Factors Associated with Cardiac/Pericardial Injury among Blunt Injury Patients: A Nationwide Study in Japan
Abstract
:1. Introduction
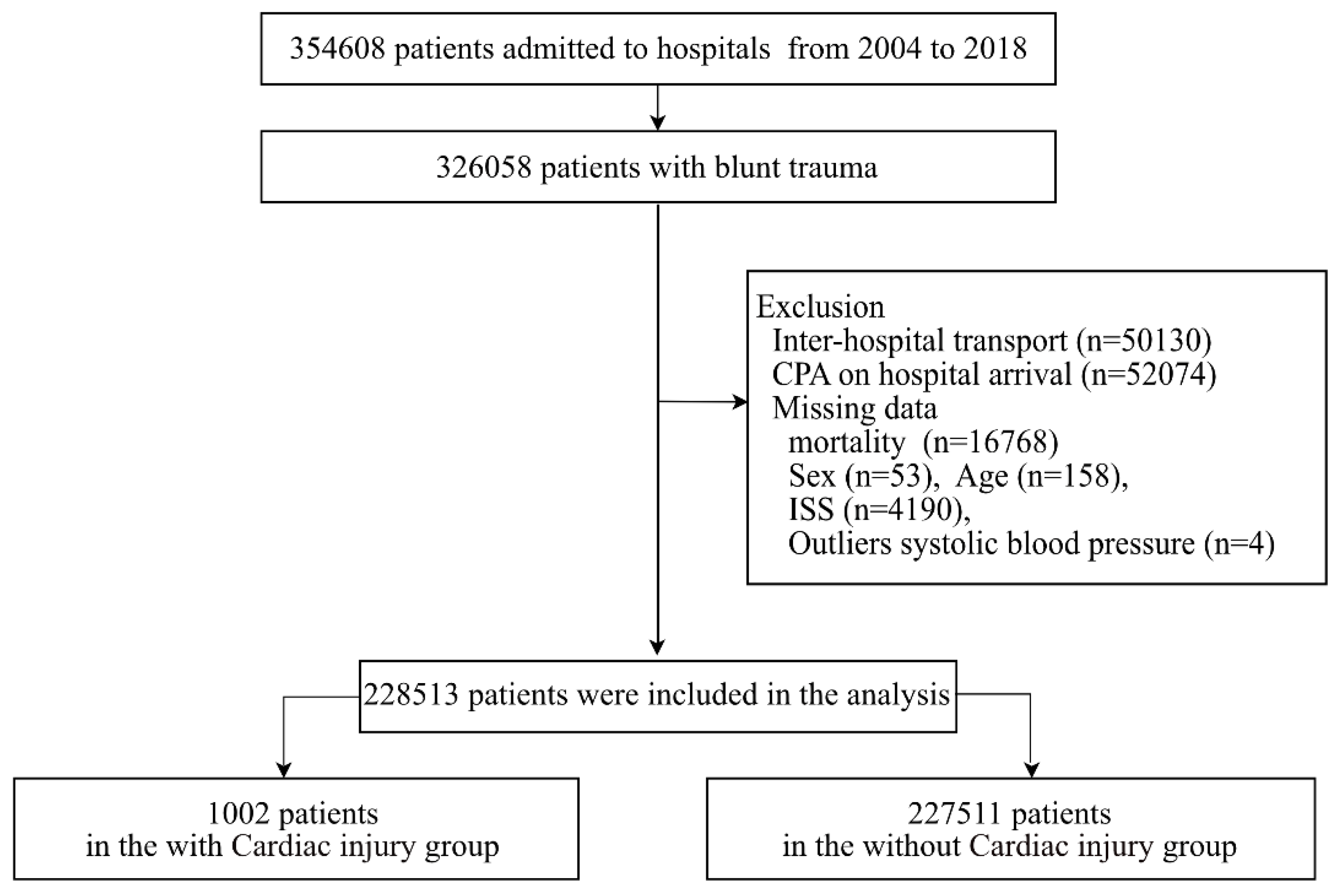
2. Materials and Methods
2.1. Study Design, Population, and Setting
2.2. Japan Trauma Data Bank
2.3. Participants
2.4. Variables
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanschen, M.; Kanz, K.G.; Kirchhoff, C.; Khalil, P.N.; Wierer, M.; van Griensven, M.; Laugwitz, K.L.; Biberthaler, P.; Lefering, R.; Huber-Wagner, S.; et al. Blunt Cardiac Injury in the Severely Injured-A Retrospective Multicentre Study. PLoS ONE 2015, 10, e0131362. [Google Scholar] [CrossRef] [PubMed]
- Grigorian, A.; Milliken, J.; Livingston, J.K.; Spencer, D.; Gabriel, V.; Schubl, S.D.; Kong, A.; Barrios, C.; Joe, V.; Nahmias, J. National risk factors for blunt cardiac injury: Hemopneumothorax is the strongest predictor. Am. J. Surg. 2019, 217, 639–642. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.V.; Charles, M.; Garrett, R.C.; Kempe, P.W.; Howard, C.A.; Khorgami, Z. Ten-Year Trends in Traumatic Cardiac Injury and Outcomes: A Trauma Registry Analysis. Ann. Thorac. Surg. 2020, 110, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Pretre, R.; Chilcott, M. Blunt trauma to the heart and great vessels. N. Engl. J. Med. 1997, 336, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, P.G.R.; Georgiou, C.; Inaba, K.; DuBose, J.; Plurad, D.; Chan, L.S.; Toms, C.; Noguchi, T.T.; Demetriades, D. Blunt Cardiac Trauma: Lessons Learned from the Medical Examiner. J. Trauma Inj. Infect. Critical Care 2009, 67, 1259–1264. [Google Scholar] [CrossRef]
- Turan, A.A.; Karayel, F.A.; Akyildiz, E.; Pakis, I.; Uzun, I.; Gurpinar, K.; Atilmis, U.; Kir, Z. Cardiac injuries caused by blunt trauma: An autopsy based assessment of the injury pattern. J. Forensic Sci. 2010, 55, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Brathwaite, C.E.; Rodriguez, A.; Turney, S.Z.; Dunham, C.M.; Cowley, R. Blunt traumatic cardiac rupture. A 5-year experience. Ann. Surg. 1990, 212, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Fulda, G.; Brathwaite, C.E.; Rodriguez, A.; Turney, S.Z.; Dunham, C.M.; Cowley, R.A. Blunt traumatic rupture of the heart and pericardium: A ten-year experience (1979–1989). J. Trauma 1991, 31, 167–172; discussion 172–173. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors: Student Course Manual, 10th ed.; American College of Surgeons: Chicago, IL, USA, 2018. [Google Scholar]
