Social Determinants of Stroke Hospitalization and Mortality in United States’ Counties
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Outcome Measures
2.2. Data Elements
2.3. Statistical Analysis
3. Results
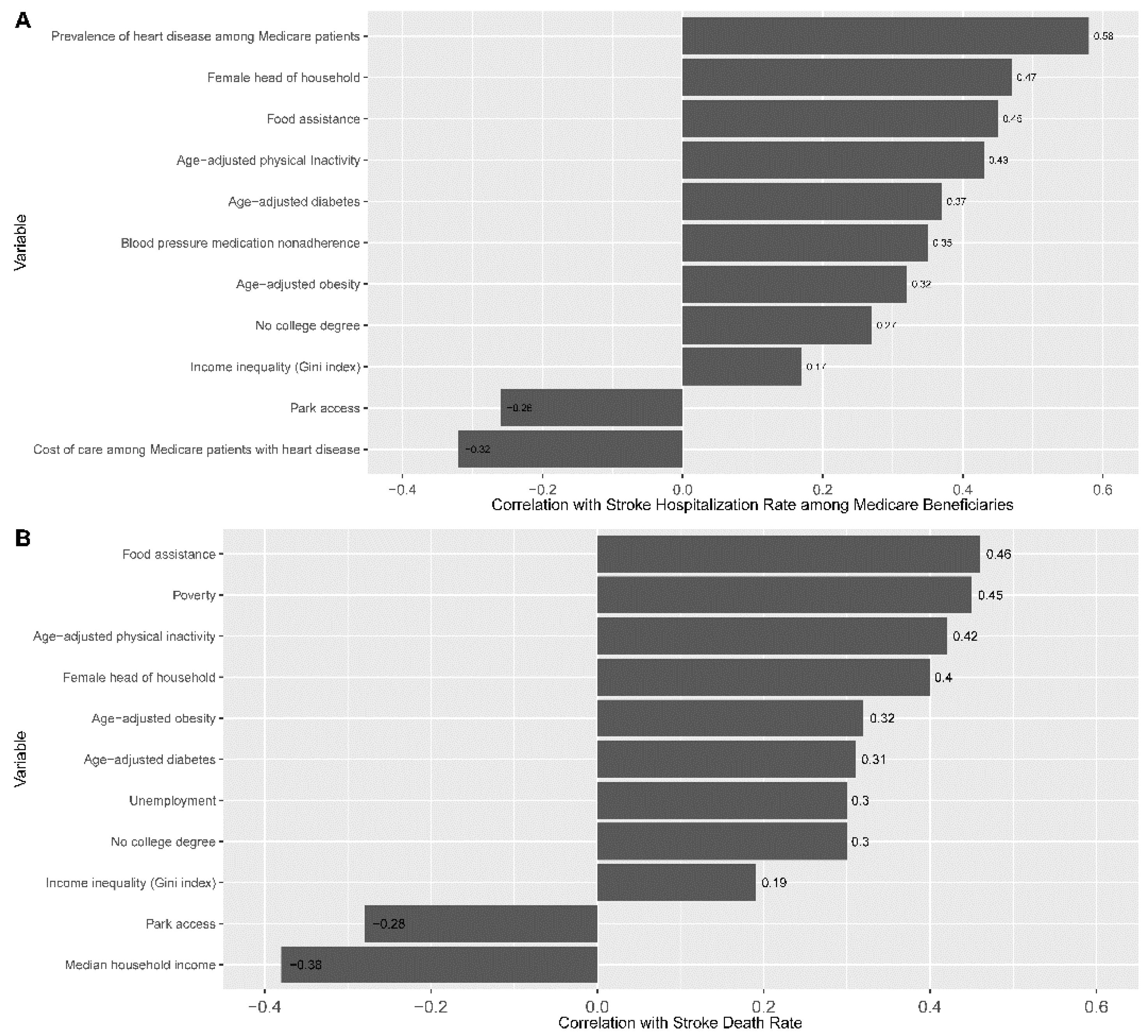
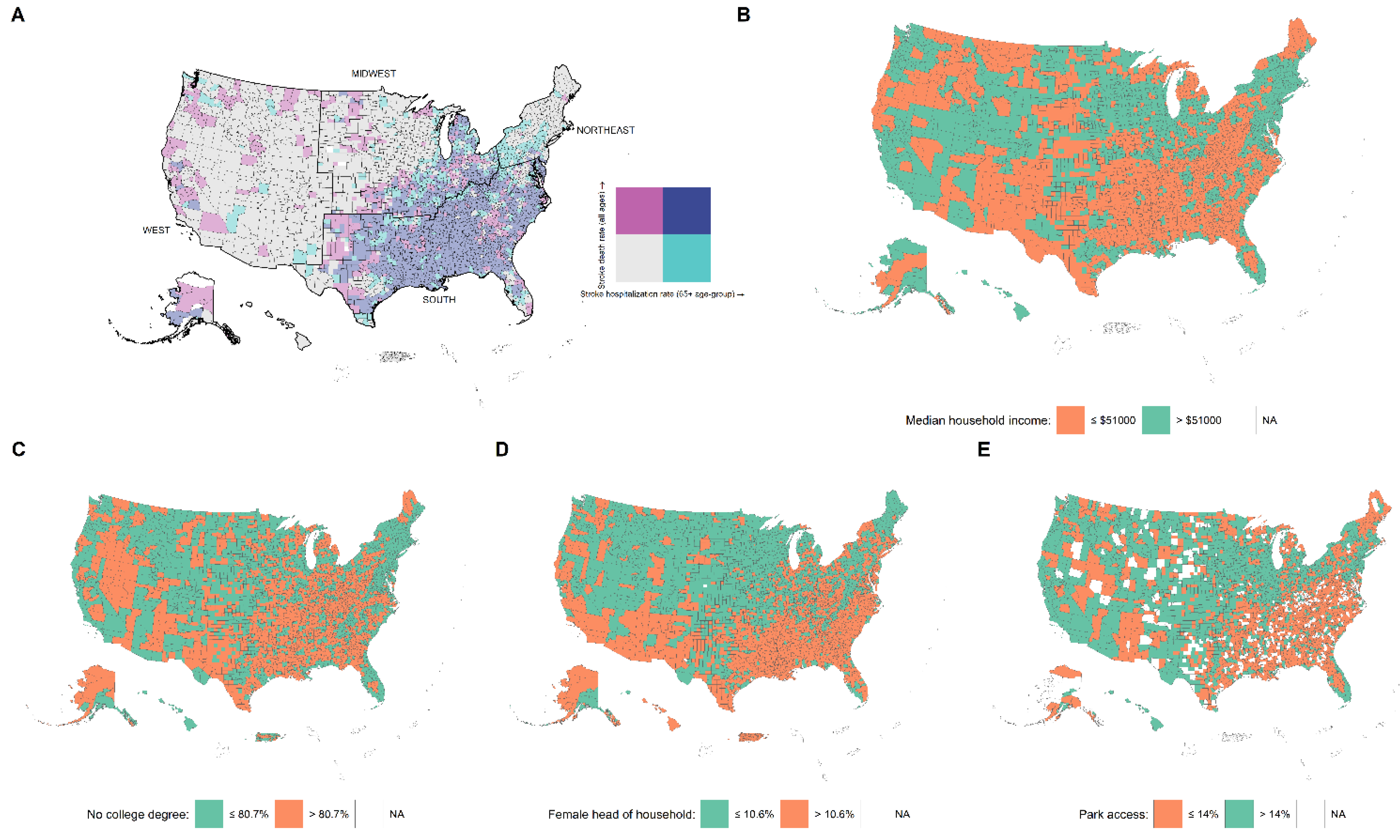
3.1. Social Determinants and Their Correlation with Outcomes
3.2. Comparison between Counties with Low vs. High Rate of Outcomes
3.3. Social Determinants Associated with Stroke Hospitalization Rate (SHR)
3.4. Social Determinants Associated with Stroke Death Rate (SDR)
3.5. Variations in Stroke Outcomes and Social Determinants by the US Census Regions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S.; Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Avendano, M.; Kawachi, I.; Van Lenthe, F.; Boshuizen, H.C.; Mackenbach, J.P.; Van den Bos, G.A.; Fay, M.E.; Berkman, L.F. Socioeconomic status and stroke incidence in the US elderly: The role of risk factors in the EPESE study. Stroke 2006, 37, 1368–1373. [Google Scholar] [CrossRef] [PubMed]
- Avendano, M.; Glymour, M.M. Stroke disparities in older Americans: Is wealth a more powerful indicator of risk than income and education? Stroke 2008, 39, 1533–1540. [Google Scholar] [CrossRef]
