Real-World Evidence of the Effectiveness and Safety of Ustekinumab for the Treatment of Crohn’s Disease: Systematic Review and Meta-Analysis of Observational Studies
Abstract
:1. Introduction
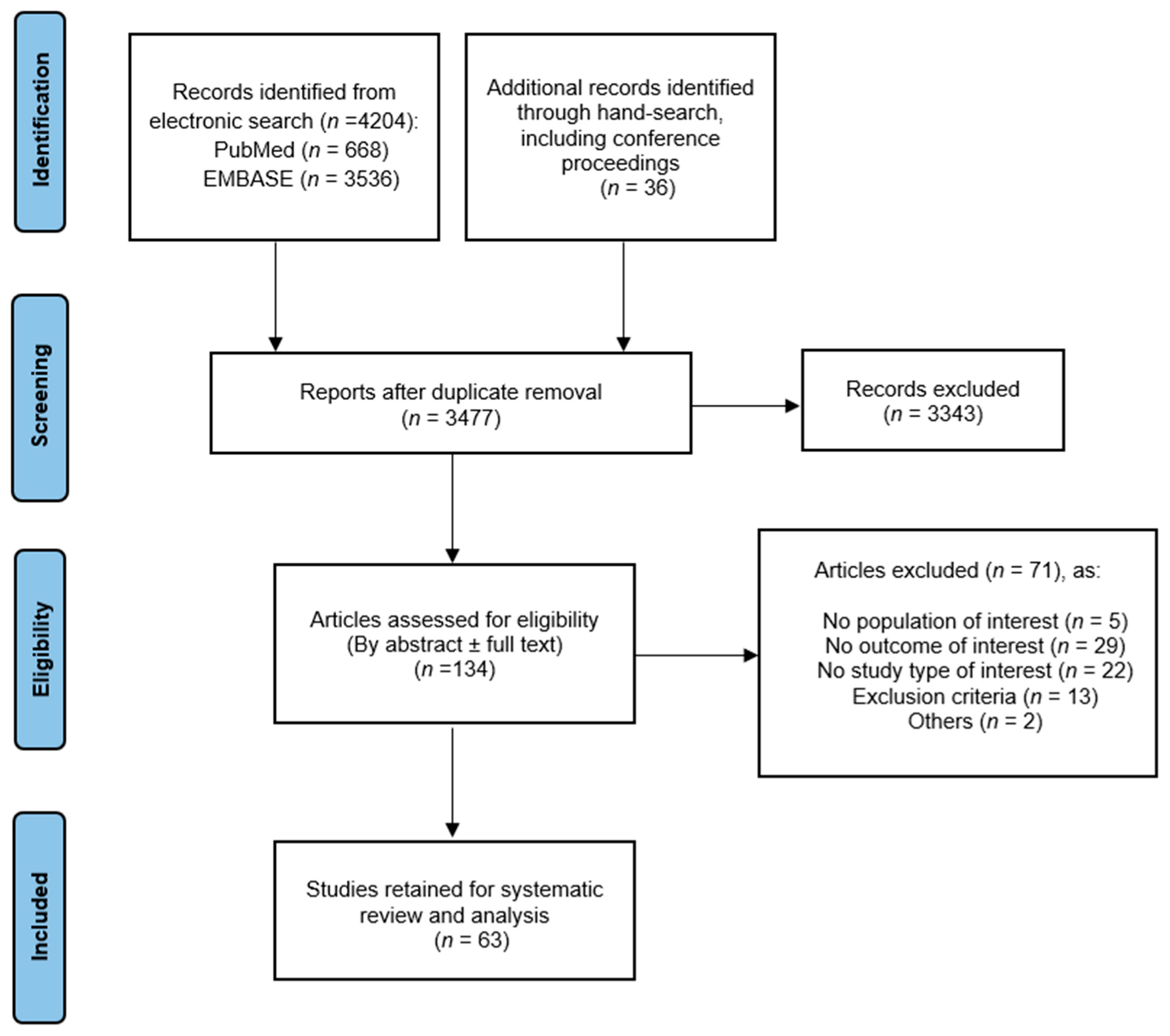
2. Materials and Methods
2.1. Literature Search and Study Selection
2.2. Selection Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Outcome Measures
2.5.1. Primary Outcomes
- Clinical and endoscopic response and remission in CD patients treated with ustekinumab in the short, medium, and long term, in a real-life setting.
- Safety of ustekinumab in CD patients.
2.5.2. Secondary Outcomes
- Effectiveness of intensification of ustekinumab treatment (either by decreasing the intervals of ustekinumab administration or by dose intensification (shortening of the ustekinumab administration interval to less than 8 weeks or administration of a reinduction IV dose of ustekinumab)).
- Predictive factors of response in a real-life setting.
2.6. Data Synthesis and Statistical Analysis
3. Results
3.1. Study Selection and Characteristics
3.2. Effectiveness of Ustekinumab
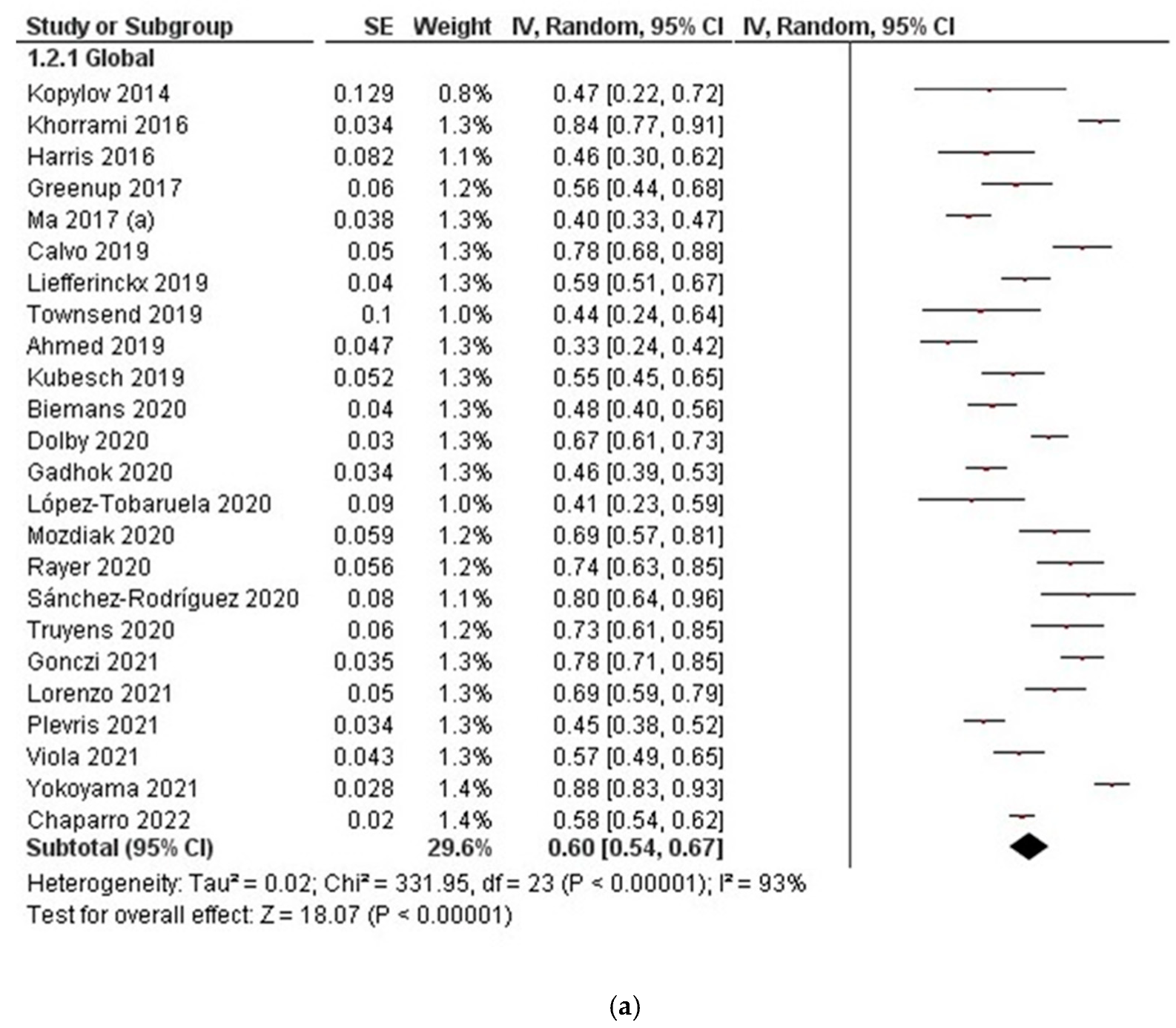
3.2.1. Clinical Response
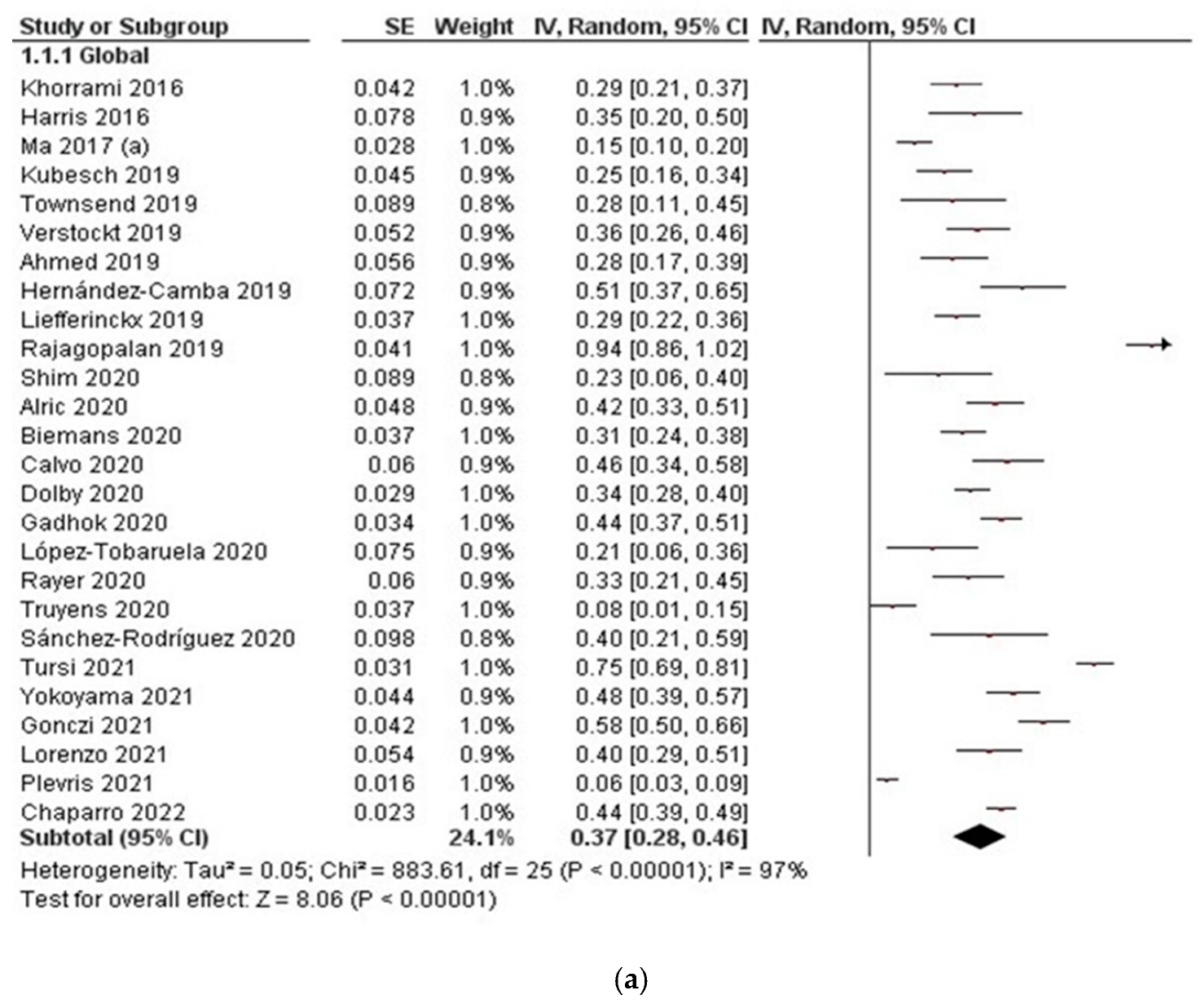
3.2.2. Clinical Remission
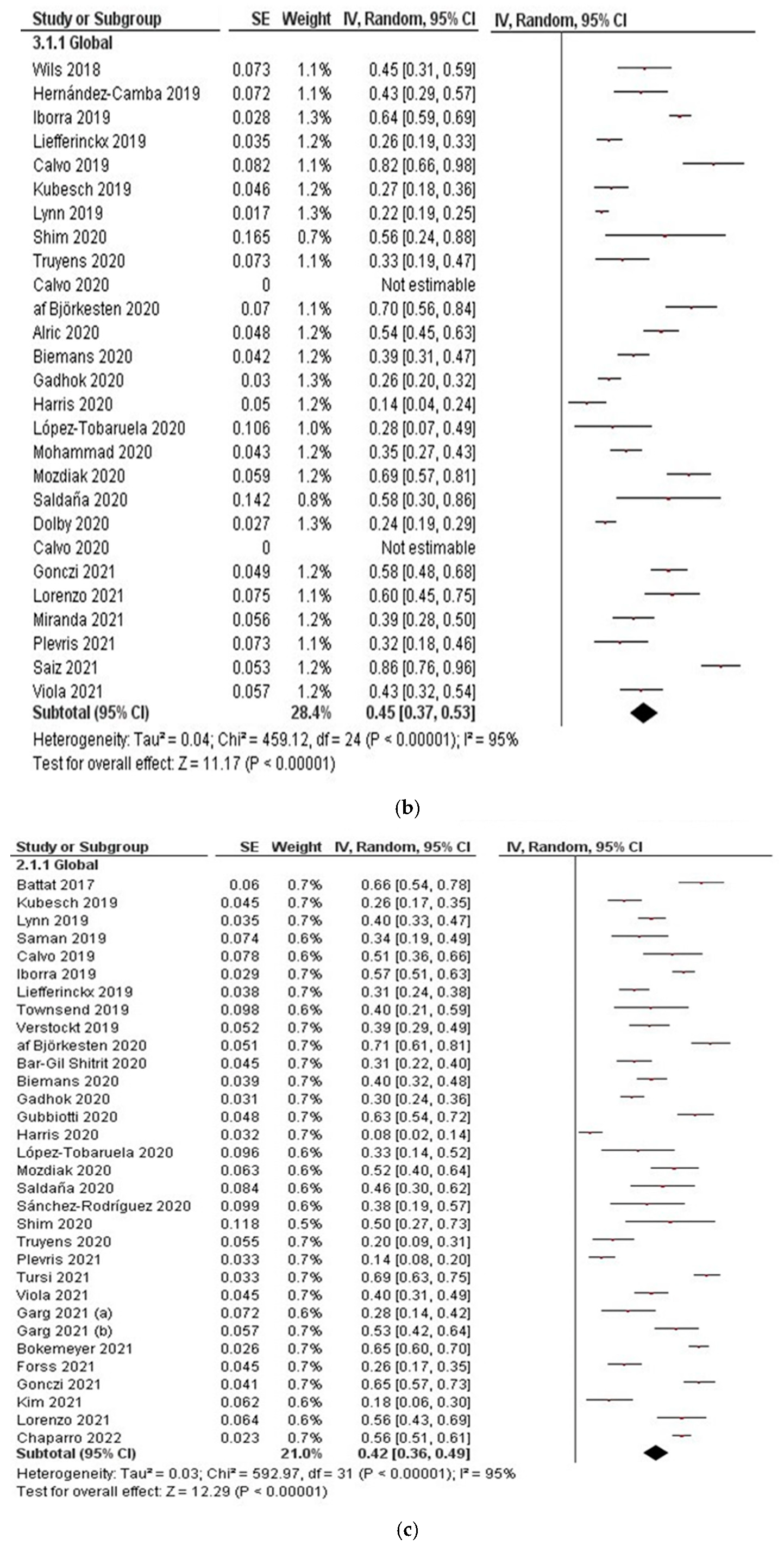
3.2.3. Corticosteroid-Free Clinical Remission
3.2.4. Endoscopic Remission
3.3. Loss of Response to Ustekinumab
3.4. Dose Optimisation
3.5. Predictors of Response
3.6. Safety
3.7. Quality of Included Studies and Risk of Publication Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, J.C.; Furlano, R.I.; Jick, S.S.; Meier, C.R. Inflammatory Bowel Disease and the Risk of Autoimmune Diseases. J. Crohn’s Colitis 2016, 10, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Bonovas, S.; Doherty, G.; Kucharzik, T.; Gisbert, J.P.; Raine, T.; Adamina, M.; Armuzzi, A.; Bachmann, O.; Bager, P.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Medical Treatment. J. Crohn’s Colitis 2020, 14, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, J.P.; Chaparro, M. Primary Failure to an Anti-TNF Agent in Inflammatory Bowel Disease: Switch (to a Second Anti-TNF Agent) or Swap (for Another Mechanism of Action)? J. Clin. Med. 2021, 10, 5318. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, J.P.; Chaparro, M. Predictors of Primary Response to Biologic Treatment [Anti-TNF, Vedolizumab, and Ustekinumab] in Patients with Inflammatory Bowel Disease: From Basic Science to Clinical Practice. J. Crohn’s Colitis 2020, 14, 694–709. [Google Scholar] [CrossRef]
- Colombel, J.F.; Feagan, B.G.; Sandborn, W.J.; Van Assche, G.; Robinson, A.M. Therapeutic drug monitoring of biologics for inflammatory bowel disease. Inflamm. Bowel Dis. 2012, 18, 349–358. [Google Scholar] [CrossRef]
- Feagan, B.G.; Sandborn, W.J.; Gasink, C.; Jacobstein, D.; Lang, Y.; Friedman, J.R.; Blank, M.A.; Johanns, J.; Gao, L.L.; Miao, Y.; et al. Ustekinumab as Induction and Maintenance Therapy for Crohn’s Disease. N. Engl. J. Med. 2016, 375, 1946–1960. [Google Scholar] [CrossRef]
- Hanauer, S.B.; Sandborn, W.J.; Feagan, B.G.; Gasink, C.; Jacobstein, D.; Zou, B.; Johanns, J.; Adedokun, O.J.; Sands, B.E.; Rutgeerts, P.; et al. IM-UNITI: Three-year Efficacy, Safety, and Immunogenicity of Ustekinumab Treatment of Crohn’s Disease. J. Crohn’s Colitis 2020, 14, 23–32. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Rebuck, R.; Wang, Y.; Zou, B.; Adedokun, O.J.; Gasink, C.; Sands, B.E.; Hanauer, S.B.; Targan, S.; Ghosh, S.; et al. Five-Year Efficacy and Safety of Ustekinumab Treatment in Crohn’s Disease: The IM-UNITI Trial. Clin. Gastroenterol. Hepatol. 2022, 20, 578–590.e574. [Google Scholar] [CrossRef]
- Adamina, M.; Bonovas, S.; Raine, T.; Spinelli, A.; Warusavitarne, J.; Armuzzi, A.; Bachmann, O.; Bager, P.; Biancone, L.; Bokemeyer, B.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Surgical Treatment. J. Crohn’s Colitis 2020, 14, 155–168. [Google Scholar] [CrossRef] [Green Version]
- Gisbert, J.P.; Chaparro, M. Ustekinumab to treat Crohn’s disease. Gastroenterol. Hepatol. 2017, 40, 688–698. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Kopylov, U.; Afif, W.; Cohen, A.; Bitton, A.; Wild, G.; Bessissow, T.; Wyse, J.; Al-Taweel, T.; Szilagyi, A.; Seidman, E. Subcutaneous ustekinumab for the treatment of anti-TNF resistant Crohn’s disease—The McGill experience. J. Crohn’s Colitis 2014, 8, 1516–1522. [Google Scholar] [CrossRef] [Green Version]
- Harris, K.A.; Horst, S.; Gadani, A.; Nohl, A.; Annis, K.; Duley, C.; Beaulieu, D.; Ghazi, L.; Schwartz, D.A. Patients with Refractory Crohn’s Disease Successfully Treated with Ustekinumab. Inflamm. Bowel Dis. 2016, 22, 397–401. [Google Scholar] [CrossRef]
- Khorrami, S.; Ginard, D.; Marin-Jimenez, I.; Chaparro, M.; Sierra, M.; Aguas, M.; Sicilia, B.; Garcia-Sanchez, V.; Suarez, C.; Villoria, A.; et al. Ustekinumab for the Treatment of Refractory Crohn’s Disease: The Spanish Experience in a Large Multicentre Open-label Cohort. Inflamm. Bowel Dis. 2016, 22, 1662–1669. [Google Scholar] [CrossRef]
- Battat, R.; Kopylov, U.; Bessissow, T.; Bitton, A.; Cohen, A.; Jain, A.; Martel, M.; Seidman, E.; Afif, W. Association between Ustekinumab trough Concentrations and Clinical, Biomarker, and Endoscopic Outcomes in Patients with Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2017, 15, 1427–1434.e1422. [Google Scholar] [CrossRef]
- Greenup, A.J.; Rosenfeld, G.; Bressler, B. Ustekinumab use in Crohn’s disease: A Canadian tertiary care centre experience. Scand. J. Gastroenterol. 2017, 52, 1354–1359. [Google Scholar] [CrossRef]
- Ma, C.; Fedorak, R.N.; Kaplan, G.G.; Dieleman, L.A.; Devlin, S.M.; Stern, N.; Kroeker, K.I.; Seow, C.H.; Leung, Y.; Novak, K.L.; et al. Clinical, endoscopic and radiographic outcomes with ustekinumab in medically-refractory Crohn’s disease: Real world experience from a multicentre cohort. Aliment. Pharmacol. Ther. 2017, 45, 1232–1243. [Google Scholar] [CrossRef]
- Ma, C.; Fedorak, R.N.; Kaplan, G.G.; Dieleman, L.A.; Devlin, S.M.; Stern, N.; Kroeker, K.I.; Seow, C.H.; Leung, Y.; Novak, K.L.; et al. Long-term Maintenance of Clinical, Endoscopic, and Radiographic Response to Ustekinumab in Moderate-to-Severe Crohn’s Disease: Real-world Experience from a Multicenter Cohort Study. Inflamm. Bowel Dis. 2017, 23, 833–839. [Google Scholar] [CrossRef] [Green Version]
- Wils, P.; Bouhnik, Y.; Michetti, P.; Flourie, B.; Brixi, H.; Bourrier, A.; Allez, M.; Duclos, B.; Serrero, M.; Buisson, A.; et al. Long-term efficacy and safety of ustekinumab in 122 refractory Crohn’s disease patients: A multicentre experience. Aliment. Pharmacol. Ther. 2018, 47, 588–595. [Google Scholar] [CrossRef]
- Ahmed, Z.; Venkata, K.; Zhang, N.; Malik, T.A. Comparative Effectiveness of Ustekinumab versus Adalimumab in Induction of Clinical Response and Remission in Crohn’s Disease: Experience of a Real-World Cohort at a Tertiary Care Inflammatory Bowel Disease Referral Center. Gastroenterol. Res. 2019, 12, 245–251. [Google Scholar] [CrossRef]
- Gonzalez-Lama, Y.; Bermejo, F.; Lopez-Sanroman, A.; Garcia-Sanchez, V.; Esteve, M.; Cabriada, J.L.; McNicholl, A.G.; Pajares, R.; Casellas, F.; Merino, O.; et al. Thiopurine methyl-transferase activity and azathioprine metabolite concentrations do not predict clinical outcome in thiopurine-treated inflammatory bowel disease patients. Aliment. Pharmacol. Ther. 2011, 34, 544–554. [Google Scholar] [CrossRef]
- Hernandez-Camba, A.; Arranz, L.; Vera, I.; Carpio, D.; Calafat, M.; Lucendo, A.J.; Taxonera, C.; Marin, S.; Garcia, M.J.; Marin, G.S.; et al. Real-world use of mycophenolate mofetil in inflammatory bowel disease: Results from the ENEIDA registry. Dig. Liver Dis. 2021, 54, 635–641. [Google Scholar] [CrossRef]
- Hoffmann, P.; Krisam, J.; Wehling, C.; Kloeters-Plachky, P.; Leopold, Y.; Belling, N.; Gauss, A. Ustekinumab: “Real-world” outcomes and potential predictors of nonresponse in treatment-refractory Crohn’s disease. World J. Gastroenterol. 2019, 25, 4481–4492. [Google Scholar] [CrossRef]
- Iborra, M.; Beltran, B.; Fernandez-Clotet, A.; Iglesias-Flores, E.; Navarro, P.; Rivero, M.; Gutierrez, A.; Sierra-Ausin, M.; Mesonero, F.; Ferreiro-Iglesias, R.; et al. Real-world long-term effectiveness of ustekinumab in Crohn’s disease: Results from the ENEIDA registry. Aliment. Pharmacol. Ther. 2020, 52, 1017–1030. [Google Scholar] [CrossRef]
