Extra-Pseudocapsular Transsphenoidal Surgery for Microprolactinoma in Women
Abstract
1. Introduction
2. Materials and Methods
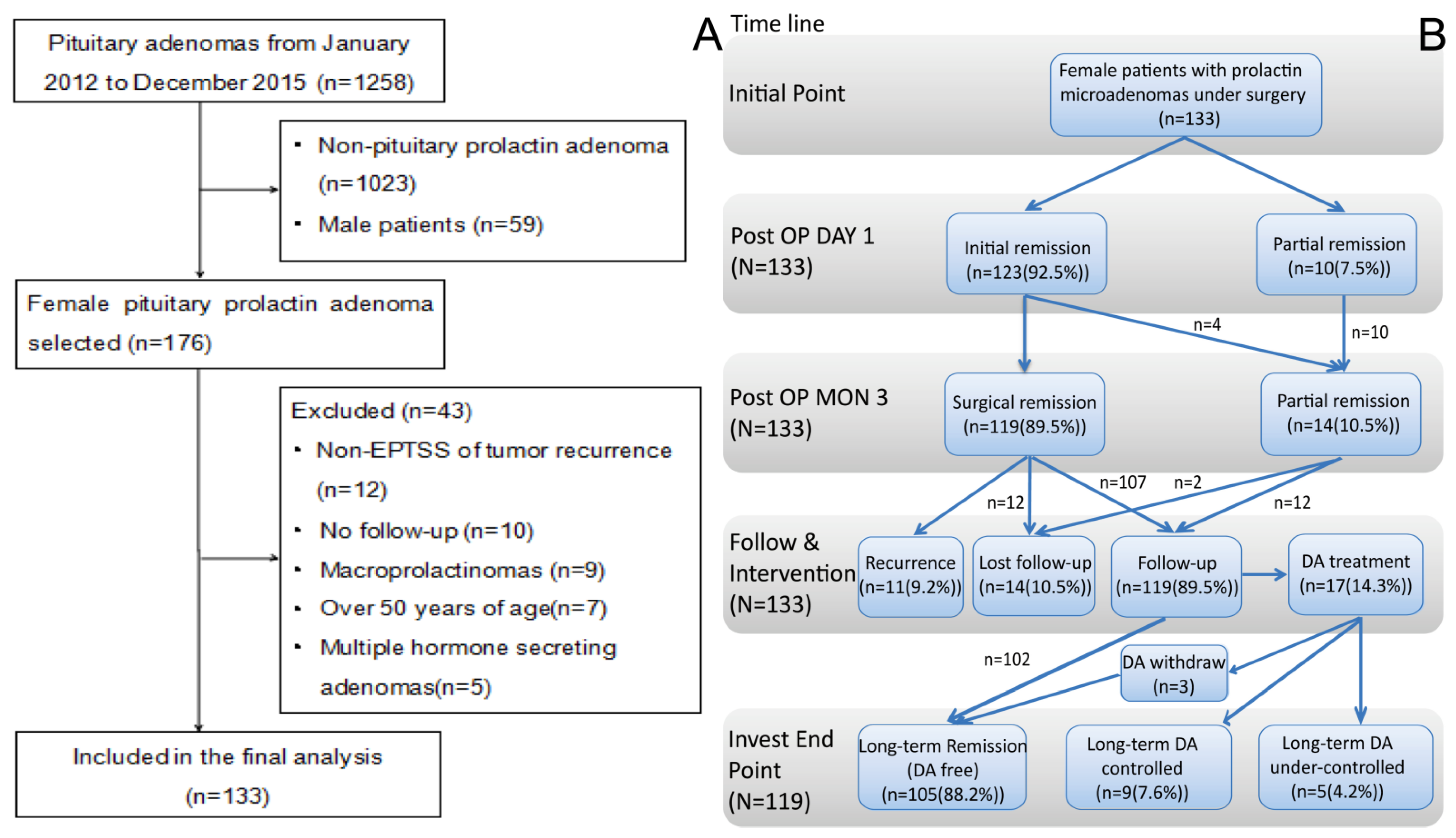
2.1. Study Population and Design
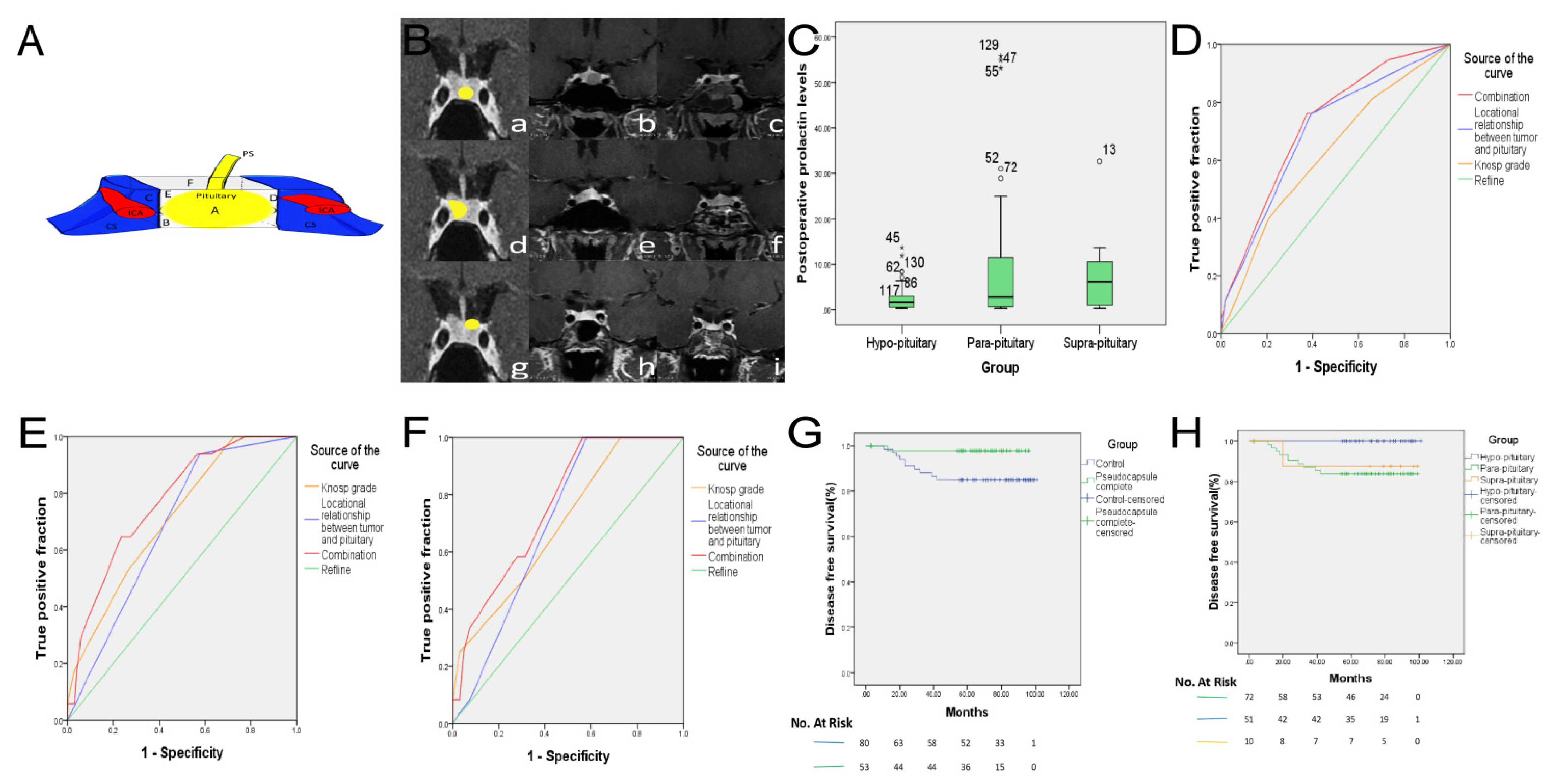
2.2. Classification of Microprolactinomas
2.3. Extra-Pseudocapsular Transsphenoidal Surgery (EPTSS) for Pituitary Adenomas
2.4. Remission and Recurrence Criteria
2.5. Statistical Analysis
3. Results
3.1. Clinical Characteristics
3.2. Pseudocapsule Status in the Microprolactinoma
3.3. Early Surgical Remission and Associated Factors
3.4. Postoperative Complications
3.5. Long-Term Follow-Up and Recurrence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ciccarelli, A.; Daly, A.; Beckers, A. The Epidemiology of Prolactinomas. Pituitary 2005, 8, 3–6. [Google Scholar] [CrossRef]
- Vroonen, L.; Daly, A.F.; Beckers, A. Epidemiology and Management Challenges in Prolactinomas. Neuroendocrinology 2019, 109, 20–27. [Google Scholar] [CrossRef]
- Melmed, S.; Casanueva, F.F.; Hoffman, A.R.; Kleinberg, D.L.; Montori, V.; Schlechte, J.; Wass, J.A.H. Diagnosis and Treatment of Hyperprolactinemia: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 273–288. [Google Scholar] [CrossRef]
- Molitch, M.E. Diagnosis and Treatment of Pituitary Adenomas: A Review. JAMA 2017, 317, 516. [Google Scholar] [CrossRef]
- Hu, J.; Zheng, X.; Zhang, W.; Yang, H. Current drug withdrawal strategy in prolactinoma patients treated with cabergoline: A systematic review and meta-analysis. Pituitary 2015, 18, 745–751. [Google Scholar] [CrossRef]
- Kim, K.; Park, Y.W.; Kim, D.; Ahn, S.S.; Moon, J.H.; Kim, E.H.; Lee, E.J.; Ku, C.R. Biochemical Remission after Cabergoline Withdrawal in Hyperprolactinemic Patients with Visible Remnant Pituitary Adenoma. J. Clin. Endocrinol. Metab. 2021, 106, e615–e624. [Google Scholar] [CrossRef]
- Espinosa-Cárdenas, E.; Sánchez-García, M.; Ramirez-Renteria, C.; Mendoza-Zubieta, V.; Sosa-Eroza, E.; Mercado, M. High biochemical recurrence rate after withdrawal of cabergoline in prolactinomas: Is it necessary to restart treatment? Endocrine 2020, 70, 143–149. [Google Scholar] [CrossRef]
- Colao, A.; Di Sarno, A.; Cappabianca, P.; Di Somma, C.; Pivonello, R.; Lombardi, G. Withdrawal of long-term cabergoline therapy for tumoral and nontumoral hyperprolactinemia. N. Engl. J. Med. 2003, 349, 2023–2033. [Google Scholar] [CrossRef]