- Bettger, J.P.; Zhao, X.; Bushnell, C.; Zimmer, L.; Pan, W.; Williams, L.S.; Peterson, E.D. The association between socioeconomic status and disability after stroke: Findings from the Adherence eValuation After Ischemic stroke Longitudinal (AVAIL) registry. BMC Public Health 2014, 14, 281. [Google Scholar] [CrossRef]
- Hanchate, A.D.; Schwamm, L.H.; Huang, W.; Hylek, E.M. Comparison of ischemic stroke outcomes and patient and hospital characteristics by race/ethnicity and socioeconomic status. Stroke 2013, 44, 469–476. [Google Scholar] [CrossRef]
- Howard, V.J.; McClure, L.A.; Kleindorfer, D.O.; Cunningham, S.A.; Thrift, A.G.; Diez Roux, A.V.; Howard, G. Neighborhood socioeconomic index and stroke incidence in a national cohort of blacks and whites. Neurology 2016, 87, 2340–2347. [Google Scholar] [CrossRef]
- Pedigo, A.; Aldrich, T.; Odoi, A. Neighborhood disparities in stroke and myocardial infarction mortality: A GIS and spatial scan statistics approach. BMC Public Health 2011, 11, 644. [Google Scholar] [CrossRef]
- Brown, A.F.; Liang, L.J.; Vassar, S.D.; Stein-Merkin, S.; Longstreth, W.T., Jr.; Ovbiagele, B.; Yan, T.; Escarce, J.J. Neighborhood disadvantage and ischemic stroke: The Cardiovascular Health Study (CHS). Stroke 2011, 42, 3363–3368. [Google Scholar] [CrossRef]