- Kubesch, A.; Rueter, L.; Farrag, K.; Krause, T.; Stienecker, K.; Hausmann, J.; Filmann, N.; Dignass, A.; Stein, J.; Blumenstein, I. Short and Long-Term Effectiveness of Ustekinumab in Patients with Crohn’s Disease: Real-World Data from a German IBD Cohort. J. Clin. Med. 2019, 8, 2140. [Google Scholar] [CrossRef] [Green Version]
- Liefferinckx, C.; Verstockt, B.; Gils, A.; Noman, M.; Van Kemseke, C.; Macken, E.; De Vos, M.; Van Moerkercke, W.; Rahier, J.F.; Bossuyt, P.; et al. Long-term Clinical Effectiveness of Ustekinumab in Patients with Crohn’s Disease Who Failed Biologic Therapies: A National Cohort Study. J. Crohn’s Colitis 2019, 13, 1401–1409. [Google Scholar] [CrossRef]
- Lynn, A.M.; Loftus, E.V., Jr. Illuminating the Black Box: The Real Risk of Serious Infection with Inflammatory Bowel Disease Therapies. Gastroenterology 2018, 155, 262–265. [Google Scholar] [CrossRef] [Green Version]
- Rajagopalan, A.N.; Chaudhuri, S.; Mudenagudi, U. Depth estimation and image restoration using defocused stereo pairs. IEEE Trans. Pattern Anal. Mach. Intell. 2004, 26, 1521–1525. [Google Scholar] [CrossRef]
- Saman, S.; Goetz, M.; Wendler, J.; Malek, N.P.; Wehkamp, J.; Klag, T. Ustekinumab is effective in biological refractory Crohn’s disease patients-regardless of approval study selection criteria. Intest. Res. 2019, 17, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Townsend, T.; Razanskaite, V.; Dodd, S.; Storey, D.; Michail, S.; Morgan, J.; Davies, M.; Penman, D.; Watters, C.; Swaminathan, M.; et al. Comparative effectiveness of ustekinumab or vedolizumab after one year in 130 patients with anti-TNF-refractory Crohn’s disease. Aliment. Pharmacol. Ther. 2020, 52, 1341–1352. [Google Scholar] [CrossRef] [PubMed]
- Verstockt, B.; Dreesen, E.; Noman, M.; Outtier, A.; Van den Berghe, N.; Aerden, I.; Compernolle, G.; Van Assche, G.; Gils, A.; Vermeire, S.; et al. Ustekinumab Exposure-outcome Analysis in Crohn’s Disease Only in Part Explains Limited Endoscopic Remission Rates. J. Crohn’s Colitis 2019, 13, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Af Bjorkesten, C.G.; Ilus, T.; Hallinen, T.; Soini, E.; Eberl, A.; Hakala, K.; Heikura, M.; Jussila, A.; Koskela, R.; Koskinen, I.; et al. Objectively assessed disease activity and drug persistence during ustekinumab treatment in a nationwide real-world Crohn’s disease cohort. Eur. J. Gastroenterol. Hepatol. 2020, 32, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Alric, H.; Amiot, A.; Kirchgesner, J.; Treton, X.; Allez, M.; Bouhnik, Y.; Beaugerie, L.; Carbonnel, F.; Meyer, A. The effectiveness of either ustekinumab or vedolizumab in 239 patients with Crohn’s disease refractory to anti-tumour necrosis factor. Aliment. Pharmacol. Ther. 2020, 51, 948–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bar-Gil Shitrit, A.; Ben-Ya’acov, A.; Siterman, M.; Waterman, M.; Hirsh, A.; Schwartz, D.; Zittan, E.; Adler, Y.; Koslowsky, B.; Avni-Biron, I.; et al. Safety and effectiveness of ustekinumab for induction of remission in patients with Crohn’s disease: A multicenter Israeli study. United Eur. Gastroenterol. J. 2020, 8, 418–424. [Google Scholar] [CrossRef] [Green Version]
- Bennett, A.; Evers Carlini, L.; Duley, C.; Garrett, A.; Annis, K.; Wagnon, J.; Dalal, R.; Scoville, E.; Beaulieu, D.; Schwartz, D.; et al. A Single Center Experience with Long-Term Ustekinumab Use and Reinduction in Patients with Refractory Crohn Disease. Crohn’s Colitis 360 2020, 2, otaa013. [Google Scholar] [CrossRef]
- Biemans, V.B.C.; van der Meulen-de Jong, A.E.; van der Woude, C.J.; Lowenberg, M.; Dijkstra, G.; Oldenburg, B.; de Boer, N.K.H.; van der Marel, S.; Bodelier, A.G.L.; Jansen, J.M.; et al. Ustekinumab for Crohn’s Disease: Results of the ICC Registry, a Nationwide Prospective Observational Cohort Study. J. Crohn’s Colitis 2020, 14, 33–45. [Google Scholar] [CrossRef]
- Calvo Moya, M.I.; Omella Usieto, I.; González Lama, Y.; Matallana Royo, V.; González Partida, I.; Menchen Viso, B.; De Lucas Téllez de Meneses, R.; González Rodriguez, M.; Bella del Castillo, P.; Vera Mendoza, M.I. P545 Deep remission assessed by endoscopy, magnetic resonance or intestinal ultrasound, in refractory Crohn’s disease patients in clinical remission with ustekinumab: A real-life single-centre experience. J. Crohn’s Colitis 2020, 14, S464–S465. [Google Scholar] [CrossRef]
- Casas Deza, D.; Garcia Lopez, S.; Lafuente Blasco, M.; Vicente Lidon, R.; Nerin de la Puerta, J.; Pena Gonzalez, E.; Ber Nieto, Y.; Charro Calvillo, M.; Alcala Escriche, M.J.; Gomollon Garcia, F.; et al. Efficacy and safety of ustekinumab in real clinical practice. Retrospective multicentre study. ARAINF cohort. Gastroenterol. Hepatol. 2020, 43, 126–132. [Google Scholar] [CrossRef]
- Gadhok, R.; Fragkos, K.; Honap, S.; Hassan, J.; Whiteley, L.; Ibarra, A.; Burgess, N.; Vega, R.; Seward, E.; Mehta, S.; et al. P507 Ustekinumab: Medium-term outcomes from a UK multicentre real-world cohort. J. Crohn’s Colitis 2020, 14, S439–S440. [Google Scholar] [CrossRef]
- Barberio, B.; Savarino, E.V.; Card, T.; Canova, C.; Baldisser, F.; Gubbiotti, A.; Massimi, D.; Ghisa, M.; Zingone, F. Incidence comparison of adverse events in patients with inflammatory bowel disease receiving different biologic agents: Retrospective long-term evaluation. Intest. Res. 2022, 20, 114–123. [Google Scholar] [CrossRef]
- Harris, R.J.; McDonnell, M.; Young, D.; Bettey, M.; Downey, L.; Pigott, L.; Felwick, R.; Gwiggner, M.; Cummings, J.R.F. Early real-world effectiveness of ustekinumab for Crohn’s disease. Frontline Gastroenterol. 2020, 11, 111–116. [Google Scholar] [CrossRef]
- Kakkadasam Ramaswamy, P.; Moattar, H.; Sawyer, E.; Edwards, J.; Shukla, D. P697 Efficacy and safety of ustekinumab in Crohn’s disease: A real-world study from Australia. J. Crohn’s Colitis 2020, 14, S564–S565. [Google Scholar] [CrossRef]
- Kopylov, U.; Hanzel, J.; Liefferinckx, C.; De Marco, D.; Imperatore, N.; Plevris, N.; Baston-Rey, I.; Harris, R.J.; Truyens, M.; Domislovic, V.; et al. Effectiveness of ustekinumab dose escalation in Crohn’s disease patients with insufficient response to standard-dose subcutaneous maintenance therapy. Aliment. Pharmacol. Ther. 2020, 52, 135–142. [Google Scholar] [CrossRef]
- Lopez Tobaruela, J.M.; Sanchez-Capilla, A.D.; Ortega-Suazo, E.J.; Fernandez-Cano, M.C.; Herrador-Paredes, M.; Cabello-Tapia, M.J.; Martin-Rodriguez, M.M. P577 Ustekinumab in actual clinical practice: Our centre experience. J. Crohn’s Colitis 2020, 14, S485–S486. [Google Scholar] [CrossRef]
- Mohammad, D.; Alshahrani, A.; Bao, Y.; Alramdan, R.; Rajani, A.; Chauhan, U.; Salena, B.; Tse, F.; Greenwald, E.; Albashir, S.; et al. P484 Effectiveness and safety of ustekinumab in patients with Crohn’s disease: A real-world experience. J. Crohn’s Colitis 2020, 14, S426. [Google Scholar] [CrossRef]
- Monin, L.; Dubois, S.; Reenaers, C.; Van Kemseke, C.; Latour, P.; Van Daele, D.; Vieujean, S.; Seidel, L.; Louis, E. Ustekinumab in bio-naive and bio-failure Crohn’s disease patients: Results from a <<real-life>> monocentric cohort. Dig. Liver Dis. 2021, 53, 72–78. [Google Scholar] [CrossRef]
- Mozdiak, E.; Wicaksono, A.N.; Covington, J.A.; Arasaradnam, R.P. Colorectal cancer and adenoma screening using urinary volatile organic compound (VOC) detection: Early results from a single-centre bowel screening population (UK BCSP). Tech. Coloproctol. 2019, 23, 343–351. [Google Scholar] [CrossRef] [Green Version]
- Rayer, C.; Roblin, X.; Laharie, D.; Caron, B.; Flamant, M.; Dewitte, M.; Fumery, M.; Viennot, S.; Bourreille, A.; Pariente, B.; et al. P665 Which second-line biologic after anti-TNF failure during Crohn’s disease: Ustekinumab or vedolizumab, a multicentre retrospective study. J. Crohn’s Colitis 2020, 14, S547. [Google Scholar] [CrossRef]
- Parra, R.S.; Chebli, J.M.F.; Queiroz, N.S.F.; Damiao, A.; de Azevedo, M.F.C.; Chebli, L.A.; Bertges, E.R.; Alves Junior, A.J.T.; Ambrogini Junior, O.; da Silva, B.; et al. Long-term effectiveness and safety of ustekinumab in bio-naive and bio-experienced anti-tumor necrosis factor patients with Crohn’s disease: A real-world multicenter Brazilian study. BMC Gastroenterol. 2022, 22, 199. [Google Scholar] [CrossRef]