- The Japanese Association for the Surgery of Trauma. Japan Advanced Trauma Evaluation and Care, 6th ed.; Herusu Shuppan Company: Tokyo, Japan, 2021. (In Japanese) [Google Scholar]
- Hondo, K.; Shiraishi, A.; Fujie, S.; Saitoh, D.; Otomo, Y. In-Hospital Trauma Mortality Has Decreased in Japan Possibly Due to Trauma Education. J. Am. Coll. Surg. 2013, 217, 850–857.e1. [Google Scholar] [CrossRef]
- Sybrandy, K.C.; Cramer, M.J.; Burgersdijk, C. Diagnosing cardiac contusion: Old wisdom and new insights. Heart 2003, 89, 485–489. [Google Scholar] [CrossRef]
- Emet, M.; Akoz, A.; Aslan, S.; Saritas, A.; Cakir, Z.; Acemoglu, H. Assessment of cardiac injury in patients with blunt chest trauma. Eur. J. Trauma Emerg. Surg. 2010, 36, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.M.; Li, H.; Wei, G.B.; Liu, C.P.; Du, D.Y.; Kong, L.W.; Li, C.H.; Yang, J.; Yang, Q. Blunt Cardiac Injury: A Single-Center 15-Year Experience. Am. Surg. 2020, 86, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Boeken, U.; Feindt, P.; Gramsch-Zabel, H.; Raunest, J.; Micek, M.; Schulte, H.D.; Gams, E. The Incidence of Myocardial Contusion in 160 Patients with Blunt Chest Trauma. Eur. J. Trauma 2000, 26, 111–115. [Google Scholar] [CrossRef]
- Joseph, B.; Jokar, T.O.; Khalil, M.; Haider, A.A.; Kulvatunyou, N.; Zangbar, B.; Tang, A.; Zeeshan, M.; O’Keeffe, T.; Abbas, D.; et al. Identifying the broken heart: Predictors of mortality and morbidity in suspected blunt cardiac injury. Am. J. Surg. 2016, 211, 982–988. [Google Scholar] [CrossRef]
- Clancy, K.; Velopulos, C.; Bilaniuk, J.W.; Collier, B.; Crowley, W.; Kurek, S.; Lui, F.; Nayduch, D.; Sangosanya, A.; Tucker, B.; et al. Screening for blunt cardiac injury: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2012, 73, S301–S306. [Google Scholar] [CrossRef] [PubMed]
- Stojanovska, J.; Koweek, L.M.H.; Chung, J.H.; Ghoshhajra, B.B.; Walker, C.M.; Beache, G.M.; Berry, M.F.; Colletti, P.M.; Davis, A.M.; Hsu, J.Y.; et al. ACR Appropriateness Criteria® Blunt Chest Trauma-Suspected Cardiac Injury. J. Am. Coll. Radiol. 2020, 17, S380–S390. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Japan Trauma Data Bank Report 2019. Available online: https://www.jtcr-jatec.org/traumabank/index.htm (accessed on 12 May 2022). (In Japanese).
