Maternal Immune Cell and Cytokine Profiles to Predict Cardiovascular Risk Six Months after Preeclampsia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Participants
2.3. Data Collection
2.4. Sample Collection and Processing
2.5. Cytokine Quantification
2.6. Immunophenotyping
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
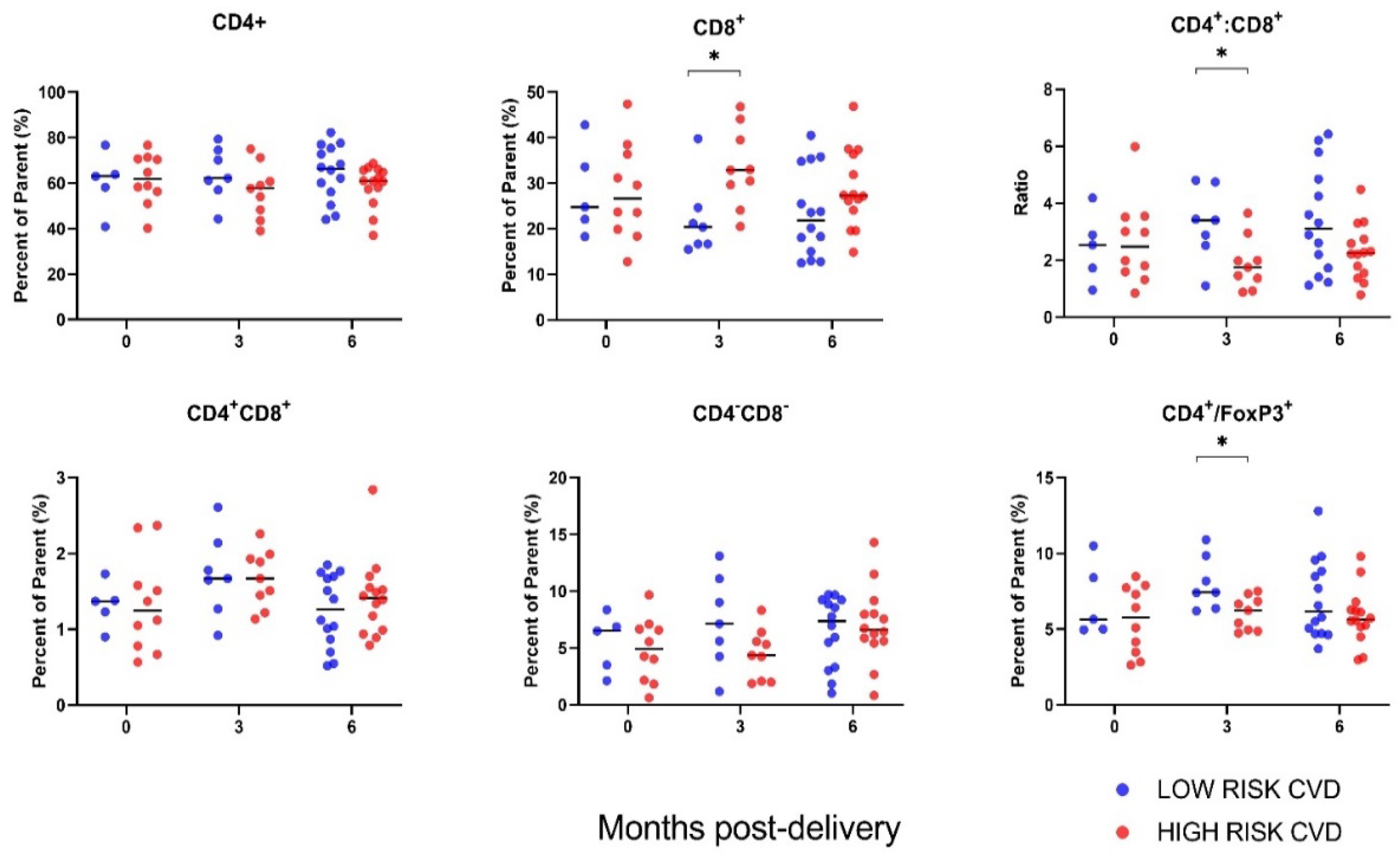
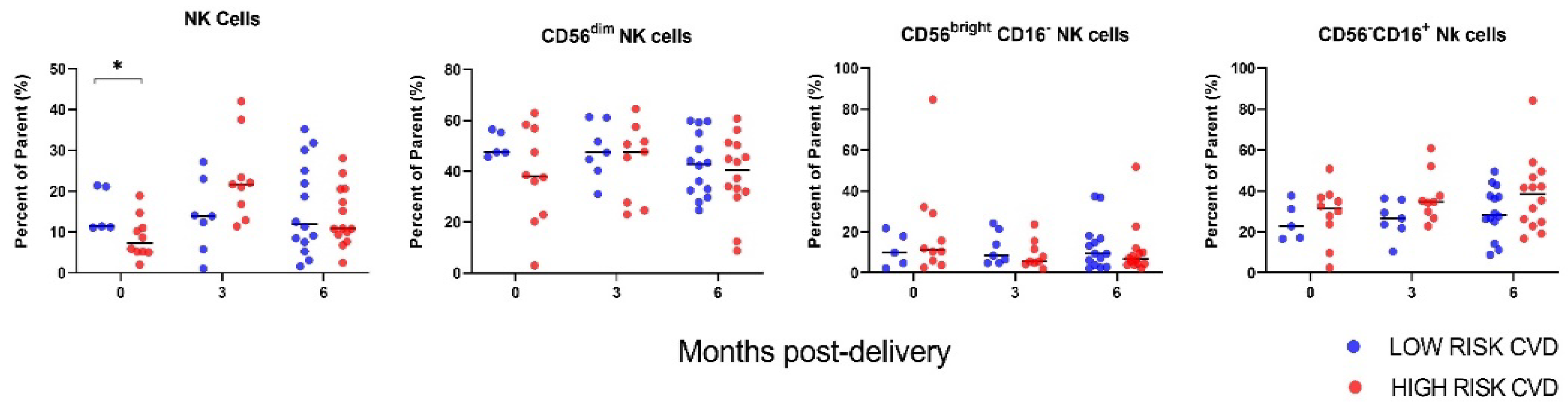
3.2. Immune Cell Profiles
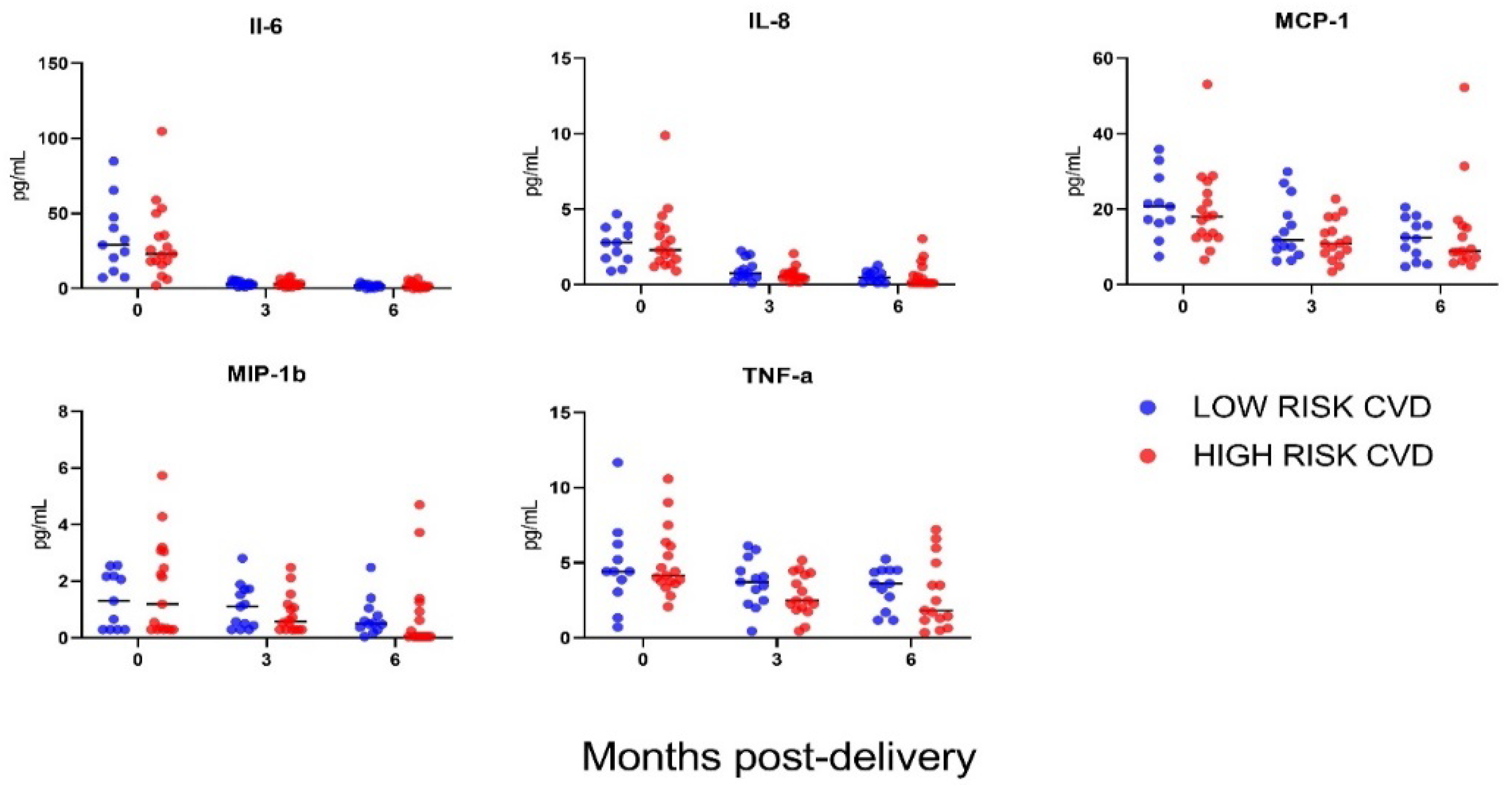
3.3. Cytokine Profiles
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lisonkova, S.; Joseph, K.S. Incidence of Preeclampsia: Risk Factors and Outcomes Associated with Early-versus Late-Onset Disease. Am. J. Obstet. Gynecol. 2013, 209, 544.e1–544.e12. [Google Scholar] [CrossRef] [PubMed]
- Kuklina, E.V.; Ayala, C.; Callaghan, W.M. Hypertensive Disorders and Severe Obstetric Morbidity in the United States. Obstet. Gynecol. 2009, 113, 1299–1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magee, L.A.; Pels, A.; Helewa, M.; Rey, E.; von Dadelszen, P.; Magee, L.A.; Audibert, F.; Bujold, E.; Côté, A.-M.; Douglas, M.J.; et al. Diagnosis, Evaluation, and Management of the Hypertensive Disorders of Pregnancy: Executive Summary. J. Obstet. Gynaecol. Can. 2014, 36, 416–438. [Google Scholar] [CrossRef]
- Leavey, K.; Wilson, S.L.; Bainbridge, S.A.; Robinson, W.P.; Cox, B.J. Epigenetic Regulation of Placental Gene Expression in Transcriptional Subtypes of Preeclampsia. Clin. Epigenetics 2018, 10, 28. [Google Scholar] [CrossRef]
- Leavey, K.; Benton, S.J.; Grynspan, D.; Kingdom, J.C.; Bainbridge, S.A.; Cox, B.J. Unsupervised Placental Gene Expression Profiling Identifies Clinically Relevant Subclasses of Human Preeclampsia. Hypertension 2016, 68, 137–147. [Google Scholar] [CrossRef] [Green Version]
- Benton, S.J.; Leavey, K.; Grynspan, D.; Cox, B.J.; Bainbridge, S.A. The Clinical Heterogeneity of Preeclampsia Is Related to Both Placental Gene Expression and Placental Histopathology. Am. J. Obstet. Gynecol. 2018, 219, 604.e1–604.e25. [Google Scholar] [CrossRef] [Green Version]
- Gladstone, R.A.; Pudwell, J.; Nerenberg, K.A.; Grover, S.A.; Smith, G.N. Cardiovascular Risk Assessment and Follow-Up of Women After Hypertensive Disorders of Pregnancy: A Prospective Cohort Study. J. Obstet. Gynaecol. Canada 2019, 41, 1157–1167. [Google Scholar] [CrossRef]
