Occurrence and Temporal Variability of Out-of-Hospital Cardiac Arrest during COVID-19 Pandemic in Comparison to the Pre-Pandemic Period in Poland—Observational Analysis of OSCAR-POL Registry
Abstract
:1. Introduction
2. Materials and Methods
3. Results
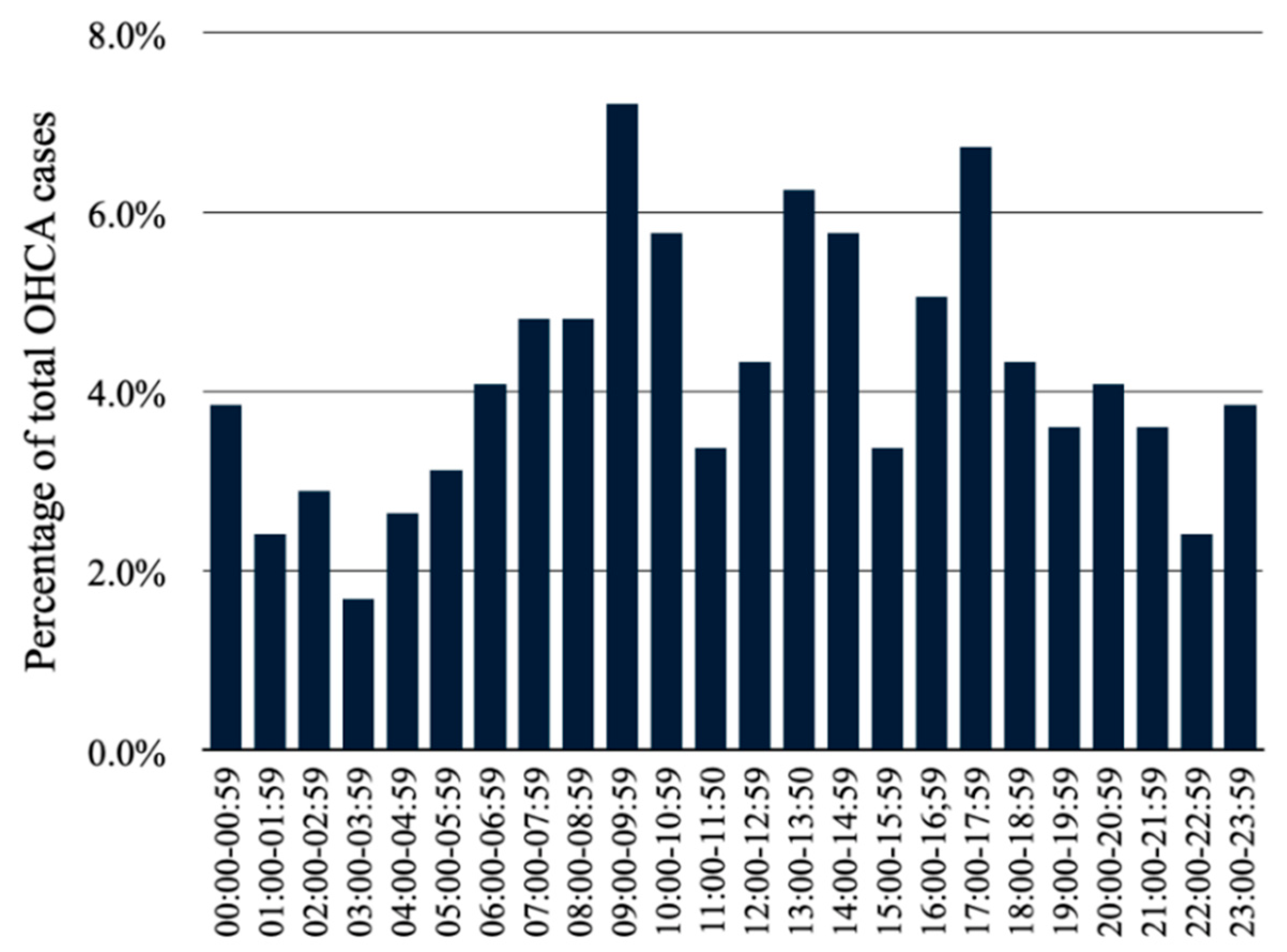
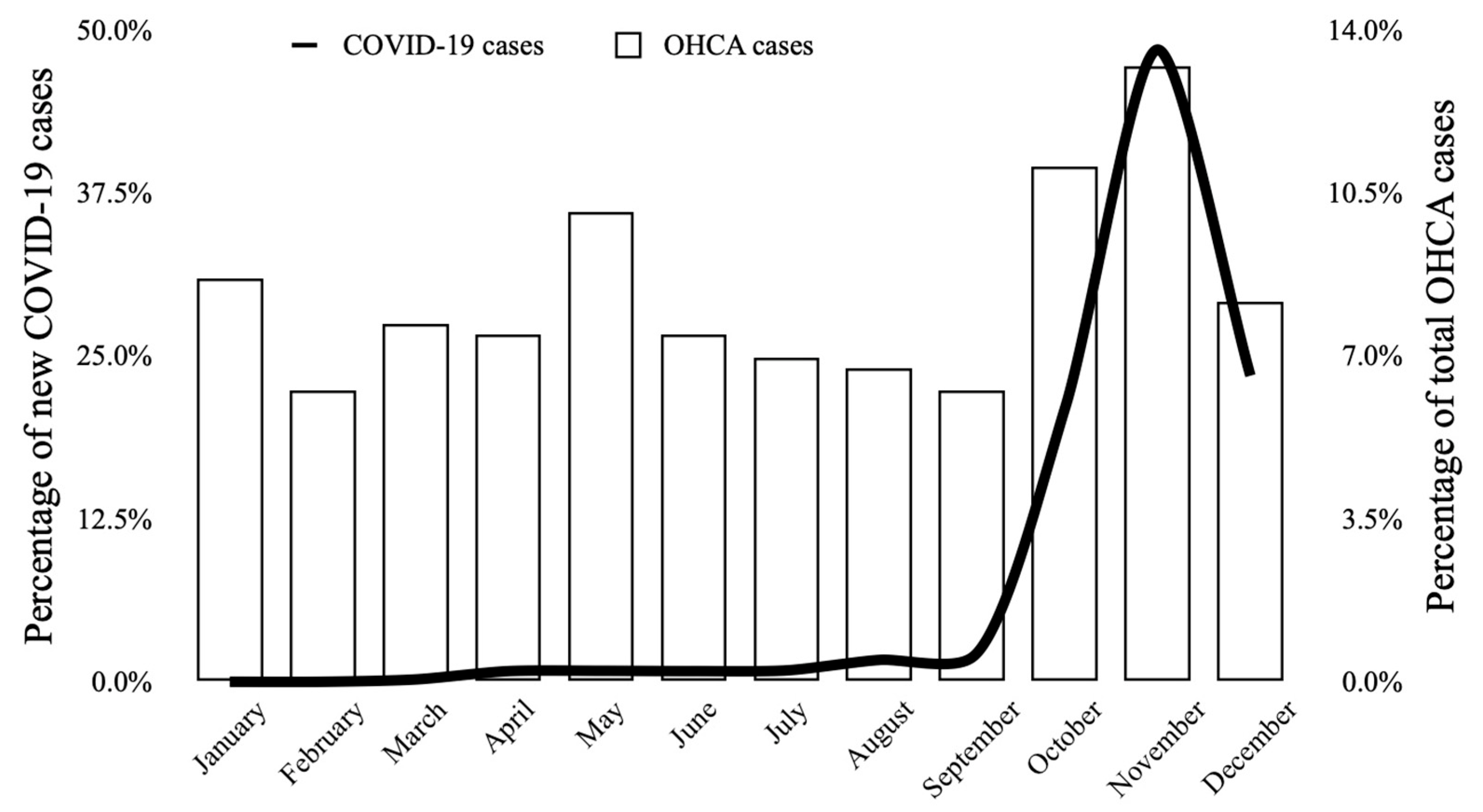
3.1. Temporal Variability of Out-of-Hospital Cardiac Arrest during 2020
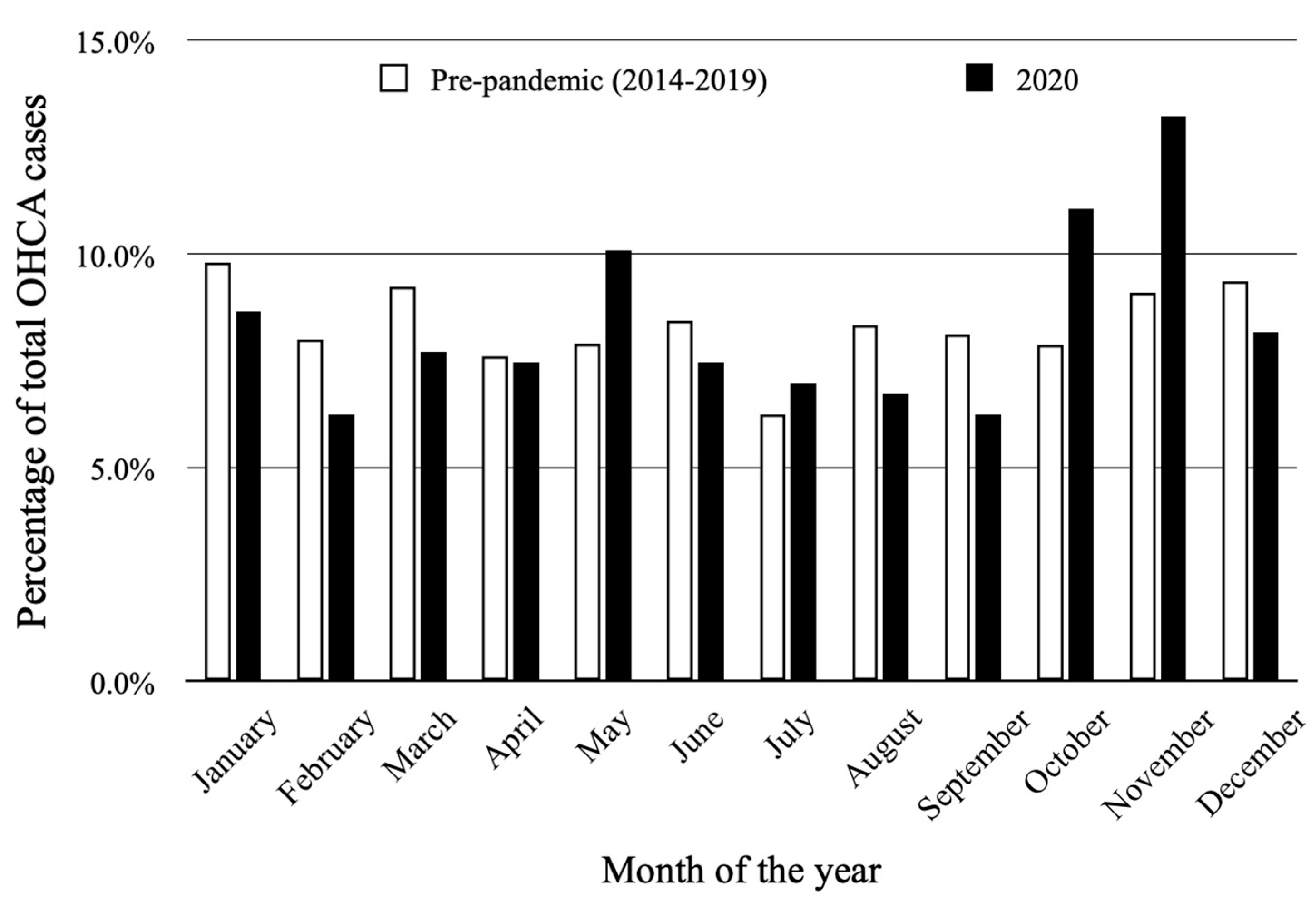
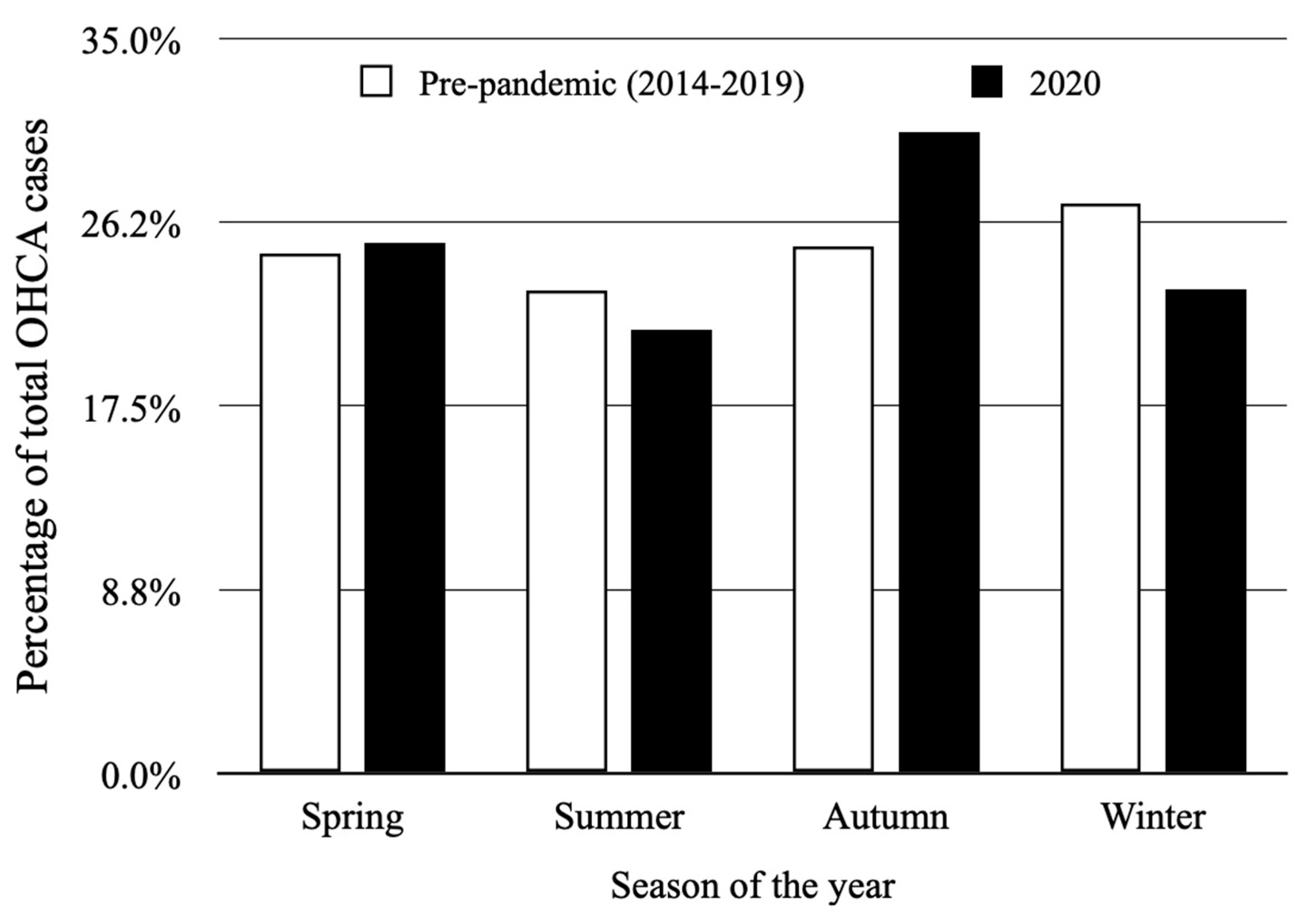
3.2. Comparison of Temporal Variability between the Year 2020 and 6-Year Pre-Pandemic Period (2014–2019)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization COVID-19 Weekly Epidemiological Update, Edition 63, 26 October 2021; World Health Organization: Geneva, Switzerland, 2021.
