How Old Is Old? An Age-Stratified Analysis of Elderly Liver Donors above 65
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Demographic Data
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
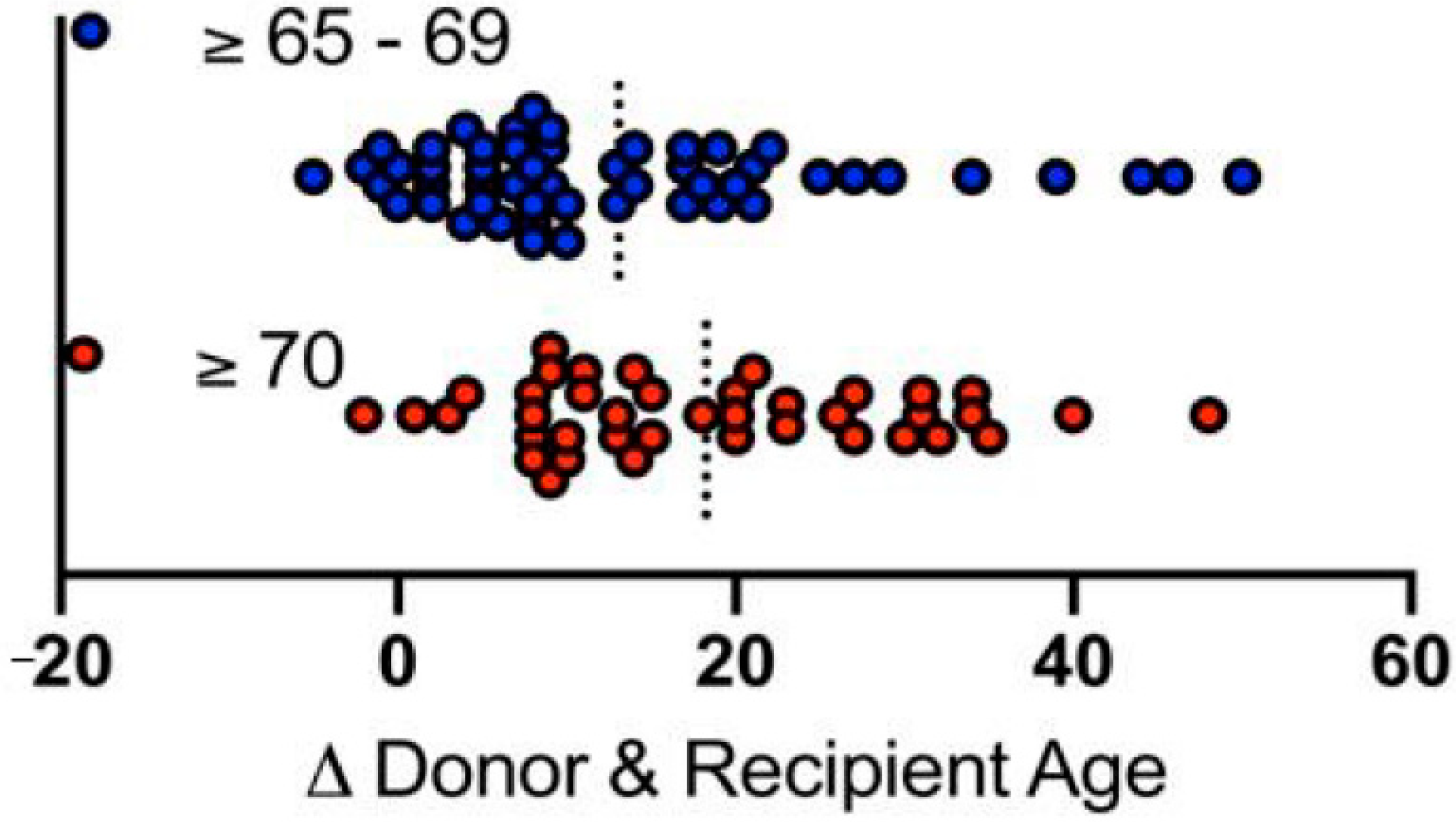
3.1. Study Population Characteristics
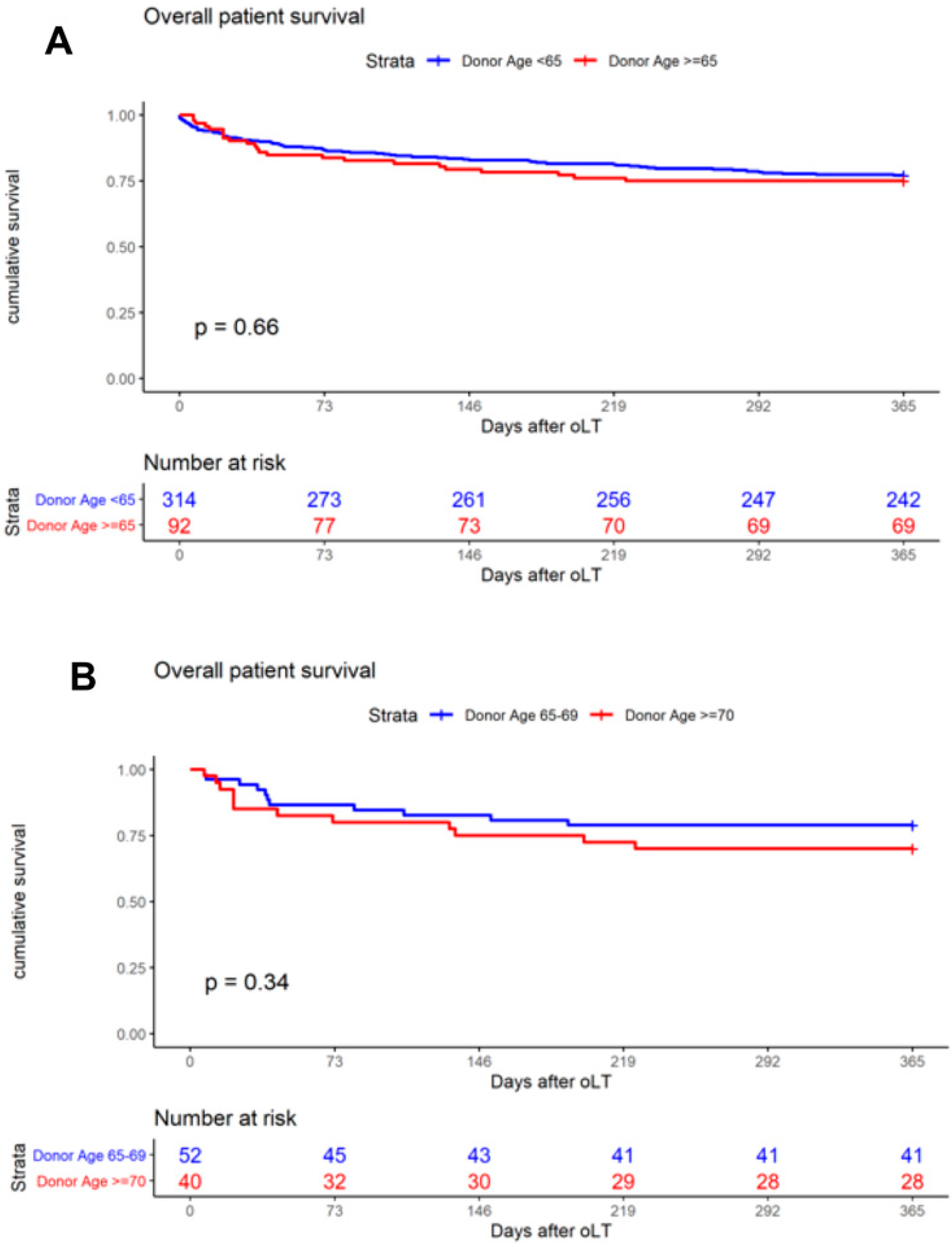
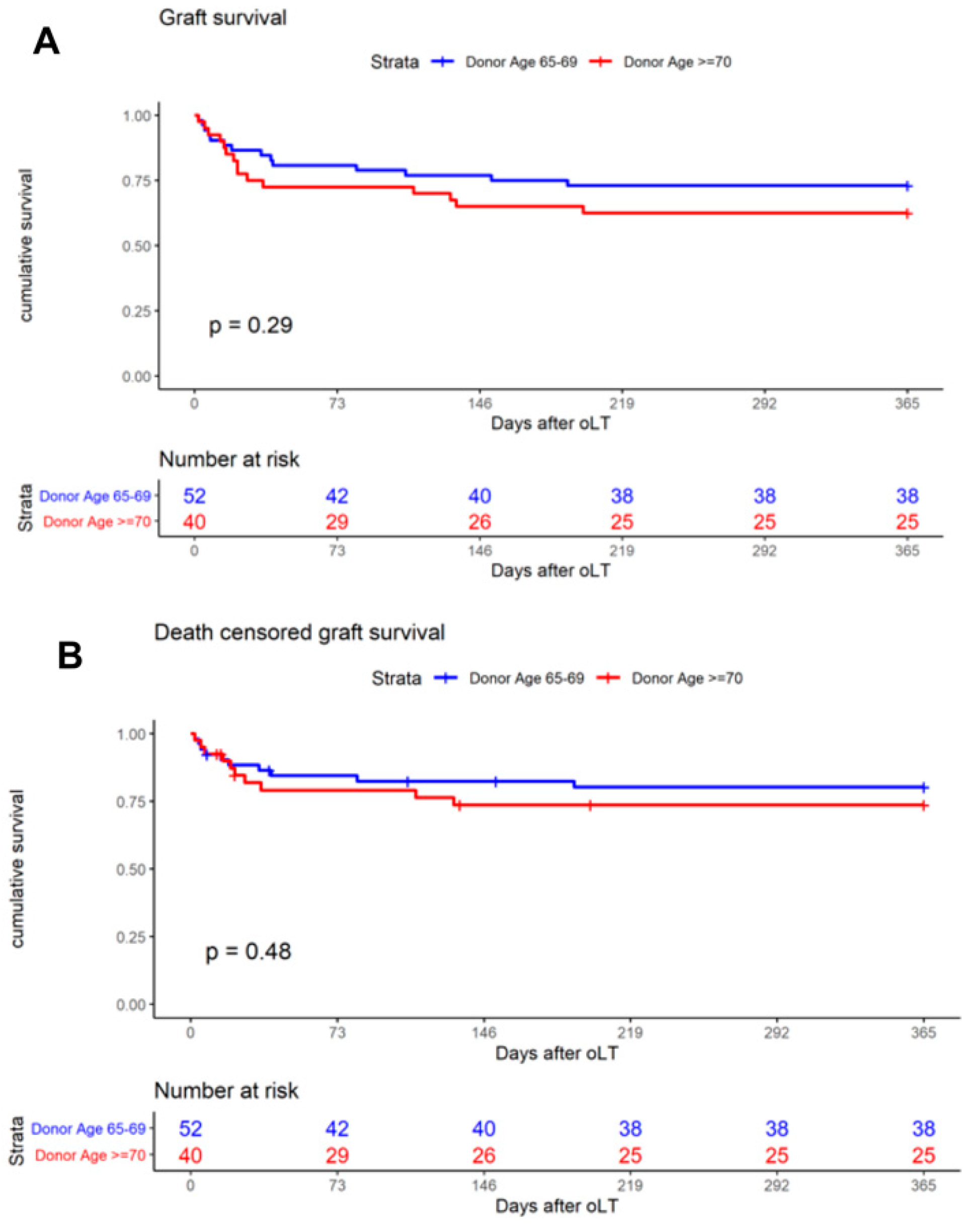
3.2. One-Year Patient and Graft Survival
3.3. Additional Outcome Parameters
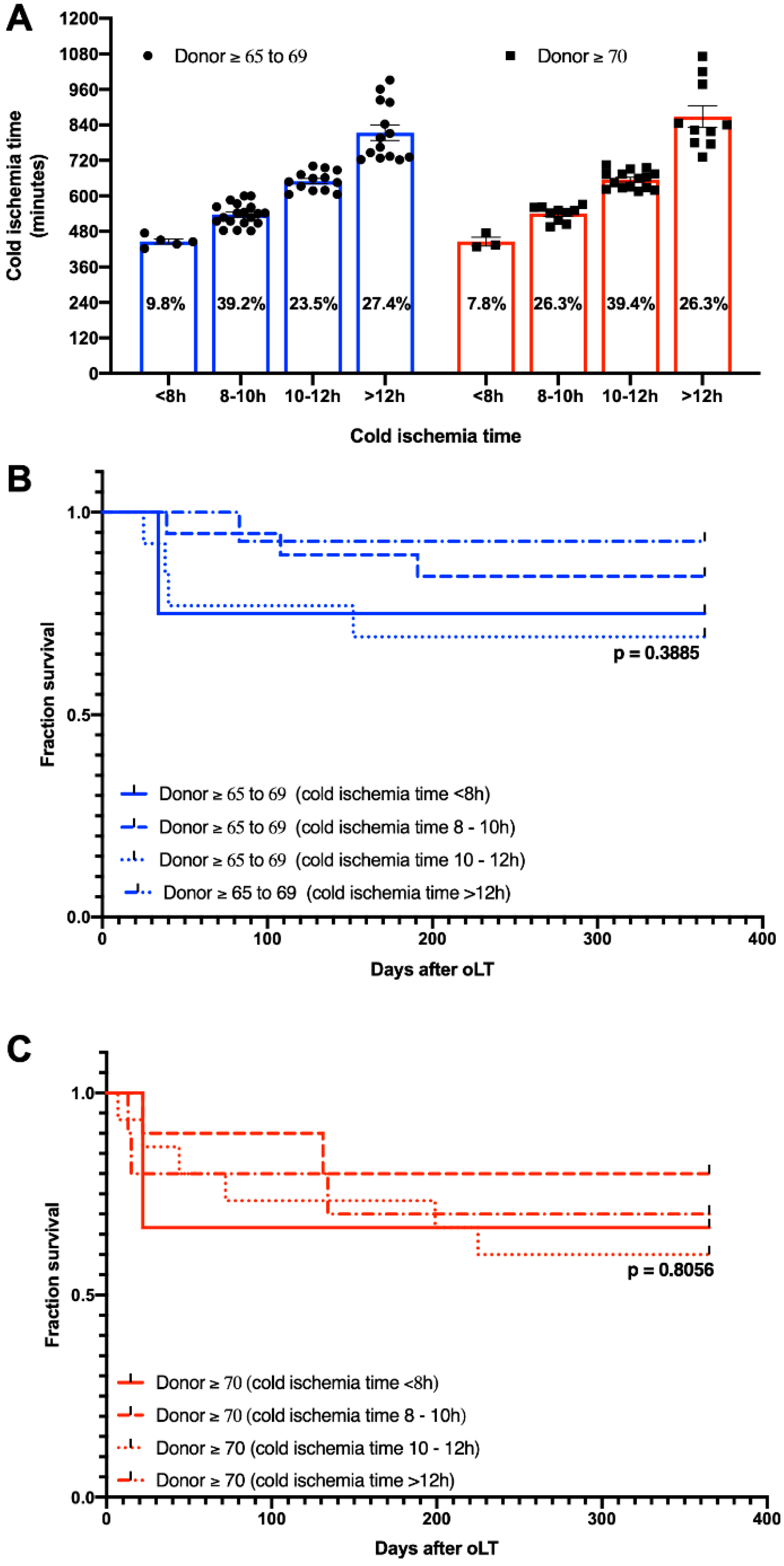
3.4. Effect of CIT
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bodzin, A.S.; Baker, T.B. Liver Transplantation Today: Where We Are Now and Where We Are Going. Liver Transplant. 2018, 24, 1470–1475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houben, P.; Döhler, B.; Weiß, K.H.; Mieth, M.; Mehrabi, A.; Süsal, C. Differential Influence of Donor Age Depending on the Indication for Liver Transplantation—A Collaborative Transplant Study Report. Transplantation 2020, 104, 779–787. [Google Scholar] [CrossRef]
- de Boer, J.D.; Blok, J.J.; Putter, H.; Koopman, J.J.E.; van Hoek, B.; Samuel, U.; van Rosmalen, M.; Metselaar, H.J.; Alwayn, I.P.J.; Guba, M.; et al. Optimizing the Use of Geriatric Livers for Transplantation in the Eurotransplant Region. Liver Transplant. 2018, 25, 260–274. [Google Scholar] [CrossRef] [Green Version]
- Feng, S.; Goodrich, N.; Bragg-Gresham, J.; Dykstra, D.; Punch, J.; DebRoy, M.; Greenstein, S.; Merion, R. Characteristics Associated with Liver Graft Failure: The Concept of a Donor Risk Index. Am. J. Transplant. 2006, 6, 783–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halazun, K.; Rana, A.A.; Fortune, B.; Quillin, R.C.; Verna, E.C.; Samstein, B.; Guarrera, J.V.; Kato, T.; Griesemer, A.D.; Fox, A.; et al. No country for old livers? Examining and optimizing the utilization of elderly liver grafts. Am. J. Transplant. 2017, 18, 669–678. [Google Scholar] [CrossRef] [Green Version]