- Katayama, Y.; Kitamura, T.; Hirose, T.; Kiguchi, T.; Matsuyama, T.; Takahashi, H.; Kiyohara, K.; Sado, J.; Adachi, S.; Noda, T.; et al. Pelvic angiography is effective for emergency pediatric patients with pelvic fractures: A propensity-score-matching study with a nationwide trauma registry in Japan. Eur. J. Trauma Emerg. Surg. 2021, 47, 515–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit Care 2019, 23, 98. [Google Scholar] [CrossRef] [Green Version]
- Neidel, T.; Salvador, N.; Heller, A.R. Impact of systolic blood pressure limits on the diagnostic value of triage algorithms. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 118. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, P.G.R.; Inaba, K.; Oncel, D.; DuBose, J.; Chan, L.; Rhee, P.; Salim, A.; Browder, T.; Brown, C.; Demetriades, D. Blunt Cardiac Rupture: A 5-Year NTDB Analysis. J. Trauma Inj. Infect. Critical Care 2009, 67, 788–791. [Google Scholar] [CrossRef] [PubMed]
- Trends in Traffic Accidents. The Open Data about Traffic Accident. Available online: https://www.e-stat.go.jp/dbview?sid=0003281500 (accessed on 12 May 2022). (In Japanese).
- White Paper on Traffic Safety in Japan 2021. Available online: https://www8.cao.go.jp/koutu/taisaku/r03kou_haku/english/pdf/wp2021-1.pdf (accessed on 26 July 2022).
- National Police Agency. Traffic Bureau. Available online: https://www.npa.go.jp/english/bureau/traffic/index.html (accessed on 22 July 2022).
- Khouzam, R.N.; Al-Mawed, S.; Farah, V.; Mizeracki, A. Next-Generation Airbags and the Possibility of Negative Outcomes Due to Thoracic Injury. Can. J. Cardiol. 2014, 30, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Parmley, L.F.; Manion, W.C.; Mattingly, T.W. Nonpenetrating traumatic injury of the heart. Circulation 1958, 18, 371–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Gabler, H.C. Risk of thoracic injury from direct steering wheel impact in frontal crashes. J. Trauma Acute Care Surg. 2014, 76, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Thor, C.P.; Gabler, H.C. The influence of airbags on thoracic organ lesion types-biomed 2009. Biomed. Sci. Instrum. 2009, 45, 352–357. [Google Scholar]
- Britt, L.D.; Weireter, L.J., Jr.; Riblet, J.L.; Asensio, J.A.; Maull, K. Priorities in the management of profound shock. Surg. Clin. N. Am. 1996, 76, 645–660. [Google Scholar] [CrossRef]
- Perez, M.R.; Rodriguez, R.M.; Baumann, B.M.; Langdorf, M.I.; Anglin, D.; Bradley, R.N.; Medak, A.J.; Mower, W.R.; Hendey, G.W.; Nishijima, D.K.; et al. Sternal fracture in the age of pan-scan. Injury 2015, 46, 1324–1327. [Google Scholar] [CrossRef] [Green Version]
- Fokin, A.A.; Wycech Knight, J.; Abid, A.T.; Yoshinaga, K.; Alayon, A.L.; Grady, R.; Weisz, R.D.; Puente, I. Sternal fractures in blunt trauma patients. Eur. J. Trauma Emerg. Surg. 2022, 1–12. [Google Scholar] [CrossRef]
- Recinos, G.; Inaba, K.; Dubose, J.; Barmparas, G.; Teixeira, P.G.; Talving, P.; Plurad, D.; Green, D.; Demetriades, D. Epidemiology of sternal fractures. Am. Surg. 2009, 75, 401–404. [Google Scholar] [CrossRef]