- Raport Zakażeń Koronawirusem (SARS-CoV-2)-Koronawirus: Informacje i Zalecenia-Portal Gov.pl. Available online: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2 (accessed on 21 November 2021).
- Kubica, J.; Podhajski, P.; Magielski, P.; Kubica, A.; Adamski, P.; Junik, R.; Pinkas, J.; Navarese, E.P. IMPACT of PCSK9 Inhibition on Clinical Outcome in Patients during the Inflammatory Stage of the SARS-COV-2 Infection: Rationale and Protocol of the IMPACT-SIRIO 5 Study. Cardiol. J. 2021, 29, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Gąsecka, A.; Borovac, J.A.; Guerreiro, R.A.; Giustozzi, M.; Parker, W.; Caldeira, D.; Chiva-Blanch, G. Thrombotic Complications in Patients with COVID-19: Pathophysiological Mechanisms, Diagnosis, and Treatment. Cardiovasc. Drugs Ther. 2021, 35, 215–229. [Google Scholar] [CrossRef] [PubMed]
- Hollenberg, J.; Svensson, L.; Rosenqvist, M. Out-of-Hospital Cardiac Arrest: 10 Years of Progress in Research and Treatment. J. Intern. Med. 2013, 273, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Borkowska, M.J.; Jaguszewski, M.J.; Koda, M.; Gasecka, A.; Szarpak, A.; Gilis-Malinowska, N.; Safiejko, K.; Szarpak, L.; Filipiak, K.J.; Smereka, J. Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. J. Clin. Med. 2021, 10, 1209. [Google Scholar] [CrossRef]
- Bruska, M.; Szankin, Z.; Ratajczak, J.; Fabiszak, T. Improvement of the Quality of Cardiopulmonary Resuscitation Performed with Real CPR Help® Device among Medical Students and Medical Workers. Med. Res. J. 2021, 6, 177–183. [Google Scholar] [CrossRef]
- Malysz, M.; Dabrowski, M.; Böttiger, B.W.; Smereka, J.; Kulak, K.; Szarpak, A.; Jaguszewski, M.; Filipiak, K.J.; Ladny, J.R.; Ruetzler, K.; et al. Resuscitation of the Patient with Suspected/Confirmed COVID-19 When Wearing Personal Protective Equipment: A Randomized Multicenter Crossover Simulation Trial. Cardiol. J. 2020, 27, 497–506. [Google Scholar] [CrossRef]
- Ahn, J.Y.; Ryoo, H.W.; Cho, J.W.; Kim, J.H.; Lee, S.-H.; Jang, T.C. Impact of the COVID-19 Outbreak on Adult out-of-Hospital Cardiac Arrest Outcomes in Daegu, South Korea: An Observational Study. Clin. Exp. Emerg. Med. 2021, 8, 137–144. [Google Scholar] [CrossRef]
- Baldi, E.; Sechi, G.M.; Mare, C.; Canevari, F.; Brancaglione, A.; Primi, R.; Klersy, C.; Palo, A.; Contri, E.; Ronchi, V.; et al. COVID-19 Kills at Home: The Close Relationship between the Epidemic and the Increase of out-of-Hospital Cardiac Arrests. Eur. Heart J. 2020, 41, 3045–3054. [Google Scholar] [CrossRef]
- Ball, J.; Nehme, Z.; Bernard, S.; Stub, D.; Stephenson, M.; Smith, K. Collateral Damage: Hidden Impact of the COVID-19 Pandemic on the out-of-Hospital Cardiac Arrest System-of-Care. Resuscitation 2020, 156, 157–163. [Google Scholar] [CrossRef]