- Machicao, V.I.; Bonatti, H.; Krishna, M.; Aqel, B.A.; Lukens, F.J.; Nguyen, J.H.; Rosser, B.G.; Satyanarayana, R.; Grewal, H.P.; Hewitt, W.R.; et al. Donor age affects fibrosis progression and graft survival after liver transplantation for hepatitis C1. Transplantation 2004, 77, 84–92. [Google Scholar] [CrossRef]
- Haugen, C.E.; Bowring, M.G.; Holscher, C.M.; Jackson, K.R.; Garonzik-Wang, J.; Cameron, A.M.; Philosophe, B.; McAdams-DeMarco, M.; Segev, D.L. Survival benefit of accepting livers from deceased donors over 70 years old. Am. J. Transplant. 2019, 19, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Olthoff, K.M.; Kulik, L.; Samstein, B.; Kaminski, M.; Abecassis, M.; Emond, J.; Shaked, A.; Christie, J.D. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transplant. 2010, 16, 943–949. [Google Scholar] [CrossRef]
- Becker, F.; Vogel, T.; Voß, T.; Mehdorn, A.-S.; Schütte-Nütgen, K.; Reuter, S.; Mohr, A.; Kabar, I.; Bormann, E.; Vowinkel, T.; et al. The weekend effect in liver transplantation. PLoS ONE 2018, 13, e0198035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Becker, F.; Voß, T.; Mohr, A.; Mehdorn, A.-S.; Schütte-Nütgen, K.; Reuter, S.; Kabar, I.; Bormann, E.; Vowinkel, T.; Palmes, D.; et al. Impact of nighttime procedures on outcomes after liver transplantation. PLoS ONE 2019, 14, e0220124. [Google Scholar] [CrossRef] [Green Version]
- Cassuto, J.R.; Patel, S.A.; Tsoulfas, G.; Orloff, M.S.; Abt, P.L. The Cumulative Effects of Cold Ischemic Time and Older Donor Age on Liver Graft Survival. J. Surg. Res. 2008, 148, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Cotter, T.G.; Paul, S.; Sandıkçı, B.; Couri, T.; Bodzin, A.S.; Little, E.C.; Sundaram, V.; Charlton, M. Improved Graft Survival After Liver Transplantation for Recipients With Hepatitis C Virus in the Direct-Acting Antiviral Era. Liver Transplant. 2019, 25, 598–609. [Google Scholar] [CrossRef] [PubMed]
