Comparison of Fragmentation and Dusting Modality Using Holmium YAG Laser during Ureteroscopy for the Treatment of Ureteral Stone: A Single-Center’s Experience
Abstract
:1. Introduction
2. Materials and Methods
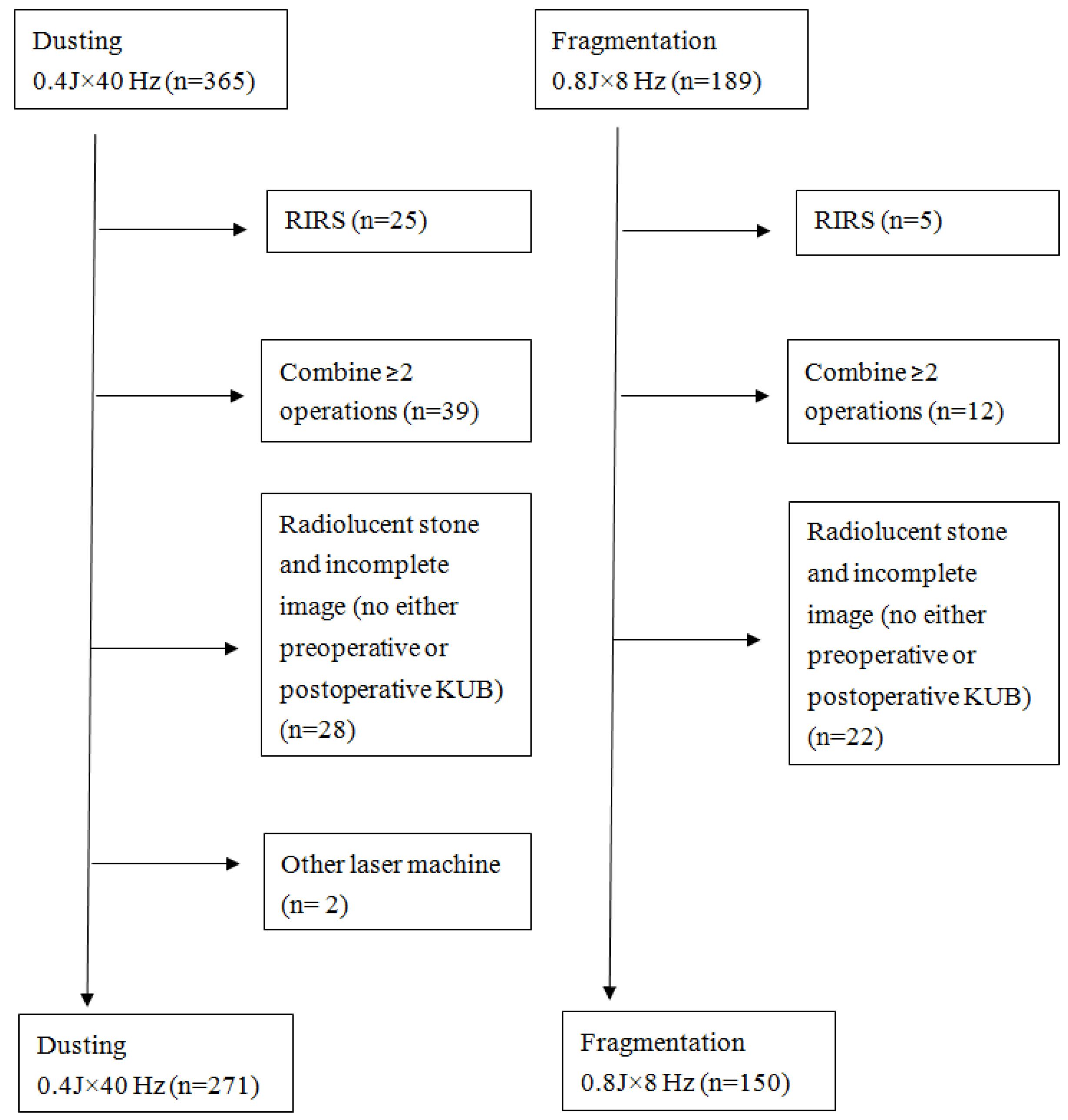
2.1. Study Population and Inclusion Criteria
2.2. Exclusion Criteria
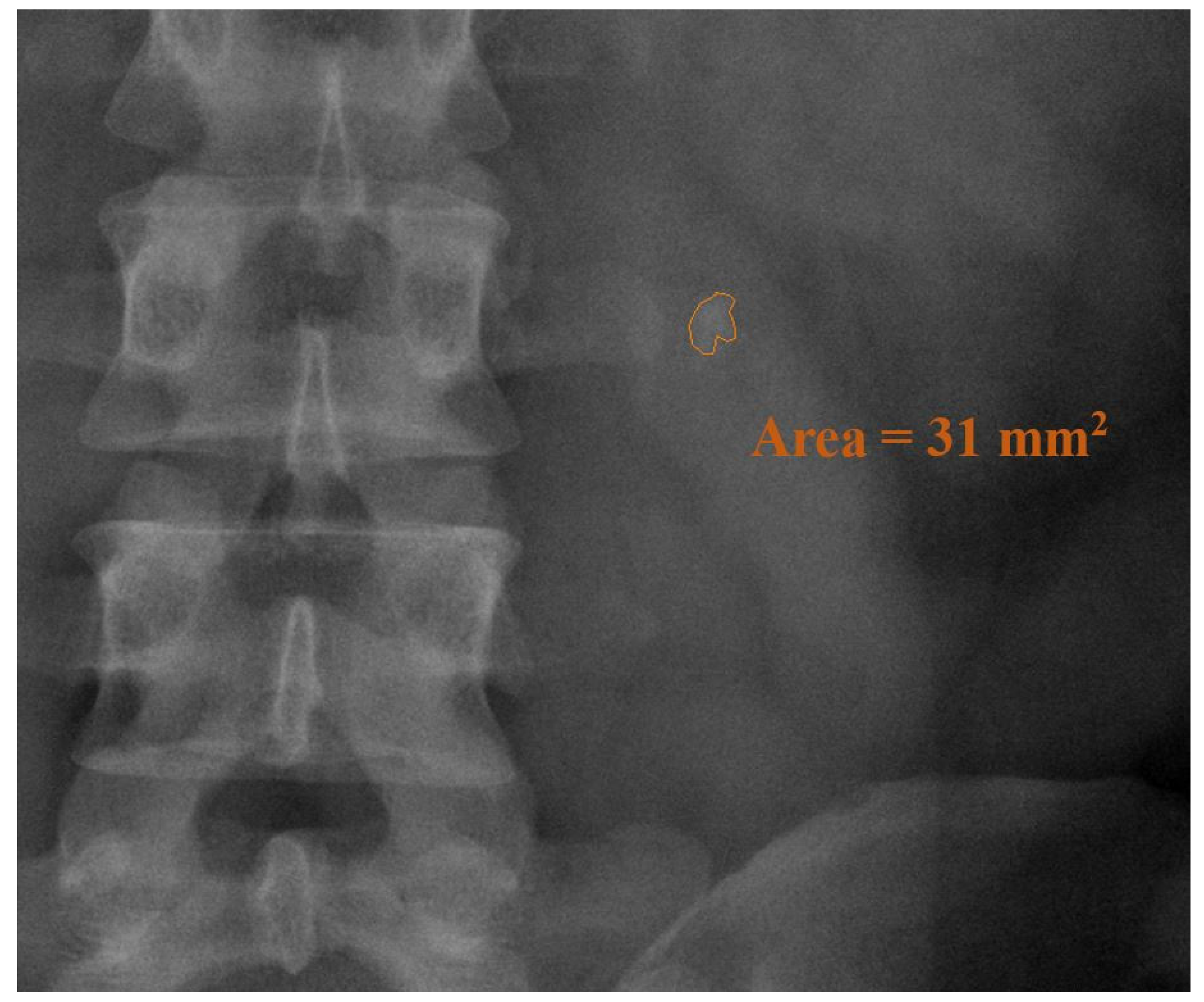
2.3. Evaluations
2.4. Procedures
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, L.; Fei, X.; Song, Y. The clinical efficacy of novel vacuum suction ureteroscopic lithotripsy in the treatment of upper ureteral calculi. World J. Urol. 2021, 39, 4261–4265. [Google Scholar] [CrossRef] [PubMed]
- Preminger, G.M.; Tiselius, H.-G.; Assimos, D.G.; Alken, P.; Buck, C.; Gallucci, M.; Knoll, T.; Lingeman, J.E.; Nakada, S.Y.; Pearle, M.S.; et al. 2007 Guideline for the Management of Ureteral Calculi. J. Urol. 2007, 178, 2418–2434. [Google Scholar] [CrossRef]
- Enikeev, D.; Grigoryan, V.; Fokin, I.; Morozov, A.; Taratkin, M.; Klimov, R.; Kozlov, V.; Gabdullina, S.; Glybochko, P. Endoscopic lithotripsy with a SuperPulsed thulium-fiber laser for ureteral stones: A single-center experience. Int. J. Urol. 2020, 28, 261–265. [Google Scholar] [CrossRef]
- Romeu, G.; Marzullo-Zucchet, L.J.; Díaz, J.; Villarroya, S.; Budía, A.; Ordaz, D.D.G.; Caballer, V.; Vivas, D. Comparing extracorporeal shock wave lithotripsy and ureteroscopy laser lithotripsy for treatment of urinary stones smaller than 2 cm: A cost-utility analysis in the Spanish clinical setting. World J. Urol. 2021, 39, 3593–3598. [Google Scholar] [CrossRef] [PubMed]
