Use of Black-and-White Digital Filters to Optimize Visualization in Cataract Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Technique
2.2. Data Collection
2.3. Statistical Analysis
3. Results
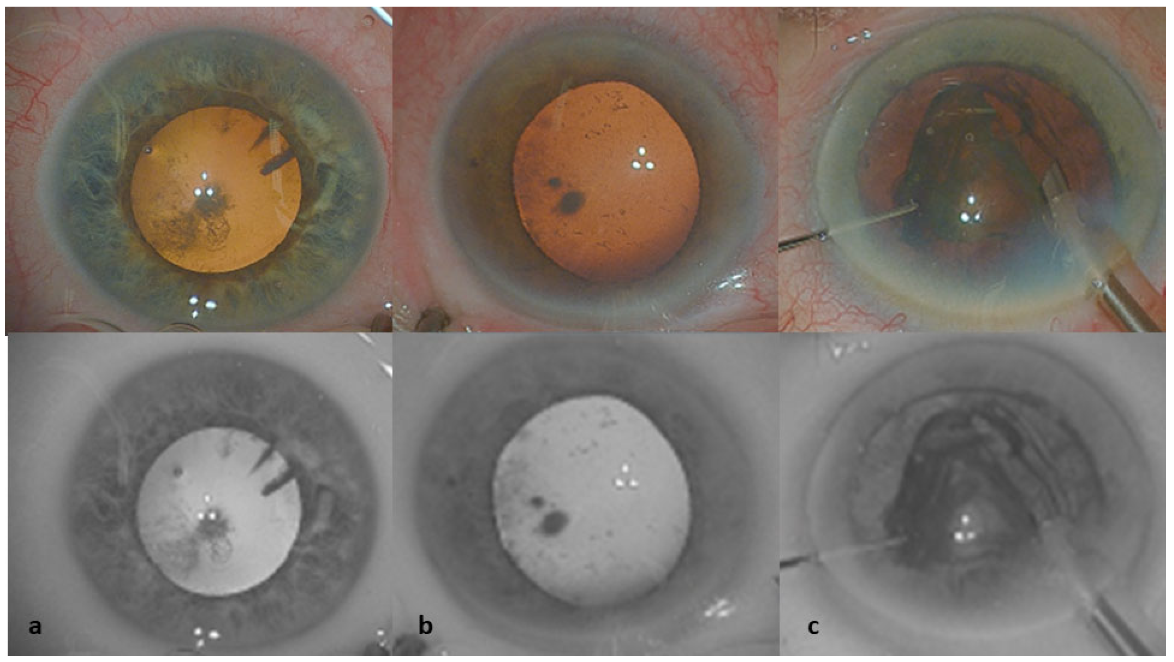
3.1. Tissue Color Modifications
3.2. Contrast Measurements and the Surgeons’ Assessments of Tissue Visibility with the BW Filter and Standard Colors during Surgery
4. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Foster, A. Vision 2020: The cataract challenge. Community Eye Health 2020, 13, 17–19. [Google Scholar]
- Stein, J.D.; Grossman, D.S.; Mundy, K.M.; Sugar, A.; Sloan, F.A. Severe adverse events after cataract surgery among medicare beneficiaries. Ophthalmology 2011, 118, 1716–1723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstock, R.J.; Diakonis, V.F.; Schwartz, A.J.; Weinstock, A.J. Heads-up cataract surgery: Complication rates, surgical duration, and comparison with traditional microscopes. J. Refract. Surg. 2019, 35, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, E.D.; Nuzbrokh, Y.; Sippel, K.C. Efficacy of 3D digital visualization in minimizing coaxial illumination and phototoxic potential in cataract surgery: Pilot study. J. Cataract Refract. Surg. 2021, 47, 291–296. [Google Scholar] [CrossRef]
- Sandali, O.; El Sanharawi, M.; Tahiri, J.H.R.; Roux, H.; Bouheraoua, N.; Borderie, V. Early corneal pachymetry maps after cataract surgery and influence of 3D digital visualization system in minimizing corneal oedema. Acta Ophtalmol. 2021; online ahead of print. [Google Scholar] [CrossRef]
- Sandali, O.; Tahiri, J.H.R.; Armia, A.B.; El Sanharawi, M.; Borderie, V. Facilitating Role of the 3D Viewing System in Tilted Microscope Positions for Cataract Surgery in Patients Unable to Lie Flat. J. Clin. Med. 2022, 11, 1865. [Google Scholar] [CrossRef]
- Sandali, O.; Tahiri, J.H.R.; Dulière, C.; El Sanharawi, M.; Borderie, V. Use of a 3D viewing system and microscope tilting to extend the peripheral retinal view. RETINA 2022. [Google Scholar] [CrossRef]
- Parthenis, K.; Metaxaki-Kossionides, C. Blood analysis using black and white digital images. J. Biomed. Eng. 1992, 14, 287–292. [Google Scholar] [CrossRef]
- Palácios, R.M.; Kayat, K.V.; Morel, C.; Conrath, J.; Matonti, F.; Morin, B.; Farah, M.E.; Devin, F. Clinical Study on the Initial Experiences of French Vitreoretinal Surgeons with Heads-up Surgery. Curr. Eye Res. 2020, 45, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Mandelblum, J.; Fischer, N.; Achiron, A.; Goldberg, M.; Tuuminen, R.; Zunz, E.; Spierer, O. A Simple Pre-Operative Nuclear Classification Score (SPONCS) for Grading Cataract Hardness in Clinical Studies. J. Clin. Med. 2020, 9, 3503. [Google Scholar] [CrossRef] [PubMed]
