Anastomotic Leak Impact on Long-Term Survival after Right Colectomy for Cancer: A Propensity-Score-Matched Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Patients
2.3. Diagnosis, Treatment, and Follow-Up of the Study Patients
2.4. Study Outcomes
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
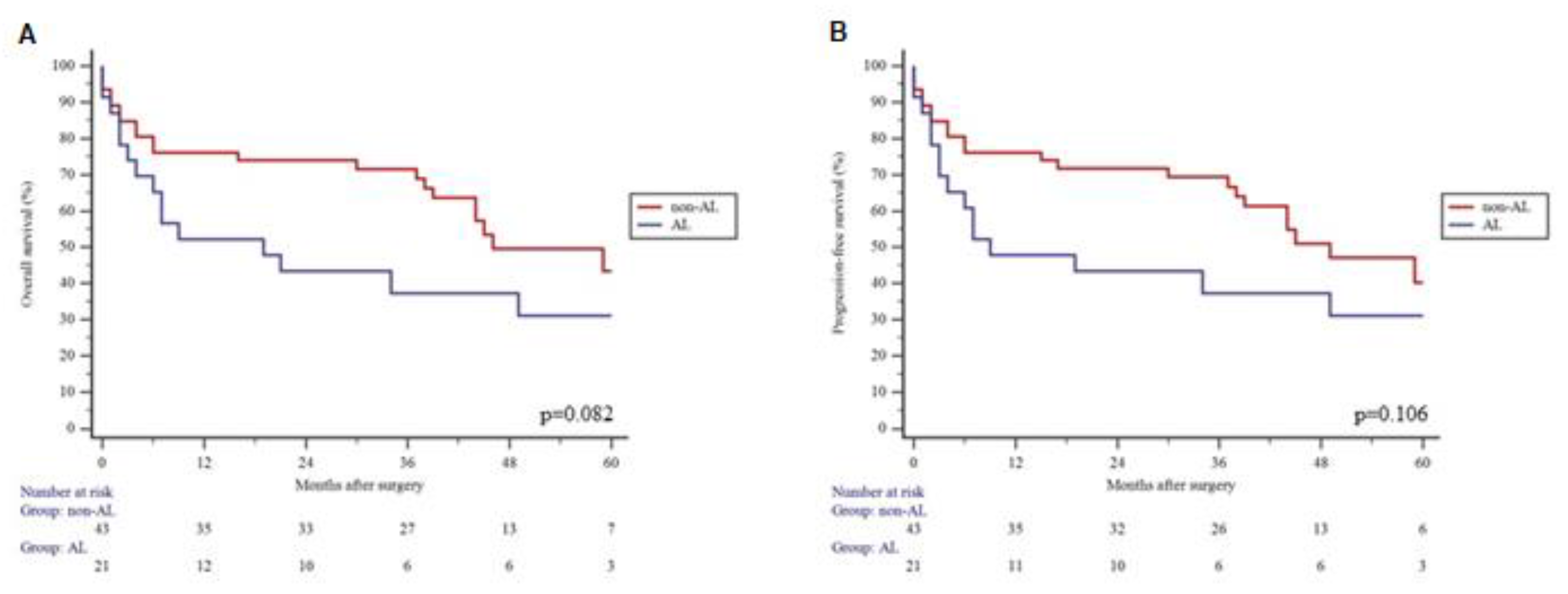
3.2. Long-Term Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Bashir Mohamed, K.; Hansen, C.H.; Krarup, P.-M.; Fransgård, T.; Madsen, M.T.; Gögenur, I. The impact of anastomotic leakage on recurrence and long-term survival in patients with colonic cancer: A systematic review and meta-analysis. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2020, 46, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Ingeholm, P.; Gögenur, I.; Iversen, L.H. Danish Colorectal Cancer Group Database. Clin. Epidemiol. 2016, 8, 465–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.S.; Huh, J.W.; Park, Y.A.; Cho, Y.B.; Yun, S.H.; Kim, H.C.; Lee, W.Y. Risk Factors of Anastomotic Leakage and Long-Term Survival after Colorectal Surgery. Medicine 2016, 95, e2890. [Google Scholar] [CrossRef]
- Kryzauskas, M.; Poskus, E.; Dulskas, A.; Bausys, A.; Jakubauskas, M.; Imbrasaite, U.; Makunaite, G.; Kuliavas, J.; Bausys, R.; Stratilatovas, E.; et al. The Problem of Colorectal Anastomosis Safety. Medicine (Baltimore). Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6959889/ (accessed on 24 February 2022).