- Black, K.M.; Aldoukhi, A.H.; Teichman, J.M.H.; Majdalany, S.E.; Hall, T.L.; Roberts, W.W.; Ghani, K.R. Pulse modulation with Moses technology improves popcorn laser lithotripsy. World J. Urol. 2020, 39, 1699–1705. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Tang, Z.; Yu, B.; Wang, Y.; Li, Y.; Yang, Q.; Tang, W. Holmium: YAG Laser lithotripsy versus pneumatic lithotripsy for treatment of distal ureteral calculi: A meta-analysis. J. Endourol. 2013, 27, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Rabani, S.M.; Rabani, S.H.; Rashidi, N. Laser Versus Pneumatic Lithotripsy With Semi-Rigid Ureteroscope; A Comparative Randomized Study. J. Lasers Med. Sci. 2019, 10, 185–188. [Google Scholar] [CrossRef] [Green Version]
- Aldoukhi, A.H.; Black, K.M.; Ghani, K.R. Emerging Laser Techniques for the Management of Stones. Urol. Clin. N. Am. 2019, 46, 193–205. [Google Scholar] [CrossRef]
- Matlaga, B.R.; Chew, B.; Eisner, B.; Humphreys, M.; Knudsen, B.; Krambeck, A.; Lange, D.; Lipkin, M.; Miller, N.L.; Monga, M.; et al. Ureteroscopic Laser Lithotripsy: A Review of Dusting vs. Fragmentation with Extraction. J. Endourol. 2018, 32, 1–6. [Google Scholar] [CrossRef]
- Aldoukhi, A.H.; Roberts, W.W.; Hall, T.L.; Teichman, J.M.; Ghani, K.R. Understanding the Popcorn Effect During Holmium Laser Lithotripsy for Dusting. Urology 2018, 122, 52–57. [Google Scholar] [CrossRef]
- Sea, J.; Jonat, L.M.; Chew, B.H.; Qiu, J.; Wang, B.; Hoopman, J.; Milner, T.; Teichman, J.M. Optimal Power Settings for Holmium: YAG Lithotripsy. J. Urol. 2012, 187, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.; Lee, F.; Yip, S.; Tam, P. Outpatient Holmium Laser Lithotripsy Using Semirigid Ureteroscope Is the Treatment Outcome Affected by Stone Load? Eur. Urol. 2001, 39, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-C.; Chiu, A.W.; Lin, W.-R.; Lin, W.-C.; Yang, S.; Hsu, J.-M.; Chow, Y.-C.; Tsai, W.-K.; Chiang, P.-K.; Chen, M. Comparison of pneumatic and Holmium laser ureteroscopic lithotripsy for upper third ureteral stones. Urol. Sci. 2017, 28, 101–104. [Google Scholar] [CrossRef]