- Melo, A.G.R.; Conti, T.F.; Hom, G.L.; Greenlee, T.E.; Cella, W.P.; Talcott, K.E.; Rachitskaya, A.; Yuan, A.; Sood, A.; Milam, R.; et al. Optimizing Visualization of Membranes in Macular Surgery with Heads-Up Display. Ophthalmic Surg. Lasers Imaging Retin. 2020, 51, 584–587. [Google Scholar] [CrossRef] [PubMed]
- Piazza, C.; Dessouky, O.; Peretti, G.; Cocco, D.; De Benedetto, L.; Nicolai, P. Narrow-band imaging: A new tool for evaluation of head and neck squamous cell carcinomas. Review of the literature. Acta Otorhinolaryngol. Ital. 2008, 28, 49–54. [Google Scholar] [PubMed]
- Kim, Y.J.; Kim, Y.J.; Nam, D.H.; Kim, K.G.; Kim, S.W.; Chung, T.Y.; Lee, S.J.; Park, K.H. Contrast, visibility, and color balance between the microscope versus intracameral illumination in cataract surgery using a 3D visualization system. Indian J. Ophthalmol. 2021, 69, 927–931. [Google Scholar] [PubMed]
- Yavuz, Z.; Köse, C. Blood Vessel Extraction in Color Retinal Fundus Images with Enhancement Filtering and Unsupervised Classification. J. Healthc. Eng. 2017, 2017, 4897258. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xin, J.; Yang, X.; Sun, J.; Xu, D.; Zheng, N.; Yuan, C. Deep morphology aided diagnosis network for segmentation of carotid artery vessel wall and diagnosis of carotid atherosclerosis on black-blood vessel wall MRI. Med. Phys. 2019, 46, 5544–5561. [Google Scholar] [CrossRef] [PubMed]
- Fenton, B.M.; Paoni, S.F.; Beauchamp, B.K.; Ding, I. Zonal image analysis of tumour vascular perfusion, hypoxia, and necrosis. Br. J. Cancer 2002, 86, 1831–1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, L.L.; Blakely, A.; Invernizzi, M.; Lin, J.; Kidambi, T.; Melstrom, K.A.; Yu, K.; Lud, T. Separation of color channels from conventional colonoscopy images improves deep neural network detection of polyps. J. Biomed. Opt. 2021, 26, 015001. [Google Scholar] [CrossRef] [PubMed]
- Mura, M.; Martin, W.; Williams, K.; Abulon, D.J.K. Comparison of 3D Digitally Assisted Visualization System with Current Standard Visualization for the Removal of Vitreous in a Preclinical Model. Clin. Ophthalmol. 2021, 15, 4499–4505. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Do, J.R.; Shin, J.P.; Park, D.H. Customized Color Settings of Digitally Assisted Vitreoretinal Surgery to Enable Use of Lower Dye Concentrations During Macular Surgery. Front. Med. 2022, 8, 810070. [Google Scholar] [CrossRef] [PubMed]