- Schieb, L.; Mobley, L.; George, M.; Casper, M. Tracking stroke hospitalization clusters over time and associations with county-level socioeconomic and healthcare characteristics. Stroke 2013, 44, 146–152. [Google Scholar] [CrossRef]
- Kulick, E.R.; Wellenius, G.A.; Boehme, A.K.; Sacco, R.L.; Elkind, M.S. Residential Proximity to Major Roadways and Risk of Incident Ischemic Stroke in NOMAS (The Northern Manhattan Study). Stroke 2018, 49, 835–841. [Google Scholar] [CrossRef]
- Sergeev, A.V. Racial and rural-urban disparities in stroke mortality outside the Stroke Belt. Ethn. Dis. 2011, 21, 307–313. [Google Scholar] [CrossRef]
- Clark, C.J.; Guo, H.; Lunos, S.; Aggarwal, N.T.; Beck, T.; Evans, D.A.; Mendes de Leon, C.; Everson-Rose, S.A. Neighborhood cohesion is associated with reduced risk of stroke mortality. Stroke 2011, 42, 1212–1217. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Interactive Atlas of Heart Disease and Stroke. Available online: http://nccd.cdc.gov/DHDSPAtlas (accessed on 9 April 2021).
- Yang, J.; Zaitlen, N.A.; Goddard, M.E.; Visscher, P.M.; Price, A.L. Advantages and pitfalls in the application of mixed-model association methods. Nat. Genet. 2014, 46, 100–106. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 7 July 2021).