- Cotter, T.G.; Paul, S.; Sandıkçı, B.; Couri, T.; Bodzin, A.S.; Little, E.C.; Sundaram, V.; Charlton, M. Increasing Utilization and Excellent Initial Outcomes Following Liver Transplant of Hepatitis C Virus (HCV)-Viremic Donors Into HCV-Negative Recipients: Outcomes Following Liver Transplant of HCV-Viremic Donors. Hepatology 2019, 69, 2381–2395. [Google Scholar] [CrossRef] [PubMed]
- Durand, F.; Francoz, C. Optimizing Allocation of Older Donors in Liver Transplantation: The Objectives of Allocation Policies Also Matter. Transplantation 2020, 104, 673–674. [Google Scholar] [CrossRef] [PubMed]
- Moosburner, S.; Ritschl, P.V.; Wiering, L.; Gassner, J.M.G.V.; Öllinger, R.; Pratschke, J.; Sauer, I.M.; Raschzok, N. High donor age for liver transplantation: Tackling organ scarcity in Germany. Der Chirurg Zeitschrift fur Alle Gebiete der Oper. Med. 2019, 90, 744–751. [Google Scholar]
- Gastaca, M.; Guerra, M.; Martinez, L.A.; Ruiz, P.; Ventoso, A.; Palomares, I.; Prieto, M.; Matarranz, A.; Valdivieso, A.; de Urbina, J.O. Octogenarian Donors in Liver Transplantation. Transplant. Proc. 2016, 48, 2856–2858. [Google Scholar] [CrossRef]
- Biancofiore, G.; Bindi, M.; Ghinolfi, D.; Lai, Q.; Bisa, M.; Esposito, M.; Meacci, L.; Mozzo, R.; Spelta, A.; Filipponi, F. Octogenarian donors in liver transplantation grant an equivalent perioperative course to ideal young donors. Dig. Liver Dis. 2017, 49, 676–682. [Google Scholar] [CrossRef]
- Martín, L.G.; Grande, A.M.; Roux, D.P.; Cibrián, C.G.; Martín, C.F.; Gandía, M.R.; Buenadicha, A.L. Short-term Results of Liver Transplantation With Octogenarian Donors. Transplant. Proc. 2018, 50, 184–191. [Google Scholar] [CrossRef]