- Benschop, L.; Duvekot, J.J.; Roeters Van Lennep, J.E. Future Risk of Cardiovascular Disease Risk Factors and Events in Women after a Hypertensive Disorder of Pregnancy. Heart 2019, 76, 1273–1278. [Google Scholar] [CrossRef]
- Bellamy, L.; Casas, J.-P.; Hingorani, A.D.; Williams, D.J. Pre-Eclampsia and Risk of Cardiovascular Disease and Cancer in Later Life: Systematic Review and Meta-Analysis. BMJ 2007, 335, 974. [Google Scholar] [CrossRef] [Green Version]
- Brown, H.L.; Warner, J.J.; Gianos, E.; Gulati, M.; Hill, A.J.; Hollier, L.M.; Rosen, S.E.; Rosser, M.L.; Wenger, N.K. Promoting Risk Identification and Reduction of Cardiovascular Disease in Women Through Collaboration With Obstetricians and Gynecologists: A Presidential Advisory From the American Heart Association and the American College of Obstetricians and Gynecologi. Circulation 2018, 137, e843–e852. [Google Scholar] [CrossRef]
- Bushnell, C.; McCullough, L.D.; Awad, I.A.; Chireau, M.V.; Fedder, W.N.; Furie, K.L.; Howard, V.J.; Lichtman, J.H.; Lisabeth, L.D.; Piña, I.L.; et al. Guidelines for the Prevention of Stroke in Women. Stroke 2014, 45, 1545–1588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J.; Grover, S.; Gupta, M.; et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can. J. Cardiol. 2016, 32, 1263–1282. [Google Scholar] [CrossRef] [PubMed]
- Harmon, A.C.; Cornelius, D.C.; Amaral, L.M.; Faulkner, J.L.; Cunningham, M.W.; Wallace, K.; LaMarca, B. The Role of Inflammation in the Pathology of Preeclampsia. Clin. Sci. 2016, 130, 409–419. [Google Scholar] [CrossRef] [Green Version]
- Smith, G.N.; Pudwell, J.; Roddy, M. The Maternal Health Clinic: A New Window of Opportunity for Early Heart Disease Risk Screening and Intervention for Women with Pregnancy Complications. J. Obstet. Gynaecol. Can. 2013, 35, 831–839. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Leip, E.P.; Larson, M.G.; D’Agostino, R.B.; Beiser, A.; Wilson, P.W.F.; Wolf, P.A.; Levy, D. Prediction of Lifetime Risk for Cardiovascular Disease by Risk Factor Burden at 50 Years of Age. Circulation 2006, 113, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Cusimano, M.C.; Pudwell, J.; Roddy, M.; Cho, C.-K.J.; Smith, G.N. The Maternal Health Clinic: An Initiative for Cardiovascular Risk Identification in Women with Pregnancy-Related Complications. Am. J. Obstet. Gynecol. 2014, 210, 438.e1–438.e9. [Google Scholar] [CrossRef]