- Donoho, D.A.; Laws, E.R. The Role of Surgery in the Management of Prolactinomas. Neurosurg. Clin. N. Am. 2019, 30, 509–514. [Google Scholar] [CrossRef]
- Giese, S.; Nasi-Kordhishti, I.; Honegger, J. Outcomes of Transsphenoidal Microsurgery for Prolactinomas—A Contemporary Series of 162 Cases. Exp. Clin. Endocrinol. Diabetes 2021, 129, 163–171. [Google Scholar] [CrossRef]
- Kreutzer, J.; Buslei, R.; Wallaschofski, H.; Hofmann, B.; Nimsky, C.; Fahlbusch, R.; Buchfelder, M. Operative treatment of prolactinomas: Indications and results in a current consecutive series of 212 patients. Eur. J. Endocrinol. 2008, 158, 11–18. [Google Scholar] [CrossRef]
- Costello, R.T. Subclinical Adenoma of the Pituitary Gland. Am. J. Pathol. 1936, 12, 205–216.1. [Google Scholar]
- Najafabadi, A.H.Z.; Zandbergen, I.M.; De Vries, F.; Broersen, L.H.A.; Marle, M.E.V.D.A.-V.; Pereira, A.M.; Peul, W.C.; Dekkers, O.M.; Van Furth, W.R.; Biermasz, N.R. Surgery as a Viable Alternative First-Line Treatment for Prolactinoma Patients. A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2020, 105, e32–e41. [Google Scholar] [CrossRef]
- Park, J.Y.; Choi, W.; Hong, A.R.; Yoon, J.H.; Kim, H.K.; Jang, W.-Y.; Jung, S.; Kang, H.-C. Surgery is a safe, effective first-line treatment modality for noninvasive prolactinomas. Pituitary 2021, 24, 955–963. [Google Scholar] [CrossRef]
- Knosp, E.; Steiner, E.; Kitz, K.; Matula, C. Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurgery 1993, 33, 610–617, discussion 617–618. [Google Scholar] [CrossRef]
- Zielinski, G.; Ozdarski, M.; Maksymowicz, M.; Szamotulska, K.; Witek, P. Prolactinomas: Prognostic Factors of Early Remission After Transsphenoidal Surgery. Front. Endocrinol. 2020, 11, 439. [Google Scholar] [CrossRef]
- Schlechte, J.; Vangilder, J.; Sherman, B. Predictors of the Outcome of Transsphenoidal Surgery for Prolactin-Secreting Pituitary Adenomas. J. Clin. Endocrinol. Metab. 1981, 52, 785–789. [Google Scholar] [CrossRef]
- Ma, Q.; Su, J.; Li, Y.; Wang, J.; Long, W.; Luo, M.; Liu, Q. The Chance of Permanent Cure for Micro- and Macroprolactinomas, Medication or Surgery? A Systematic Review and Meta-Analysis. Front. Endocrinol. 2018, 9, 636. [Google Scholar] [CrossRef]