- Saldana Duenas, C.; Rullan Iriarte, M.; Elosua Gonzalez, A.; Rodriguez Gutierrez, C.; Rubio Iturria, S.; Nantes Castillejo, O. Ustekinumab in Crohn’s disease: Effectiveness and safety in clinical practice. Gastroenterol. Hepatol. 2020, 43, 497–505. [Google Scholar] [CrossRef]
- Sánchez Rodríguez, E.; Mesonero Gismero, F.; López Sanroman, A. P737 Ustekinumab induction effectiveness in Crohn’s disease in a real-life cohort. J. Crohn’s Colitis 2020, 14, S590–S591. [Google Scholar] [CrossRef]
- Shim, H.H.; Kong, S.C.; Ong, W.C.; Lim, T.G.; Chan, P.W. P381 Use of ustekinumab in Crohn’s disease: Singapore largest single-centre experience. J. Crohn’s Colitis 2020, 14, S357. [Google Scholar] [CrossRef]
- Duvnjak, M.; Bilic, A.; Barsic, N.; Tomasic, V.; Stojsavljevic, S. Classical medications in the treatment of inflammatory bowel diseases. Acta Med. Croat. 2013, 67, 111–124. [Google Scholar]
- Truyens, M.; Geldof, J.; Dewitte, G.; Glorieus, E.; Hindryckx, P.; Lobaton Ortega, T. P344 Effectiveness of ustekinumab in refractory Crohn’s disease: A real-life experience in a tertiary referral centre. J. Crohn’s Colitis 2020, 14, S330. [Google Scholar] [CrossRef]
- Bokemeyer, B.; Plachta-Danielzik, S.; Di Giuseppe, R.; Mohl, W.; Teich, N.; Hoffstadt, M.; Schweitzer, A.; von der Ohe, M.; Gauss, A.; Atreya, R.; et al. DOP47 Real World Evidence on the effectiveness of ustekinumab in Crohn’s Disease: Induction phase results from the prospective, observational RUN-CD Study. J. Crohn’s Colitis 2021, 15, S083–S084. [Google Scholar] [CrossRef]
- Casas Deza, D.; Lamuela Calvo, L.J.; Arbonés Mainar, J.M.; Ricart, E.; Gisbert, J.P.; Rivero Tirado, M.; Sanchez Rodríguez, E.; Sicilia, B.; Gutierrez Casbas, A.; Merino Ochoa, O.; et al. P262 Effectiveness and safety of ustekinumab in elderly patients: Real world evidence from ENEIDA registry. J. Crohn’s Colitis 2021, 15, S298–S299. [Google Scholar] [CrossRef]
- Cohen, A.; Ahmed, N.; Sant’Anna, A. Ustekinumab for the treatment of refractory pediatric Crohn’s disease: A single-center experience. Intest. Res. 2021, 19, 217–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forss, A.; Clements, M.; Myrelid, P.; Strid, H.; Soderman, C.; Wagner, A.; Andersson, D.; Hjelm, F.; The PROSE SWIBREG Study Group; Olen, O.; et al. Prospective observational study on Stelara (ustekinumab) assessing effectiveness in Crohn’s disease (PROSE): A 16-week follow-up. Scand. J. Gastroenterol. 2021, 56, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Garg, R.; Aggarwal, M.; Butler, R.; Achkar, J.P.; Lashner, B.; Philpott, J.; Cohen, B.; Qazi, T.; Rieder, F.; Regueiro, M.; et al. Real-World Effectiveness and Safety of Ustekinumab in Elderly Crohn’s Disease Patients. Dig. Dis. Sci. 2022, 67, 3138–3147. [Google Scholar] [CrossRef]
- Gonczi, L.; Szanto, K.; Farkas, K.; Molnar, T.; Szamosi, T.; Schafer, E.; Golovics, P.A.; Barkai, L.; Lontai, L.; Lovasz, B.; et al. Clinical efficacy, drug sustainability and serum drug levels in Crohn’s disease patients treated with ustekinumab—A prospective, multicenter cohort from Hungary. Dig. Liver Dis. 2022, 54, 207–213. [Google Scholar] [CrossRef]
- Kim, F.S.; Patel, P.V.; Stekol, E.; Ali, S.; Hamandi, H.; Heyman, M.B.; Verstraete, S.G. Experience Using Ustekinumab in Pediatric Patients with Medically Refractory Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 610–614. [Google Scholar] [CrossRef]
- Lorenzo Gonzalez, L.; Valdes Delgado, T.; Vazquez Moron, J.M.; Castro Laria, L.; Leo Carnerero, E.; Maldonado Perez, M.B.; Sanchez Capilla, D.; Pallares Manrique, H.; Saez Diaz, A.; Arguelles Arias, F.; et al. Ustekinumab in Crohn’s disease: Real-world outcomes and predictors of response. Rev. Esp. Enferm. Dig. 2022, 114, 272–279. [Google Scholar] [CrossRef]
- Manlay, L.; Boschetti, G.; Pereira, B.; Flourie, B.; Dapoigny, M.; Reymond, M.; Sollelis, E.; Gay, C.; Boube, M.; Buisson, A.; et al. Comparison of short- and long-term effectiveness between ustekinumab and vedolizumab in patients with Crohn’s disease refractory to anti-tumour necrosis factor therapy. Aliment. Pharmacol. Ther. 2021, 53, 1289–1299. [Google Scholar] [CrossRef]
- Miranda, A.; Gravina, A.G.; Cuomo, A.; Mucherino, C.; Sgambato, D.; Facchiano, A.; Granata, L.; Priadko, K.; Pellegrino, R.; de Filippo, F.R.; et al. Efficacy of ustekinumab in the treatment of patients with Crohn’s disease with failure to previous conventional or biologic therapy: A prospective observational real-life study. J. Physiol. Pharmacol. 2021, 72, 537–543. [Google Scholar] [CrossRef]
- Plevris, N.; Fulforth, J.; Siakavellas, S.; Robertson, A.; Hall, R.; Tyler, A.; Jenkinson, P.W.; Campbell, I.; Chuah, C.S.; Kane, C.; et al. Real-world effectiveness and safety of ustekinumab for the treatment of Crohn’s disease: The Scottish ustekinumab cohort. J. Gastroenterol. Hepatol. 2021, 36, 2067–2075. [Google Scholar] [CrossRef]
- Saiz Chumillas, R.M.; Alba Hernández, L.; Chivato Martín-Falquina, I.; Badia Aranda, E.; Arias García, M.L.; Sicilia Aladrén, B. P389 Efficacy and safety of ustekinumab in patients with Crohn’s disease refractory to anti-tumour necrosis factor: Real clinical practice. J. Crohn’s Colitis 2021, 15, S400–S401. [Google Scholar] [CrossRef]
- Scribano, M.L.; Aratari, A.; Neri, B.; Bezzio, C.; Balestrieri, P.; Baccolini, V.; Falasco, G.; Camastra, C.; Pantanella, P.; Monterubbianesi, R.; et al. Effectiveness of ustekinumab in patients with refractory Crohn’s disease: A multicentre real-life study in Italy. Ther. Adv. Gastroenterol. 2022, 15, 17562848211072412. [Google Scholar] [CrossRef]
- Sipponen, T.; Af Bjorkesten, C.G.; Hallinen, T.; Ilus, T.; Soini, E.; Eberl, A.; Heikura, M.; Kellokumpu, M.; Koskela, R.; Nielsen, C.; et al. A nationwide real-world study on dynamic ustekinumab dosing and concomitant medication use among Crohn’s disease patients in Finland. Scand. J. Gastroenterol. 2021, 56, 661–670. [Google Scholar] [CrossRef]
- Straatmijer, T.; Biemans, V.B.C.; Hoentjen, F.; de Boer, N.K.H.; Bodelier, A.G.L.; Dijkstra, G.; van Dop, W.A.; Haans, J.J.L.; Jansen, J.M.; Maljaars, P.W.J.; et al. Ustekinuma b for Crohn’s Disease: Two-Year Results of the Initiative on Crohn and Colitis (ICC) Registry, a Nationwide Prospective Observational Cohort Study. J. Crohn’s Colitis 2021, 15, 1920–1930. [Google Scholar] [CrossRef]
- Tursi, A.; Mocci, G.; Cuomo, A.; Allegretta, L.; Aragona, G.; Colucci, R.; Della Valle, N.; Ferronato, A.; Forti, G.; Gaiani, F.; et al. Real-life efficacy and safety of Ustekinumab as second- or third-line therapy in Crohn’s disease: Results from a large Italian cohort study. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2099–2108. [Google Scholar] [CrossRef]
- Viola, A.; Muscianisi, M.; Macaluso, F.S.; Ventimiglia, M.; Cappello, M.; Privitera, A.C.; Magnano, A.; Pluchino, D.; Magri, G.; Ferracane, C.; et al. Ustekinumab in Crohn’s disease: Real-world outcomes from the Sicilian network for inflammatory bowel diseases. JGH Open 2021, 5, 364–370. [Google Scholar] [CrossRef]
- Yokoyama, S.; Asano, T.; Nagano, K.; Tsuchiya, H.; Takagishi, M.; Tsujioka, S.; Miura, N.; Matsumoto, T. Safety and effectiveness of ustekinumab in Crohn’s disease: Interim results of post-marketing surveillance in Japan. J. Gastroenterol. Hepatol. 2021, 36, 3069–3076. [Google Scholar] [CrossRef]
- Chaparro, M.; Baston-Rey, I.; Fernandez-Salgado, E.; Gonzalez Garcia, J.; Ramos, L.; Diz-Lois Palomares, M.T.; Arguelles-Arias, F.; Iglesias Flores, E.; Cabello, M.; Rubio Iturria, S.; et al. Long-Term Real-World Effectiveness and Safety of Ustekinumab in Crohn’s Disease Patients: The SUSTAIN Study. Inflamm. Bowel Dis. 2022, izab357, Online ahead of print. [Google Scholar] [CrossRef]
- Lenti, M.V.; Dolby, V.; Clark, T.; Hall, V.; Tattersall, S.; Fairhurst, F.; Kenneth, C.; Walker, R.; Kemp, K.; Borg-Bartolo, S.; et al. A propensity score-matched, real-world comparison of ustekinumab vs. vedolizumab as a second-line treatment for Crohn’s disease. The Cross Pennine study II. Aliment. Pharmacol. Ther. 2022, 55, 856–866. [Google Scholar] [CrossRef]