- Oyetunji, T.A.; Jackson, H.T.; Obirieze, A.C.; Moore, D.; Branche, M.J.; Greene, W.R.; Cornwell, E.E., 3rd; Siram, S.M. Associated injuries in traumatic sternal fractures: A review of the National Trauma Data Bank. Am. Surg. 2013, 79, 702–705. [Google Scholar] [CrossRef]
- Fokin, A.A.; Wycech Knight, J.; Yoshinaga, K.; Abid, A.T.; Grady, R.; Alayon, A.L.; Puente, I. Blunt Cardiac Injury in Patients with Sternal Fractures. Cureus 2022, 14, e22841. [Google Scholar] [CrossRef] [PubMed]
- Racine, S.; Drake, D. BET 3: Bedside ultrasound for the diagnosis of sternal fracture. Emerg. Med. J. 2015, 32, 971–972. [Google Scholar] [CrossRef] [PubMed]
- Rovida, S.; Orso, D.; Naeem, S.; Vetrugno, L.; Volpicelli, G. Lung ultrasound in blunt chest trauma: A clinical review. Ultrasound 2022, 30, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.M.; Du, D.Y.; Kong, L.W.; Yang, J.; Li, H.; Wei, G.B.; Li, C.H.; Liu, C.P. Emergency Surgery for Blunt Cardiac Injury: Experience in 43 Cases. World J. Surg. 2020, 44, 1666–1672. [Google Scholar] [CrossRef] [PubMed]
| Cardiac Injury (+) | Cardiac Injury (−) | ||
|---|---|---|---|
| N = 1002 | N = 227,511 | p Value | |
| Admission year, n (%) | <0.001 | ||
| 2004–2006 | 51 (5.1) | 7612 (3.4) | |
| 2007–2009 | 171 (17.1) | 24,145 (10.6) | |
| 2010–2012 | 276 (27.5) | 49,482 (21.8) | |
| 2013–2015 | 270 (27.0) | 77,749 (34.2) | |
| 2016–2018 | 234 (23.4) | 68,523 (30.1) | |
| Age, years, median (IQR) | 49 [27–68] | 62 [38–78] | <0.001 |
| Male, sex, n (%) | 702 (70.1) | 141,711 (62.3) | <0.001 |
| Type of patients, n (%) | <0.001 | ||
| Car driver | 313 (31.2) | 20,272 (8.9) | |
| Front seat passenger | 48 (4.8) | 3879 (1.7) | |
| Back seat passenger | 24 (2.4) | 2952 (1.3) | |
| Motorcyclist | 193 (19.3) | 27,425 (12.1) | |
| Bicyclist | 59 (5.9) | 19,098 (8.4) | |
| Pedestrian | 94 (9.4) | 18,368 (8.1) | |
| Fall from heights | 128 (12.8) | 21,631 (9.5) | |
| Fall down | 39 (3.9) | 91,036 (40.0) | |
| Other | 104 (10.4) | 22,850 (10.0) | |
| Systolic BP on arrival, mmHg, median (IQR) | 114 [83–139] | 137 [137–158] | <0.001 |
| Heart rate on arrival, bpm, median (IQR) | 96 [80–116] | 83 [72–96] | <0.001 |
| Hypotension (SBP < 80 mmHg), n (%) | 207 (20.7) | 7441 (3.3) | <0.001 |
| Concomitant injury | |||
| Head injury, n (%) | 238 (23.8) | 72,207 (31.7) | <0.001 |
| Face injury, n (%) | 11 (1.1) | 1805 (0.8) | 0.366 |
| Neck injury, n (%) | 1 (0.1) | 374 (0.2) | 0.910 |
| Chest injury, n (%) | 824 (82.2) | 49,037 (21.6) | <0.001 |
| Abdominal injury, n (%) | 160 (16.0) | 10,550 (4.6) | <0.001 |
| Spine injury, n (%) | 75 (7.5) | 23,976 (10.5) | 0.002 |
| Lower extremity injury including pelvis, n (%) | 237 (23.7) | 64,644 (28.4) | 0.001 |
| Upper extremity injury, n (%) | 52 (5.2) | 12,202 (5.4) | 0.863 |
| Concomitant thoracic injury | |||
| Thoracic aortic injury, n (%) | 41 (4.1) | 1069 (0.5) | <0.001 |
| Esophageal injury, n (%) | 0 (0.0) | 23 (0.0) | 1.000 |
| Pulmonary contusion, n (%) | 420 (41.9) | 25,084 (11.0) | <0.001 |
| Tracheal injury, n (%) | 2 (0.2) | 108 (0.0) | 0.142 |
| Rib fracture, n (%) | 483 (48.2) | 42,585 (18.7) | <0.001 |