- Phelan, S. Pregnancy: A “Teachable Moment” for Weight Control and Obesity Prevention. Am. J. Obstet. Gynecol. 2010, 202, 135.e1–135.e8. [Google Scholar] [CrossRef] [Green Version]
- Dayan, N.; Nerenberg, K. Postpartum Cardiovascular Prevention: The Need for a National Health Systems-Based Strategy. Can. J. Cardiol. 2019, 35, 701–704. [Google Scholar] [CrossRef] [Green Version]
- Battistoni, A.; Rubattu, S.; Volpe, M. Circulating Biomarkers with Preventive, Diagnostic and Prognostic Implications in Cardiovascular Diseases. Int. J. Cardiol. 2012, 157, 160–168. [Google Scholar] [CrossRef]
- Arant, C.B.; Wessel, T.R.; Ridker, P.M.; Olson, M.B.; Reis, S.E.; Delia Johnson, B.; Sharaf, B.L.; Pauly, D.F.; Handberg, E.; Zineh, I.; et al. Multimarker Approach Predicts Adverse Cardiovascular Events in Women Evaluated for Suspected Ischemia: Results from the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation. Clin. Cardiol. 2009, 32, 244–250. [Google Scholar] [CrossRef]
- Cesari, M.; Penninx, B.W.J.H.; Newman, A.B.; Kritchevsky, S.B.; Nicklas, B.J.; Sutton-Tyrrell, K.; Rubin, S.M.; Ding, J.; Simonsick, E.M.; Harris, T.B.; et al. Inflammatory Markers and Onset of Cardiovascular Events: Results from the Health ABC Study. Circulation 2003, 108, 2317–2322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, S.Y.; Guild, S.-J.; Barrett, C.J.; Chen, Q.; McCowan, L.; Jordan, V.; Chamley, L.W. Tumor Necrosis Factor-Alpha, Interleukin-6, and Interleukin-10 Levels Are Altered in Preeclampsia: A Systematic Review and Meta-Analysis. Am. J. Reprod. Immunol. 2013, 70, 412–427. [Google Scholar] [CrossRef] [PubMed]
- Ozler, A.; Turgut, A.; Sak, M.E.; Evsen, M.S.; Soydinc, H.E.; Evliyaoglu, O.; Gul, T. Serum Levels of Neopterin, Tumor Necrosis Factor-Alpha and Interleukin-6 in Preeclampsia: Relationship with Disease Severity. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1707–1712. [Google Scholar]
