Characterization of Cognitive, Language and Adaptive Profiles of Children and Adolescents with Malan Syndrome
Abstract
:1. Introduction
- -
- Generalized overgrowth. MS individuals may present with prenatal overgrowth resulting as Large for Gestational Age (LGA) newborns with birth weight >2 standard deviations (SDS) in 14.6% of cases. More frequently, they may present with a post-natal overgrowth, typically in childhood and adolescence, with a height >2 SDS reported in 56% of patients. Final height during adulthood is less marked, falling within two SDS of the mean in two-thirds of individuals;
- -
- Macrocephaly. This sign is observed in more than 75% of individuals;
- -
- Facial gestalt. Long and narrow face with a triangular shape (84%), high and prominent forehead (96%), short nose with anteverted nares (48%), everted lower lip and small mouth (54%), prognathia/prominent chin (74.5%), and blue sclerae (28.7%) are the facial hallmarks of the condition. Other less frequent features are highly arched palate and dental crowding, sparse hair, loose and soft skin, and facial asymmetry;
- -
- Neurological features. Hypotonia is observed in 76% of individuals. Seizures and EEG anomalies are common and more frequently observed among the population with NFIX microdeletions. Central nervous system (CNS) anomalies are characterized by wide ventricles, corpus callosum hypoplasia, Chiari malformation and, less frequently, brain atrophy. Optic nerves hypoplasia has been reported, as well;
- -
- Muscolo-skeletal anomalies. MS individuals may have advanced bone age. Scoliosis, hyper-kyphosis or hyper-lordosis, pectus excavatum/carinatum, slender habitus, and long hands are extremely frequent;
- -
- Ophthalmological features. Strabismus and refractive disorders, such as myopia, hypermetropia, and astigmatism are quite common. Nystagmus has been reported as well;
- -
- -
- -
- In addition to the abovementioned distinctive features, MS is invariably associated with developmental delay and intellectual disability (DD/ID) [2,13,14,15], ranging from moderate to severe, even though mild ID has been rarely reported. Behavioral abnormalities, such as anxiety, autistic traits, hyperactivity, hetero- and auto- aggressivity and noise sensitivity are also reported in previous studies [2,3,13,14]. The sensory difficulties may worsen the severity of behavioral and psychiatric symptoms, mainly auditory hypersensitivity, that may increase anxiety, trigger challenging behavior [2], impair sustained attention and disrupt task performance [16].
2. Materials and Methods
2.1. Participants
2.2. Neuropsychological Assessment
2.2.1. Cognitive Assessment
2.2.2. Adaptive Behavior Assessment
2.2.3. Language Assessment
2.2.4. Visuomotor Integration Assessment
2.3. Statistical Analysis
3. Results
3.1. Descriptive Analysis
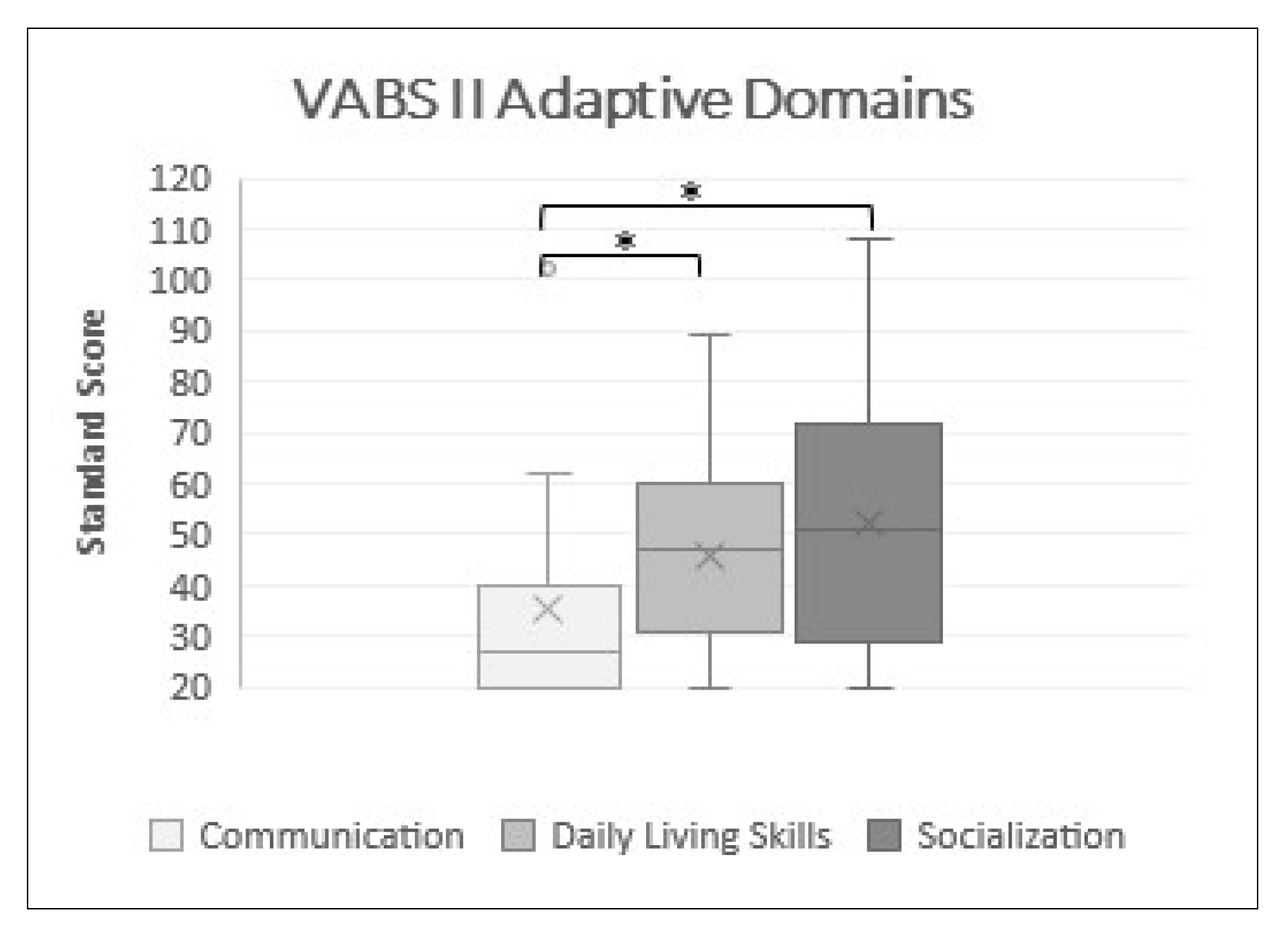