- Li, C.; Hedblad, B.; Rosvall, M.; Buchwald, F.; Khan, F.A.; Engstrom, G. Stroke incidence, recurrence, and case-fatality in relation to socioeconomic position: A population-based study of middle-aged Swedish men and women. Stroke 2008, 39, 2191–2196. [Google Scholar] [CrossRef]
- Gezmu, T.; Gizzi, M.; Kirmani, J.; Schneider, D.; Moussavi, M. Disparities in acute stroke severity, outcomes, and care relative to health insurance status. J. Stroke Cerebrovasc. Dis. 2014, 23, e93–e98. [Google Scholar] [CrossRef]
- James, M.L.; Grau-Sepulveda, M.V.; Olson, D.M.; Smith, E.E.; Hernandez, A.F.; Peterson, E.D.; Schwamm, L.H.; Bhatt, D.L.; Fonarow, G.C. Insurance status and outcome after intracerebral hemorrhage: Findings from Get With The Guidelines-stroke. J. Stroke Cerebrovasc. Dis. 2014, 23, 283–292. [Google Scholar] [CrossRef]
- Shen, J.; Washington, E. Disparities in outcomes among patients with stroke associated with insurance status. Stroke 2007, 38, 1010–1016. [Google Scholar] [CrossRef]
- Bravata, D.M.; Wells, C.K.; Gulanski, B.; Kernan, W.N.; Brass, L.M.; Long, J.; Concato, J. Racial disparities in stroke risk factors: The impact of socioeconomic status. Stroke 2005, 36, 1507–1511. [Google Scholar] [CrossRef]
- Vivanco-Hidalgo, R.M.; Ribera, A.; Abilleira, S. Association of Socioeconomic Status With Ischemic Stroke Survival. Stroke 2019, 50, 3400–3407. [Google Scholar] [CrossRef]
- Morovatdar, N.; Thrift, A.G.; Stranges, S.; Kapral, M.; Behrouz, R.; Amiri, A.; Heshmati, A.; Ghahremani, A.; Farzadfard, M.T.; Mokhber, N.; et al. Socioeconomic Status and Long-Term Stroke Mortality, Recurrence and Disability in Iran: The Mashhad Stroke Incidence Study. Neuroepidemiology 2019, 53, 27–31. [Google Scholar] [CrossRef]
- Saposnik, G.; Jeerakathil, T.; Selchen, D.; Baibergenova, A.; Hachinski, V.; Kapral, M.K.; Stroke Outcome Research Canada Working Group. Socioeconomic status, hospital volume, and stroke fatality in Canada. Stroke 2008, 39, 3360–3366. [Google Scholar] [CrossRef]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef]
- Marshall, I.J.; Wang, Y.; Crichton, S.; McKevitt, C.; Rudd, A.G.; Wolfe, C.D. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015, 14, 1206–1218. [Google Scholar] [CrossRef]
- Chen, R.; Crichton, S.; McKevitt, C.; Rudd, A.G.; Sheldenkar, A.; Wolfe, C.D. Association between socioeconomic deprivation and functional impairment after stroke: The South London Stroke Register. Stroke 2015, 46, 800–805. [Google Scholar] [CrossRef]
- Addo, J.; Ayerbe, L.; Mohan, K.M.; Crichton, S.; Sheldenkar, A.; Chen, R.; Wolfe, C.D.; McKevitt, C. Socioeconomic status and stroke: An updated review. Stroke 2012, 43, 1186–1191. [Google Scholar] [CrossRef]
- Sturm, J.W.; Donnan, G.A.; Dewey, H.M.; Macdonell, R.A.; Gilligan, A.K.; Thrift, A.G. Determinants of handicap after stroke: The North East Melbourne Stroke Incidence Study (NEMESIS). Stroke 2004, 35, 715–720. [Google Scholar] [CrossRef]
- Grube, M.M.; Koennecke, H.C.; Walter, G.; Thummler, J.; Meisel, A.; Wellwood, I.; Heuschmann, P.U.; Berlin Stroke Register. Association between socioeconomic status and functional impairment 3 months after ischemic stroke: The Berlin Stroke Register. Stroke 2012, 43, 3325–3330. [Google Scholar] [CrossRef]
- Blank, N.; Diderichsen, F. Social inequalities in the experience of illness in Sweden: A “double suffering”. Scand. J. Soc. Med. 1996, 24, 81–89. [Google Scholar] [CrossRef]
- Claxton, J.S.; Lutsey, P.L.; MacLehose, R.F.; Chen, L.Y.; Lewis, T.T.; Alonso, A. Geographic Disparities in the Incidence of Stroke among Patients with Atrial Fibrillation in the United States. J. Stroke Cerebrovasc. Dis. 2019, 28, 890–899. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed]