- Szarka, A.; Rigó, J.; Lázár, L.; Bekő, G.; Molvarec, A. Circulating Cytokines, Chemokines and Adhesion Molecules in Normal Pregnancy and Preeclampsia Determined by Multiplex Suspension Array. BMC Immunol. 2010, 11, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahimzadeh, M.; Norouzian, M.; Arabpour, F.; Naderi, N. Regulatory T-Cells and Preeclampsia: An Overview of Literature. Expert Rev. Clin. Immunol. 2016, 12, 209–227. [Google Scholar] [CrossRef]
- Darmochwal-Kolarz, D.; Saito, S.; Rolinski, J.; Tabarkiewicz, J.; Kolarz, B.; Leszczynska-Gorzelak, B.; Oleszczuk, J. Activated T Lymphocytes in Pre-Eclampsia. Am. J. Reprod. Immunol. 2007, 58, 39–45. [Google Scholar] [CrossRef]
- Fukui, A.; Yokota, M.; Funamizu, A.; Nakamua, R.; Fukuhara, R.; Yamada, K.; Kimura, H.; Fukuyama, A.; Kamoi, M.; Tanaka, K.; et al. Changes of NK Cells in Preeclampsia. Am. J. Reprod. Immunol. 2012, 67, 278–286. [Google Scholar] [CrossRef]
- Kieffer, T.E.C.; Scherjon, S.A.; Faas, M.M.; Prins, J.R. Lower Activation of CD4+ Memory T Cells in Preeclampsia Compared to Healthy Pregnancies Persists Postpartum. J. Reprod. Immunol. 2019, 136, 102613. [Google Scholar] [CrossRef]
- Albany, C.J.; Trevelin, S.C.; Giganti, G.; Lombardi, G.; Scottà, C. Getting to the Heart of the Matter: The Role of Regulatory T-Cells (Tregs) in Cardiovascular Disease (CVD) and Atherosclerosis. Front. Immunol. 2019, 10, 2795. [Google Scholar] [CrossRef] [Green Version]
- Meng, X.; Yang, J.; Dong, M.; Zhang, K.; Tu, E.; Gao, Q.; Chen, W.; Zhang, C.; Zhang, Y. Regulatory T Cells in Cardiovascular Diseases. Nat. Rev. Cardiol. 2016, 13, 167–179. [Google Scholar] [CrossRef]
- Klingenberg, R.; Gerdes, N.; Badeau, R.M.; Gisterå, A.; Strodthoff, D.; Ketelhuth, D.F.J.; Lundberg, A.M.; Rudling, M.; Nilsson, S.K.; Olivecrona, G.; et al. Depletion of FOXP3+Regulatory T Cells Promotes Hypercholesterolemia and Atherosclerosis. J. Clin. Investig. 2013, 123, 1323–1334. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Schwartzenberg, S.; Medvedovsky, D.; Jonas, M.; Charach, G.; Afek, A.; Shamiss, A. Regulatory T Cells and IL-10 Levels Are Reduced in Patients with Vulnerable Coronary Plaques. Atherosclerosis 2012, 222, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, L.; Lu, F.; Pan, H.; Zhao, Y.; Wang, S.; Sun, S.; Li, C.; Hu, X. Increased Th17 Cell Frequency Concomitant with Decreased Foxp3+ Treg Cell Frequency in the Peripheral Circulation of Patients with Carotid Artery Plaques. Inflamm. Res. 2012, 61, 1155–1165. [Google Scholar] [CrossRef]