- Oldfield, E.H.; Vortmeyer, A.O. Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J. Neurosurg. 2006, 104, 7–19. [Google Scholar] [CrossRef]
- Lee, E.J.; Ahn, J.Y.; Noh, T.; Kim, S.H.; Kim, T.S.; Kim, S.H. Tumor Tissue Identification in the Pseudocapsule of Pituitary Adenoma: Should the Pseudocapsule be Removed for Total Resection of Pituitary Adenoma? Oper. Neurosurg. 2009, 64 (Suppl. 1), ONS62–ONS70. [Google Scholar] [CrossRef]
- Jagannathan, J.; Smith, R.; DeVroom, H.L.; Vortmeyer, A.O.; Stratakis, C.A.; Nieman, L.K.; Oldfield, E.H. Outcome of using the histological pseudocapsule as a surgical capsule in Cushing disease: Clinical article. J. Neurosurg. 2009, 111, 531–539. [Google Scholar] [CrossRef]
- Xie, T.; Liu, T.; Zhang, X.; Chen, L.; Luo, R.; Sun, W.; Hu, F.; Yu, Y.; Gu, Y.; Lu, Z. Time to Revive the Value of the Pseudocapsule in Endoscopic Endonasal Transsphenoidal Surgery for Growth Hormone Adenomas. World Neurosurg. 2016, 89, 65–71. [Google Scholar] [CrossRef]
- Andereggen, L.; Frey, J.; Andres, R.H.; Luedi, M.M.; El-Koussy, M.; Widmer, H.R.; Beck, J.; Mariani, L.; Seiler, R.W.; Christ, E. First-line surgery in prolactinomas: Lessons from a long-term follow-up study in a tertiary referral center. J. Endocrinol. Investig. 2021, 44, 2621–2633. [Google Scholar] [CrossRef]
- Tampourlou, M.; Trifanescu, R.; Paluzzi, A.; Ahmed, S.K.; Karavitaki, N. Therapy of Endocrine Disease: Surgery in microprolactinomas: Effectiveness and risks based on contemporary literature. Eur. J. Endocrinol. 2016, 175, R89–R96. [Google Scholar] [CrossRef]
- Landolt, A.M.; Osterwalder, V. Perivascular Fibrosis in Prolactinomas: Is it Increased by Bromocriptine. J. Clin. Endocrinol. Metab. 1984, 58, 1179–1183. [Google Scholar] [CrossRef]
- Tamasauskas, A.; Sinkunas, K.; Bunevicius, A.; Radžiūnas, A.; Skiriute, D.; Deltuva, V.P. Transsphenoidal surgery for microprolactinomas in women: Results and prognosis. Acta Neurochir. 2012, 154, 1889–1893. [Google Scholar] [CrossRef]
- Landolt, A.M.; Keller, P.J.; Froesch, E.R.; Mueller, J. Bromocriptine: Does it jeopardise the result of later surgery for prolactinomas? Lancet 1982, 2, 657–658. [Google Scholar] [CrossRef]
- Sughrue, M.E.; Chang, E.F.; Tyrell, J.B.; Kunwar, S.; Wilson, C.B.; Blevins, L.S. Pre-operative dopamine agonist therapy improves post-operative tumor control following prolactinoma resection. Pituitary 2009, 12, 158–164. [Google Scholar] [CrossRef]