- Wagner, P.; Duan, Y.P.; Zhang, R.; Wulff, H.; Brehm, W. Association of psychosocial and perceived environmental factors with park-based physical activity among elderly in two cities in China and Germany. BMC Public Health 2020, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Xian, Y.; Holloway, R.G.; Chan, P.S.; Noyes, K.; Shah, M.N.; Ting, H.H.; Chappel, A.R.; Peterson, E.D.; Friedman, B. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA 2011, 305, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Meretoja, A.; Roine, R.O.; Kaste, M.; Linna, M.; Roine, S.; Juntunen, M.; Erila, T.; Hillbom, M.; Marttila, R.; Rissanen, A.; et al. Effectiveness of primary and comprehensive stroke centers: PERFECT stroke: A nationwide observational study from Finland. Stroke 2010, 41, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.K.; Cordato, D.; O’Rourke, F.; Chan, D.L.; Pollack, M.; Middleton, S.; Levi, C. Comprehensive stroke units: A review of comparative evidence and experience. Int. J. Stroke 2013, 8, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.F.; Newcommon, N.N.; Cooper, M.E.; Green, T.L.; Seal, B.; Klein, G.; Weir, N.U.; Coutts, S.B.; Watson, T.; Barber, P.A.; et al. Impact of a stroke unit on length of hospital stay and in-hospital case fatality. Stroke 2009, 40, 18–23. [Google Scholar] [CrossRef]
- Foley, N.; Salter, K.; Teasell, R. Specialized stroke services: A meta-analysis comparing three models of care. Cerebrovasc. Dis. 2007, 23, 194–202. [Google Scholar] [CrossRef]
- Stroke Unit Trialists Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst. Rev. 2007, CD000197. [Google Scholar] [CrossRef]
- Lackland, D.T.; Roccella, E.J.; Deutsch, A.F.; Fornage, M.; George, M.G.; Howard, G.; Kissela, B.M.; Kittner, S.J.; Lichtman, J.H.; Lisabeth, L.D.; et al. Factors influencing the decline in stroke mortality: A statement from the American Heart Association/American Stroke Association. Stroke 2014, 45, 315–353. [Google Scholar] [CrossRef]
- El-Saed, A.; Kuller, L.H.; Newman, A.B.; Lopez, O.; Costantino, J.; McTigue, K.; Cushman, M.; Kronmal, R. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke 2006, 37, 1975–1979. [Google Scholar] [CrossRef]
- Liao, Y.; Greenlund, K.J.; Croft, J.B.; Keenan, N.L.; Giles, W.H. Factors explaining excess stroke prevalence in the US Stroke Belt. Stroke 2009, 40, 3336–3341. [Google Scholar] [CrossRef]
- Lanska, D.J. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology 1993, 43, 1839–1851. [Google Scholar] [CrossRef]
- Lanska, D.J.; Kuller, L.H. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke 1995, 26, 1145–1149. [Google Scholar] [CrossRef]
- Howard, V.J.; Kleindorfer, D.O.; Judd, S.E.; McClure, L.A.; Safford, M.M.; Rhodes, J.D.; Cushman, M.; Moy, C.S.; Soliman, E.Z.; Kissela, B.M.; et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann. Neurol. 2011, 69, 619–627. [Google Scholar] [CrossRef]
- Nguyen-Huynh, M.N.; Johnston, S.C. Regional variation in hospitalization for stroke among Asians/Pacific Islanders in the United States: A nationwide retrospective cohort study. BMC Neurol. 2005, 5, 21. [Google Scholar] [CrossRef]
- Lackland, D.T.; Bachman, D.L.; Carter, T.D.; Barker, D.L.; Timms, S.; Kohli, H. The geographic variation in stroke incidence in two areas of the southeastern stroke belt: The Anderson and Pee Dee Stroke Study. Stroke 1998, 29, 2061–2068. [Google Scholar] [CrossRef]
- Labarthe, D.R.; Howard, G.; Safford, M.M.; Howard, V.J.; Judd, S.E.; Cushman, M.; Kissela, B.M.; Reasons for Geographic and Racial Differences in Stroke Investigators. Incidence and Case Fatality at the County Level as Contributors to Geographic Disparities in Stroke Mortality. Neuroepidemiology 2016, 47, 96–102. [Google Scholar] [CrossRef]