- Bertuzzo, V.R.; Cescon, M.; Odaldi, F.; Di Laudo, M.; Cucchetti, A.; Ravaioli, M.; Del Gaudio, M.; Ercolani, G.; D’Errico, A.; Pinna, A.D. Actual Risk of Using Very Aged Donors for Unselected Liver Transplant Candidates: A European Single-center Experience in the MELD Era. Ann. Surg. 2017, 265, 388–396. [Google Scholar] [CrossRef]
- Becker, F.; Pascher, A.; Brockmann, J.G. Maschinenperfusion zur Konditionierung der Leber und Niere vor Transplantation. Der Chirurg Zeitschrift fur Alle Gebiete der Oper. Med. 2020, 91, 913–917. [Google Scholar] [CrossRef]
- Ghinolfi, D.; Rreka, E.; De Tata, V.; Franzini, M.; Pezzati, D.; Fierabracci, V.; Masini, M.; Insilla, A.C.; Bindi, M.L.; Marselli, L.; et al. Pilot, Open, Randomized, Prospective Trial for Normothermic Machine Perfusion Evaluation in Liver Transplantation From Older Donors. Liver Transplant. 2019, 25, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Segev, D.L.; Maley, W.R.; Simpkins, C.E.; Locke, J.E.; Nguyen, G.C.; Montgomery, R.A.; Thuluvath, P.J. Minimizing risk associated with elderly liver donors by matching to preferred recipients. Hepatology 2007, 46, 1907–1918. [Google Scholar] [CrossRef]
- Haugen, C.E.; Thomas, A.; Garonzik-Wang, J.; Massie, A.B.; Segev, D.L. Minimizing Risk Associated With Older Liver Donors by Matching to Preferred Recipients: A National Registry and Validation Study. Transplantation 2018, 102, 1514–1519. [Google Scholar] [CrossRef] [PubMed]
- Dasari, B.V.; Mergental, H.; Isaac, J.R.; Muiesan, P.; Mirza, D.F.; Perera, T. Systematic review and meta-analysis of liver transplantation using grafts from deceased donors aged over 70 years. Clin. Transplant. 2017, 31, e13139. [Google Scholar] [CrossRef]