- Szmygin, H.; Szydełko, J.; Matyjaszek-Matuszek, B. Dopamine Agonist-Resistant Microprolactinoma-Mechanisms, Predictors and Management: A Case Report and Literature Review. J. Clin. Med. 2022, 11, 3070. [Google Scholar] [CrossRef]
- Feigenbaum, S.L.; E Downey, D.; Wilson, C.B.; Jaffe, R.B. Transsphenoidal pituitary resection for preoperative diagnosis of prolactin-secreting pituitary adenoma in women: Long term follow-up. J. Clin. Endocrinol. Metab. 1996, 81, 1711–1719. [Google Scholar] [CrossRef][Green Version]
- Losa, M.; Mortini, P.; Barzaghi, R.; Gioia, L.; Giovanelli, M. Surgical Treatment of Prolactin-Secreting Pituitary Adenomas: Early Results and Long-Term Outcome. J. Clin. Endocrinol. Metab. 2002, 87, 3180–3186. [Google Scholar] [CrossRef]
- Primeau, V.; Raftopoulos, C.; Maiter, D. Outcomes of transsphenoidal surgery in prolactinomas: Improvement of hormonal control in dopamine agonist-resistant patients. Eur. J. Endocrinol. 2012, 166, 779–786. [Google Scholar] [CrossRef]
- Kawamata, T.; Kubo, O.; Hori, T. Surgical removal of growth hormone-secreting pituitary adenomas with intensive microsurgical pseudocapsule resection results in complete remission of acromegaly. Neurosurg. Rev. 2005, 28, 201–208. [Google Scholar] [CrossRef]
- Nagata, Y.; Takeuchi, K.; Yamamoto, T.; Ishikawa, T.; Kawabata, T.; Shimoyama, Y.; Inoshita, N.; Wakabayashi, T. Peel-off resection of the pituitary gland for functional pituitary adenomas: Pathological significance and impact on pituitary function. Pituitary 2019, 22, 507–513. [Google Scholar] [CrossRef]
- Laws, E.R. Pituitary pseudocapsule. J. Neurosurg. 2006, 104, 1–2. [Google Scholar] [CrossRef]
- Babey, M.; Sahli, R.; Vajtai, I.; Andres, R.H.; Seiler, R.W. Pituitary surgery for small prolactinomas as an alternative to treatment with dopamine agonists. Pituitary 2011, 14, 222–230. [Google Scholar] [CrossRef]
- Koutourousiou, M.; Filho, F.V.G.; Fernandez-Miranda, J.C.; Wang, E.W.; Stefko, S.T.; Snyderman, C.H.; Gardner, P.A. Endoscopic Endonasal Surgery for Tumors of the Cavernous Sinus: A Series of 234 Patients. World Neurosurg. 2017, 103, 713–732. [Google Scholar] [CrossRef]