- Simons, K.H.; de Jong, A.; Jukema, J.W.; de Vries, M.R.; Arens, R.; Quax, P.H.A. T Cell Co-Stimulation and Co-Inhibition in Cardiovascular Disease: A Double-Edged Sword. Nat. Rev. Cardiol. 2019, 16, 325–343. [Google Scholar] [CrossRef] [PubMed]
- Kolbus, D.; Ljungcrantz, I.; Andersson, L.; Hedblad, B.; Fredrikson, G.N.; Björkbacka, H.; Nilsson, J. Association between CD8+ T-Cell Subsets and Cardiovascular Disease. J. Intern. Med. 2013, 274, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.S.Q.; Tayade, C.; Smith, G.N. Evidence of Inflammation and Predisposition toward Metabolic Syndrome after Pre-Eclampsia. Pregnancy Hypertens. An Int. J. Women’s Cardiovasc. Heal. 2015, 5, 354–358. [Google Scholar] [CrossRef]
- Vitoratos, N.; Economou, E.; Iavazzo, C.; Panoulis, K.; Creatsas, G. Maternal Serum Levels of TNF-Alpha and IL-6 Long after Delivery in Preeclamptic and Normotensive Pregnant Women. Mediators Inflamm. 2010, 2010, 908649. [Google Scholar] [CrossRef] [Green Version]
- Hermes, W.; Tamsma, J.T.; Grootendorst, D.C.; Franx, A.; van der Post, J.; van Pampus, M.G.; Bloemenkamp, K.W.; Porath, M.; Mol, B.W.; de Groot, C.J. Cardiovascular Risk Estimation in Women with a History of Hypertensive Pregnancy Disorders at Term: A Longitudinal Follow-up Study. BMC Pregnancy Childbirth 2013, 13, 126. [Google Scholar] [CrossRef] [Green Version]
- Van Rijn, B.B.; Bruinse, H.W.; Veerbeek, J.H.; Post Uiterweer, E.D.; Koenen, S.V.; van der Bom, J.G.; Rijkers, G.T.; Roest, M.; Franx, A. Postpartum Circulating Markers of Inflammation and the Systemic Acute-Phase Response after Early-Onset Preeclampsia. Hypertension 2016, 67, 404–414. [Google Scholar] [CrossRef]
- Yinon, Y.; Kingdom, J.C.P.; Odutayo, A.; Moineddin, R.; Drewlo, S.; Lai, V.; Cherney, D.Z.I.; Hladunewich, M.A. Vascular Dysfunction in Women With a History of Preeclampsia and Intrauterine Growth Restriction. Circulation 2010, 122, 1846–1853. [Google Scholar] [CrossRef] [Green Version]
- Ramsay, J. Microvascular Dysfunction: A Link between Pre-Eclampsia and Maternal Coronary Heart Disease. BJOG An Int. J. Obstet. Gynaecol. 2003, 110, 1029–1031. [Google Scholar] [CrossRef]