- Pratschke, S.; Bender, A.; Boesch, F.; Andrassy, J.; van Rosmalen, M.; Samuel, U.; Rogiers, X.; Meiser, B.; Küchenhoff, H.; Driesslein, D.; et al. Association between donor age and risk of graft failure after liver transplantation: An analysis of the Eurotransplant database. Transpl. Int. 2018, 32, 270–279. [Google Scholar] [CrossRef]
| <65 (n = 314) | ≥65 (n = 92) | p-Value | |
|---|---|---|---|
| Age (mean ± SD) | 51.5 ± 11.9 | 55.4 ± 10.3 | 0.005 a |
| Gender (% males) | 64.3 | 65.2 | 0.902 b |
| BMI (mean ± SD) | 26.00 ± 5.4 | 26.86 ± 4.7 | 0.051 a |
| Indications for transplant (%) | 0.455 b | ||
| ALF | 14.3 | 8.7 | |
| HCC | 21.0 | 22.8 | |
| Viral hepatitis | 12.7 | 10.8 | |
| PSC, PBC, SSC | 12.1 | 13.0 | |
| Alcoholic cirrhosis | 13.6 | 23.9 | |
| Cirrhosis other | 7.3 | 7.6 | |
| Other | 19.4 | 13.0 | |
| HCV (% antibody positive) | 16.5 | 14.1 | 0.631 b |
| Cold ischemia time (min, mean ± SD) | 616.1 ± 167.9 | 641.1 ± 143.9 | 0.245 a |
| Warm ischemia time (min, mean ± SD) | 40.4 ± 9.6 | 40.2 ± 8.1 | 0.968 a |
| labMELD (mean ± SD) | 22.5 ± 11.9 | 21.8 ± 11.9 | 0.722 a |
| HU status (n) | 22 | 1 | 0.037 b |
| Previous transplants (% ≥1) | 12.7 | 8.7 | 0.360 b |
| ≥65–69 (n = 52) | ≥70 (n = 40) | p-Value | |
|---|---|---|---|
| Age (mean ± SD) | 54.7 ± 10.6 | 56.3 ± 9.9 | 0.462 a |
| Gender (% males) | 71.1 | 57.5 | 0.191 b |
| BMI (mean ± SD) | 26.89 ± 4.6 | 26.82 ± 4.8 | 0.793 a |
| Indications for transplant (%) | 0.073 b | ||
| ALF | 13.5 | 2.5 | |
| HCC | 17.3 | 30.0 | |
| Viral hepatitis | 11.5 | 10.0 | |
| PSC, PBC, SSC | 13.4 | 12.5 | |
| Alcoholic cirrhosis | 15.3 | 35.0 | |
| Cirrhosis other | 11.5 | 2.5 | |
| Other | 13.5 | 7.5 | |
| HCV (% antibody positive) | 11.5 | 17.5 | 0.548 b |
| Cold ischemia time (min, mean ± SD) | 632.9 ± 137.1 | 651.5 ± 153.4 | 0.580 a |