| Sternal fracture, n (%) | 127 (12.7) | 3675 (1.6) | <0.001 |
| Clavicle fracture, n (%) | 91 (9.1) | 12,240 (5.4) | <0.001 |
| Hemothorax/pneumothorax, n (%) | 372 (37.1) | 26,893 (11.8) | <0.001 |
| Thoracic spinal cord injury/fracture, n (%) | 66 (6.6) | 11,105 (4.9) | 0.015 |
| AIS of cardiac injury, n (%) | |||
| 1 | 594 (59.3) | − | |
| 2 | 43 (4.3) | − | |
| 3 | 88 (8.8) | − | |
| 4 | 20 (2.0) | − | |
| 5 | 224 (22.4) | − | |
| 6 | 33 (3.3) | − | |
| ISS, median (IQR) | 25 [17–35] | 10 [9–19] | <0.001 |
| Cardiac Injury | Univariable Analyses | Multivariable Analyses | |||
|---|---|---|---|---|---|
| N = 228,513 | % (n/N) | Crude OR (95% CI) | p Value | Adjusted a OR (95% CI) | p Value |
| Admission year | |||||
| 2004–2006 | 0.67 (51/7663) | Reference | Reference | ||
| 2007–2009 | 0.70 (171/24,316) | 1.057 (0.772–1.447) | 0.729 | 1.167 (0.849–1.604) | 0.340 |
| 2010–2012 | 0.55 (276/49,758) | 0.833 (0.617–1.123) | 0.231 | 1.058 (0.780–1.434) | 0.716 |
| 2013–2015 | 0.35 (270/78,019) | 0.518 (0.384–0.700) | <0.001 | 0.719 (0.530–0.976) | 0.034 |
| 2016–2018 | 0.34 (234/68,757) | 0.510 (0.376–0.691) | <0.001 | 0.711 (0.521–0.970) | 0.032 |
| Age groups | |||||
| <20 years | 0.54 (123/22,798) | 0.936 (0.770–1.138) | 0.507 | 1.323 (1.076–1.626) | 0.008 |
| 20–64 years | 0.58 (575/99,788) | Reference | Reference | ||
| ≧65 years | 0.29 (304/105,927) | 0.497 (0.432–0.571) | <0.001 | 1.029 (0.885–1.196) | 0.713 |
| Sex | |||||
| Male | 0.49 (702/142,413) | 1.417 (1.237–1.622) | <0.001 | 0.968 (0.838–1.118) | 0.657 |
| Female | 0.35 (300/86,100) | Reference | Reference | ||
| Type of patients | |||||
| Car driver | 1.52 (313/20,585) | Reference | Reference | ||
| Front seat passenger | 1.22 (48/3927) | 0.801 (0.590–1.088) | 0.156 | 0.722 (0.526–0.991) | 0.044 |
| Back seat passenger | 0.81 (24/2976) | 0.527 (0.347–0.799) | 0.003 | 0.554 (0.361–0.850) | 0.007 |
| Motorcyclist | 0.70 (193/27,618) | 0.456 (0.381–0.546) | <0.001 | 0.534 (0.441–0.647) | <0.001 |
| Bicyclist | 0.31 (59/19,157) | 0.200 (0.151–0.264) | <0.001 | 0.311 (0.232–0.415) | <0.001 |
| Pedestrian | 0.51 (94/18,462) | 0.331 (0.263–0.418) | <0.001 | 0.393 (0.307–0.502) | <0.001 |
| Fall from heights | 0.59 (128/21,759) | 0.383 (0.312–0.471) | <0.001 | 0.390 (0.313–0.486) | <0.001 |
| Fall down | 0.04 (39/91,075) | 0.028 (0.020–0.039) | <0.001 | 0.058 (0.041–0.082) | <0.001 |
| Other | 0.45 (104/22,954) | 0.295 (0.236–0.368) | <0.001 | 0.421 (0.335–0.530) | <0.001 |
| Hypotension on arrival | |||||
| (+) | 2.71 (207/7648) | 7.701 (6.597–8.989) | <0.001 | 4.536 (3.802–5.412) | <0.001 |
| (−) | 0.36 (795/220,865) | Reference | Reference | ||
| Head injury | |||||
| (+) | 0.33 (238/72,445) | 0.670 (0.579–0.775) | <0.001 | 0.692 (0.593–0.807) | <0.001 |
| (−) | 0.49 (764/156,068) | Reference | Reference | ||
| Face injury | |||||
| (+) | 0.61 (11/1816) | 1.388 (0.765–2.519) | 0.281 | 1.100 (0.601–2.014) | 0.758 |
| (−) | 0.44 (991/226,697) | Reference | Reference | ||
| Neck injury | |||||
| (+) | 0.27 (1/375) | 0.607 (0.085–4.322) | 0.618 | 0.362 (0.050–2.612) | 0.314 |