- Koedam, T.W.A.; Bootsma, B.T.; Deijen, C.L.; van de Brug, T.; Kazemier, G.; Cuesta, M.A.; Fürst, A.; Lacy, A.M.; Haglind, E.; Tuynman, J.B.; et al. Oncological Outcomes After Anastomotic Leakage After Surgery for Colon or Rectal Cancer: Increased Risk of Local Recurrence. Ann. Surg. 2020, 275, e420–e427. [Google Scholar] [CrossRef]
- Stormark, K.; Krarup, P.; Sjövall, A.; Søreide, K.; Kvaløy, J.T.; Nordholm-Carstensen, A.; Nedrebø, B.S.; Kørner, H. Anastomotic leak after surgery for colon cancer and effect on long-term survival. Colorectal. Dis. Off. J. Assoc. Coloproctology. G B Irel. 2020, 22, 1108–1118. [Google Scholar] [CrossRef] [Green Version]
- Kryzauskas, M.; Bausys, A.; Degutyte, A.E.; Abeciunas, V.; Poskus, E.; Bausys, R.; Dulskas, A.; Strupas, K.; Poskus, T. Risk factors for anastomotic leakage and its impact on long-term survival in left-sided colorectal cancer surgery. World J. Surg. Oncol. 2020, 18, 205. [Google Scholar] [CrossRef] [PubMed]
- Jessen, M.; Nerstrøm, M.; Wilbek, T.E.; Roepstorff, S.; Rasmussen, M.S.; Krarup, P.-M. Risk factors for clinical anastomotic leakage after right hemicolectomy. Int. J. Colorectal. Dis. 2016, 31, 1619–1624. [Google Scholar] [CrossRef]
- Juvik, A.F.; Nielsen, S.; Tolstrup, M.-B.; Lykke, J.; Klein, M. Anastomotic technique is not associated with leakage rate after right hemicolectomy. Dan. Med. J. 2020, 67, A01200014. [Google Scholar]
- 2015 European Society of Coloproctology Collaborating Group. The relationship between method of anastomosis and anastomotic failure after right hemicolectomy and ileo-caecal resection: An international snapshot audit. Colorectal. Dis. Off. J. Assoc. Coloproctology G B Irel. 2017; preprint. [Google Scholar]
- Sueda, T.; Tei, M.; Yoshikawa, Y.; Furukawa, H.; Matsumura, T.; Koga, C.; Wakasugi, M.; Miyagaki, H.; Kawabata, R.; Tsujie, M.; et al. Prognostic impact of postoperative intra-abdominal infections after elective colorectal cancer resection on survival and local recurrence: A propensity score-matched analysis. Int. J. Colorectal. Dis. 2020, 35, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.Y.; Kim, B.R.; Kim, Y.W. The impact of anastomotic leakage on oncologic outcomes and the receipt and timing of adjuvant chemotherapy after colorectal cancer surgery. Int. J. Surg. 2015, 22, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Son, S.-Y.; Park, Y.-S.; Ahn, S.-H.; Park, D.J.; Kim, H.-H. Risk Factors for Anastomotic Leakage: A Retrospective Cohort Study in a Single Gastric Surgical Unit. J. Gastric. Cancer 2015, 15, 167–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fawcett, A.; Shembekar, M.; Church, J.S.; Vashisht, R.; Springall, R.G.; Nott, D.M. Smoking, hypertension, and colonic anastomotic healing; a combined clinical and histopathological study. Gut 1996, 38, 714–718. [Google Scholar] [CrossRef] [Green Version]
- Bosker, R.J.I.; Van’t Riet, E.; de Noo, M.; Vermaas, M.; Karsten, T.M.; Pierie, J.-P. Minimally Invasive versus Open Approach for Right-Sided Colectomy: A Study in 12,006 Patients from the Dutch Surgical Colorectal Audit. Dig. Surg. 2019, 36, 27–32. [Google Scholar] [CrossRef]