- Blaauw, J.; Graaff, R.; van Pampus, M.G.; van Doormaal, J.J.; Smit, A.J.; Rakhorst, G.; Aarnoudse, J.G. Abnormal Endothelium-Dependent Microvascular Reactivity in Recently Preeclamptic Women. Obstet. Gynecol. 2005, 105, 626–632. [Google Scholar] [CrossRef] [PubMed]
| Immune Cell Families | Phenotypes and Parent Populations |
|---|---|
| T Cells | CD3+ CD45+ T cells |
| └ CD4+ T cells | |
| └ FoxP3+ regulatory T cells | |
| └ CD8+ T cells | |
| └ CD4+ CD8+ (double positive) T cells | |
| └ CD4− CD8− (double negative) T cells | |
| └ CD25+ activated T cells | |
| └ CD69+ activated T cells | |
| Non T Cell lymphocytes and Myeloid cells | CD3−CD45+ |
| └ CD3− CD45+ CD19+ B cells | |
| └ HLA DR+ B cells | |
| └ CD3− CD45+ NK cells | |
| └ CD56bright CD16− NK cells | |
| └ CD56dim NK cells | |
| └ CD56neg CD16+ NK cells | |
| └ CD14+ Myeloid cells | |
| └ CD11b+ Monocytes | |
| └ HLA-DR+ Monocytes |
| Characteristic | Total Cohort, n = 31 |
|---|---|
| Maternal Age, years, median (IQR) | 33 (30, 38) |
| College/University education, n(%) | 29 (93.5) |
| Fulltime employment, n(%) | 24 (77.4) |
| Current smoker, n(%) | 1 (3.2) |
| Pre-pregnancy alcohol consumption, n(%) b,c | 15 (48.4) |
| Physically active a,d, n(%) | |
| Before pregnancy | 12 (38.7) |
| During pregnancy | 9 (29.0) |
| Pre-pregnancy BMI, kg/m2, median (IQR) | 27.4 (23.3, 34.0) |
| Underweight (<18.5 kg/m2), n(%) | 1 (3.2) |
| Healthy (18.5–24.9 kg/m2), n(%) | 11 (35.5) |
| Overweight (25–29.9 kg/m2), n(%) | 7 (22.6) |
| Obese (≥30 kg/m2), n(%) | 12 (38.7) |
| Maternal history of complications in pregnancy, n(%) | |
| Gestational hypertension | 7 (22.6) |
| Preeclampsia | 6 (19.4) |
| Intrauterine growth restricted fetus | 1 (3.2) |
| Placental abruption | 1 (3.2) |
| Preterm birth < 34 weeks | 3 (9.7) |
| Known family medical history (1st degree relatives), n(%) | |
| Coronary artery disease | 14 (45.2) |
| Cerebrovascular disease | 8 (25.8) |
| Diabetes (type 1 or 2) | 19 (61.3) |
| Hypertension | 25 (80.6) |
| Malignancy | 21 (67.7) |
| Obesity | 10 (32.3) |
| Gestational hypertension | 6 (19.4) |
| Preeclampsia | 6 (19.4) |
| Nulliparous, n(%) | 21 (67.7) |
| Gestational weight gain, kg, median (IQR) a | 13.4 (8.1, 18.4) |
| Inadequate e, n(%) | 8 (25.8) |
| Adequate e, n(%) | 8 (25.8) |