- Tyrrell, J.B.; Lamborn, K.R.; Hannegan, L.T.; Applebury, C.B.; Wilson, C.B. Transsphenoidal microsurgical therapy of prolactinomas: Initial outcomes and long-term results. Neurosurgery 1999, 44, 254–261, discussion 261–263. [Google Scholar] [CrossRef]
- Zygourakis, C.C.; Imber, B.S.; Chen, R.; Han, S.J.; Blevins, L.; Molinaro, A.; Kahn, J.G.; Aghi, M.K. Cost-Effectiveness Analysis of Surgical versus Medical Treatment of Prolactinomas. J. Neurol. Surg. Part B Skull Base 2017, 78, 125–131. [Google Scholar] [CrossRef]
- Jethwa, P.R.; Patel, T.D.; Hajart, A.F.; Eloy, J.A.; Couldwell, W.T.; Liu, J.K. Cost-Effectiveness Analysis of Microscopic and Endoscopic Transsphenoidal Surgery Versus Medical Therapy in the Management of Microprolactinoma in the United States. World Neurosurg. 2016, 87, 65–76. [Google Scholar] [CrossRef]
- Yi, N.; Ji, L.; Zhang, Q.; Zhang, S.; Liu, X.; Shou, X.; Lu, B. Long-term follow-up of female prolactinoma patients at child-bearing age after transsphenoidal surgery. Endocrine 2018, 62, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, H.; Watanabe, K.; Tominaga, T.; Yoshimoto, T. Transsphenoidal microsurgical results of female patients with prolactinomas. Clin. Neurol. Neurosurg. 2013, 115, 1621–1625. [Google Scholar] [CrossRef] [PubMed]
- Yatavelli, R.K.R.; Bhusal, K. Prolactinoma; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
| Surgical Indication | Patients (n = 133) |
|---|---|
| Drug intolerant (%) | 8 (6.0) |
| Drug resistance (%) | 36 (27.1) |
| Personal willing (%) | 67 (50.4) |
| Cystic prolactinoma (%) | 14 (10.5) |
| Tumor stroke (%) | 8 (6.0) |
| Variables | Patients (n = 133) | ||
|---|---|---|---|
| Age, years (mean ± SD) | 27.3 ± 6.5 | ||
| Tumor diameter, mm (mean ± SD) | 8.4 ± 1.7 | ||
| Ki-67 (%) | |||
| <3 | 110 (82.7) | ||
| ≥3 | 23 (17.3) | ||
| Follow-up time, months (median) | 72 | ||
| PRL level, ng/mL (mean ± SD) | 146.19 ± 103.84 | ||
| Clinical symptoms (%) | Preoperation | Postoperation | p value |
| Menstrual disorder | 105 (78.9) | 7 (5.3) | 0.000 a |
| Hyposexuality | 7 (5.3) | 1 (0.8) | 0.066 b |
| Galactosis | 46 (34.6) | 4 (3.0) | 0.000 a |
| Infertility | 19 (14.3) | 3 (2.3) | 0.001 a |
| Total | Pseudocapsule Complete | Pseudocapsule Incomplete/No Pseudocapsule | p Value | |
|---|---|---|---|---|
| Total (n) | 133 | 53 | 80 | |
| Age, years (mean ± SD) | 27.3 ± 6.5 | 28.1 ± 6.8 | 26.8 ± 6.3 | 0.252 a |