3.2. Adaptive Domains and Subdomains in VABS II
3.3. Correlation between Cognitive Abilities and Adaptive Behavior
3.4. Correlation between VABS-II-Daily Living Skills Subdomains and VMI-Visuomotor Integration
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malan, V.; Rajan, D.; Thomas, S.; Shaw, A.C.; Louis Dit Picard, H.; Layet, V.; Till, M.; van Haeringen, A.; Mortier, G.; Nampoothiri, S.; et al. Distinct effects of allelic NFIX mutations on nonsense-mediated mRNA decay engender either a Sotos-like or a Marshall-Smith syndrome. Am. J. Hum. Genet. 2010, 87, 189–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Priolo, M.; Schanze, D.; Tatton-Brown, K.; Mulder, P.A.; Tenorio, J.; Kooblall, K.; Acero, I.H.; Alkuraya, F.S.; Arias, P.; Bernardini, L.; et al. Further delineation of Malan syndrome. Hum. Mutat. 2018, 39, 1226–1237. [Google Scholar] [CrossRef] [PubMed]
- Gurrieri, F.; Cavaliere, M.L.; Wischmeijer, A.; Mammì, C.; Neri, G.; Pisanti, M.A.; Rodella, G.; Laganà, C.; Priolo, M. NFIX mutations affecting the DNA-binding domain cause a peculiar overgrowth syndrome (Malan syndrome): A new patients series. Eur. J. Med. Genet. 2015, 58, 488–491. [Google Scholar] [CrossRef] [PubMed]
- Harris, L.; Zalucki, O.; Clément, O.; Fraser, J.; Matuzelski, E.; Oishi, S.; Harvey, T.J.; Burne, T.; Heng, J.I.; Gronostajski, R.M.; et al. Neurogenic differentiation by hippocampal neural stem and progenitor cells is biased by NFIX expression. Development 2018, 145, dev155689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, G.; Antonini, S.; Bonfanti, C.; Monteverde, S.; Vezzali, C.; Tajbakhsh, S.; Cossu, G.; Messina, G. Nfix Regulates Temporal Progression of Muscle Regeneration through Modulation of Myostatin Expression. Cell Rep. 2016, 14, 2238–2249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez, F.; Marín-Reina, P.; Sanchis-Calvo, A.; Perez-Aytés, A.; Oltra, S.; Roselló, M.; Mayo, S.; Monfort, S.; Pantoja, J.; Orellana, C. Novel mutations of NFIX gene causing Marshall-Smith syndrome or Sotos-like syndrome: One gene, two phenotypes. Pediatric Res. 2015, 78, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.C.; van Balkom, I.D.; Bauer, M.; Cole, T.R.; Delrue, M.A.; Van Haeringen, A.; Holmberg, E.; Knight, S.J.; Mortier, G.; Nampoothiri, S.; et al. Phenotype and natural history in Marshall-Smith syndrome. Am. J. Med. Genet. 2010, 152A, 2714–2726. [Google Scholar] [CrossRef] [PubMed]
- Schanze, D.; Neubauer, D.; Cormier-Daire, V.; Delrue, M.A.; Dieux-Coeslier, A.; Hasegawa, T.; Holmberg, E.E.; Koenig, R.; Krueger, G.; Schanze, I.; et al. Deletions in the 3′ part of the NFIX gene including a recurrent Alu-mediated deletion of exon 6 and 7 account for previously unexplained cases of Marshall-Smith syndrome. Hum. Mutat. 