- Vassar, G.J.; Chan, K.F.; Teichman, J.M.; Glickman, R.D.; Weintraub, S.T.; Pfefer, T.J.; Welch, A.J. Holmium: YAG lithotripsy: Photothermal mechanism. J. Endourol. 1999, 13, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Elhilali, M.M.; Fahmy, N.; Carrier, S.; Andonian, S. Double-Blinded Prospective Randomized Clinical Trial Comparing Regular and Moses Modes of Holmium Laser Lithotripsy. J. Endourol. 2020, 34, 624–628. [Google Scholar] [CrossRef] [PubMed]
- White, M.D.; Moran, M.E.; Calvano, C.J.; Borhan-Manesh, A.; Mehlhaff, B.A. Evaluation of retropulsion caused by holmium: YAG laser with various power settings and fibers. J. Endourol. 1998, 12, 183–186. [Google Scholar] [CrossRef]
- Senocak, C.; Ozcan, C.; Sahin, T.; Yilmaz, G.; Ozyuvali, E.; Sarikaya, S.; Resorlu, B.; Oguz, U.; Bozkurt, O.F.; Unsal, A.; et al. Risk Factors of Infectious Complications after Flexible Uretero-renoscopy with Laser Lithotripsy. Urol. J. 2018, 15, 158–163. [Google Scholar] [CrossRef]
- Kızılay, F.; Irer, B.; Şen, V.; Erbatu, O.; Ongün, Ş.; Yıldız, A.; Çınar, .; Cihan, A.; Üçer, O.; Bozkurt, O.; et al. Effect of the Anesthetic Method on the Outcomes of Ureteroscopy for Proximal Ureteral Stones: A Multi-center Study of the Society of Urological Surgery Aegean Study Group. J. Urol. Surg. 2018, 5, 170–175. [Google Scholar] [CrossRef]
- Hsieh, C.-H.; Yang, S.S.-D.; Lin, C.-D.; Chang, S.-J. Are prophylactic antibiotics necessary in patients with preoperative sterile urine undergoing ureterorenoscopic lithotripsy? Br. J. Urol. 2014, 113, 275–280. [Google Scholar] [CrossRef] [Green Version]
- Bai, T.; Yu, X.; Qin, C.; Xu, T.; Shen, H.; Wang, L.; Liu, X. Identification of Factors Associated with Postoperative Urosepsis after Ureteroscopy with Holmium: Yttrium-Aluminum-Garnet Laser Lithotripsy. Urol. Int. 2019, 103, 311–317. [Google Scholar] [CrossRef]