- Fothergill, R.T.; Smith, A.L.; Wrigley, F.; Perkins, G.D. Out-of-Hospital Cardiac Arrest in London during the COVID-19 Pandemic. Resusc. Plus 2021, 5, 100066. [Google Scholar] [CrossRef]
- Glober, N.K.; Supples, M.; Faris, G.; Arkins, T.; Christopher, S.; Fulks, T.; Rayburn, D.; Weinstein, E.; Liao, M.; O’Donnell, D.; et al. Out-of-Hospital Cardiac Arrest Volumes and Characteristics during the COVID-19 Pandemic. Am. J. Emerg. Med. 2021, 48, 191–197. [Google Scholar] [CrossRef]
- Lim, S.L.; Shahidah, N.; Saffari, S.E.; Ng, Q.X.; Ho, A.F.W.; Leong, B.S.-H.; Arulanandam, S.; Siddiqui, F.J.; Ong, M.E.H. Impact of COVID-19 on Out-of-Hospital Cardiac Arrest in Singapore. Int. J. Environ. Res. Public. Health 2021, 18, 3646. [Google Scholar] [CrossRef]
- Lim, Z.J.; Ponnapa Reddy, M.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and Outcome of Out-of-Hospital Cardiac Arrests in the COVID-19 Era: A Systematic Review and Meta-Analysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef]
- Marijon, E.; Karam, N.; Jost, D.; Perrot, D.; Frattini, B.; Derkenne, C.; Sharifzadehgan, A.; Waldmann, V.; Beganton, F.; Narayanan, K.; et al. Out-of-Hospital Cardiac Arrest during the COVID-19 Pandemic in Paris, France: A Population-Based, Observational Study. Lancet Public Health 2020, 5, e437–e443. [Google Scholar] [CrossRef]
- McVaney, K.E.; Pepe, P.E.; Maloney, L.M.; Bronsky, E.S.; Crowe, R.P.; Augustine, J.J.; Gilliam, S.O.; Asaeda, G.H.; Eckstein, M.; Mattu, A.; et al. The Relationship of Large City Out-of-Hospital Cardiac Arrests and the Prevalence of COVID-19. EClinicalMedicine 2021, 34, 100815. [Google Scholar] [CrossRef]
- Talikowska, M.; Ball, S.; Tohira, H.; Bailey, P.; Rose, D.; Brink, D.; Bray, J.; Finn, J. No Apparent Effect of the COVID-19 Pandemic on out-of-Hospital Cardiac Arrest Incidence and Outcome in Western Australia. Resusc. Plus 2021, 8, 100183. [Google Scholar] [CrossRef]
- Uy-Evanado, A.; Chugh, H.S.; Sargsyan, A.; Nakamura, K.; Mariani, R.; Hadduck, K.; Salvucci, A.; Jui, J.; Chugh, S.S.; Reinier, K. Out-of-Hospital Cardiac Arrest Response and Outcomes during the COVID-19 Pandemic. JACC Clin. Electrophysiol. 2021, 7, 6–11. [Google Scholar] [CrossRef]
- Borkowska, M.J.; Smereka, J.; Safiejko, K.; Nadolny, K.; Maslanka, M.; Filipiak, K.J.; Jaguszewski, M.J.; Szarpak, L. Out-of-Hospital Cardiac Arrest Treated by Emergency Medical Service Teams during COVID-19 Pandemic: A Retrospective Cohort Study. Cardiol. J. 2021, 28, 15–22. [Google Scholar] [CrossRef]
- Hawranek, M.; Grygier, M.; Bujak, K.; Bartuś, S.; Gierlotka, M.; Wojakowski, W.; Legutko, J.; Lesiak, M.; Pączek, P.; Kleinrok, A.; et al. Characteristics of Patients from the Polish Registry of Acute Coronary Syndromes during the COVID-19 Pandemic: The First Report. Kardiol. Pol. 2021, 79, 192–195. [Google Scholar] [CrossRef]