- Macaluso, F.S.; Maida, M.; Ventimiglia, M.; Cottone, M.; Orlando, A. Effectiveness and safety of Ustekinumab for the treatment of Crohn’s disease in real-life experiences: A meta-analysis of observational studies. Expert Opin. Biol. Ther. 2020, 20, 193–203. [Google Scholar] [CrossRef]
- Rutgeerts, P.; Gasink, C.; Chan, D.; Lang, Y.; Pollack, P.; Colombel, J.F.; Wolf, D.C.; Jacobstein, D.; Johanns, J.; Szapary, P.; et al. Efficacy of Ustekinumab for Inducing Endoscopic Healing in Patients with Crohn’s Disease. Gastroenterology 2018, 155, 1045–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bermejo, F.; Jimenez, L.; Algaba, A.; Vela, M.; Bastida, G.; Merino, O.; Lopez-Garcia, A.; Melcarne, L.; Rodriguez-Lago, I.; de la Maza, S.; et al. Re-induction with Intravenous Ustekinumab in Patients with Crohn’s Disease and a Loss of Response to This Therapy. Inflamm. Bowel Dis. 2022, 28, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Rolston, V.S.; Kimmel, J.; Popov, V.; Bosworth, B.P.; Hudesman, D.; Malter, L.B.; Hong, S.; Chang, S. Ustekinumab Does Not Increase Risk of Adverse Events: A Meta-Analysis of Randomized Controlled Trials. Dig. Dis. Sci. 2021, 66, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Engel, T.; Yung, D.E.; Ma, C.; Pariente, B.; WIls, P.; Eliakim, R.; Ungar, B.; Ben-Horin, S.; Kopylov, U. Effectiveness and safety of Ustekinumab for Crohn’s disease; systematic review and pooled analysis of real-world evidence. Dig. Liver Dis. 2019, 51, 1232–1240. [Google Scholar] [CrossRef]
- Honap, S.; Meade, S.; Ibraheim, H.; Irving, P.M.; Jones, M.P.; Samaan, M.A. Effectiveness and Safety of Ustekinumab in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Dig. Dis. Sci. 2022, 67, 1018–1035. [Google Scholar] [CrossRef]

| Authors | Year | Abstract or Full Text | N | Design | Period | Median Follow-Up | Adult or Children | Dose UST (Induction ± Maintenance) | Prior IMM | Prior Biologic | Concomitant CE | Concomitant IMM | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥1 Biologic | Anti-TNF Failure | Anti-TNF + Vedolizumab Failure | ||||||||||||
| Kopylov [14] | 2014 | F | 38 | R | March 2011 to November 2013 | 32 w | Ad | sc + 90 mg sc q8w | 38/38 (100%) | 38/38 (100%) | 1 anti-TNF: 38/38 (100%) ≥2 anti-TNF: 36/38 (95%) | NR | 22/38 (57.8%) | 4/38 (10.6%) |
| Harris [15] | 2016 | F | 45 | R | June 2011 to June 2014 | 12 w | Ad | sc + 90 mg sc q8w | NR | 45/45 (100%) | 1 anti-TNF: 45/45 (100%) ≥2 anti-TNF: 44/45 (98%) | NR | 32/45 (71%) | 29/45 (65%) |
| Khorrami [16] | 2016 | F | 116 | R | March 2011 to December 2014 | 40 w | Ad | sc + 90 mg sc q8w | 116/116 (100%) | 116/116 (100%) | 1 anti-TNF 116/116 (100%) ≥2 anti-TNF: 101/116 (87.1%) | NR | 37/116 (31.9%) | 42/116 (36.2%) |
| Battat [17] | 2017 | F | 62 | P | April 2014 to September 2015 | NR | Ad | sc+ 90 mg sc q8w | NR | 61/62 (98.4%) | 1 anti-TNF: 61/62 (98.4%) | NR | 19/62 (30.7%) | Thiopurines: 10/62 (16.1%) Methotrexate: 6/62 (9.7%) |
| Greenup [18] | 2017 | F | 73 | R | May 2013 to November 2016 | NR | Ad | sc + 90 mg q8w | NR | 72/73 (99%) | 1 anti-TNF 72/73 (99%) ≥2 anti-TNF 9/73 (12.5%) | NR | 19/73 (26%) | 30/73 (42%) |
| Ma (a) [19] | 2017 | F | 167 | R | January 2011 to July 2016 | 45 w | Ad | sc/IV + 90 mg sc q8w | 126/167 (75.4%) | 159/167 (95.2%) | 1 anti-TNF: 117/167 (70.1%) ≥2 anti-TNF: 93/167 (55.7%) | 8/167 (4.8%) | 72/167 (43.1%) | 73/167 (43.7%) |
| Ma (b) [20] | 2017 | F | 104 | R | January 2011 to July 2016 | 57.2 w | Ad | 90 mg sc q8w-q12w-q6w | NR | 96/104 (92.3%) | 1 anti-TNF: 96/104 (92.3%) | NR | 40/104 (38.5%) | 44/104 (42.3%) |
| Wils [21] | 2018 | F | 88 | R | March 2011 to December 2014 | 106.4 w | Ad | 90 mg sc q8w-q12w | 86/88 (98%) | 88/88 (100%) | 1 anti-TNF: 88/88 (100%) ≥2 anti-TNF: 79/88 (90%) | 0/88 (0%) | 13/88 (15%) | 26/88 (30%) |
| Ahmed [22] | 2019 | F | 66 | R/P | 2014 to 2017 | 16 w | Ad | NR | Thiopurines: 23/66 (34.8%) Methotrexate: 7/66 (10.6%) | 56/66 (84.8%) | 1 anti-TNF: 56/66 (84.8%) | 19/66 (28.8%) | NR | NR |
| Calvo [23] | 2019 | A | 68 | R | April 2010 to April 2019 | 76 w | Ad | IV + 90 mg sc q8w-q12w | 61/68 (90%) | 68/68 (100%) | 1 anti-TNF: 67/68 (98%) ≥2 anti-TNF: 47/68 (69%) | 11/68 (16%) | 12/68 (18%) | 15/68 (22%) |
| Hernández Camba [24] | 2019 | A | 47 | R | June 2017 to June 2018 | NR | Ad | IV + 90 mg sc q12w | NR | 39/47 (82.6%) | NR | NR | NR | 43/47 (91%) |
| Hoffmann [25] | 2019 | F | 57 | R | December 2016 to March 2018 | 32 w | Ad | IV + 90 mg sc q8w-q12w | 47/57 (82.5%) | 54/57 (94.7%) | NR | NR | 20/57 (35.1%) | 3/57 (5.3%) |
| Iborra [26] | 2019 | F | 407 | R | Since June 2017 | NR | Ad | IV + 90 mg sc q4w-q8w-q12w | NR | 389/407 (96%) | 1 anti-TNF: 389/407 (96%) ≥2 anti-TNF: 248/407 (61%) | 88/407 (22%) | 135/407 (33.2%) | 147/407 (36.1%) |
| Kubesch [27] | 2019 | F | 106 | R | NR | 49.1 w | Ad | IV + 90 mg sc q8-q12w | 95/106 (89.6%) | 102/106 (96.2%) | 1 anti-TNF: 55/106 (51.9%) ≥2 anti-TNF: 46/106 (43.4%) | 36/106 (34.4%) | 38/106 (35.8%) | NR |
| Liefferinckx [28] | 2019 | F | 152 | R | September 2016 to August 2017 | NR | Ad | IV + 90 mg sc q8w | NR | 151/152 (99.3%) | 1 anti-TNF: 151/152 (99.3%) ≥2 anti-TNF: 124/152 (82%) | 106/152 (69.7%) | 68/152 (44.7%) | 25/152 (16.4%) |
| Lynn [29] | 2019 | A | 594 | R | NR | NR | Ad | NR | NR | 559/594 (94%) | 1 anti-TNF: 309/594 (52%) | 238/594 (40%) | NR | NR |
| Rajagopalan [30] | 2019 | A | 33 | R | May 2017 to January 2019 | 12 w (mean) | Ad | NR | NR | 31/33 (94%) | NR | NR | NR | NR |
| Saman [31] | 2019 | F | 41 | R | December 2016 to July 2018 | 32 w | Ad | IV + 90 mg sc q8w-q12w | 38/41 (92.7%) | 38/41 (92.7%) | 1 anti-TNF: 28/41 (68.3%) ≥2 anti-TNF: 10/41 (24.4%) | 10/41 (24.4%) | 15/41 (36.6%) | NR |
| Townsend [32] | 2020 | F | 45 | R | NR | NR | Ad | IV + 90 mg sc q8w | NR | 45/45 (100%) | 1 anti-TNF: 45/45 (100%) ≥2 anti-TNF: 12 (26.7%) | NR | 19/45 (42.2) | 16 (35.6) |
| Verstockt [33] | 2019 | F | 86 | P | September 2016 to January 2018 | 32 w | Ad | IV + 90 mg sc q8w | NR | 82/86 (95.3%) | 1 anti-TNF: 82 (95.3%) | 58/86 (67.4%) | 30/86 (34.9%) | 2/86 (2.4%) |
| af Björkesten [34] | 2020 | F | 155 | R | January 2017 to December 2018 | 56.8 w | Ad | IV + 90 mg sc q8w-q12w | 57/155 (36.8%) | 150/155 (96.8%) | NR | 61/155 (39.4%) | NR | NR |
| Alric [35] | 2020 | F | 107 | R | December 2016 to August 2018 | NR | Ad | IV + 90 mg sc q8w-q12w | Thiopurines: 94/107 (87.9%) Methotrexate: 35/107 (32.7%) | 83/107 (77.6%) | 1 anti-TNF: 83/107 (77.6%) ≥2 anti-TNF: 58/107 (54.2%) | NR | 30/107 (28%) | 21/107 (19.6%) |
| Bar-Gil Shitrit [36] | 2020 | F | 106 | P | NR | NR | Ad | IV + 90 mg sc q8w | 45/106 (41.7%) | 106/106 (100%) | NR | NR | NR | 29/106 (26.9%) |
| Bennett [37] | 2020 | F | 96 | R | September 2009 to November 2017 | 40.3 w (IV reinduction) 62.9w (sc reinduction) | Ad | sc/IV + 90 mg sc q8w | NR | 96/96 (100%) | 1 anti-TNF: 96/96 (100%) ≥2 anti-TNF: 58/96 (60%) | 31/96 (32%) | 33/96 (34.4%) | 43/96 (44.8%) |
| Biemans [38] | 2020 | F | 221 | P | December 2016 to January 2019 | 48 w | Ad * | IV + 90 mg sc q8w-q12w | 216/221 (97.7%) | 218/221 (98.6%) | 1 anti-TNF: 218/221 (98.6%) ≥2 anti-TNF: 162/221 (73.3%) | 102/221 [46.2] | 35/221 (15.8%) | 44/212 (19.9%) |
| Calvo [39] | 2020 | A | 28 | R | April 2017 to April 2019 | 76 w | Ad | IV + 90 mg sc q8w-q12w | NR | 28/28 (100%) | NR | NR | NR | NR |
| Casas [40] | 2020 | F | 69 | R | NR | 32 w | Ad | IV/sc + 90 mg sc q8w | NR | 69/69 (100%) | NR | 12/69 (17%) | 20/69 (29%) | 15/69 (22%) |
| Gadhok [41] | 2020 | A | 211 | NR | October 2016 to October 2018 | NR | Ad | IV + 90 mg sc q8w-q12w | NR | 207/211 (96%) | NR | NR | NR | 49/211 (23%) |
| Gubbiotti [42] | 2020 | A | 104 | NR | NR | 32 w | Ad | IV + 90 mg sc q8w-q12w | NR | 104/104 (100%) | NR | NR | 31/104 (29.7%) | NR |
| Harris [43] | 2020 | F | 84 | R | Up to December 2018 | 27,809 (treatment days) | Ad | IV + 90 mg sc q8w-q12w | NR | 82/84 (97.6%) | 1 anti-TNF: 81/84 (96.4%) | 35/84 (42%) | 6/84 (7.1%) | 38/84 (45.2%) |
| Kakkadasam [44] | 2020 | A | 76 | R | June 2017 to July 2019 | 61 w | Ad | IV + 90 mg sc q8w | NR | 50/76 (65.8%) | 1 anti-TNF: 49/76 (64.5%) | 10/76 (13.1%) | 38/76 (50%) | 32/76 (42.1%) |