- Voron, T.; Bruzzi, M.; Ragot, E.; Zinzindohoue, F.; Chevallier, J.-M.; Douard, R.; Berger, A. Anastomotic Location Predicts Anastomotic Leakage After Elective Colonic Resection for Cancer. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract. 2019, 23, 339–347. [Google Scholar] [CrossRef]
- Skipper, D.; Jeffrey, M.J.; Cooper, A.J.; Alexander, P.; Taylor, I. Enhanced growth of tumour cells in healing colonic anastomoses and laparotomy wounds. Int. J. Colorectal. Dis. 1989, 4, 172–177. [Google Scholar] [CrossRef] [PubMed]
- McGregor, J.R.; Galloway, D.J.; George, W.D. Intra-luminal tumour cells and peri-anastomotic tumour growth in experimental colonic surgery. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 1992, 18, 368–372. [Google Scholar]
- Umeto, H.; Yoshida, T.; Araki, K.; Yagishita, H.; Mikami, T.; Okayasu, I. Appearance of epithelial and stromal genomic instability in background colorectal mucosa of sporadic colorectal cancer patients: Relation to age and gender. J. Gastroenterol. 2009, 44, 1036–1045. [Google Scholar] [CrossRef]
- Medzhitov, R. Origin and physiological roles of inflammation. Nature 2008, 454, 428–435. [Google Scholar] [CrossRef]
- Foppa, C.; Ng, S.C.; Montorsi, M.; Spinelli, A. Anastomotic leak in colorectal cancer patients: New insights and perspectives. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2020, 46, 943–954. [Google Scholar] [CrossRef] [PubMed]
- Iida, N.; Dzutsev, A.; Stewart, C.A.; Smith, L.; Bouladoux, N.; Weingarten, R.A.; Molina, D.A.; Salcedo, R.; Back, T.; Cramer, S.; et al. Commensal bacteria control cancer response to therapy by modulating the tumor microenvironment. Science 2013, 342, 967–970. [Google Scholar] [CrossRef] [PubMed]
| Age, Years; Mean ± SD | 69.3 ± 11.0 | |
| Gender; n (%) | Male | 206 (42.2%) |
| Female | 282 (57.8%) | |
| ASA score; n (%) | I–II | 208 (42.6%) |
| III–IV | 280 (57.4%) | |
| Chronic kidney failure; n (%) | 10 (2%) | |
| Diabetes; n (%) | 65 (13.3%) | |
| Coronary heart; n (%) | 130 (26.6%) | |
| History of stroke; n (%) | 15 (3.1%) | |
| Tumor localization; n (%) | Caecum; n (%) | 128 (26.2%) |
| Ascending colon; n (%) | 265 (54.3%) | |
| Hepatic flexure; n (%) | 63 (12.9%) | |
| Transverse colon; n (%) | 32 (6.6%) | |
| Surgical radicality | Radical; n (%) | 453 (92.8%) |
| Palliative; n (%) | 35 (7.2%) | |
| pT | T1/2; n (%) | 69 (14.1%) |
| T3/4; n (%) | 419 (85.9%) | |
| pN | N0; n (%) | 249 (51.0%) |
| N+; n (%) | 239 (49.0%) | |
| pM | 0; n (%) | 415 (85.0%) |
| 1; n (%) | 73 (15.0%) | |
| Surgical approach | Open; n (%) | 402 (82.4%) |
| MIS; n (%) | 86 (17.6%) | |
| Type of anastomosis | End-to-end; n (%) | 43 (8.8%) |
| End-to-side; n (%) | 204 (41.8%) | |
| Side-to-side; n (%) | 241 (49.4%) | |
| Anastomotic technique | Hand sewn; n (%) | 484 (99.2%) |
| Stapled; n (%) | 4 (0.8%) | |
| Postoperative complications; n (%) | 111 (22.7%) | |
| Anastomotic leakage; n (%) | 23 (4.7%) | |
| Intrahospital mortality; n (%) | 8 (1.6%) | |
| Postoperative hospitalization length, days; mean ± SD | 12 ± 7 | |
| 3 months readmission rate; n (%) | 32 (6.6%) | |
| Before Propensity Score Matching | After Propensity Score Matching | ||||||