2014, 35, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Nimmakayalu, M.; Horton, V.K.; Darbro, B.; Patil, S.R.; Alsayouf, H.; Keppler-Noreuil, K.; Shchelochkov, O.A. Apparent germline mosaicism for a novel 19p13.13 deletion disrupting NFIX and CACNA1A. Am. J. Med. Genet. 2013, 161A, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Oshima, T.; Hara, H.; Takeda, N.; Hasumi, E.; Kuroda, Y.; Taniguchi, G.; Inuzuka, R.; Nawata, K.; Morita, H.; Komuro, I. A novel mutation of NFIX causes Sotos-like syndrome (Malan syndrome) complicated with thoracic aortic aneurysm and dissection. Hum. Genome Var. 2017, 4, 17022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hancarova, M.; Havlovicova, M.; Putzova, M.; Vseticka, J.; Prchalova, D.; Stranecky, V.; Sedlacek, Z. Parental gonadal but not somatic mosaicism leading to de novo NFIX variants shared by two brothers with Malan syndrome. Am. J. Med. Genet. 2019, 179, 2119–2123. [Google Scholar] [CrossRef] [PubMed]
- Sihombing, N.; Winarni, T.I.; van Bokhoven, H.; van der Burgt, I.; de Leeuw, N.; Faradz, S. Pathogenic variant in NFIX gene affecting three sisters due to paternal mosaicism. Am. J. Med. Genet. 2020, 182, 2731–2736. [Google Scholar] [CrossRef] [PubMed]
- Van Balkom, I.D.; Shaw, A.; Vuijk, P.J.; Franssens, M.; Hoek, H.W.; Hennekam, R.C. Development and behaviour in Marshall-Smith syndrome: An exploratory study of cognition, phenotype and autism. J. Intellect. Disabil. Res. 2011, 55, 973–987. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, A.C.; Kalish, J.M. Overgrowth Syndromes. J. Pediatric Genet. 2015, 4, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Klaassens, M.; Morrogh, D.; Rosser, E.M.; Jaffer, F.; Vreeburg, M.; Bok, L.A.; Segboer, T.; van Belzen, M.; Quinlivan, R.M.; Kumar, A.; et al. Malan syndrome: Sotos-like overgrowth with de novo NFIX sequence variants and deletions in six new patients and a review of the literature. Eur. J. Hum. Genet. 2015, 23, 610–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaaf, C.P.; Wiszniewska, J.; Beaudet, A.L. Copy number and SNP arrays in clinical diagnostics. Annu. Rev. Genom. Hum. Genet. 2011, 12, 25–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulder, P.A.; van Balkom, I.; Landlust, A.M.; Priolo, M.; Menke, L.A.; Acero, I.H.; Alkuraya, F.S.; Arias, P.; Bernardini, L.; Bijlsma, E.K.; et al. Development, behaviour and sensory processing in Marshall-Smith syndrome and Malan syndrome: Phenotype comparison in two related syndromes. J. Intellect. Disabil. Res. 2020, 64, 956–969. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Macchiaiolo, M.; Panfili, F.P.; Vecchio, D.; Gonfiantini, M.V.; Cortellessa, F.; Caciolo, C.; Zollino, M.; Accadia, M.; Seri, M.; Chinali, M.; et al. A deep phenotyping experience: Up to date in management and diagnosis of Malan syndrome in a single center surveillance report. Orphanet J. Rare Dis. 2022, 17, 235. [Google Scholar] [CrossRef] [PubMed]