| Tumor diameter, mm (mean ± SD) | 8.4 ± 1.7 | 8.7 ± 1.5 | 8.3 ± 1.8 | 0.202 a |
| Ki-67 (%) | 0.138 b | |||
| <3 | 110 (82.7) | 47 (88.7) | 63 (78.8) | |
| ≥3 | 23 (17.3) | 6 (11.3) | 17 (21.2) | |
| Preoperation PRL (ng/mL) | 0.986 b | |||
| <200 | 108 (81.2) | 43 (81.1) | 65 (81.3) | |
| ≥200 | 25 (18.8) | 10 (18.9) | 15 (18.7) | |
| Preoperative medication of DA | 0.564 b | |||
| With | 44 (33.1) | 16 (30.2) | 28 (35.0) | |
| Without | 89 (66.9) | 37 (69.8) | 52 (65.0) | |
| Knosp grade (%) | 0.000 c | |||
| Grade 0 | 33 (24.8) | 18 (34.0) | 15 (18.8) | |
| Grade I | 57 (42.9) | 24 (45.3) | 33 (41.3) | |
| Grade II | 36 (27.1) | 9 (17.0) | 27 (33.8) | |
| Grade III | 6 (4.5) | 2 (3.8) | 4 (5.0) | |
| Grade IV | 1 (0.7) | 0 (0) | 1 (1.3) | |
| Locational relationship between tumor and pituitary (%) | 0.001 c | |||
| Hypo-pituitary | 51 (38.4) | 32 (60.4) | 19 (23.7) | |
| Para-pituitary | 72 (54.1) | 20 (37.7) | 52 (65.0) | |
| Supra-pituitary | 10 (7.5) | 1 (1.9) | 9 (11.3) | |
| Follow-up time, months (mean ± SD) | 61.9 ± 32.0 | 61.7 ± 28.7 | 62.1 ± 34.2 | 0.946 a |
| Follow-up loss rate (%) | 14 (10.5) | 5 (9.4) | 9 (11.3) | 0.738 b |
| Initial remission rate (%) | 123 (92.5) | 51 (96.2) | 72 (90.0) | 0.314 d |
| Surgical remission rate (%) | 119 (89.5) | 50 (94.3) | 69 (86.3) | 0.137 b |
| Long-term remission rate (%) | 102 (85.7) | 45 (93.8) | 57 (80.3) | 0.039 b |
| Recurrence rate (%) | 11 (9.2) | 1 (2.1) | 10 (14.1) | 0.048 d |
| Pseudocapsule Complete/Incomplete | No Pseudocapsule | p Value | |
|---|---|---|---|
| Total (n) | 113 | 20 | |
| Age, years (mean ± SD) | 27.3 ± 6.5 | 27.4 ± 6.6 | 0.928 a |
| Tumor diameter, mm (mean ± SD) | 8.6 ± 1.6 | 7.4 ± 2.0 | 0.018 a |
| Ki-67 (%) | 0.750 b | ||
| <3 | 94 (83.2) | 16 (80.0) | |
| ≥3 | 19 (16.8) | 4 (20.0) | |
| Knosp grade (%) | 0.023 c | ||
| Grade 0 | 27 (23.9) | 3 (15.0) | |
| Grade I | 53 (46.9) | 4 (20.0) | |
| Grade II | 27 (23.9) | 9 (45.0) | |
| Grade III | 5 (4.4) | 3 (15.0) | |
| Grade IV | 1 (0.9) | 1 (5.0) | |
| Preoperative medication of DA | 0.476 d | ||
| With | 36 (31.9) | 8 (40.0) | |
| Without | 77 (68.1) | 12 (60.0) | |
| Locational relationship between tumor and pituitary (%) | 0.000 c | ||
| Hypo-pituitary | 47 (41.6) | 4 (20.0) | |
| Para-pituitary | 62 (54.9) | 10 (50.0) | |