| Standard Colors | Black and White Filters | Agreement (κ Value) | |
|---|---|---|---|
| Limbus identification before incision (n = 40) | Better | Worse | 1.00 |
| Capsulorhexis (n = 40) | Worse | Better | 0.86 |
| hydrodissection fluid wave perception (n = 40) | Worse | Better | 0.74 |
| Nucleus sculpting (n = 14) | Better | Worse | 0.81 |
| Phaco-chop (n = 26) | Worse | Better | 0.74 |
| Nucleus removal (n = 40) | No difference | No difference | 0.70 |
| Cortex removal through subincisional edema (n = 40) | Worse | Better | 0.67 |
| Posterior capsule polishing (n = 40) | No difference | No difference | 0.80 |
| Viscous removal (n = 40) | No difference | No difference | 0.90 |
| Standard Color | Black and White Filters | p Value | |
|---|---|---|---|
| Limbus area (n = 40) | 13.06 (1.05) | 12.42 (1.37) | 0.0006 * |
| Capsulorhexis (n = 40) | 10.49 (2.79) | 17.04 (5.26) | <0.0001 * |
| Nucleus grooves during sculpting (n = 14) | 13.37 (3.27) | 13.97 (4.21) | 0.22 † |
| Instrument contrasts through the nucleus during phaco-chop (n = 26) | 13.82 (2.34) | 15.70 (2.77) | <0.0001 † |
| Nucleus removal (n = 40) | 11.17 (1.98) | 12.06 (2.92) | 0.003 * |
| Cortex removal through subincisional edema (n = 40) | 13.88 (3.46) | 21.34 (5.12) | <0.0001 * |
| Residual debris on the posterior capsule (n = 40) | 11.94 (1.83) | 14.66 (3.16) | <0.0001 * |
| Viscous removal (n = 40) | 15.96 (2.99) | 18.08 (4.04) | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sandali, O.; Tahiri, J.H.R.; Armia Balamoun, A.; Duliere, C.; El Sanharawi, M.; Borderie, V. Use of Black-and-White Digital Filters to Optimize Visualization in Cataract Surgery. J. Clin. Med. 2022, 11, 4056. https://doi.org/10.3390/jcm11144056
Sandali O, Tahiri JHR, Armia Balamoun A, Duliere C, El Sanharawi M, Borderie V. Use of Black-and-White Digital Filters to Optimize Visualization in Cataract Surgery. Journal of Clinical Medicine. 2022; 11(14):4056. https://doi.org/10.3390/jcm11144056
Chicago/Turabian StyleSandali, Otman, Joutei Hassani Rachid Tahiri, Ashraf Armia Balamoun, Cedric Duliere, Mohamed El Sanharawi, and Vincent Borderie. 2022. "Use of Black-and-White Digital Filters to Optimize Visualization in Cataract Surgery" Journal of Clinical Medicine 11, no. 14: 4056. https://doi.org/10.3390/jcm11144056
APA StyleSandali, O., Tahiri, J. H. R., Armia Balamoun, A., Duliere, C., El Sanharawi, M., & Borderie, V. (2022). Use of Black-and-White Digital Filters to Optimize Visualization in Cataract Surgery. Journal of Clinical Medicine, 11(14), 4056. https://doi.org/10.3390/jcm11144056