- Morovatdar, N.; Avan, A.; Azarpazhooh, M.R.; Di Napoli, M.; Stranges, S.; Kapral, M.K.; Rezayat, A.A.; Shariatzadeh, A.; Abootalebi, S.; Mokhber, N.; et al. Secular trends of ischaemic heart disease, stroke, and dementia in high-income countries from 1990 to 2017: The Global Burden of Disease Study 2017. Neurol. Sci. 2021, 43, 255–264. [Google Scholar] [CrossRef]
- Blais, C.; Rochette, L. Trends in prevalence, incidence and mortality of diagnosed and silent coronary heart disease in Quebec. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2015, 35, 184–193. [Google Scholar] [CrossRef]
- Sposato, L.A.; Kapral, M.K.; Fang, J.; Gill, S.S.; Hackam, D.G.; Cipriano, L.E.; Hachinski, V. Declining Incidence of Stroke and Dementia: Coincidence or Prevention Opportunity? JAMA Neurol. 2015, 72, 1529–1531. [Google Scholar] [CrossRef][Green Version]
- Tu, J.V.; Nardi, L.; Fang, J.; Liu, J.; Khalid, L.; Johansen, H. National trends in rates of death and hospital admissions related to acute myocardial infarction, heart failure and stroke, 1994–2004. CMAJ Can. Med. Assoc. J. 2009, 180, E118–E125. [Google Scholar] [CrossRef]
- Kamal, N.; Lindsay, M.P.; Côté, R.; Fang, J.; Kapral, M.K.; Hill, M.D. Ten-year trends in stroke admissions and outcomes in Canada. Can. J. Neurol. Sci. 2015, 42, 168–175. [Google Scholar] [CrossRef]
- Tu, J.V.; Chu, A.; Maclagan, L.; Austin, P.C.; Johnston, S.; Ko, D.T.; Cheung, I.; Atzema, C.L.; Booth, G.L.; Bhatia, R.S.; et al. Regional variations in ambulatory care and incidence of cardiovascular events. CMAJ Can. Med. Assoc. J. 2017, 189, E494–E501. [Google Scholar] [CrossRef]
- Douthit, N.; Kiv, S.; Dwolatzky, T.; Biswas, S. Exposing some important barriers to health care access in the rural USA. Public Health 2015, 129, 611–620. [Google Scholar] [CrossRef]
- Trivedi, T.; Liu, J.; Probst, J.; Merchant, A.; Jhones, S.; Martin, A.B. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural Remote Health 2015, 15, 3267. [Google Scholar] [CrossRef]
- O’Connor, A.; Wellenius, G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012, 126, 813–820. [Google Scholar] [CrossRef]
- Baciu, A.; Negussie, Y.; Geller, A. The Root Causes of Health Inequity. In Communities in Action: Pathways to Health Equity; National Academies Press: Washington, DC, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK425845/ (accessed on 11 July 2021).
- Krieger, N. Structural Racism, Health Inequities, and the Two-Edged Sword of Data: Structural Problems Require Structural Solutions. Front. Public Health 2021, 9, 655447. [Google Scholar] [CrossRef]
- Carthon, J.M.B.; Brom, H.; McHugh, M.; Daus, M.; French, R.; Sloane, D.M.; Berg, R.; Merchant, R.; Aiken, L.H. Racial Disparities in Stroke Readmissions Reduced in Hospitals with Better Nurse Staffing. Nurs. Res. 2021, 71, 33–42. [Google Scholar] [CrossRef]
- Skolarus, L.E.; Sharrief, A.; Gardener, H.; Jenkins, C.; Boden-Albala, B. Considerations in Addressing Social Determinants of Health to Reduce Racial/Ethnic Disparities in Stroke Outcomes in the United States. Stroke 2020, 51, 3433–3439. [Google Scholar] [CrossRef]
- Khaw, K.T.; Barrett-Connor, E.; Suarez, L.; Criqui, M.H. Predictors of stroke-associated mortality in the elderly. Stroke 1984, 15, 244–248. [Google Scholar] [CrossRef]
- Lafta, R.K.; Hayawi, A.H.; Khudhairi, J.M. Medical and social problems among women headed families in Baghdad. Qatar Med. J. 2013, 2012, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Hunger and Poverty in Female-Headed Households. Available online: https://www.bread.org/sites/default/files/downloads/hunger-poverty-female-headed-households-may-2019.pdf (accessed on 10 May 2022).
- 2013–2017 ACS 5-year Estimates. Available online: https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2017/5-year.html (accessed on 10 May 2022).
