680
Verheul LM, Groeneveld SA, Kirkels FP, Volders PGA, Teske AJ, Cramer MJ, Guglielmo M, Hassink RJ. State-of-the-Art Multimodality Imaging in Sudden Cardiac Arrest with Focus on Idiopathic Ventricular Fibrillation: A Review. Journal of Clinical Medicine. 2022; 11(16):4680. https://doi.org/10.3390/jcm11164680
Chicago/Turabian StyleVerheul, Lisa M., Sanne A. Groeneveld, Feddo P. Kirkels, Paul G. A. Volders, Arco J. Teske, Maarten J. Cramer, Marco Guglielmo, and Rutger J. Hassink. 2022. "State-of-the-Art Multimodality Imaging in Sudden Cardiac Arrest with Focus on Idiopathic Ventricular Fibrillation: A Review" Journal of Clinical Medicine 11, no. 16: 4680. https://doi.org/10.3390/jcm11164680
APA StyleVerheul, L. M., Groeneveld, S. A., Kirkels, F. P., Volders, P. G. A., Teske, A. J., Cramer, M. J., Guglielmo, M., & Hassink, R. J. (2022). State-of-the-Art Multimodality Imaging in Sudden Cardiac Arrest with Focus on Idiopathic Ventricular Fibrillation: A Review. Journal of Clinical Medicine, 11(16), 4680. https://doi.org/10.3390/jcm11164680