- Ozgor, F.; Kucuktopcu, O.; Ucpinar, B.; Gurbuz, Z.G.; Sarilar, O.; Berberoglu, A.Y.; Baykal, M.; Binbay, M. Is There A Difference Between Presence of Single Stone And Multiple Stones in Flexible Ureterorenoscopy And Laser Lithotripsy For Renal Stone Burden. Int. Braz. J. Urol 2016, 42, 1168–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degirmenci, T.; Gunlusoy, B.; Kozacioglu, Z.; Arslan, M.; Kara, C.; Koras, O.; Minareci, S. Outcomes of ureteroscopy for the management of impacted ureteral calculi with different localizations. Urology 2012, 80, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chen, Y.; Liao, B.; Luo, D.; Wang, K.; Li, H.; Zeng, G. Epidemiology of urolithiasis in Asia. Asian J. Urol. 2018, 5, 205–214. [Google Scholar] [CrossRef] [PubMed]
| Variables | Dusting Group (n = 271) | Fragmentation Group (n = 150) | p-Value | |
|---|---|---|---|---|
| Female/Male (Female %) | 114/157 (42.1) | 50/100 (33.3) | 0.078 | |
| Left/Right (Left %) | 151/120 (55.7) | 84/66 (56) | 0.956 | |
| Admission rate, n (%) | 206 (76) | 125 (83) | 0.079 | |
| Mean age, year; mean ± SD * | 54.1 ± 12.63 | 53.9 ± 13.57 | 0.89 | |
| Mean stone burden, mm2; mean ± SD * | 56.8 ± 60.71 | 48.9 ± 59.23 | 0.199 | |
| Anesthesia, n (%) | 0.312 | |||
| Spinal | 102 (38) | 64 (43) | ||
| General | 169 (62) | 86 (57) | ||
| Number of stones, n (%) | 0.023 | |||
| Single | 219 (81) | 134 (89) | ||
| Multiple | 52 (19) | 16 (11) | ||
| Stone location, n (%) | ||||
| Upper | 234 (86) | 135 (90) | 0.275 | |
| Middle | 25 (9) | 12 (8) | 0.671 | |
| Lower | 20 (7) | 10 (7) | 0.785 | |
| Ureter condition, n (%) | ||||
| Polyposis | 55 (20) | 22 (15) | 0.153 | |
| Angulation | 40 (15) | 26 (17) | 0.487 | |
| Stricture | 32 (12) | 23 (15) | 0.304 | |
| Edema | 22 (8) | 5 (3) | 0.055 | |
| Pyuria, n (%) | 110 (41) | 33 (22) | <0.001 | |
| Variables 1 | Dusting Group (n = 150) | Fragmentation Group (n = 150) | p-Value | |