- Tu, J.V.; Ko, D.T. Ecological Studies and Cardiovascular Outcomes Research. Circulation 2008, 118, 2588–2593. [Google Scholar] [CrossRef] [PubMed]
| Data Elements | Unit | Missing % | Overall | Low Hospitalization Rate (≤11.7) | High Hospitalization Rate (>11.7) | p-Value | Low Death Rate (≤ 39.0) | High Death Rate (>39.0) | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |||||
| Heart disease among Medicare beneficiaries | % | 0.1 | 35.6 (31.9, 39.5) | 32.7 (29.7, 36.0) | 38.5 (35.5, 41.6) | <0.001 | - | - | - |
| Blood pressure medication non-adherence (Medicare Part D beneficiaries) | % | 1.8 | 23.1 (19.8, 26.2) | 21.3 (18.2, 24.5) | 24.6 (21.5, 27.2) | <0.001 | - | - | - |
| Cost of care (per capita for Medicare beneficiaries diagnosed with heart disease) | USD | 0.3 | 3972.0 (3222.5, 5091.2) | 4510.0 (3402.5, 6013.8) | 3665.0 (3151.8, 4366.8) | <0.001 | - | - | - |
| Poverty | % | 2.6 | 14.1 (10.8, 18.3) | - | - | - | 12.2 (9.6, 15.1) | 16.5 (13.1, 20.8) | <0.001 |
| Unemployment | % | 0.2 | 3.9 (3.1, 4.9) | - | - | - | 3.6 (2.9, 4.7) | 4.1 (3.5, 5.1) | <0.001 |
| Household income | USD | 2.6 | 51,000.0 (44,000.0, 59,000.0) | - | - | - | 55,000.0 (48,000.0, 63,000.0) | 46,000.0 (41,000.0, 53,000.0) | <0.001 |
| Income inequality (Gini index) | % | 0.2 | 0.4 (0.4, 0.5) | 0.4 (0.4, 0.5) | 0.4 (0.4, 0.5) | <0.001 | 0.4 (0.4, 0.5) | 0.5 (0.4, 0.5) | <0.001 |
| Food assistance | % | 2.6 | 12.9 (8.6, 17.9) | 9.8 (6.6, 14.1) | 15.7 (12.2, 20.3) | <0.001 | 10.2 (6.9, 14.6) | 15.5 (11.6, 20.4) | <0.001 |
| Female head of household | % | 0.2 | 10.6 (8.4, 13.4) | 9.1 (7.1, 11.5) | 12.0 (10.0, 14.7) | <0.001 | 9.4 (7.5, 11.7) | 12.0 (9.6, 14.9) | <0.001 |
| No college degree | % | 0.2 | 80.7 (74.5, 84.9) | 78.6 (71.6, 82.5) | 83.3 (77.7, 86.6) | <0.001 | 78.3 (70.7, 82.6) | 83.1 (78.2, 86.5) | <0.001 |
| Park access | % | 2.7 | 14.0 (4.0, 30.0) | 22.0 (8.0, 38.0) | 9.0 (2.0, 21.0) | <0.001 | 22.0 (8.0, 38.0) | 9.0 (2.0, 21.0) | <0.001 |
| Age-adjusted physical inactivity | % | 2.6 | 25.9 (22.5, 29.6) | 24.0 (20.6, 27.0) | 28.1 (24.8, 31.9) | <0.001 | 24.0 (20.7, 27.0) | 28.1 (24.8, 31.8) | <0.001 |
| Age-adjusted obesity | % | 2.6 | 33.0 (28.9, 36.6) | 31.0 (27.0, 34.8) | 34.6 (31.3, 37.9) | <0.001 | 31.5 (27.5, 35.0) | 34.4 (30.7, 38.0) | <0.001 |
| Age-adjusted diabetes | % | 0.2 | 10.0 (7.8, 12.7) | 8.6 (6.9, 10.8) | 11.5 (9.4, 13.9) | <0.001 | 8.8 (7.1, 11.0) | 11.3 (9.0, 13.9) | <0.001 |
| n (%) | n (%) | n (%) | n (%) | n (%) | |||||
| Hospitals with Neurological services | % | 0.1 | 927 (28.8) | 441 (27.0) | 486 (31.1) | 0.012 | 521 (32.0) | 406 (25.6) | <0.001 |
| Hospital present | % | 0.1 | 2482 (77.0) | 1296 (79.2) | 1179 (75.3) | 0.010 | 1278 (78.5) | 1202 (75.8) | 0.068 |
| Unadjusted OR | Adjusted OR | |||
|---|---|---|---|---|
| Variable | OR with 95% CI | p-Value | OR with 95% CI | p-Value |
| Prevalence of heart disease among Medicare patients | 2.55 (2.18–2.99) | <0.001 | 2.03 (1.66–2.49) | <0.001 |
| Blood pressure medication nonadherence | 2.88 (2.34–3.54) | <0.001 | 2.02 (1.5–2.73) | <0.001 |
| Cost of care among Medicare patients with heart disease | 0.6 (0.52–0.68) | <0.001 | 0.5 (0.42–0.6) | <0.001 |