| Supra-pituitary | 4 (3.5) | 6 (30.0) | |
| Preoperation PRL, ng/mL (mean ± SD) | 150.14 ± 106.11 | 123.90 ± 88.98 | 0.299 a |
| Postoperation PRL, ng/mL (mean ± SD) | 4.81 ± 8.74 | 13.81 ± 13.64 | 0.009 a |
| Predictive | Uni Variable Analyses OR (95% CI) | p Value | Multivariable Analyses OR (95% CI) | p Value |
|---|---|---|---|---|
| Age | 1.060 (0.980–1.147) | 0.148 | ||
| 1.078 (0.963–1.207) | 0.191 | |||
| Medication (preoperative) | 1.357 (0.539–3.416) | 0.517 | ||
| 4.020 (1.142–14.151) | 0.030 | 8.075 (1.309–49.813) | 0.024 | |
| Tumor diameter | 1.200 (0.946–1.521) | 0.133 | ||
| 0.915 (0.618–1.356) | 0.659 | |||
| Ki-67 | 0.923 (0.709–1.202) | 0.553 | ||
| 1.001 (0.659–1.520) | 0.997 | |||
| Preoperative PRL levels | 0.993 (0.989–0.996) | 0.000 | 0.992 (0.986–0.998) | 0.015 |
| 0.986 (0.981–0.992) | 0.000 | 0.982 (0.970–0.93) | 0.002 | |
| Postoperative PRL levels | 0.807 (0.751–0.867) | 0.000 | 0.830 (0.758–0.908) | 0.000 |
| 0.827 (0.762–0.897) | 0.000 | 0.831 (0.752–0.918) | 0.000 | |
| Knosp grading | 0.466 (0.274–0.790) | 0.005 | 0.981 (0.404–2.378) | 0.966 |
| 0.322 (0.155–0.669) | 0.002 | 0.444 (0.087–2.265) | 0.329 | |
| Locational relationship between tumor and pituitary | 0.449 (0.217–0.932) | 0.032 | 1.546 (0.420–5.684) | 0.512 |
| 0.319 (0.118–0.861) | 0.024 | 0.492 (0.045–5.425) | 0.563 | |
| Classification of pseudocapsule | 2.759 (1.436–5.302) | 0.002 | 1.819 (0.595–5.556) | 0.294 |
| 3.134 (1.286–7.638) | 0.012 | 0.419 (0.025–6.956) | 0.544 | |
| GTR | 25.682 (8.470–77.873) | 0.000 | 1.901 (0.297–12.170) | 0.498 |
| 62.400 (14.346–271.423) | 0.000 | 0.018 (0.003–0.110) | 0.000 |
| Variables | Patients (n = 133) | ||
|---|---|---|---|
| Postoperative complications (%) | |||
| Epistaxis | 2 (1.5) | ||
| CSF rhinorrhea | 1 (0.8) | ||
| Temporary diabetes insipidus | 5 (3.8) | ||
| Hypophysis hypofunction | 4 (3.0) | ||
| Hormonal axis | Preoperation | Postoperation | p value |
| Adrenal axis (%) | 5 (3.8) | 2 (1.5) | 0.447 a |
| Gonadal axis (%) | 2 (1.5) | 1 (0.8) | 1.000 a |
| Thyroidal axis (%) | 3 (2.3) | 1 (0.8) | 0.622 a |
| Hypo-Pituitary | Para-Pituitary | Supra-Pituitary | p Value | |
|---|---|---|---|---|
| Total (n) | 51 | 72 | 10 | |
| Age, years (mean ± SD) | 27.8 ± 7.2 | 27.5 ± 6.2 | 23.4 ± 3.6 | 0.143 a |