| Excessive e, n(%) | 14 (45.2) |
| Systolic blood pressure at delivery, mmHg, median (IQR) | 135.0 (125.0, 152.0) |
| Diastolic blood pressure at delivery, mmHg, median (IQR) | 85.0 (78.0, 91.0) |
| Mode of delivery, n(%) | |
| Spontaneous vaginal | 6 (19.4) |
| Induced vaginal | 13 (41.9) |
| Planned Cesarean section | 3 (9.7) |
| Emergency Cesarean section | 9 (29.0) |
| Gestational age at delivery, weeks, median (IQR) | 38.0 (36.3, 39.4) |
| Preterm (<37 weeks), n(%) | 8 (25.8) |
| Term (≥37 weeks), n(%) | 23 (74.2) |
| Infant birthweight, g, median (IQR) | 3029 (2335, 3497) |
| Characteristic | Overall, n = 31 |
|---|---|
| Weeks postpartum, median (IQR) | 26.0 (26.0, 27.0) |
| Waist circumference, cm, median (IQR) a | 91.4 (83.8, 104.1) |
| Hip circumference, cm, median (IQR) a | 106.0 (96.5, 119.4) |
| Maternal BMI, kg/m2, median (IQR) | 28.1 (24.4, 35.5) |
| Underweight (<18.5 kg/m2), n(%) | 1 (3.2) |
| Healthy (18.5–24.9 kg/m2), n(%) | 8 (25.8) |
| Overweight (25–29.9 kg/m2), n(%) | 11 (35.5) |
| Obese (≥30 kg/m2), n(%) | 11 (35.5) |
| Postpartum weight retention, kg, median (IQR) | 0.4 (−1.7, 7.0) |
| ≥150 min/week moderate to vigorous physical activity a, n(%) | 16 (53.3) |
| Breastfeeding (exclusive or combination feeding) a, n(%) | 18 (60.0) |
| HbA1C, %, median (IQR) | 5.3 (5.1, 5.5) |
| <4.8%, n(%) | 2 (6.5) |
| 4.8–6.0%, n(%) | 29 (93.5) |
| >6.0%, n(%) | 0 (0) |
| LDL, mmol/L, median (IQR) a | 3.0 (4.2, 5.6) |
| <2.6, n(%) | 11 (36.7) |
| ≥2.6, n(%) | 19 (63.3) |
| HDL, mmol/L, median (IQR) | 1.56 (1.2, 1.9) |
| <1.3, n(%) | 9 (29.0) |
| ≥1.3, n(%) | 22 (71.0) |
| Triglycerides, mmol/L, median (IQR) | 0.98 (0.73, 1.6) |
| <1.7, n(%) | 23 (74.2) |
| ≥1.7, n(%) | 8 (25.8) |
| High-sensitivity CRP, mg/L, median (IQR) | 2.6 (1.0, 9.6) |
| ≤10, n(%) | 23 (74.2) |
| >10, n(%) | 8 (25.8) |
| Albumin:Creatinine ratio, median (IQR) b | 1.95 (1.2, 3.9) |
| ≤2.0, n(%) | 14 (56.0) |
| >2.0, n(%) | 11 (44.0) |
| Systolic blood pressure, mmHg, median (IQR) | 117.0 (111.0, 126.0) |
| <120 (optimal), n(%) | 19 (61.3) |
| 120–139 (not optimal), n(%) | 5 (16.1) |
| 140–159 (elevated), n(%) | 1 (3.2) |
| ≥160 or taking an antihypertensive medication (major), n(%) | 6 (19.4) |
| Diastolic blood pressure, mmHg, median (IQR) | 78.0 (73.0, 82.0) |