- Roid, G.L.; Miller, L.J.; Pomplun, M.; Koch, C. Leiter International Performance Scale—Third Edition, Stoelting Co 2013; Italian edition; Cornoldi, C., Giofrè, D., Belacchi, C., Eds.; Giunti Psychometrics: Florence, Italy, 2016. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children, 4th ed.; Italian edition; Orsini, A., Pezzuti, L., Picone, L., Eds.; Giunti Psychometrics: Florence, Italy, 2014. [Google Scholar]
- Green, E.; Stroud, L.; O’Connell, R.; Bloomfield, S.; Cronje, J.; Foxcroft, C.; Hunter, K. Griffith III: Griffiths Scales of Child Development, 3rd ed.; Italian edition; Lanfranchi, S., Rea, M., Ferri, R., Vianello, R., Eds.; Hogrefe: Firenze, Italy, 2017. [Google Scholar]
- Balboni, G.; Belacchi, C.; Bonichini, S.; Coscarelli, A. Vineland II. Vineland Adaptive Behavior Scales, 2nd ed.; Survey Form-Standardizzazione Italiana; Giunti Psychometrics: Florence, Italy, 2016. [Google Scholar]
- Bello, A.; Caselli, M.C.; Pettenati, P.; Stefanini, S. Parole in Gioco: Una Prova di Comprensione e Produzione Lessicale; [Picture Naming Game: A Lexical Comprehension and Production Task]; Giunti, Organizzazioni Speciali: Firenze, Italy, 2010. [Google Scholar]
- Vicari, S.; Marotta, L.; Luci, A. TFL Test Fono-lessicale: Valutazione delle Abilità Lessicali in età Prescolare; Edizioni Erickson: Trento, Italy, 2007. [Google Scholar]
- Marini, A.; Marotta, L.; Bulgheroni, S.; Fabbro, F. Batteria per la Valutazione del Linguaggio in Bambini Dai 4 ai 12 Anni; Giunti, O.S: Firenze, Italy, 2014. [Google Scholar]
- Bishop, D.V.M. Test for Reception of Grammar—Version 2 (TROG-2); The Psychological Corporation Limited: London, UK, 2003. [Google Scholar]
- Beery, K.E.; Buktenica, N.A.; Beery, N.A. The Beery-Buktenica Developmental Test of Visual-Motor Integration: Administration, Scoring, and Teaching Manual, 6th ed; NSC Pearson: Minneapolis, MN, USA, 2010. [Google Scholar]

| N | Gender | Age | IQ | ABC | Language Production: Qualitative Analysis | VMI | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 2.7 | 70 * | 87 | 0 | n.a. | n.a. | prevalent use of olophrases | n.a. |
| 2 | M | 6.4 | 65 | 39 | −2.1 | −2.2 | n.a. | prevalent use of olophrases | 45 |
| 3 | F | 7.3 | 54 | 23 | −0.8 | n.a. | n.a. | prevalent use of olophrases | 45 |
| 4 | M | 7.11 | 58 | 48 | −1.3 | −1.2 | n.a. | use of telegraphic language, phonological disorder | 45 |
| 5 | M | 8.1 | 52 | 42 | −1.2 | −1.2 | n.a. | use of telegraphic language, phonological disorder | 45 |
| 6 | F | 8.7 | 54 | 31 | −1.6 | n.a. | n.a | prevalent use of olophrases | 45 |
| 7 | M | 8.11 | 40 | 33 | −0.1 | −1 | n.a. | prevalent use of olophrases | n.a. |
| 8 | M | 11.3 | 62 | 56 | −0.8 | 0 | −2.8 | use of complex sentence, phonological disorders | 72 |
| 9 | M | 13.3 | 42 | 20 | −2.5 | n.a. | n.a | prevalent use of olophrases | 45 |
| 10 | M | 13.10 | 69 | 100 | −3.8 | −3.7 | −3.9 | use of complex sentences, phonological disorders | 65 |