| Kopylov [45] | 2020 | F | 142 | R | NR | 26 w | Ad | IV + 90 mg sc q8w | NR | 137/142 (96.5%) | NR | 57/142 (40%) | 34/142 (24%) | 24/142 (16.9%) |
| López- Tobaruela [46] | 2020 | A | 37 | R | NR | 50 w (mean) | Ad | NR | 35/37 (94.6%) | 35/37 (94.6%) | 1 anti-TNF: 35/37 (94.6%) ≥2 anti-TNF: 23/37 (65.7%) | 4/37 (10.8%) | 11/37 (29.7%) | 12/37 (32.4%) |
| Mohammad [47] | 2020 | A | 123 | R | January 2017 to August 2019 | NR | Ad | NR | NR | 98/123 (79.5%) | 1 anti-TNF: 98/123 (79.5%) | 21/123 (17.1%) | NR | NR |
| Monin [48] | 2020 | F | 156 | R | October 2016 to May 2020 | 60 w | Ad | IV + 90 mg sc q8w | 111/148 (75.5%) | 113/148 (76.4%) | NR | 110/148 (74.3%) | 51/148 (34.5%) | 20/148 (13.5%) |
| Mozdiak [49] | 2020 | A | 62 | R | NR | NR | Ad | IV + 90 mg sc q8w | NR | 60/62 (97%) | NR | NR | NR | 19/62 (30.6%) |
| Rayer [50] | 2020 | A | 61 | R | NR | 67 w (mean) | Ad | NR | NR | NR | NR | NR | NR | NR |
| Parra [51] | 2022 | F | 245 | R | November 2017 to November 2019 | up to 56 w | Ad | IV + 90 mg sc q8w | 50/204 (25%) | 212/245 (86.5%) | 1 anti-TNF:182/245 (74.3%) | NR | 135/245 (60.5%) | 54/245 (22.1%) |
| Saldaña [52] | 2020 | F | 61 | P | August 2017 to February 2019 | NR | Ad | IV + 90 mg sc q8w | NR | 61/61 (100%) | NR | 9/61 (48%) | 10/61 (16.4%) | 16/61 (26.2%) |
| Sánchez-Rodríguez [53] | 2020 | A | 25 | R | June 2017 to May 2019 | 53.3 w | Ad | IV + 90 mg sc q8w | 25/25 (100%) | 24/25 (96%) | NR | NR | NR | NR |
| Shim [54] | 2020 | A | 22 | NR | NR | NR | Both | NR | NR | 19/22 (86.4%) | NR | NR | 6/22 (27.3%) | 13/22 (59.1%) |
| Tomasic [55] | 2020 | A | 42 | R | January 2018 to April 2020 | 64 w | Ad | NR | NR | 0/42 (0%) | 0/42 (0%) | 0/42 (0%) | NR | NR |
| Truyens [56] | 2020 | A | 67 | R | December 2017 to August 2019 | 60 w | Ad | IV + 90 mg sc q8w | NR | 62/67 (92.5%) | NR | NR | 29/67 (43.3%) | 14/67 (20.9%) |
| Bokemeyer [57] | 2021 | A | 339 | P | January 2017 to December 2020 | NR | NR | NR | NR | 305/339 (90%) | NR | NR | NR | NR |
| Casas [58] | 2021 | A | 648 >60 y: 212 <60 y: 436 | R | NR | NR | NR | NR | NR | >65y: 180/212 (84.8%) <65y: 421/436 (96.7%) | NR | NR | >65y: 54/212 (25.5%) <65y: 127/436 (29.3%) | NR |
| Cohen [59] | 2021 | F | 11 | R | December 2015 to July 2018 | 24–88 w | C | sc/IV + 90 mg sc q8w | 10/11 (90.9%) | 11/11 (100%) | 1 anti-TNF: 11/11 (100%) ≥2 anti-TNF: 3/11 (27.3%) | NR | 4/11 (36.4%) | 4/11 (36.4%) |
| Forss [60] | 2021 | F | 114 | P | January 2017 to November 2018 | NR | Ad | IV + 90 mg sc q8w-q12w | NR | 107/112 (94%) | NR | NR | 21/114 (18%) | 26/114 (23%) |
| Garg [61] | 2021 | F | 117 >65 y: 39 <65 y: 78 | R | September 2016 to September 2019 | >65 y: 70 w (mean) <65 y: 70 w (mean) | Ad | IV + 90 mg sc q12w | >65y: 19/39 (48.7%) <65: 41/78 (52.6%) | >65y: 37/39 (94.9%) <65y: 77/78 (98.7%) | NR | >65y: 0/39 (0%) <65y: 7/78 (8.6%) | >65y: 20/39 (51.3%) <65y: 37/78 (47.4%) | >65y: 2/39 (5.1%) <65y: 11/78 (14.1%) |
| Gonczi [62] | 2021 | F | 142 | P | January 2019 to May 2020 | 60 w | Ad | IV + 90 mg sc q12w | 115/142 (80.9%) | 138/142 (97.2%) | 1 anti-TNF: 138/142 (97.2%) ≥2 anti-TNF: 90/142 (63.1%) | 36/142 (25.5%) | 48/142 (34%) | 29/142 (20.2%) |
| Kim [63] | 2021 | F | 38 | R | January 2016 to December 2019 | 62.1 w | C * | IV + 90 mg sc q8w | 17/38 (44.7%) | 38/38 (100%) | 1 anti-TNF: 38/38 (100%) ≥2 anti-TNF: 13/38 (34.2%) | 5/38 (13.2%) | 7/38 (18.4%) | NR |
| Lorenzo [64] | 2021 | F | 98 | R | July 2017 to December 2019 | 28 w (mean) | Ad | IV + 90 mg sc q8w | Thiopurines: 81/98 (91%) Methotrexate: 48/98 (49%) | 97/98 (99%) | NR | NR | 27/98 (27.5%) | Thiopurines: 13/98 (13.9%) Methotrexate: 2/98 (2.0%) |
| Manlay [65] | 2021 | F | 224 | R | July 2014 to May 2020 | 66 w (mean) | Ad | IV + 90 mg sc q8w | Thiopurines: 159/224 (70.9%) Methotrexate: 39/224 (17.4%) | 224/224 (100%) | NR | 54/224 (24.1%) | 59/224 (26.3%) | 32/224 (14.3%) |
| Miranda [66] | 2021 | F | 92 | P | NR | NR | Ad | IV + 90 mg sc q8w | NR | 85/92 (92.4%) | NR | 6/92 (6.5%) | NR | NR |
| Plevris [67] | 2021 | F | 216 | R | July 2017 to December 2019 | 35 w | Ad | IV + 90 mg sc q8w | NR | 213/216 (98.6%) | NR | NR | 88/216 (40.7%) | 55/216 (25.5%) |
| Saiz [68] | 2021 | A | 49 | R | January 2013 to March 2020 | 112 w | Ad | IV/sc + 90 mg sc q8w | NR | 49/49 (100%) | 1 anti-TNF: 49/49 (100%) ≥2 anti-TNF: 13/49 (27%) | NR | NR | 35/49 (71.4%) |
| Scribano [69] | 2021 | F | 140 | R | November 2018 to February 2020 | NR | Ad | IV + 90 mg sc q8w-q12w | NR | 140/140 (100%) | 1 anti-TNF: 140/140 (100%) ≥2 anti-TNF 38/140 (27.1%) | 28/140 (20%) | 22/140 (15.7%) | 12/140 (8.6%) |
| Sipponen [70] | 2021 | F | 155 | R | January 2017 to December 2018 | 62.8 w (mean, intensification) 50.8 w (mean, no intensif.) | Ad | IV + 90 mg sc q8w-q12w | NR | 150/155 (96.8%) | NR | NR | 64/155 (41.3%) | 51/155 (32.9%) |
| Straatmijer [71] | 2021 | F | 252 | P | NR | NR | Ad | IV + 90 mg sc q8w-q12w | NR | 50/252 (99.2%) | 1 anti-TNF: 250/252 (99.2%) ≥2 anti-TNF: 184/252 (73%) | 108/252 (42.9) | NR | NR |
| Tursi [72] | 2021 | F | 194 | R | Until December 2019 | 24 w (mean) | Ad | IV + 90 mg sc q8w | 121/194 (62.4%) | 147/194 (75.8%) | NR | 47/194 (24.2%) | 177/194 (91.2%) | NR |
| Viola [73] | 2021 | F | 131 | P | January 2019 to August 2019 | NR | Ad | IV + 90 mg sc q8w-q12w | NR | 130/131 (99%) | ≥2 anti-TNF: 38/131 (29%) | 46/131 (35%) | 56/131 (43%) | 14/131 (11%) |
| Yokoyama [74] | 2021 | F | 341 | P | May 2017 to June 2020 | NR | Ad * | IV + 90 mg sc q8w-q12w | 72/339 (24.8%) | 245/341 (72.3%) | NR | 1/341 (0.4%) | 104/339 (30.7%) | 68/339 (20.1%) |
| Chaparro [75] | 2022 | F | 463 | R | Before July 2018 | 62 w | Ad | IV + 90 mg sc q8-q12w | 162/463 (35%) | 447/463 (96.5%) | 1 anti-TNF: 374/463 (83.7%) | 109/463 (24.4%) | NR | 162/463 (35%) |
| Lenti [76] | 2022 | F | 259 | R | NR | NR | Ad | NR | NR | 209/259 (80.7%) | NR | 78/259 (30.1%) | NR | NR |
| Authors | Clinical Response | Clinical Remission | CE-Free Clinical Remission | Endoscopic Remission | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| w8–w14 | w24–w36 | w48–w52 | w52–w104 | w8–w14 | w24–w36 | w48–w52 | w52–w104 | w8–w14 | w24–w36 | w48–w52 | w52–w104 | w24–w36 | w48–w52 | |
| Kopylov [14] | 28/38 (73.7%) | 20/31 (64.5%) | 9/19 (47.4%) | NR | NR | NR | NR | NR | NR | NR | NR | NR | 2/13 (15.4%) | NR |
| Harris [15] | 17/37 (46%) | NR | NR | NR | 13/37 (35%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Khorrami [16] | 97/116 (73.6%) | 81/106 (76.4%) | 56/88 (63.6%) | NR | 33/116 (28.4%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Battat [17] | NR | 50/62 (80.7%) | NR | NR | NR | 41/62 (66.1%) | NR | NR | NR | 31/62 (50%) | NR | NR | 11/56 (19.6%) | NR |
| Greenup [18] | 38/68 (56%) | NR | 21/29 (72%) | NR | NR | NR | NR | NR | 9/19 (47%) | NR | NR | NR | NR | NR |
| Ma (a) [19] | 65/167 (38.9%) | NR | NR | NR | 25/167 (15%) | NR | NR | NR | NR | NR | 31/111 (27.9%) | NR | NR | 25/92 (27.2%) |
| Ma (b) [20] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 36/94 (38.3%) |
| Wils [21] | NR | NR | NR | 47/47 (100%) | NR | NR | 21/47 (45%) | NR | NR | NR | NR | NR | NR | NR |
| Ahmed [22] | 33/66 (50%) | NR | NR | NR | 18/65 (27.2%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Calvo [23] | 53/68 (78%) | 39/41 (95%) | 22/22 (100%) | NR | 31/68 (45%) | 21/41 (71%) | 18/22 (82%) | NR | NR | NR | NR | NR | NR | NR |
| Hernández-Camba [24] | NR | NR | NR | NR | 24/47 (51.6%) | NR | 20/47 (42%) | NR | 38/47 (80%) | NR | NR | NR | NR | NR |
| Hoffmann [25] | NR | NR | NR | NR | NR | NR | NR | NR | NR | 20/57 (35.1%) | NR | NR | 0/6 (0%) | 7/17 (41.1%) |
| Iborra [26] | NR | 218/295 (73.9%) | 225/295 (76.3%) | NR | NR | 169/295 (57.3%) | 190/295 (64.4%) | NR | NR | NR | 80/135 (59%) | NR | NR | 25/159 (15.7%) |
| Kubesch [27] | 51/93 (54.8%) | 37/93 (39.8%) | 48/93 (51.6%) | 23/93 (24.7%) | 24/93 (24.7%) | 19/93 (20.4%) | 25/93 (26.9%) | 16/93 (17.2%) | 18/93 (19.3%) | NR | 19/93 (20.4%) | NR | NR | NR |
| Liefferinckx [28] | 90/152 (59.2%) | 79/152 (51.9%) | 64/152 (42.1%) | NR | 44/152 (28.2%) | 47/152 (30.9%) | 39/152 (25.7%) | NR | 30/152 (19.7%) | 41/152 (26.9%) | 37/152 (24.3%) | NR | NR | NR |