| (−) | 0.44 (1001/228,138) | Reference | Reference | ||
| Abdominal injury | |||||
| (+) | 1.49 (160/10,710) | 3.908 (3.296–4.633) | <0.001 | 1.192 (0.991–1.433) | 0.063 |
| (−) | 0.39 (842/217,803) | Reference | Reference | ||
| Spine injury | |||||
| (+) | 0.31 (75/24,051) | 0.687 (0.543–0.869) | 0.002 | 0.671 (0.523–0.861) | 0.002 |
| (−) | 0.45 (927/204,462) | Reference | Reference | ||
| Lower extremity injury including pelvis | |||||
| (+) | 0.37 (237/64,881) | 0.781 (0.675–0.903) | <0.001 | 0.896 (0.767–1.047) | 0.167 |
| (−) | 0.47 (765/163,632) | Reference | Reference | ||
| Upper extremity injury | |||||
| (+) | 0.42 (52/12,254) | 0.966 (0.730–1.278) | 0.808 | 0.844 (0.635–1.122) | 0.243 |
| (−) | 0.44 (950/216,259) | Reference | Reference | ||
| Thoracic aortic injury | |||||
| (+) | 3.69 (41/1110) | 9.037 (6.574–12.424) | <0.001 | 2.722 (1.947–3.806) | <0.001 |
| (−) | 0.42 (961/227,403) | Reference | Reference | ||
| Pulmonary contusion | |||||
| (+) | 1.65 (420/25,504) | 5.824 (5.133–6.607) | <0.001 | 2.532 (2.204–2.909) | <0.001 |
| (−) | 0.29 (582/203,009) | Reference | Reference | ||
| Rib fracture | |||||
| (+) | 1.12 (483/43,068) | 4.041 (3.569–4.576) | < 0.001 | 1.362 (1.147–1.618) | <0.001 |
| (−) | 0.28 (519/185,445) | Reference | Reference | ||
| Sternal fracture | |||||
| (+) | 3.34 (127/3802) | 8.840 (7.318–10.679) | < 0.001 | 3.319 (2.696–4.085) | <0.001 |
| (−) | 0.39 (875/224,711) | Reference | Reference | ||
| Clavicle fracture | |||||
| (+) | 0.74 (91/12,331) | 1.757 (1.415–2.181) | <0.001 | 0.792 (0.631–0.992) | 0.043 |
| (−) | 0.42 (911/216,182) | Reference | Reference | ||
| Hemothorax/pneumothorax | |||||
| (+) | 1.36 (372/27,265) | 4.405 (3.873–5.010) | <0.001 | 1.689 (1.423–2.006) | <0.001 |
| (−) | 0.31 (630/201,248) | Reference | Reference | ||
| Thoracic spinal cord injury/fracture | |||||
| (+) | 0.59 (66/11,171) | 1.374 (1.070–1.765) | 0.013 | 0.828 (0.633–1.084) | 0.170 |
| (−) | 0.43 (936/217,342) | Reference | Reference | ||
| Cardiac Injury | Univariable Analyses | Multivariable Analyses | |||
|---|---|---|---|---|---|
| N = 65,107 | % (n/N) | Crude OR (95% CI) | p Value | Adjusted a OR (95% CI) | p Value |
| Admission year | |||||
| 2004–2006 | 0.98 (43/4368) | Reference | Reference | ||
| 2007–2009 | 1.04 (124/11,933) | 1.056 (0.745–1.497) | 0.759 | 1.016 (0.714–1.446) | 0.931 |
| 2010–2012 | 0.97 (203/21,028) | 0.980 (0.704–1.365) | 0.907 | 0.955 (0.683–1.336) | 0.787 |
| 2013–2015 | 0.63 (191/30,505) | 0.634 (0.455–0.884) | 0.007 | 0.618 (0.441–0.866) | 0.005 |
| 2016–2018 | 0.68 (170/24,891) | 0.692 (0.494–0.968) | 0.032 | 0.642 (0.455–0.905) | 0.011 |
| Age groups | |||||
| <20 years | 0.63 (88/14,035) | 0.783 (0.621–0.986) | 0.038 | 1.235 (0.967–1.577) | 0.090 |
| 20–64 years | 0.8 (411/51,402) | Reference | Reference | ||
| ≧65 years | 0.85 (232/27,288) | 1.064 (0.905–1.250) | 0.453 | 1.155 (0.969–1.376) | 0.108 |
| Sex | |||||
| Male | 0.78 (495/63,157) | 0.982 (0.840–1.147) | 0.817 | 0.873 (0.738–1.032) | 0.111 |
| Female | 0.8 (236/29,568) | Reference | Reference | ||