|---|---|---|---|---|
| Female/Male (Female %) | 101/49 (67) | 100/50 (67) | 0.902 | |
| Left/Right (Left %) | 81/69 (54) | 84/66 (56) | 0.728 | |
| Admission, n (%) | 125 (83) | 125 (83) | 1 | |
| Mean age, year; mean ± SD 2 | 53.23 ± 12.68 | 53.95 ± 13.57 | 0.638 | |
| Mean stone burden, mm2; mean ± SD 2 | 51.33 ± 58.69 | 48.9 ± 59.24 | 0.722 | |
| Anesthesia, n (%) | 0.816 | |||
| Spinal | 66 (91) | 64 (89) | ||
| General | 84 (9) | 86 (11) | ||
| Number of stones, n (%) | 0.558 | |||
| Single | 137 (91) | 134 (89) | ||
| Multiple | 13 (9) | 16 (11) | ||
| Stone location, n (%) | ||||
| Upper | 128 (85) | 135 (90) | 0.219 | |
| Middle | 12 (8) | 12 (8) | 1 | |
| Lower | 9 (6) | 10 (7) | 0.813 | |
| Ureter condition, n (%) | ||||
| Polyposis | 24 (16) | 22 (15) | 0.749 | |
| Angulation | 25 (17) | 26 (17) | 0.878 | |
| Stricture | 26 (17) | 23 (15) | 0.639 | |
| Edema | 1 (1) | 5 (3) | 0.214 | |
| Pyuria, n (%) | 35 (23) | 33 (22) | 0.783 | |
| Variables | Dusting Group (n = 150) | Fragmentation Group (n = 150) | p-Value | |
|---|---|---|---|---|
| OP 1 time, min; mean ± SD 2 | 37.73 ± 17.92 | 37.6 ± 19.14 | 0.95 | |
| Effectiveness, mm2/min; mean ± SD 2 | 1.37 ± 1.16 | 1. 45 ± 1.56 | 0.613 | |
| Ureteral stent insertion, n (%) | 128 (85) | 127 (85) | 0.872 | |
| RUC 3 | 7 (5) | 9 (6) | 0.607 | |
| DJ 4 | 121 (81) | 118 (79) | 0.667 | |
| Basket use, n (%) | 87 (58) | 93 (62) | 0.48 | |
| Stone free, n (%) | 113 (75) | 123 (82) | 0.159 | |
| Retropulsion, n (%) | 29 (20) | 15 (10) | 0.022 | |
| Secondary intervention, n (%) | 19 (18) | 29 (19) | 0.115 | |
| Ureter injury, n (%) | 0 (0) | 1 (1) | 0.5 | |
| Complication, n (%) | 6 (4) | 3 (2) | 0.501 | |
| Variables | Univariate | Multivariate | ||||||
|---|---|---|---|---|---|---|---|---|
| p-Value | OR1 | 95% CI 2 of OR 1 | p-Value | OR 1 | 95% CI 2 of OR 1 | |||