| Lynn [29] | NR | NR | NR | NR | NR | 77/594 (13%) | 130/594 (22%) | NR | NR | NR | NR | NR | 101/594 (17%) | 202/594 (34%) |
| Rajagopalan [30] | NR | NR | NR | NR | 31/33 (96%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Saman [31] | NR | 24/41 (58.3%) | NR | NR | NR | 14/41 (34.1%) | NR | NR | NR | NR | NR | NR | NR | NR |
| Townsend [32] | 22/45 (48.9%) | 22/45 (48.9%) | 24/45 (53.3%) | NR | 16/45 (35.6%) | 18/45 (40%) | 19/45 (42.2%) | NR | 13/45 (28.9%) | 17/45 (37.8%) | 19/45 (42.2%) | NR | NR | NR |
| Verstockt [33] | NR | NR | NR | NR | 31/86 (36%) | 34/86 (39.5%) | NR | NR | 27/86 (31.4%) | 33/86 (38.4%) | NR | NR | 6/86 (7.1%) | NR |
| af Björkesten [34] | NR | NR | NR | NR | NR | 55/78 (70.5%) | 30/43 (69.8%) | NR | NR | NR | NR | NR | 6/17 (35.3%) | 6/18 (33.3%) |
| Alric [35] | NR | NR | NR | NR | 45/107 (42.3%) | NR | 58/107 (54.4%) | NR | 41/107 (38.2%) | NR | 48/107 (44.7%) | NR | NR | NR |
| Bar-Gil Shitrit [36] | NR | 55/106 (52%) | NR | NR | NR | 3/106 (31.1%) | NR | NR | NR | 4/37 (10.8%) | NR | NR | NR | NR |
| Bennett [37] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 13/51 (25%) | NR |
| Biemans [38] | 73/153 (47.7%) | 70/152 (46.1%) | 56/132 (42.4%) | NR | 47/153 (30.7%) | 61/152 (40.1%) | 52/132 (39.4%) | NR | 37/153 (24.2%) | 58/152 (38.2%) | 49/132 (37.1%) | NR | NR | NR |
| Calvo [39] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 18/28 (18%) |
| Casas [40] | NR | 62/69 (89.9%) | NR | NR | NR | NR | NR | NR | NR | 5/69 (7%) | NR | NR | NR | NR |
| Gadhok [41] | 97/211 (46.2%) | 67/211 (31.9%) | 53/211 (25.3%) | NR | 92/211 (43.5%) | 63/211 (29.7%) | 54/211 (25.7%) | NR | 85/211 (40.3%) | 59/211 (28.1%) | 54/211 (25.7%) | NR | NR | NR |
| Gubbiotti [42] | NR | NR | NR | NR | NR | 65/104 (62.3%) | NR | NR | NR | 53/104 (50.7%) | NR | NR | NR | NR |
| Harris [43] | NR | 38/72 (53%) | 35/49 (71%) | NR | NR | 6/72 (8%) | 7/49 (14%) | NR | NR | NR | 31/49 (65%) | NR | NR | NR |
| Kakkadasam [44] | NR | NR | NR | NR | NR | NR | NR | NR | NR | 35/76 (46%) | NR | NR | NR | NR |
| Kopylov [45] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| López-Tobaruela [46] | 12/29 (41.4%) | 12/24 (50%) | 11/18 (61.1%) | NR | 6/29 (20.7%) | 8/24 (33.3%) | 5/18 (27.8%) | NR | NR | NR | NR | NR | NR | NR |
| Mohammad [47] | NR | NR | 108/123 (88%) | NR | NR | NR | 43/123 (35%) | NR | NR | NR | NR | NR | NR | NR |
| Monin [48] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Mozdiak [49] | 43/62 (69%) | NR | NR | NR | NR | 32/62 (52%) | 43/62 (69%) | NR | NR | NR | NR | NR | NR | NR |
| Rayer [50] | 45/61 (74%) | NR | NR | NR | 20/61 (33%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Parra [51] | 189/239 (79.1%) | NR | NR | NR | 98/239 (41%) | 165/239 (68.9%) | 209/235 (87.3%) | NR | NR | NR | 80/135 (59.3%) | NR | NR | NR |
| Saldaña [52] | NR | 24/35 (69.9%) | 9/12 (75%) | NR | NR | 16/35 (45.7%) | 7/12 (58.3%) | NR | NR | 16/35 (45.7%) | 7/12 (58.3%) | NR | NR | NR |
| Sánchez-Rodríguez [53] | 20/25 (80%) | 20/24 (83.3%) | NR | NR | 10/25 (40%) | 9/24 (37.5%) | NR | NR | 6/25 (24%) | 7/24 (29.2%) | 16/18 (88.9%) | NR | NR | NR |
| Shim [54] | NR | NR | NR | NR | 5/22 (22.7%) | 9/18 (50%) | 5/9 (55.6%) | NR | NR | NR | NR | NR | NR | 2/5 (40%) |
| Tomasic [55] | NR | 35/42 (84%) | NR | 30/42 (71.4%) | NR | NR | NR | NR | NR | 16/42 (38.1%) | NR | 15/42 (35.7%) | NR | NR |
| Truyens [56] | 38/52 (73.1%) | 43/54 (79.6%) | 28/42 (66.7%) | NR | 4/52 (7.7%) | 11/54 (20.4%) | 14/42 (42.4%) | NR | NR | NR | NR | NR | 1/16 (6.3%) | 2/16 (12.5%) |
| Bokemeyer [57] | NR | NR | NR | NR | NR | 222/339 (65.5%) | NR | NR | NR | 181/339 (53.4%) | NR | NR | NR | NR |
| Casas (a) [58] | NR | 150/212 (70.5%) | 157/212 (74%) | NR | NR | NR | - | NR | NR | NR | NR | NR | NR | NR |
| Casas (b) [58] | NR | 334/436 (76.6%) | 327/436 (74.9%) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Cohen [59] | NR | NR | 5/11 (45.5%) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Forss [60] | NR | 38/96 (40%) | NR | NR | NR | 25/96 (26%) | NR | NR | NR | NR | NR | NR | NR | NR |
| Garg (a) [61] | NR | 18/39 (46.2%) | NR | NR | NR | 11/39 (28.2%) | NR | NR | NR | 6/20 (30%) | NR | NR | 18/71 (25.9%) | NR |
| Garg (b) [61] | NR | 18/78 (23.1%) | NR | NR | NR | 41/78 (52.6%) | NR | NR | NR | 20/37 (54.1%) | NR | NR | 21/71 (29.5%) | NR |
| Gonczi [62] | 107/137 (78.1%) | 106/136 (77.9%) | 84/122 (69%) | NR | 79/137 (57.7%) | 88/136 (64.7%) | 58/100 (58%) | NR | 56/128 (43.8%) | 76/132 (57.6%) | 47/92 (51.1%) | NR | NR | NR |
| Kim [63] | NR | NR | NR | NR | NR | 7/38 (18.4%) | NR | 23/38 (60.5%) | NR | NR | NR | NR | NR | NR |
| Lorenzo [64] | 58/84 (69%) | 50/61 (82%) | 32/43 (73.7%) | NR | 34/84 (40.8%) | 34/61 (56%) | 26/43 (60.5%) | NR | 27/84 (32.4%) | 27/61 (44%) | 20/43 (47.4%) | NR | NR | NR |
| Manlay [65] | NR | NR | NR | NR | NR | NR | NR | NR | 111/198 (56.1%) | 100/161 (62.1%) | 104/206 (50.6%) | NR | NR | NR |
| Miranda [66] | NR | NR | 38/75 (50,5%) | NR | NR | NR | 29/75 (39%) | NR | NR | NR | NR | NR | NR | 26/75 (34%) |
| Plevris [67] | 98/216 (45.4%) | NR | NR | NR | 13/216 (6%) | 15/108 (13.5%) | 13/41 (32%) | NR | NR | NR | NR | NR | 7/67 (10.8%) | 6/19 (32.7%) |
| Saiz [68] | NR | NR | 40/43 (93%) | 13/21 (62%) * | NR | NR | 37/43 (86%) | 11/21 (52%) * | NR | NR | NR | NR | NR | NR |
| Scribano [69] | NR | NR | NR | NR | NR | NR | NR | NR | NR | 85/140 (61%) | 46/140 (64.2%) | NR | NR | NR |
| Sipponen [70] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Straatmijer [71] | NR | NR | NR | NR | NR | NR | NR | NR | 81/251 (32.3%) | 104/251 (41.4%) | 97/249 (39%) | 84/247 (34%) | NR | NR |
| Tursi [72] | NR | NR | NR | NR | 146/194 (75.2%) | 135/194 (69.9%) | NR | NR | NR | 115/191 (59.3%) | NR | NR | 33/62 (53.2%) | NR |
| Viola [73] | 75/131 (68%) | 75/117 (64%) | 45/76 (59%) | NR | NR | 47/117 (40%) | 33/76 (43%) | NR | 46/131 (35%) | NR | 73/76 (96%) | NR | NR | NR |
| Yokoyama [74] | 115/130 (88.5%) | NR | NR | NR | 63/130 (48.5%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Chaparro [75] | 268/463 (58%) | 320/457 (70%) | NR | NR | 204/463 (44%) | 256/457 (56%) | NR | 113/272 (41.5%) | NR | 247/463 (53.3%) | 222/437 (50.8%) | 97/272 (35.7%) | NR | NR |
| Lenti [76] | 173/259 (66.8%) | NR | 97/259 (37.5%) | NR | 89/259 (34.4%) | NR | 63/259 (24.3%) | NR | NR | NR | NR | NR | NR | NR |
| Author | Loss of Response Rate (n/N, %) | Median Time to Loss of Response | Dose Optimisation (Dose Escalation and/or Intensification) ** | Time to Dose Optimisation (Median) | Effectiveness of Dose Optimisation |
|---|---|---|---|---|---|
| Kopylov [14] | NR | NR | Dose escalation: 18/38 (47.4%) | NR | 11/18 (61.1%) |
| Harris [15] | 2/45 (4.4%) | NR | NR | NR | NR |
| Khorrami [16] | 29/116 (25%) | NR | Intensification: 11/116 (9.5%) | NR | 8/11 (73%) |
| Greenup [18] | 12/42 (8.6%) | 88 w | Intensification: 16/62 (25.8%) | NR | 3/16 (19%) |
| Ma (a) [19] | 15/167 (9%) | 29.3 w | NR | NR | NR |
| Ma (b) [20] | 35/104 (33.7%) | 47.4 w | Dose optimisation: 24/104 (23%) * Dose escalation: 17/104 (16.3%) * IV reinduction + dose escalation: 7/104 (6.7%) | Dose escalation: 49.6 w IV reinduction + dose escalation: 84.3 w | Clinical response: * Dose escalation: 9/17 (52.9%) * IV reinduction + dose escalation: 4/7 (57.1%) |
| Wils [21] | 27/88 (30.7%) | NR | 32/88 (36.4%) | 106.4 w | 18/36 (56%) |
| Calvo [23] | 6/68 (8.8%) | 20 w | Intensification: 8/68 (15%) | 52 w | Clinical response: 4/8 (50%) Clinical remission: 1/8 (13%) |
| Hernández-Camba [24] | 14/47 (30%) | 26.8 w (mean) | Dose escalation: 38/47 (80%) | NR | NR |
| Hoffmann [25] | 5/48 (10.4%) | 24 w | NR | NR | NR |
| Iborra [26] | 49/407 (12%) | NR | Dose optimisation: 114/407 (28%) * Dose escalation: 12/407 (2.9%) * Intensification: 102/407 (25.1%) | NR | NR |
| Kubesch [27] | 8/106 (7.5%) | NR | Intensification: 4/106 (3.8%) | NR | NR |
| Liefferinckx [28] | 41/152 (27%) | NR | Intensification: 10/152 (6.6%) | NR | 10/10 (100%) |
| Rajagopalan [30] | 8/33 (24.2%) * | 52 w | NR | NR | NR |
| Saman [31] | 3/41 (7.3%) | NR | NR | NR | NR |
| Verstockt [33] | 31/86 (36%) | 24 w | NR | NR | NR |
| Af Björkesten [34] | 17/155 (11%) | 104 w | NR | NR | NR |
| Alric [35] | NR | NR | Intensification: 32/107 (30.1%) | 58w | NR |