| Type of patients | |||||
| Car driver | 1.52 (313/20,585) | Reference | Reference | ||
| Front seat passenger | 1.22 (48/3927) | 0.801 (0.590–1.088) | 0.156 | 0.711 (0.517–0.976) | 0.035 |
| Back seat passenger | 0.81 (24/2976) | 0.527 (0.347–0.799) | 0.003 | 0.533 (0.347–0.819) | 0.004 |
| Motorcyclist | 0.7 (193/27,618) | 0.456 (0.381–0.546) | <0.001 | 0.535 (0.441–0.649) | <0.001 |
| Bicyclist | 0.31 (59/19,157) | 0.200 (0.151–0.264) | <0.001 | 0.289 (0.216–0.388) | <0.001 |
| Pedestrian | 0.51 (94/18,462) | 0.331 (0.263–0.418) | <0.001 | 0.360 (0.280–0.462) | <0.001 |
| Hypotension on arrival | |||||
| (+) | 3.7 (137/3704) | 5.718 (4.734–6.905) | <0.001 | 4.369 (3.529–5.408) | <0.001 |
| (−) | 0.67 (594/89,021) | Reference | Reference | ||
| Head injury | |||||
| (+) | 0.55 (179/32,658) | 0.594 (0.502–0.704) | <0.001 | 0.720 (0.601–0.862) | <0.001 |
| (−) | 0.92 (552/60,067) | Reference | Reference | ||
| Face injury | |||||
| (+) | 0.81 (8/991) | 1.024 (0.509–2.062) | 0.946 | 1.145 (0.563–2.326) | 0.709 |
| (−) | 0.79 (723/91,734) | Reference | Reference | ||
| Neck injury | |||||
| (+) | 0.55 (1/183) | 0.691 (0.097–4.934) | 0.713 | 0.524 (0.072–3.801) | 0.523 |
| (−) | 0.79 (730/92,542) | Reference | Reference | ||
| Abdominal injury | |||||
| (+) | 1.76 (122/6944) | 2.501 (2.056–3.043) | <0.001 | 1.186 (0.959–1.466) | 0.116 |
| (−) | 0.71 (609/85,781) | Reference | Reference | ||
| Spine injury | |||||
| (+) | 0.44 (33/7526) | 0.533 (0.376–0.757) | <0.001 | 0.490 (0.341–0.705) | <0.001 |
| (−) | 0.82 (698/85,199) | Reference | Reference | ||
| Lower extremity injury including pelvis | |||||
| (+) | 0.8 (162/20,346) | 1.013 (0.850–1.207) | 0.886 | 0.920 (0.765–1.106) | 0.376 |
| (−) | 0.79 (569/72,379) | Reference | Reference | ||
| Upper extremity injury | |||||
| (+) | 0.81 (35/4309) | 1.032 (0.734–1.451) | 0.856 | 0.915 (0.646–1.295) | 0.615 |
| (−) | 0.79 (696/88,416) | Reference | Reference | ||
| Thoracic aortic injury | |||||
| (+) | 4.22 (30/711) | 5.738 (3.951–8.334) | <0.001 | 2.830 (1.914–4.184) | <0.001 |
| (−) | 0.76 (701/92,014) | Reference | Reference | ||
| Pulmonary contusion | |||||
| (+) | 1.87 (303/16,246) | 3.377 (2.912–3.916) | <0.001 | 2.427 (2.068–2.847) | <0.001 |
| (−) | 0.56 (428/76,479) | Reference | Reference | ||
| Rib fracture | |||||
| (+) | 1.44 (341/23,615) | 2.582 (2.231–2.988) | <0.001 | 1.260 (1.035–1.532) | 0.021 |
| (−) | 0.56 (390/69,110) | Reference | Reference | ||
| Sternal fracture | |||||
| (+) | 3.37 (95/2818) | 4.897 (3.934–6.095) | <0.001 | 2.715 (2.138–3.447) | <0.001 |
| (−) | 0.71 (636/89,907) | Reference | Reference | ||
| Clavicle fracture | |||||
| (+) | 0.82 (70/8557) | 1.042 (0.814–1.334) | 0.745 | 0.756 (0.584–0.978) | 0.033 |
| (−) | 0.79 (661/84,168) | Reference | Reference | ||
| Hemothorax/pneumothorax | |||||
| (+) | 1.77 (248/14,011) | 2.919 (2.502–3.405) | <0.001 | 1.591 (1.303–1.942) | <0.001 |
| (−) | 0.61 (483/78,714) | Reference | Reference | ||
| Thoracic spinal cord injury/fracture | |||||
| (+) | 0.87 (32/3694) | 1.104 (0.774–1.576) | 0.585 | 0.809 (0.557–1.175) | 0.267 |