| Fragmenation system | 0.16 | 1.492 | 0.854 | 2.606 | ||||
| Basket use | <0.001 | 4.632 | 2.555 | 8.397 | <0.001 | 3.932 | 2.136 | 7.238 |
| General anesthesia | 0.136 | 1.525 | 0.876 | 2.656 | ||||
| Female gender | 0.737 | 1.107 | 0.611 | 2.004 | ||||
| Right ureter stone | 0.428 | 1.254 | 0.716 | 2.197 | ||||
| Single stone | 0.074 | 2.115 | 0.93 | 4.81 | ||||
| No upper ureteral stone | 0.018 | 11.34 | 1.524 | 84.387 | 0.044 | 8.095 | 1.063 | 61.667 |
| No pyuria | 0.001 | 2.877 | 1.577 | 5.249 | 0.013 | 2.245 | 1.184 | 4.254 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, B.-H.; Lin, T.-F.; Tsai, C.-C.; Chen, M.; Chiu, A.W. Comparison of Fragmentation and Dusting Modality Using Holmium YAG Laser during Ureteroscopy for the Treatment of Ureteral Stone: A Single-Center’s Experience. J. Clin. Med. 2022, 11, 4155. https://doi.org/10.3390/jcm11144155
Chen B-H, Lin T-F, Tsai C-C, Chen M, Chiu AW. Comparison of Fragmentation and Dusting Modality Using Holmium YAG Laser during Ureteroscopy for the Treatment of Ureteral Stone: A Single-Center’s Experience. Journal of Clinical Medicine. 2022; 11(14):4155. https://doi.org/10.3390/jcm11144155
Chicago/Turabian StyleChen, Bo-Han, Tsu-Feng Lin, Chih-Chun Tsai, Marcelo Chen, and Allen W. Chiu. 2022. "Comparison of Fragmentation and Dusting Modality Using Holmium YAG Laser during Ureteroscopy for the Treatment of Ureteral Stone: A Single-Center’s Experience" Journal of Clinical Medicine 11, no. 14: 4155. https://doi.org/10.3390/jcm11144155
APA StyleChen, B.-H., Lin, T.-F., Tsai, C.-C., Chen, M., & Chiu, A. W. (2022). Comparison of Fragmentation and Dusting Modality Using Holmium YAG Laser during Ureteroscopy for the Treatment of Ureteral Stone: A Single-Center’s Experience. Journal of Clinical Medicine, 11(14), 4155. https://doi.org/10.3390/jcm11144155