- Ratajczak, J.; Łach, P.; Szczerbiński, S.; Paciorek, P.; Karłowska-Pik, J.; Ziemkiewicz, B.; Jasiewicz, M.; Kubica, A. Atmospheric Conditions and the Occurrence of Out-of-Hospital Cardiac Arrest in Poland—Preliminary Analysis of Poorly Understood Phenomena. Med. Res. J. 2018, 3, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Kubica, A.; Szczerbiński, S.; Kieszkowska, M.; Świątkiewicz, I.; Paciorek, P. Wpływ czynników klimatycznych i chronologicznych na występowanie ostrych incydentów chorobowych. Folia Cardiol. 2014, 9, 263–266. [Google Scholar]
- Kim, J.-H.; Hong, J.; Jung, J.; Im, J.-S. Effect of Meteorological Factors and Air Pollutants on Out-of-Hospital Cardiac Arrests: A Time Series Analysis. Heart Br. Card. Soc. 2020, 106, 1218–1227. [Google Scholar] [CrossRef]
- Gentile, F.R.; Primi, R.; Baldi, E.; Compagnoni, S.; Mare, C.; Contri, E.; Reali, F.; Bussi, D.; Facchin, F.; Currao, A.; et al. Out-of-Hospital Cardiac Arrest and Ambient Air Pollution: A Dose-Effect Relationship and an Association with OHCA Incidence. PLoS ONE 2021, 16, e0256526. [Google Scholar] [CrossRef]
- Szczerbinski, S.; Ratajczak, J.; Lach, P.; Rzeszuto, J.; Paciorek, P.; Karlowska-Pik, J.; Ziemkiewicz, B.; Jasiewicz, M.; Kubica, A. Epidemiology and Chronobiology of Out-of-Hospital Cardiac Arrest in a Subpopulation of Southern Poland: A Two-Year Observation. Cardiol. J. 2020, 27, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Szczerbiński, S.; Ratajczak, J.; Jasiewicz, M.; Kubica, A. Observational AnalysiS of Out-of-Hospital Cardiac Arrest OccurRence and Temporal Variability Patterns in Subpopulation of Southern POLand from 2006 to 2018: OSCAR-POL Registry. Cardiol. J. ahead of print. 2021. [Google Scholar] [CrossRef]
- Paciorek, P.; Obońska, K.; Skrzyński, W.; Ratajczak, J. Observational, Retrospective Study Evaluating the Temporal Variability of out-of-Hospital Cardiac Arrests (OHCA) in the District of Bydgoszcz in a 24-Month Period. Med. Res. J. 2021, 6, 217–223. [Google Scholar] [CrossRef]
- Onozuka, D.; Hagihara, A. Extreme Influenza Epidemics and Out-of-Hospital Cardiac Arrest. Int. J. Cardiol. 2018, 263, 158–162. [Google Scholar] [CrossRef]
- Rashid, M.; Gale, C.P.; Curzen, N.; Ludman, P.; De Belder, M.; Timmis, A.; Mohamed, M.O.; Lüscher, T.F.; Hains, J.; Wu, J.; et al. Impact of COVID19 Pandemic on the Incidence and Management of Out of Hospital Cardiac Arrest in Patients Presenting with Acute Myocardial Infarction in England. J. Am. Heart Assoc. 2020, 9, e018379. [Google Scholar] [CrossRef]
- Lai, P.H.; Lancet, E.A.; Weiden, M.D.; Webber, M.P.; Zeig-Owens, R.; Hall, C.B.; Prezant, D.J. Characteristics Associated with Out-of-Hospital Cardiac Arrests and Resuscitations During the Novel Coronavirus Disease 2019 Pandemic in New York City. JAMA Cardiol. 2020, 5, 1154–1163. [Google Scholar] [CrossRef]