| Warm ischemia time (min, mean ± SD) | 40.6 ± 8.6 | 39.8 ± 7.5 | 0.726 a |
| labMELD (mean ± SD) | 23.4 ± 12.9 | 20.1 ± 10.3 | 0.299 a |
| HU status (n) | 1 | 0 | 0.066 b |
| Previous transplants (% ≥1) | 7.69 | 10.0 | 0.724 b |
| ≥65–69 (n = 52) | ≥70 (n = 40) | p-Value | |
|---|---|---|---|
| Age (mean ± SD) | 66.8 ± 1.5 | 74.7 ± 3.7 | <0.0001 a |
| Gender (% males) | 63.5 | 50.0 | 0.209 b |
| BMI (mean ± SD) | 27.4 ± 3.9 | 26.6 ± 2.8 | 0.381 a |
| Donor Center (% national) | 86.5 | 87.5 | 1.000 b |
| DRI (mean ± SD) | 2.0 ± 0.2 | 2.2 ± 0.3 | <0.0001 a |
| ≥65–69 (n = 52) | ≥70 (n = 40) | p-Value | |
|---|---|---|---|
| Patient survival (%) | 0.335 b | ||
| 30 d | 94.2 | 85.0 | |
| 90 d | 84.6 | 80.0 | |
| 365 d | 78.8 | 70.0 | |
| Graft survival (%) | 0.291 b | ||
| 30 d | 86.5 | 75.0 | |
| 90 d | 78.8 | 72.5 | |
| 365 d | 73.1 | 62.6 | |
| Re-oLT within 1y (%) | 9.6 | 20.0 | 0.227 b |
| PNF (%) | 15.3 | 7.5 | 0.337 b |
| Biopsy-proven rejection (%) | 19.2 | 15.0 | 0.782 b |
| Re-operation (%) | 55.8 | 65.0 | 0.398 b |
| Number of reoperations (median MIN, MAX) | 1 (0.12) | 1 (0.8) | 0.101 a |
| EAD (%) | 41.17 | 42.50 | 0.898 b |
| Peak AST (U/l) | 5932.4 ± 7269.0 | 4576.5 ± 5045.4 | 0.878 a |
| Peak ALT (U/l) | 3453.5 ± 4528.9 | 2646.6 ± 3246.9 | 0.829 a |
| ITBL (%) | 3.93 | 5.00 | 0.960 b |
| Stay at ICU (d, mean ± SD) | 12.9 ± 17.7 | 13.8 ± 19.4 | 0.971 a |
| Initial hospital stay (d, mean ± SD) | 48.5 ± 33.0 | 47.2 ± 36.0 | 0.545 a |
| Number of readmissions (mean ± median (MIN, MAX)) | 2 (0–10) | 1 (0–8) | 0.678 a |
| Length of readmissions (d, median (MIN, MAX)) | 22.0 (0.122) | 21 (0.191) | 0.762 a |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Donor age (continuous variable) | 1.054 (0.976–1.139) | 0.1808 | ||
| Donor age (≥65–69 vs. ≥70) | 0.671 (0.296–1.521) | 0.3395 | ||
| Recipient age | 0.992 (0.954–1.032) | 0.7017 | ||