|---|---|---|---|---|---|---|---|
| AL (n = 23) | Non-AL (n = 465) | p Value | AL (n = 23) | Non-AL (n = 46) | p Value | ||
| Age, years; mean ± SD | 72 ± 10 | 69 ± 11 | 0.227 | 72 ± 10 | 73 ± 8 | 0.584 | |
| Gender; n (%) | Male | 9 (39.1%) | 197 (42.4%) | 0.759 | 9 (39.1%) | 20 (43.5%) | 0.730 |
| Female | 14 (60.9%) | 268 (57.6%) | 14 (60.9%) | 26 (56.5%) | |||
| ASA score; n (%) | I-II | 8 (34.8%) | 200 (43.0%) | 0.436 | 8 (34.8%) | 13 (28.3%) | 0.579 |
| III-IV | 15 (65.2%) | 265 (57.0%) | 15 (65.2%) | 33 (71.7%) | |||
| Chronic kidney failure; n (%) | 1 (4.3%) | 9 (1.9%) | 0.425 | 1 (4.3%) | 0 (0%) | 0.333 | |
| Diabetes; n (%) | 2 (8.7%) | 63 (13.5%) | 0.504 | 2 (8.7%) | 8 (17.4%) | 0.477 | |
| Coronary heart; n (%) | 8 (34.8%) | 122 (26.2%) | 0.365 | 8 (34.8%) | 14 (30.4%) | 0.715 | |
| History of stroke; n (%) | 3 (13.0%) | 12 (2.6%) | 0.005 | 3 (13.0%) | 6 (13.0%) | 0.999 | |
| Tumor localization; n (%) | Caecum; n (%) | 7 (30.4%) | 127 (27.3%) | 0.445 | 7 (30.4%) | 14 (30.4%) | 0.974 |
| Ascending colon; n (%) | 11 (47.8%) | 248 (53.3%) | 11 (47.8%) | 24 (52.2%) | |||
| Hepatic flexure; n (%) | 2 (8.7%) | 64 (13.8%) | 2 (8.7%) | 3 (6.5%) | |||
| Transverse colon; n (%) | 3 (13.1%) | 26 (5.6%) | 3 (13.1%) | 5 (10.9%) | |||
| Surgical radicality | Radical; n (%) | 20 (87.0%) | 433 (93.1%) | 0.264 | 20 (87.0%) | 38 (82.6%) | 0.740 |
| Palliative; n (%) | 3 (13.0%) | 32 (6.9%) | 3 (13.0%) | 8 (17.4%) | |||
| pT | T1/2; n (%) | 3 (13.0%) | 66 (14.2%) | 0.877 | 3 (13.0%) | 8 (17.4%) | 0.740 |
| T3/4; n (%) | 20 (87.0%) | 399 (85.8%) | 20 (87.0%) | 38 (82.6%) | |||
| pN | N0; n (%) | 14 (60.9%) | 235 (50.5%) | 0.333 | 14 (60.9%) | 24 (52.2%) | 0.494 |
| N+; n (%) | 9 (39.1%) | 230 (49.5%) | 9 (39.1%) | 22 (47.8%) | |||
| pM | 0; n (%) | 18 (78.3%) | 397 (85.4%) | 0.350 | 18 (78.3%) | 36 (78.3%) | 0.999 |
| 1; n (%) | 5 (21.7%) | 68 (14.6%) | 5 (21.7%) | 10 (21.7%) | |||
| Surgical approach | Open; n (%) | 20 (87.0%) | 382 (82.2%) | 0.555 | 20 (87.0%) | 37 (80.4%) | 0.500 |
| MIS; n (%) | 3 (13.0%) | 83 (17.8%) | 3 (13.0%) | 9 (19.6%) | |||
| Type of anastomosis | End-to-end; n (%) | 2 (8.7%) | 41 (8.8%) | 0.961 | 2 (8.7%) | 3 (6.5%) | 0.945 |
| End-to-side; n (%) | 9 (39.1%) | 195 (41.9%) | 9 (39.1%) | 18 (39.1%) | |||
| Side-to-side; n (%) | 12 (52.2%) | 229 (49.3%) | 12 (52.2%) | 25 (54.3%) | |||
| Anastomotic technique | Hand sewn; n (%) | 22 (95.7%) | 462 (99.4%) | 0.055 | 22 (95.7%) | 46 (100%) | 0.154 |
| Stapled; n (%) | 1 (4.3%) | 3 (0.6%) | 1 (4.3%) | 0 (0%) | |||
| Intrahospital mortality; n (%) | 2 (8.7%) | 6 (1.3%) | 0.006 | 2 (8.7%) | 1 (2.2%) | 0.210 | |
| Postoperative hospitalization length, days; mean ± SD | 25 ± 11 | 12 ± 7 | 0.001 | 25 ± 11 | 12 ± 4 | 0.001 | |
| 3 months readmission rate; n (%) | 5 (21.7%) | 27 (5.8%) | 0.003 | 5 (21.7%) | 4 (8.7%) | 0.129 | |
| Variable | Category | Overall Survival | Disease-Free Survival | ||
|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| Anastomotic leakage | No | 1 (Reference) | 1 (Reference) | ||
| Yes | 1.77 (0.91–3.46) | 0.091 | 1.69 (0.87–3.28) | 0.116 | |
| Age | 1.09 (1.04–1.14) | 0.001 | 1.08 (1.03–1.13) | 0.001 | |