| Bar-Gil Shitrit [36] | 7/106 (6.6%) | 24 w | NR | NR | NR |
| Bennett [37] | 23/96 (16.7%) | 20.6 w | Intensification: 34/96 (35.4%) | NR | Endoscopic response: 7/14 (50%). Endoscopic remission: 5/14 (35.7%). |
| Biemans [38] | 59/221 (26.7%) | 24.6 w | Dose optimisation: 38/221 (17.2%) * Dose escalation: 31/221 (14%) * Intensification: 7/221 (3.2%) | 48 w | CE free clinical remission * Dose escalation: 17/31 (54.8%) Clinical remission: * Intensification: 3/7 (42.9%) |
| Casas [40] | NR | NR | Intensification: 10/69 (14%) | NR | NR |
| Gadhok [41] | 10/211 (4.7%) | NR | NR | NR | NR |
| Gubbiotti [42] | NR | NR | Dose escalation: 84/104 (80.9%) | 32 w | NR |
| Harris [43] | 7/84 (8.3%) | 36.6 w | Intensification: 8/84 (9.5%) | NR | 1/8 (12.5%) |
| Kakkadasam [44] | 7/84 (8.3%) | 36.6 w | 22/76 (29%) | 52.5 w | NR |
| Kopylov [45] | 31/98 (31.6%) | 26 w | Intensification: * q8w-q4w: 91/142 (64.1%) * q8w-q6w: 20/142 (14.1%) * IV reinduction: 14/142 (12%) * IV reinduction + interval shortening: 17/142 (12%) | 29 w (mean) | Clinical response w16 from dose optimisation: 73/142 (51.4%) Clinical remission w16 from dose optimisation: 55/142 (38.7%) CE free clinical remission w16 from dose optimisation: 6/34 (17.6%) Endoscopic response 24w from dose optimisation: 10/23 (43.4%) Mucosal healing 24w from dose optimisation: 2/23 (8.6%) Clinical response w52 from dose optimisation: 51/98 (52%) Clinical remission w52 from dose optimisation: 41/98 (42%) CE free clinical remission w52 from dose optimisation: 9/34 (26.5%) |
| López-Tobaruela [46] | NR | NR | Intensification: 11/37 (29.7%) * q6w/q4w: 7/37 (18.9%) * IV reinduction: 4/37 (10.8%) | NR | NR |
| Monin [48] | 17/118 (14.4%) | 59.6 w | Intensification: 17/118 (14.4%) | NR | NR |
| Parra [51] | 17/39 (43.6%) | NR | Intensification: * q8w-q4w: 8/245 (3.2%) | NR | 4/8 (50%) |
| Saldaña [52] | 11/35 (31.4%) 3/12 (25%) | 24 w 52 w | Intensification: 6/35 (17%) *q8w-q4w: 4/35 (11.3%) * q8w-q6w: 2/35 (5.7%) | 24 w | NR |
| Sánchez-Rodríguez [53] | 0/25 (0%) | NR | NR | NR | NR |
| Tomasic [55] | 5/42 (11.9%) | 64 w (mean) | 13/42 (31%) | NR | NR |
| Truyens [56] | 3/67 (4.5%) | 27.5 w | Intensification: 29/67 (43.3%) * IV reinduction: 2/67 (3%) * Shortening dosage interval: 16/67 (23.9%) * IV reinduction + shortening interval: 11/67 (16.4%) | NR | Clinical response: 15/22 (68.2%) Clinical remission: 5/22 (22.7%) |
| Cohen [59] | 6/11 (54.5%) | 2–24 m | Intensification: 9/11 (81.8%) | 8–52 w | Clinical remission: 3/9 (33.3%) |
| Forss [60] | 6/114 (5.3%) | 16 w | NR | NR | NR |
| Garg [61] | (a) Elderly patients: 3/39 (7.7%) (b) Young patients: 9/78 (11.5%) | NR | Dose escalation: (a) Elderly patients: 7/39 (17.9%) (b) Young patients: 20/78 (25.6%) | NR | NR |
| Gonczi [62] | 14/142 (9.9%) | 60 w | Dose optimisation: 77/142 (54.2%) Dose escalation: 61/142 (43%) Intensification: 16/142 (11.2%) | NR | NR |
| Kim [63] | 5/38 (13.2%) | 62.1 w | Intensification: 18/38 (47.4%): * q8w-q4w: 15/38 (39.5%) * q8w-q6w: 1/38 (2.6%) * IV reinduction: 2/38 (5.3%) | NR | Clinical remission: 11/18 (61.1%) |
| Lorenzo [64] | 12/98 (12.2%) | 36 w (mean) | NR | NR | NR |
| Manlay [65] | NR | NR | Intensification: 96/224 (42.9%) | NR | NR |
| Plevris [67] | NR | NR | Dose optimisation: 30/216 (13.9%) * Dose escalation: 11/216 (5.1%) * Intensification q8w-q6w: 4/216 (1.9%) * Intensification q8w-q4w: 15/216 (6.9%) | NR | NR |
| Saiz [68] | 7/49 (14.3%) | NR | 16/49 (33%) | NR | NR |
| Sipponen [70] | 15/155 (9.7%) | 16 w | 47/140: 33.6% * Dose escalation: 22/140 (15.7%) * Intensification: 25/140 (17.9%) | NR | 41/47 (87.2%) |
| Straatmijer [71] | 167/251 (66.7%) | 52 w | NR | NR | NR |
| Tursi [72] | NR | NR | Intensification: 1/194 (0.5%) | NR | NR |
| Viola [73] | 13/131 (9.9%) | 52 w | NR | NR | NR |
| Chaparro [75] | 13/456 (12.7%) | 60 w | Dose optimisation: 121/463 (26.1%) * Dose escalation: 21/463 (4.5%) * Intensification: 100/463 (21.6%) | NR | Clinical remission: 63/80 (78.8%) * Dose escalation: 16/20 (80%) * Intensification (q8w-q4w): 42/54 (77.8%) * IV reinduction: 5/6 (83.3%) |
| Lenti [76] | 65/259 (25%) | NR | NR | NR | NR |
| Authors | AEs | Patients with AEs | AEs Requiring Ustekinumab Discontinuation | SAEs | Infections | Arthralgia or Myalgia | Skin Reactions | Infusion or Allergic Reaction | Headache | Malignancy | Others |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kopylov [14] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Harris [15] | 5/45 (11.1%) | 5/45 (11.1%) | NR | NR | 4/45 (8.9%) | 0 | 1/45 (2.2%) | 0 | 0 | 0 | 0 |
| Khorrami [16] | 14/116 (12.1%) | 11/116 (9.5%) | 0/116 (0%) | 0/116 (0%) | 3/116 (2.6%) | 1/116 (0.8%) | 1/116 (0.8%) | 0/116 (0%) | 2/116 (1.7%) | 0/116 (0%) | 4/116 (3.4%) |
| Battat [17] | 43/62 (69.4%) | 43/62 (69.4%) | 2/62 (3.2%) | 2/62 (3.2%) | 3/62 (4.8%) | 8/62 (12.9%) | 5/62 (8.1%) | 0/62 (0%) | 14/62 (22.5%) | 2/62 (3.2%) | 11/62 (17.7%) |
| Greenup [18] | 18/73 (24.7%) | 18/73 (24.7%) | NR | NR | 4/73 (5.5%) | 6/73 (8.2%) | 2/73 (2.7%) | 1/73 (1.4%) | 4/73 (5.5%) | 0/73 (0%) | 1/73 (1.4%) |
| Ma (a) [19] | 61/167 (36.5%) | 53/167 (31.1%) | 11/167 (6.6%) | 11/167 (6.6%) | 20/167 (12%) | 19/167 (11.4%) | 3/167 (1.8%) | 11/167 (6.6%) | 6/167 (3.6%) | 0/67 (0%) | 2/167 (1.2%) |
| Ma (b) [20] | 34/104 (32.7%) | 34/104 (32.7%) | 1/104 (1%) | NR | 12/104 (11.5%) | 13/104 (12.5%) | NR | NR | NR | NR | 1/104 (1%) |
| Wils [21] | NR | NR | 5/88 (5.7%) | 1/88 (1.1%) | 2/88 (2.2%) | 1/88 (1.1%) | 1/88 (1.1%) | NR | NR | 1/88 (1.1%) | NR |
| Ahmed [22] | NR | NR | NR | NR | NR | NR | NR | NR | _ | NR | NR |
| Calvo [23] | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) | 0/68 (0%) |
| Hernández-Camba [24] | 1/47 (2.1%) | 1/47 (2.1%) | NR | NR | 1/47 (2.1%) | 0/47 (0%) | 0/47 (0%) | 0/47 (0%) | 0/47 (0%) | 0/47 (0%) | 0/47 (0%) |
| Hoffmann [25] | 140/57 (245.6%) | 140/57 (245.6%) | NR | NR | 24/57 (42.1%) | 24/57 (42.1%) | 18/57 (31.6%) | 0/57 (0%) | 11/57 (19.3%) | 0/57 (0%) | 63/57 (110.5%) |
| Iborra [26] | 71/407 (17.4%) | 60/407 (14.7%) | NR | NR | 40/407 (9.8%) | 5/407 (1.2%) | 5/407 (1.2%) | 0/407 (0%) | 2/407 (0.5%) | 1/407 (0.25%) | 18/407 (4.4%) |
| Kubesch [27] | 3/106 (2.8%) | 3/106 (2.8%) | 0/106 (0%) | 0/106 (0%) | 2/106 (1.9%) | 0/106 (0%) | 0/106 (0%) | 0/106 (0%) | 0/106 (0%) | 0/106 (0%) | 1/106 (0.9%) |
| Liefferinckx [28] | 11/152 (7.2%) | 11/152 (7.2%) | 1/152 (0.7%) | 6/152 (3.9%) | 2/152 (1.3%) | 0/152 (0%) | 1/152 (0.7%) | 0/152 (0%) | 0/152 (0%) | 2/152 (1.3%) | |
| Lynn [29] | 56/594 (9.4%) | 56/594 (9.4%) | NR | NR | 51/594 (8.6%) | NR | NR | NR | NR | NR | 5/594 (0.8%) |
| Rajagopalan [30] | 3/33 (9%) | 3/33 (9%) | NR | NR | 1/33 (3%) | 2/33 (6%) | 0/33 (0%) | 0/33 (0%) | 0/33 (0%) | 0/33 (0%) | 0/33 (0%) |
| Saman [31] | 2/41 (4.8%) | 2/41 (4.8%) | 2/41 (4.8%) | 0/41 (0%) | 0/41 (0%) | 1/41 (2.4%) | 1/41 (2.4%) | 0/41 (0%) | 0/41 (0%) | 0/41 (0%) | 0/41 (0%) |
| Townsend [32] | NR | NR | 7/45 (15.6%) | NR | NR | NR | NR | NR | NR | NR | NR |
| Verstockt [33] | 12/86 (14%) | 12/86 (14%) | 5/86 (5.8%) | NR | 6/86 (7%) | 2/86 (2.4%) | 1/86 (1.2%) | 0/86 (0%) | 0/86 (0%) | 0/86 (0%) | 3/86 (3.5%) |
| af Björkesten [34] | 5/155 (3.2%) | NR | 5/155 (3.2%) | NR | 3/155 (1.9%) | 0/155 (0%) | 0/155 (0%) | 0/155 (0%) | 0/155 (0%) | 1/155 (0.6%) | 1/155 (0.6%) |
| Alric [35] | 25/107 (23.4%) | 21/107 (19.6%) | 1/107 (0.9%) | NR | 12/107 (11.2%) | 1/107 (0.9%) | 6/107 (5.6%) | 0/107 (0%) | 1/107 (0.9%) | 1/107 (0.9%) | 4/107 (3.7%) |
| Bar-Gil Shitrit [36] | 15/106 (14.2%) | 15/106 (14.2%) | 3/106 (2.8%) | 0/106 (0%) | 0/106 (0%) | 4/106 (3.6%) | 3/106 (2.8%) | 0/106 (0%) | 1/106 (0.9%) | 0/106 (0%) | 7/106 (6.6%) |
| Bennett [37] | 5/96 (5.2%) | 5/96 (5.2%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Biemans [38] | 110/221 (49.8%) | 110/221(49.8%) | 8/221 (3.6%) | NR | 70/221 (31.7%): | 5/221 (2.3%) | 13/221 (5.9%) | 1/221 (0.4%) | 7/221 (3.2%) | 0/221 (0%) | 14/221 (6.3%) |
| Calvo [39] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Casas [40] | 4/69 (5.8%) | 4/69 (5.8%) | 0/69 (0%) | 0/69 (0%) | 0/69 (0%) | 1/69 (1.4%) | 2/69 (2.9%) | 0/69 (0%) | 0/69 (0%) | 0/69 (0%) | 1/69 (1.4%) |