| (−) | 0.79 (699/89,031) | Reference | Reference | ||
| Overall | AIS 1 | AIS 2 | AIS 3 | AIS 4 | AIS 5 | AIS 6 | p for Trend | |
|---|---|---|---|---|---|---|---|---|
| N = 1002 | N = 594 | N = 43 | N = 88 | N = 20 | N = 224 | N = 33 | ||
| Procedure, n (%) | ||||||||
| Emergency pericardiocentesis | 99 (9.9) | 7 (1.2) | 4 (9.3) | 19 (21.6) | 1 (5.0) | 60 (26.8) | 8 (24.2) | <0.001 |
| Emergency pericardial incision | 64 (6.4) | 1 (0.2) | 2 (4.7) | 13 (14.8) | 6 (30.0) | 34 (15.2) | 8 (24.2) | <0.001 |
| Emergency thoracotomy | 235 (23.5) | 22 (3.7) | 7 (16.3) | 26 (29.5) | 11 (55.0) | 147 (65.6) | 22 (66.7) | <0.001 |
| Cardiac operation | 116 (11.6) | 0 (0.0) | 1 (2.3) | 5 (5.7) | 0 (0.0) | 100 (44.6) | 10 (30.3) | <0.001 |
| Prognosis, n (%) | ||||||||
| Death in the ER | 96 (9.6) | 8 (1.3) | 1 (2.3) | 10 (11.4) | 6 (30.0) | 55 (24.6) | 16 (48.5) | <0.001 |
| In-hospital mortality | 233 (23.3) | 44 (7.4) | 10 (23.3) | 30 (34.1) | 14 (70.0) | 108 (48.2) | 27 (81.8) | <0.001 |
| Complication, n (%) | ||||||||
| Acute kidney injury | 4 (0.4) | 0 (0.0) | 2 (4.7) | 0 (0.0) | 0 (0.0) | 2 (0.9) | 0 (0.0) | 0.192 |
| Acute respiratory distress syndrome | 7 (0.7) | 3 (0.5) | 1 (2.3) | 1 (1.1) | 0 (0.0) | 1 (0.4) | 1 (3.0) | 0.575 |
| Myocardial infarction | 1 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.4) | 0 (0.0) | 0.136 |
| Pulmonary embolism | 2 (0.2) | 0 (0.0) | 1 (2.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.0) | 0.187 |
| Pneumonia | 29 (2.9) | 17 (2.9) | 3 (7.0) | 4 (4.5) | 1 (5.0) | 4 (1.8) | 0 (0.0) | 0.354 |
| ER, emergency room |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishida, K.; Katayama, Y.; Kitamura, T.; Hirose, T.; Ojima, M.; Nakao, S.; Tachino, J.; Umemura, Y.; Kiguchi, T.; Matsuyama, T.; et al. Factors Associated with Cardiac/Pericardial Injury among Blunt Injury Patients: A Nationwide Study in Japan. J. Clin. Med. 2022, 11, 4534. https://doi.org/10.3390/jcm11154534
Ishida K, Katayama Y, Kitamura T, Hirose T, Ojima M, Nakao S, Tachino J, Umemura Y, Kiguchi T, Matsuyama T, et al. Factors Associated with Cardiac/Pericardial Injury among Blunt Injury Patients: A Nationwide Study in Japan. Journal of Clinical Medicine. 2022; 11(15):4534. https://doi.org/10.3390/jcm11154534
Chicago/Turabian StyleIshida, Kenichiro, Yusuke Katayama, Tetsuhisa Kitamura, Tomoya Hirose, Masahiro Ojima, Shunichiro Nakao, Jotaro Tachino, Yutaka Umemura, Takeyuki Kiguchi, Tasuku Matsuyama, and et al. 2022. "Factors Associated with Cardiac/Pericardial Injury among Blunt Injury Patients: A Nationwide Study in Japan" Journal of Clinical Medicine 11, no. 15: 4534. https://doi.org/10.3390/jcm11154534
APA StyleIshida, K., Katayama, Y., Kitamura, T., Hirose, T., Ojima, M., Nakao, S., Tachino, J., Umemura, Y., Kiguchi, T., Matsuyama, T., Noda, T., Kiyohara, K., Oda, J., & Ohnishi, M. (2022). Factors Associated with Cardiac/Pericardial Injury among Blunt Injury Patients: A Nationwide Study in Japan. Journal of Clinical Medicine, 11(15), 4534. https://doi.org/10.3390/jcm11154534