- Mathew, S.; Harrison, N.; Chalek, A.D.; Gorelick, D.; Brennan, E.; Wise, S.; Gandolfo, L.; O’Neil, B.; Dunne, R. Effects of the COVID-19 Pandemic on out-of-Hospital Cardiac Arrest Care in Detroit. Am. J. Emerg. Med. 2021, 46, 90–96. [Google Scholar] [CrossRef]
- Baldi, E.; Auricchio, A.; Klersy, C.; Burkart, R.; Benvenuti, C.; Vanetta, C.; Bärtschi, J. SWISSRECA researchers Out-of-Hospital Cardiac Arrests and Mortality in Swiss Cantons with High and Low COVID-19 Incidence: A Nationwide Analysis. Resusc. Plus 2021, 6, 100105. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Brischigliaro, L.; Scquizzato, T.; Favaretto, A.; Spagna, A. Out-of-Hospital Cardiac Arrest during the COVID-19 Pandemic in the Province of Padua, Northeast Italy. Resuscitation 2020, 154, 47–49. [Google Scholar] [CrossRef] [PubMed]
- Baldi, E.; Primi, R.; Bendotti, S.; Currao, A.; Compagnoni, S.; Gentile, F.R.; Sechi, G.M.; Mare, C.; Palo, A.; Contri, E.; et al. Relationship between Out-of-Hospital Cardiac Arrests and COVID-19 during the First and Second Pandemic Wave. The Importance of Monitoring COVID-19 Incidence. PLoS ONE 2021, 16, e0260275. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.-H.; Liu, C.-Y.; Chen, W.-K.; Yu, S.-H.; Huang, F.-W.; Yang, M.-T.; Chen, C.-Y.; Shih, H.-M. Impact of the COVID-19 Pandemic on Emergency Medical Service Response to out-of-Hospital Cardiac Arrests in Taiwan: A Retrospective Observational Study. Emerg. Med. J. 2021, 38, 679–684. [Google Scholar] [CrossRef]
- Nadolny, K.; Zyśko, D.; Obremska, M.; Wierzbik-Strońska, M.; Ładny, J.R.; Podgórski, M.; Gałązkowski, R. Analysis of Out-of-Hospital Cardiac Arrest in Poland in a 1-Year Period: Data from the POL-OHCA Registry. Kardiol. Pol. 2020, 78, 404–411. [Google Scholar] [CrossRef] [Green Version]
- Gach, D.; Nowak, J.U.; Krzych, Ł.J. Epidemiology of Out-of-Hospital Cardiac Arrest in the Bielsko-Biala District: A 12-Month Analysis. Kardiol. Pol. 2016, 74, 1180–1187. [Google Scholar] [CrossRef]
- Kubica, J.; Ostrowska, M.; Stolarek, W.; Kasprzak, M.; Grzelakowska, K.; Kryś, J.; Kubica, A.; Adamski, P.; Podhajski, P.; Navarese, E.P.; et al. Impact of COVID-19 Pandemic on Acute Heart Failure Admissions and Mortality: A Multicentre Study (COV-HF-SIRIO 6 Study). ESC Heart Fail. 2021, 9, 721–728. [Google Scholar] [CrossRef]
- Al-Wathinani, A.; Hertelendy, A.J.; Alhurishi, S.; Mobrad, A.; Alhazmi, R.; Altuwaijri, M.; Alanazi, M.; Alotaibi, R.; Goniewicz, K. Increased Emergency Calls during the COVID-19 Pandemic in Saudi Arabia: A National Retrospective Study. Healthcare 2020, 9, 14. [Google Scholar] [CrossRef]
- Lackowski, P.; Piasecki, M.; Kasprzak, M.; Kryś, J.; Niezgoda, P.; Kubica, J. COVID-19 Pandemic Year in the Cardiology Department. Med. Res. J. 2021, 6, 40–46. [Google Scholar] [CrossRef]
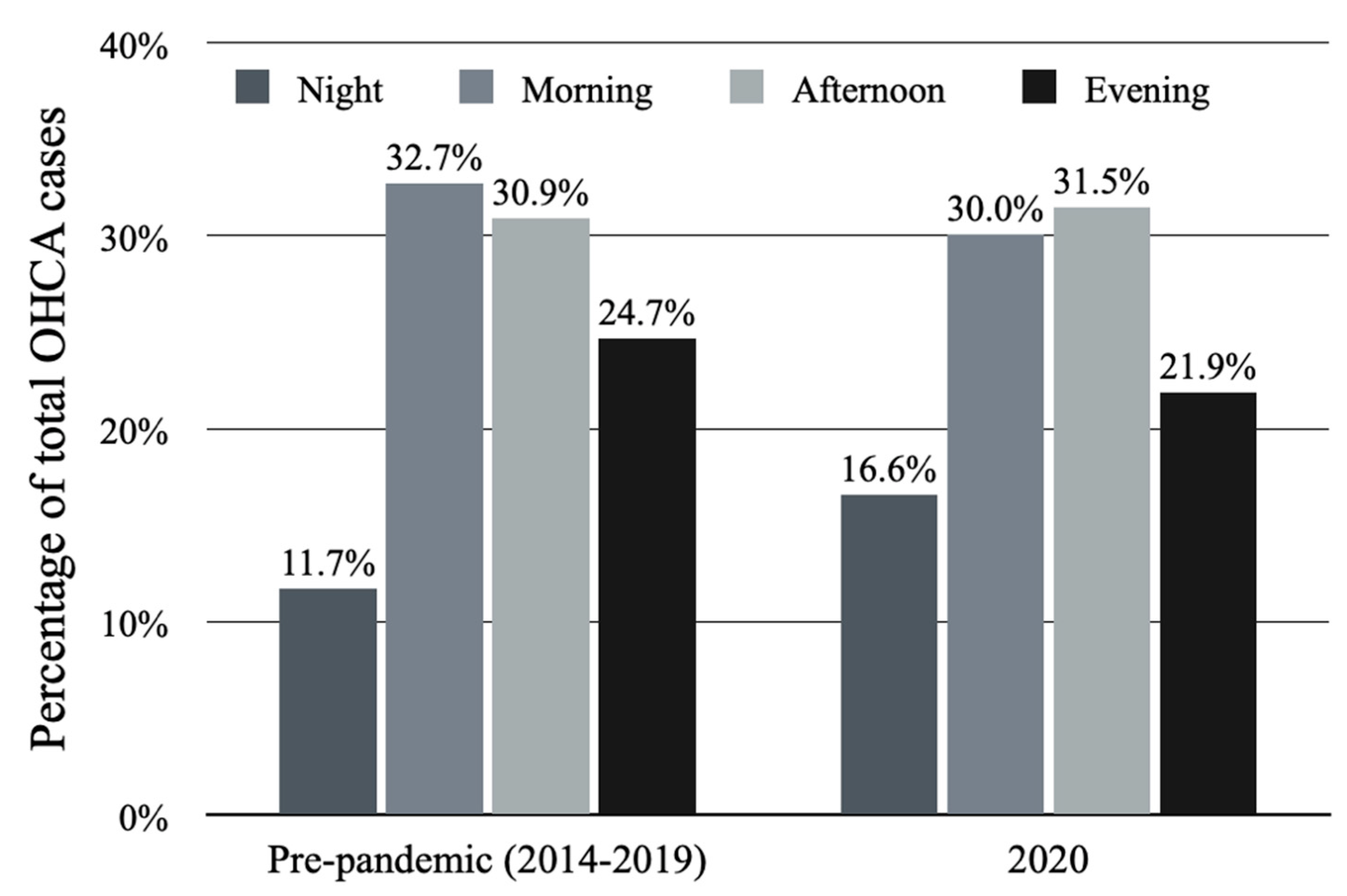