| 11 | F | 15.5 | 50 ** | 21 | −2.7 | −0.8 | −3.4 | use of complex sentences, phonological disorders | 49 |
| 12 | M | 16.2 | 48 | 25 | −2.6 | −0.3 | −3.6 | use of telegraphic language, phonological disorder | 59 |
| 13 | M | 16.4 | 45 | 20 | −2.7 | n.a. | −3.9 | prevalent use of olophrases | 45 |
| 14 | F | 17.6 | 47 | 20 | −3.1 | −1.3 | −4.2 | use of telegraphic language, phonological disorder | 47 |
| 15 | F | 25.6 | 40 | 20 | −7.3 | −7.5 | −7.4 | use of telegraphic language, phonological disorder | 45 |
| VABS II Domains | MED | M | Min–Max | SD |
|---|---|---|---|---|
| Communication | 27.0 | 35.4 | 20.0–102.0 | 22.2 |
| Daily Living Skills | 47.0 | 45.7 | 20.0–89.0 | 19.7 |
| Socialization | 51.0 | 52.3 | 20.0–108.0 | 25.4 |
| Motor Skills | 54.5 | 54.5 | 33.0–76.0 | 30.4 |
| ABC | 31.0 | 39.0 | 20.0–100.0 | 25.0 |
| VABS II Subdomains | MED | M | Min–Max | SD |
|---|---|---|---|---|
| Receptive | 8.0 | 8.1 | 6.0–15.0 | 2.5 |
| Expressive | 6.0 | 5.9 | 6.0–15.0 | 4.0 |
| Written | 4.0 | 4.3 | 1.0–14.0 | 7.1 |
| Personal | 2.0 | 3.9 | 1.0–11.0 | 3.0 |
| Domestic | 11.0 | 10.5 | 4.0–15.0 | 2.8 |
| Community | 4.0 | 5.4 | 1.0–13.0 | 3.8 |
| Interpersonal | 4.0 | 6.3 | 2.0–15.0 | 4.4 |
| Play and Leisure | 8.0 | 8.3 | 2.0–17.0 | 3.7 |
| Coping Skills | 6.0 | 7.2 | 2.0–16.0 | 3.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfieri, P.; Macchiaiolo, M.; Collotta, M.; Montanaro, F.A.M.; Caciolo, C.; Cumbo, F.; Galassi, P.; Panfili, F.M.; Cortellessa, F.; Zollino, M.; et al. Characterization of Cognitive, Language and Adaptive Profiles of Children and Adolescents with Malan Syndrome. J. Clin. Med. 2022, 11, 4078. https://doi.org/10.3390/jcm11144078
Alfieri P, Macchiaiolo M, Collotta M, Montanaro FAM, Caciolo C, Cumbo F, Galassi P, Panfili FM, Cortellessa F, Zollino M, et al. Characterization of Cognitive, Language and Adaptive Profiles of Children and Adolescents with Malan Syndrome. Journal of Clinical Medicine. 2022; 11(14):4078. https://doi.org/10.3390/jcm11144078
Chicago/Turabian StyleAlfieri, Paolo, Marina Macchiaiolo, Martina Collotta, Federica Alice Maria Montanaro, Cristina Caciolo, Francesca Cumbo, Paolo Galassi, Filippo Maria Panfili, Fabiana Cortellessa, Marcella Zollino, and et al. 2022. "Characterization of Cognitive, Language and Adaptive Profiles of Children and Adolescents with Malan Syndrome" Journal of Clinical Medicine 11, no. 14: 4078. https://doi.org/10.3390/jcm11144078
APA StyleAlfieri, P., Macchiaiolo, M., Collotta, M., Montanaro, F. A. M., Caciolo, C., Cumbo, F., Galassi, P., Panfili, F. M., Cortellessa, F., Zollino, M., Accadia, M., Seri, M., Tartaglia, M., Bartuli, A., Mammì, C., Vicari, S., & Priolo, M. (2022). Characterization of Cognitive, Language and Adaptive Profiles of Children and Adolescents with Malan Syndrome. Journal of Clinical Medicine, 11(14), 4078. https://doi.org/10.3390/jcm11144078