| Tumor diameter, mm (mean ± SD) | 8.6 ± 1.6 | 8.5 ± 1.6 | 7.3 ± 2.3 | 0.087 a |
| Ki-67(%) | 0.589 b | |||
| <3 | 44 (86.3) | 57 (79.2) | 9 (90.0) | |
| ≥3 | 7 (13.7) | 15 (20.8) | 1 (10.0) | |
| Preoperation PRL (ng/mL) | 0.083 b | |||
| <200 | 46 (90.2) | 54 (75.0) | 8 (80.0) | |
| ≥200 | 5 (9.8) | 18 (25.0) | 2 (20.0) | |
| Knosp grade (%) | 0.000 c | |||
| Grade 0 | 27 (52.9) | 4 (5.6) | 2 (20.0) | |
| Grade I | 18 (35.3) | 35 (48.6) | 4 (40.0) | |
| Grade II | 4 (7.8) | 28 (38.9) | 4 (40.0) | |
| Grade III | 2 (3.9) | 4 (5.6) | 0 (0) | |
| Grade IV | 0 (0) | 1 (1.4) | 0 (0) | |
| Classification of pseudocapsule (%) | 0.000 c | |||
| Complete | 32 (62.7) | 20 (27.8) | 1 (10.0) | |
| Incomplete | 15 (29.5) | 42 (58.3) | 3 (30.0) | |
| No | 4 (7.8) | 10 (13.9) | 6 (60.0) | |
| Preoperation PRL, ng/mL (mean ± SD) | 125.06 ± 68.52 | 162.25 ± 123.87 | 138.40 ± 79.72 | 0.143 a |
| Postoperation PRL, ng/mL (mean ± SD) | 2.51 ± 2.99 | 8.45 ± 12.48 | 8.33 ± 9.76 | 0.004 a |
| Initial remission rate (%) | 51 (100) | 63 (87.5) | 9 (90.0) | 0.015 b |
| Surgical remission rate (%) | 50 (98.0) | 61 (84.7) | 8 (80.0) | 0.018 b |
| Long-term remission rate (%) | 42 (95.5) | 53 (80.3) | 7 (77.8) | 0.045 b |
| Recurrence rate (%) | 0 (0) | 10 (15.2) | 1 (11.1) | 0.012 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Guo, X.; Miao, Z.; Zhang, Z.; Liu, S.; Wan, X.; Shu, K.; Yang, Y.; Lei, T. Extra-Pseudocapsular Transsphenoidal Surgery for Microprolactinoma in Women. J. Clin. Med. 2022, 11, 3920. https://doi.org/10.3390/jcm11133920
Chen J, Guo X, Miao Z, Zhang Z, Liu S, Wan X, Shu K, Yang Y, Lei T. Extra-Pseudocapsular Transsphenoidal Surgery for Microprolactinoma in Women. Journal of Clinical Medicine. 2022; 11(13):3920. https://doi.org/10.3390/jcm11133920
Chicago/Turabian StyleChen, Juan, Xiang Guo, Zhuangzhuang Miao, Zhuo Zhang, Shengwen Liu, Xueyan Wan, Kai Shu, Yan Yang, and Ting Lei. 2022. "Extra-Pseudocapsular Transsphenoidal Surgery for Microprolactinoma in Women" Journal of Clinical Medicine 11, no. 13: 3920. https://doi.org/10.3390/jcm11133920
APA StyleChen, J., Guo, X., Miao, Z., Zhang, Z., Liu, S., Wan, X., Shu, K., Yang, Y., & Lei, T. (2022). Extra-Pseudocapsular Transsphenoidal Surgery for Microprolactinoma in Women. Journal of Clinical Medicine, 11(13), 3920. https://doi.org/10.3390/jcm11133920