| Gadhok [41] | 27/211 (12.8%) | 27/211 (12.8%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Gubbiotti [42] | 3/104 (2.9%) | 3/104 (2.9%) | 2/104 (1.9%) | NR | NR | NR | NR | NR | NR | NR | NR |
| Harris [43] | 21/84 (25%) | 21/84 (25%) | 3/84 (3.6%) | 20/84 (23.8%) | 4/84 (4.8%) | 0/84 (0%) | 1/84 (1.2%) | 0/84 (0%) | 0/84 (0%) | 0/84 (0%) | 16/84 (19%) |
| Kakkadasam [44] | 1/76 (1.3%) | 1/76 (1.3%) | 1/76 (1.3%) | 0/76 (0%) | 0/76 (0%) | 1/76 (1.3%) | 0/76 (0%) | 0/76 (0%) | 0/76 (0%) | 0/76 (0%) | 0/76 (0%) |
| Kopylov [45] | 11/142 (7.7%) | 11/142 (7.7%) | 1/142 (0.7%) | 1/142 (0.7%) | 5/142 (3.5%) | 0/142 (0%) | 2/142 (1.4%) | 0/142 (0%) | 0/142 (0%) | 2 (1.4%) | 2 (1.4%) |
| López-Tobaruela [46] | 3/37 (8.1%) | 3/37 (8.1%) | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Mohammad [47] | 16/123 (13%) | 16/123 (13%) | NR | NR | 13/123 (1%) | NR | NR | NR | NR | NR | NR |
| Monin [48] | 26/156 (17.1%) | 26/156 (17.1%) | 9/156 (5.8%) | 7/156 (4.6%) | 26/156 (17.1%) | NR | NR | NR | NR | NR | NR |
| Mozdiak [49] | 8/62 (13%) | 8/62 (13%) | NR | 3/62 (4.8%) | NR | NR | NR | NR | NR | NR | NR |
| Rayer [50] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Parra [51] | 60/245 (24.5%) | 48/245 (19.6%) | 8/245 (3.2%) | 8/245 (3.2%) | 14/245 (5.7%) | 2/245 (0.8%) | 9/245 (3.7%) | NR | 3/245 (1.2%) | 0/245 (0%) | NR |
| Saldaña [52] | NR | NR | 2/61 (3.3%) | 11/61 (18%) | 1/61 (1.6%) | NR | NR | NR | NR | NR | 10/61 (16.4%) |
| Sánchez-Rodríguez [53] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Shim [54] | NR | NR | NR | NR | NR | NR | NR | 0/22 (0%) | NR | 0/22 (0%) | NR |
| Tomasic [55] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Truyens [56] | 2/67 (3%) | 2/67 (3%) | 2/67 (3%) | NR | 0/67 (0%) | 0/67 (0%) | 0/67 (0%) | 0/67 (0%) | 0/67 (0%) | 1/67 (1.5%) | 1/67 (1.5%) |
| Bokemeyer [57] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Casas [58] | 79/648 (12.2%) * Elderly: 30/212 (14.2%) * Young: 49/436 (11.2%) | 79/648 (12.2%) | 47/648 (7.3%) | NR | NR | NR | NR | NR | NR | * Elderly: 9/212 (4.3%) * Young: 3/436 (0.69%) | NR |
| Cohen [59] | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) |
| Forss [60] | NR | NR | NR | 0/114 (0%) | NR | NR | NR | NR | NR | NR | NR |
| Garg [61] | 14/117 (12%) * Elderly: 3/39 (7.7%) * Young: 11/78 (14.1%) | 14/117 (12%) | 3/117 (2.6%) | NR | 8/117 (6.8%) * Elderly: 2/39 (5.2%) * Young: 6/78 (7.7%) | 0/117 (0%) | 0/117 (0%) | 6/117 (5.1%) * Elderly: 1/39 (2.5%) * Young: 5/78 (6.4%) | 0/117 (0%) | 0/117 (0%) | 0/117 (0%) |
| Gonczi [62] | 5/142 (3.5%) | 5/142 (3.5%) | 2/142 (1.4%) | 0/142 (0%) | 0/142 (0%) | 1/142 (0.7%) | 4/142 (2.8%) | 0/142 (0%) | 0/142 (0%) | 0/142 (0%) | 0/142 (0%) |
| Kim [63] | 4/38 (10.5%): | 4/38 (10.5%): | 0/38 (0%) | 1/38 (2.6%) | 3/38 (7.9%) | 0/38 (0%) | 0/38 (0%) | 1/38 (2.6%) | 0/38 (0%) | 0/38 (0%) | 0/38 (0%) |
| Lorenzo [64] | 4/98 (4%): | 4/98 (4%): | 0/98 (0%) | 0/98 (0%) | 1/98 (1%) | 0/98 (0%) | 1/98 (1%) | 1/98 (1%) | 0/98 (0%) | 0/98 (0%) | 1/98 (1%) |
| Manlay [65] | NR | NR | 11/224 (4.9%) | NR | NR | NR | NR | NR | NR | NR | NR |
| Miranda [66] | NR | NR | NR | 0/92 (0%) | NR | NR | NR | NR | NR | NR | NR |
| Plevris [67] | NR | NR | NR | 19/216 (8.8%) | NR | NR | NR | NR | NR | NR | NR |
| Saiz [68] | NR | NR | NR | 0/49 (0%) | NR | NR | NR | NR | NR | NR | NR |
| Scribano [69] | 10/140 (7.1%) | 9/140 (6.4%) | 3/140 (2.1%) | NR | 0/140 (0%) | 1/140 (0.7%) | 3/140 (2.1%) | 2/140 (1.4%) | 1/140 (0.7%) | 0/140 (0%) | 3/140 (2.1%) |
| Sipponen [70] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Straatmijer [71] | NR | NR | 8/252 (3.2%) | NR | NR | NR | NR | NR | NR | 2/252 (7.9%) | NR |
| Tursi [72] | 5/194 (2.6%) | 5/194 (2.6%) | 4/194 (2%) | 0/194 (0%) | 1/194 (0.5%) | 2/194 (1%) | 0/194 (0%) | 1/194 (0.5%) | 0/194 (0%) | 0/194 (0%) | 1/194 (0.5%) |
| Viola [73] | 21/131 (16%) | 21/131 (16%) | 3/131 (2.1%) | 0/131 (0%) | 4/131 (3%) | 1/131 (0.7%) | 2/131 (1.4%) | 0/131 (0%) | 0/131 (0%) | 0/131 (0%) | 14/131 (10.7%) |
| Yokoyama [74] | 24/339 (7.1%) | 18/339 (5.3%) | NR | 7/339 (2.1%) | NR | NR | NR | NR | NR | NR | NR |
| Chaparro [75] | 50/463 (10.8%) | 39/463 (8.4%) | 4/463 (0.9%) | 4/463 (0.9%) | 5/463 (1.1%) | 5/463 (1.1%) | 9/463 (1.9%) | 38/463 (8.2%) | 7/463 (1.5%) | 1/463 (0.2%) | 13/463 (2.8%) |
| Lenti [76] | 130/256 (50.2%) | 130/256 (50.2%) | NR | 103 (40.2%) | NR | 8/256 (3.1%) | 6/256 (2.3%) | NR | 8/256 (3.1%) | 3/256 (1.1%) | 5/256 (1.9%) |
| Authors | Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of The Exposed Cohort | Selection of the Non-Exposed Cohort? | Ascertainment of Exposure | Demonstration that Outcome of Interest Was Not Present at the Start of the Study? | Comparability of Cohorts on the Basis of the Design or Analysis | Assessment of Outcome? | Was Follow-Up Long Enough for Outcome to Occur? | Adequacy of Follow-Up of Cohorts? | Overall Quality Score (Max. = 9) | |
| Kopylov [14] | * | * | * | * | * | 5 | |||
| Harris [15] | * | * | * | * | * | * | 6 | ||
| Khorrami [16] | * | * | * | * | * | * | 6 | ||
| Battat [17] | * | * | * | * | * | 5 | |||
| Greenup [18] | * | * | * | * | * | * | 6 | ||
| Ma (a) [19] | * | * | * | * | * | * | 6 | ||
| Ma (b) [20] | * | * | * | * | * | * | 6 | ||
| Wils [21] | * | * | * | * | * | * | 6 | ||
| Ahmed [22] | * | * | * | * | * | * | * | * | 8 |
| Hoffmann [25] | * | * | * | * | * | * | 6 | ||
| Iborra [26] | * | * | * | * | * | * | 6 | ||
| Kubesch [27] | * | * | * | * | * | 5 | |||
| Liefferinckx [28] | * | * | * | * | * | * | 6 | ||
| Saman [31] | * | * | * | * | * | * | 6 | ||
| Townsend [32] | * | * | * | * | ** | * | * | * | 9 |
| Verstockt [33] | * | * | * | * | * | * | 6 | ||
| af Björkesten [34] | * | * | * | * | * | * | 6 | ||
| Alric [35] | * | * | * | * | ** | * | * | * | 9 |
| Bar-Gil Shitrit [36] | * | * | * | * | * | * | 6 | ||
| Bennett [37] | * | * | * | * | * | * | 6 | ||
| Biemans [38] | * | * | * | * | * | 5 | |||
| Casas [40] | * | * | * | * | * | 5 | |||
| Harris [43] | * | * | * | * | * | * | 6 | ||
| Kopylov [45] | * | * | * | * | * | 5 | |||
| Monin [48] | * | * | * | * | * | * | 6 | ||
| Parra [51] | * | * | * | * | * | * | 6 | ||
| Saldaña [52] | * | * | * | * | * | * | 6 | ||
| Cohen [59] | * | * | * | * | * | * | 6 | ||
| Forss [60] | * | * | * | * | * | * | 6 | ||
| Garg [61] | * | * | * | * | * | * | * | * | 8 |
| Gonczi [62] | * | * | * | * | * | * | 6 | ||
| Kim [63] | * | * | * | * | * | * | 6 | ||
| Lorenzo [64] | * | * | * | * | * | 5 | |||
| Manlay [65] | * | * | * | * | * | * | * | * | 8 |
| Miranda [66] | * | * | * | * | * | 5 | |||
| Plevris [67] | * | * | * | * | * | * | 6 | ||
| Scribano [69] | * | * | * | * | * | * | 6 | ||
| Sipponen [70] | * | * | * | * | * | * | 6 | ||
| Straatmijer [71] | * | * | * | * | * | 5 | |||
| Tursi [72] | * | * | * | * | * | * | 6 | ||
| Viola [73] | * | * | * | * | * | 5 | |||
| Yokoyama [74] | * | * | * | * | * | 6 | |||
| Chaparro [75] | * | * | * | * | * | * | 6 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubín de Célix, C.; Chaparro, M.; Gisbert, J.P. Real-World Evidence of the Effectiveness and Safety of Ustekinumab for the Treatment of Crohn’s Disease: Systematic Review and Meta-Analysis of Observational Studies. J. Clin. Med. 2022, 11, 4202. https://doi.org/10.3390/jcm11144202
Rubín de Célix C, Chaparro M, Gisbert JP. Real-World Evidence of the Effectiveness and Safety of Ustekinumab for the Treatment of Crohn’s Disease: Systematic Review and Meta-Analysis of Observational Studies. Journal of Clinical Medicine. 2022; 11(14):4202. https://doi.org/10.3390/jcm11144202
Chicago/Turabian StyleRubín de Célix, Cristina, María Chaparro, and Javier P. Gisbert. 2022. "Real-World Evidence of the Effectiveness and Safety of Ustekinumab for the Treatment of Crohn’s Disease: Systematic Review and Meta-Analysis of Observational Studies" Journal of Clinical Medicine 11, no. 14: 4202. https://doi.org/10.3390/jcm11144202
APA StyleRubín de Célix, C., Chaparro, M., & Gisbert, J. P. (2022). Real-World Evidence of the Effectiveness and Safety of Ustekinumab for the Treatment of Crohn’s Disease: Systematic Review and Meta-Analysis of Observational Studies. Journal of Clinical Medicine, 11(14), 4202. https://doi.org/10.3390/jcm11144202