| HCV (positive vs. negative) | 1.825 (0.428–7.783) | 0.4163 | ||
| Cold ischemia time | 1.000 (0.997–1.003) | 0.9076 | ||
| Warm ischemia time | 1.039 (0.988–1.092) | 0.1325 | ||
| labMELD | 1.011 (0.975–1.048) | 0.5520 | ||
| PNF (yes vs. no) | 5.660 (2.307–13.883) | 0.0002 | ||
| Biopsy-proven rejection (yes vs. no) | 1.874 (0.738–4.756) | 0.1865 | ||
| Re-operation (yes vs. no) | 18.694 (2.518–138.808) | 0.0042 | 23.971 (3.163–181.638) | 0.0021 |
| Number of readmissions | 0.331 (0.188–0.584) | 0.0001 | 0.308 (0.171–0.554) | <0.0001 |
| Stay at ICU | 1.029 (1.016–1.041) | <0.0001 | ||
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Donor age (continuous variable) | 1.032 (0.946–1.125) | 0.4840 | ||
| Donor age (≥65–69 vs. ≥70) | 0.732 (0.305–1.759) | 0.4856 | 0.215 (0.067–0.688) | 0.0096 |
| Recipient age | 1.019 (0.971–1.069) | 0.4511 | ||
| HCV (positive vs. negative) | 0.899 (0.263–3.067) | 0.8644 | ||
| Cold ischemia time | 1.001 (0.998–1.004) | 0.6721 | ||
| Warm ischemia time | 1.009 (0.956–1.066) | 0.7400 | ||
| labMELD | 1.017 (0.979–1.056) | 0.3899 | ||
| PNF (yes vs. no) | 49.862 (16.468–150.975) | <0.0001 | 70.749 (18.744–267.043) | <0.0001 |
| Biopsy-proven rejection (yes vs. no) | 0.863 (0.253–2.948) | 0.8143 | ||
| Re-operation (yes vs. no) | 0.9888 | |||
| Number of readmissions | 0.668 (0.487–0.918) | 0.0129 | ||
| Stay at ICU | 1.029 (1.016–1.042) | <0.0001 | 1.036 (1.017–1.055) | 0.0002 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Donor age (continuous variable) | 1.048 (0.977–1.125) | 0.1887 | ||
| Donor age (≥65–69 vs. ≥70) | 0.678 (0.327–1.404) | 0.2952 | 0.270 (0.102–0.711) | 0.0081 |
| Recipient age | 0.986 (0.952–1.021) | 0.4351 | ||
| HCV (positive vs. negative) | 1.384 (0.419–4.573) | 0.5923 | ||