| <80 (optimal), n(%) | 16 (51.6) |
| 80–89 (not optimal), n(%) | 8 (25.8) |
| 90–99 (elevated), n(%) | 1 (3.2) |
| ≥100 or taking an antihypertensive medication (major), n(%) | 6 (19.4) |
| Fasting glucose, mmol/L, median (IQR) a | 4.7 (4.4, 5.0) |
| ≤6.88 (optimal), n(%) | 30 (100) |
| >6.88 or previous diagnosis of type 1 or 2 diabetes (major), n(%) | - |
| Total cholesterol, median (IQR) | 5.1 (4.0, 5.6) |
| <4.65 (optimal), n(%) | 12 (38.5) |
| 4.65–5.15 (not optimal), n(%) | 4 (12.9) |
| 5.16–6.19 (elevated), n(%) | 14 (45.2) |
| ≥6.20 (major), n(%) | 1 (3.2) |
| Smoking, n(%) | |
| No (optimal) | 30 (96.8) |
| Yes (major) | 1 (3.2) |
| Lifetime CVD risk score, n(%) | |
| <39% (low) | 13 (41.9) |
| ≥39% (high) | 18 (58.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murphy, M.S.Q.; Benton, S.J.; Cox, B.; Nerenberg, K.; McComb, S.; Krishnan, L.; Weeratna, R.D.; Paré, J.-F.; Dingwall-Harvey, A.L.J.; Bainbridge, S.A.; et al. Maternal Immune Cell and Cytokine Profiles to Predict Cardiovascular Risk Six Months after Preeclampsia. J. Clin. Med. 2022, 11, 4185. https://doi.org/10.3390/jcm11144185
Murphy MSQ, Benton SJ, Cox B, Nerenberg K, McComb S, Krishnan L, Weeratna RD, Paré J-F, Dingwall-Harvey ALJ, Bainbridge SA, et al. Maternal Immune Cell and Cytokine Profiles to Predict Cardiovascular Risk Six Months after Preeclampsia. Journal of Clinical Medicine. 2022; 11(14):4185. https://doi.org/10.3390/jcm11144185
Chicago/Turabian StyleMurphy, Malia S. Q., Samantha J. Benton, Brian Cox, Kara Nerenberg, Scott McComb, Lakshmi Krishnan, Risini D. Weeratna, Jean-François Paré, Alysha L. J. Dingwall-Harvey, Shannon A. Bainbridge, and et al. 2022. "Maternal Immune Cell and Cytokine Profiles to Predict Cardiovascular Risk Six Months after Preeclampsia" Journal of Clinical Medicine 11, no. 14: 4185. https://doi.org/10.3390/jcm11144185
APA StyleMurphy, M. S. Q., Benton, S. J., Cox, B., Nerenberg, K., McComb, S., Krishnan, L., Weeratna, R. D., Paré, J.-F., Dingwall-Harvey, A. L. J., Bainbridge, S. A., Gruslin, A., & Gaudet, L. M. (2022). Maternal Immune Cell and Cytokine Profiles to Predict Cardiovascular Risk Six Months after Preeclampsia. Journal of Clinical Medicine, 11(14), 4185. https://doi.org/10.3390/jcm11144185