| Gender | Male | 1 (Reference) | 1 (Reference) | ||
| Female | 1.58 (0.79–3.16) | 0.196 | 1.70 (0.85–3.38) | 0.130 | |
| ASA score | 1–2 | 1 (Reference) | 1 (Reference) | ||
| 3–4 | 1.72 (0.78–3.79) | 0.173 | 1.77 (0.81–3.89) | 0.150 | |
| pT | 1–2 | 1 (Reference) | 1 (Reference) | ||
| 3–4 | 4.00 (0.96–16.68) | 0.05 | 4.21 (1.01–17.54) | 0.048 | |
| pN | N0 | 1 (Reference) | 1 (Reference) | ||
| N+ | 2.31 (1.17–4.52) | 0.015 | 2.23 (1.15–4.33) | 0.017 | |
| pM | M0 | 1 (Reference) | 1 (Reference) | ||
| M1 | 3.84 (1.89–7.80) | 0.001 | 3.66 (1.82–7.39) | 0.001 | |
| Type of surgery | Open | 1 (Reference) | 1 (Reference) | ||
| MIS | 0.99 (0.14–0.72) | 0.023 | 0.94 (0.13–0.68) | 0.020 | |
| Variable | Category | Overall Survival | Disease-Free Survival | ||
|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| Anastomotic leakage | No | 1 (Reference) | 1 (Reference) | ||
| Yes | 2.63 (1.26–5.48) | 0.010 | 2.43 (1.18–5.02) | 0.016 | |
| Age | 1.09 (1.03–1.16) | 0.001 | 1.07 (1.02–1.13) | 0.005 | |
| Gender | Male | 1 (Reference) | 1 (Reference) | ||
| Female | 1.77 (0.81–3.82) | 0.146 | 1.96 (0.91–4.21) | 0.084 | |
| ASA score | 1–2 | 1 (Reference) | 1 (Reference) | ||
| 3–4 | 0.87 (0.36–2.13) | 0.771 | 0.83 (0.34–2.04) | 0.697 | |
| pT | 1–2 | 1 (Reference) | 1 (Reference) | ||
| 3–4 | 1.36 (0.27–6.76) | 0.704 | 1.67 (0.34–8.12) | 0.524 | |
| pN | N0 | 1 (Reference) | 1 (Reference) | ||
| N+ | 1.60 (0.70–3.66) | 0.259 | 1.48 (0.66–3.32) | 0.342 | |
| pM | M0 | 1 (Reference) | 1 (Reference) | ||
| M1 | 2.34 (1.07–5.10) | 0.032 | 2.27 (1.05–4.90) | 0.036 | |
| Type of surgery | Open | 1 (Reference) | 1 (Reference) | ||
| MIS | 6.79 (0.87–52.76) | 0.067 | 7.07 (0.92–54.15) | 0.059 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dulskas, A.; Kuliavas, J.; Sirvys, A.; Bausys, A.; Kryzauskas, M.; Bickaite, K.; Abeciunas, V.; Kaminskas, T.; Poskus, T.; Strupas, K. Anastomotic Leak Impact on Long-Term Survival after Right Colectomy for Cancer: A Propensity-Score-Matched Analysis. J. Clin. Med. 2022, 11, 4375. https://doi.org/10.3390/jcm11154375
Dulskas A, Kuliavas J, Sirvys A, Bausys A, Kryzauskas M, Bickaite K, Abeciunas V, Kaminskas T, Poskus T, Strupas K. Anastomotic Leak Impact on Long-Term Survival after Right Colectomy for Cancer: A Propensity-Score-Matched Analysis. Journal of Clinical Medicine. 2022; 11(15):4375. https://doi.org/10.3390/jcm11154375
Chicago/Turabian StyleDulskas, Audrius, Justas Kuliavas, Artiomas Sirvys, Augustinas Bausys, Marius Kryzauskas, Klaudija Bickaite, Vilius Abeciunas, Tadas Kaminskas, Tomas Poskus, and Kestutis Strupas. 2022. "Anastomotic Leak Impact on Long-Term Survival after Right Colectomy for Cancer: A Propensity-Score-Matched Analysis" Journal of Clinical Medicine 11, no. 15: 4375. https://doi.org/10.3390/jcm11154375
APA StyleDulskas, A., Kuliavas, J., Sirvys, A., Bausys, A., Kryzauskas, M., Bickaite, K., Abeciunas, V., Kaminskas, T., Poskus, T., & Strupas, K. (2022). Anastomotic Leak Impact on Long-Term Survival after Right Colectomy for Cancer: A Propensity-Score-Matched Analysis. Journal of Clinical Medicine, 11(15), 4375. https://doi.org/10.3390/jcm11154375