| Temporal Variables | 2020 Mean ± SD | Pre-Pandemic Period (2014–2019) Mean ± SD | p-Value |
|---|---|---|---|
| Time of the day | |||
| Night | 1.06 ± 1.12 | 1.64 ± 1.21 | 0.001 |
| Morning | 2.96 ± 1.85 | 2.98 ± 1.70 | 0.80 |
| Afternoon | 2.79 ± 1.67 | 3.12 ± 1.81 | 0.35 |
| Evening | 2.23 ± 1.68 | 2.17 ± 1.59 | 0.96 |
| Day of the week | |||
| Monday | 0.87 ± 0.95 | 1.08 ± 1.12 | 0.24 |
| Tuesday | 1.04 ± 0.99 | 0.98 ± 1.10 | 0.47 |
| Wednesday | 1.19 ± 1.18 | 0.98 ± 1.11 | 0.17 |
| Thursday | 1.08 ± 1.11 | 1.04 ± 1.08 | 0.85 |
| Friday | 1.35 ± 1.12 | 1.11 ± 1.11 | 0.12 |
| Saturday | 1.17 ± 1.17 | 1.05 ± 1.22 | 0.36 |
| Sunday | 1.27 ± 0.93 | 1.03 ± 1.15 | 0.026 |
| Month of the year | |||
| January | 1.16 ± 1.16 | 1.20 ± 1.21 | 0.95 |
| February | 0.90 ± 0.82 | 1.08 ± 1.09 | 0.58 |
| March | 1.03 ± 1.11 | 1.13 ± 1.22 | 0.81 |
| April | 1.03 ± 0.93 | 0.96 ± 1.03 | 0.51 |
| May | 1.35 ± 1.14 | 0.97 ± 0.99 | 0.06 |
| June | 1.03 ± 1.03 | 1.07 ± 1.13 | 0.99 |
| July | 0.94 ± 1.03 | 0.76 ± 1.06 | 0.29 |
| August | 0.90 ± 1.04 | 1.02 ± 1.16 | 0.66 |
| September | 0.87 ± 0.94 | 1.03 ± 1.18 | 0.65 |
| October | 1.48 ± 1.12 | 0.96 ± 0.99 | 0.009 |
| November | 1.83 ± 1.15 | 1.15 ± 1.13 | 0.002 |
| December | 1.10 ± 1.04 | 1.15 ± 1.27 | 0.89 |
| Season of the year | |||
| Spring | 1.14 ± 1.07 | 1.02 ± 1.08 | 0.22 |
| Summer | 0.96 ± 1.03 | 0.95 ± 1.12 | 0.73 |
| Autumn | 1.40 ± 1.13 | 1.05 ± 1.1 | 0.003 |
| Winter | 1.05 ± 1.02 | 1.14 ± 1.19 | 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ratajczak, J.; Szczerbiński, S.; Kubica, A. Occurrence and Temporal Variability of Out-of-Hospital Cardiac Arrest during COVID-19 Pandemic in Comparison to the Pre-Pandemic Period in Poland—Observational Analysis of OSCAR-POL Registry. J. Clin. Med. 2022, 11, 4143. https://doi.org/10.3390/jcm11144143
Ratajczak J, Szczerbiński S, Kubica A. Occurrence and Temporal Variability of Out-of-Hospital Cardiac Arrest during COVID-19 Pandemic in Comparison to the Pre-Pandemic Period in Poland—Observational Analysis of OSCAR-POL Registry. Journal of Clinical Medicine. 2022; 11(14):4143. https://doi.org/10.3390/jcm11144143
Chicago/Turabian StyleRatajczak, Jakub, Stanisław Szczerbiński, and Aldona Kubica. 2022. "Occurrence and Temporal Variability of Out-of-Hospital Cardiac Arrest during COVID-19 Pandemic in Comparison to the Pre-Pandemic Period in Poland—Observational Analysis of OSCAR-POL Registry" Journal of Clinical Medicine 11, no. 14: 4143. https://doi.org/10.3390/jcm11144143
APA StyleRatajczak, J., Szczerbiński, S., & Kubica, A. (2022). Occurrence and Temporal Variability of Out-of-Hospital Cardiac Arrest during COVID-19 Pandemic in Comparison to the Pre-Pandemic Period in Poland—Observational Analysis of OSCAR-POL Registry. Journal of Clinical Medicine, 11(14), 4143. https://doi.org/10.3390/jcm11144143