| Cold ischemia time | 1.001 (0.998–1.003) | 0.6600 | ||
| Warm ischemia time | 1.019 (0.975–1.066) | 0.4018 | ||
| labMELD | 1.013 (0.981–1.045) | 0.4266 | ||
| PNF (yes vs. no) | 32.894 (12.940–83.620) | <0.0001 | 33.421 (10.391–107.490) | <0.0001 |
| Biopsy-proven rejection (yes vs. no) | 1.578 (0.674–3.699) | 0.2935 | ||
| Re-operation (yes vs. no) | 26.129 (3.550–192.310) | 0.0014 | 10.182 (1.293–80.172) | |
| Number of readmissions | 0.612 (0.458–0.817) | 0.0009 | ||
| Stay at ICU | 1.030 (1.019–1.041) | <0.0001 | 1.027 (1.010–1.043) | 0.0015 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Houben, P.; Bormann, E.; Kneifel, F.; Katou, S.; Morgül, M.H.; Vogel, T.; Bahde, R.; Radünz, S.; Pascher, A.; Schmidt, H.; et al. How Old Is Old? An Age-Stratified Analysis of Elderly Liver Donors above 65. J. Clin. Med. 2022, 11, 3899. https://doi.org/10.3390/jcm11133899
Houben P, Bormann E, Kneifel F, Katou S, Morgül MH, Vogel T, Bahde R, Radünz S, Pascher A, Schmidt H, et al. How Old Is Old? An Age-Stratified Analysis of Elderly Liver Donors above 65. Journal of Clinical Medicine. 2022; 11(13):3899. https://doi.org/10.3390/jcm11133899
Chicago/Turabian StyleHouben, Philipp, Eike Bormann, Felicia Kneifel, Shadi Katou, Mehmet Haluk Morgül, Thomas Vogel, Ralf Bahde, Sonia Radünz, Andreas Pascher, Hartmut Schmidt, and et al. 2022. "How Old Is Old? An Age-Stratified Analysis of Elderly Liver Donors above 65" Journal of Clinical Medicine 11, no. 13: 3899. https://doi.org/10.3390/jcm11133899
APA StyleHouben, P., Bormann, E., Kneifel, F., Katou, S., Morgül, M. H., Vogel, T., Bahde, R., Radünz, S., Pascher, A., Schmidt, H., Brockmann, J. G., & Becker, F. (2022). How Old Is Old? An Age-Stratified Analysis of Elderly Liver Donors above 65. Journal of Clinical Medicine, 11(13), 3899. https://doi.org/10.3390/jcm11133899