| Hospital with neurological services | 1.22 (0.99–1.5) | 0.062 | 1.9 (1.41–2.57) | <0.001 |
| Age-adjusted obesity | 1.83 (1.64–2.04) | <0.001 | 1.24 (1.06–1.44) | 0.006 |
| Female head of household | 2.01 (1.76–2.29) | <0.001 | 1.32 (1.04–1.67) | 0.021 |
| Hospital present | 0.7 (0.56–0.89) | 0.003 | 0.69 (0.5–0.95) | 0.025 |
| No college degree | 1.39 (1.25–1.54) | <0.001 | 1.13 (0.94–1.36) | 0.189 |
| Park access | 0.85 (0.76–0.95) | 0.004 | 0.91 (0.78–1.06) | 0.224 |
| Age-adjusted physical inactivity | 1.86 (1.64–2.11) | <0.001 | 1.08 (0.9–1.3) | 0.426 |
| Food assistance | 2.02 (1.78–2.3) | <0.001 | 1.09 (0.87–1.37) | 0.453 |
| Age-adjusted diabetes | 1.47 (1.31–1.64) | <0.001 | 1 (0.86–1.15) | 0.977 |
| Income inequality (Gini index) | 1.04 (0.94–1.16) | 0.47 | ||
| Unadjusted OR | Adjusted OR | |||
|---|---|---|---|---|
| Variable | OR with 95% CI | p-Value | OR with 95% CI | p-Value |
| Median household income | 0.62 (0.56–0.69) | <0.001 | 0.69 (0.57–0.83) | <0.001 |
| Park access | 0.81 (0.73–0.9) | <0.001 | 0.85 (0.74–0.98) | 0.023 |
| No college degree | 1.44 (1.3–1.59) | <0.001 | 1.24 (1.03–1.5) | 0.024 |
| Poverty | 1.83 (1.63–2.04) | <0.001 | - | - |
| Age-adjusted diabetes | 1.25 (1.13–1.39) | <0.001 | 0.9 (0.79–1.03) | 0.121 |
| Food assistance | 1.94 (1.71–2.19) | <0.001 | - | - |
| Age-adjusted physical inactivity | 1.71 (1.52–1.92) | <0.001 | 1.13 (0.95–1.33) | 0.174 |
| Unemployment | 1.63 (1.44–1.84) | <0.001 | 1.05 (0.89–1.25) | 0.554 |
| Female head of household | 1.49 (1.32–1.68) | <0.001 | 0.98 (0.8–1.19) | 0.821 |
| Income inequality (Gini index) | 1.17 (1.05–1.29) | 0.003 | 1.04 (0.9–1.2) | 0.620 |
| Age-adjusted obesity | 1.46 (1.32–1.62) | <0.001 | 1.03 (0.89–1.19) | 0.713 |
| Hospital with neurological services | 0.71 (0.58–0.86) | 0.001 | 1.00 (0.76–1.31) | 0.985 |
| Hospital present | 0.92 (0.74–1.15) | 0.471 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yadav, R.S.; Chaudhary, D.; Avula, V.; Shahjouei, S.; Azarpazhooh, M.R.; Abedi, V.; Li, J.; Zand, R. Social Determinants of Stroke Hospitalization and Mortality in United States’ Counties. J. Clin. Med. 2022, 11, 4101. https://doi.org/10.3390/jcm11144101
Yadav RS, Chaudhary D, Avula V, Shahjouei S, Azarpazhooh MR, Abedi V, Li J, Zand R. Social Determinants of Stroke Hospitalization and Mortality in United States’ Counties. Journal of Clinical Medicine. 2022; 11(14):4101. https://doi.org/10.3390/jcm11144101
Chicago/Turabian StyleYadav, Randhir Sagar, Durgesh Chaudhary, Venkatesh Avula, Shima Shahjouei, Mahmoud Reza Azarpazhooh, Vida Abedi, Jiang Li, and Ramin Zand. 2022. "Social Determinants of Stroke Hospitalization and Mortality in United States’ Counties" Journal of Clinical Medicine 11, no. 14: 4101. https://doi.org/10.3390/jcm11144101
APA StyleYadav, R. S., Chaudhary, D., Avula, V., Shahjouei, S., Azarpazhooh, M. R., Abedi, V., Li, J., & Zand, R. (2022). Social Determinants of Stroke Hospitalization and Mortality in United States’ Counties. Journal of Clinical Medicine, 11(14), 4101. https://doi.org/10.3390/jcm11144101








