Outcomes of Microhook ab Interno Trabeculotomy in Consecutive 36 Eyes with Uveitic Glaucoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
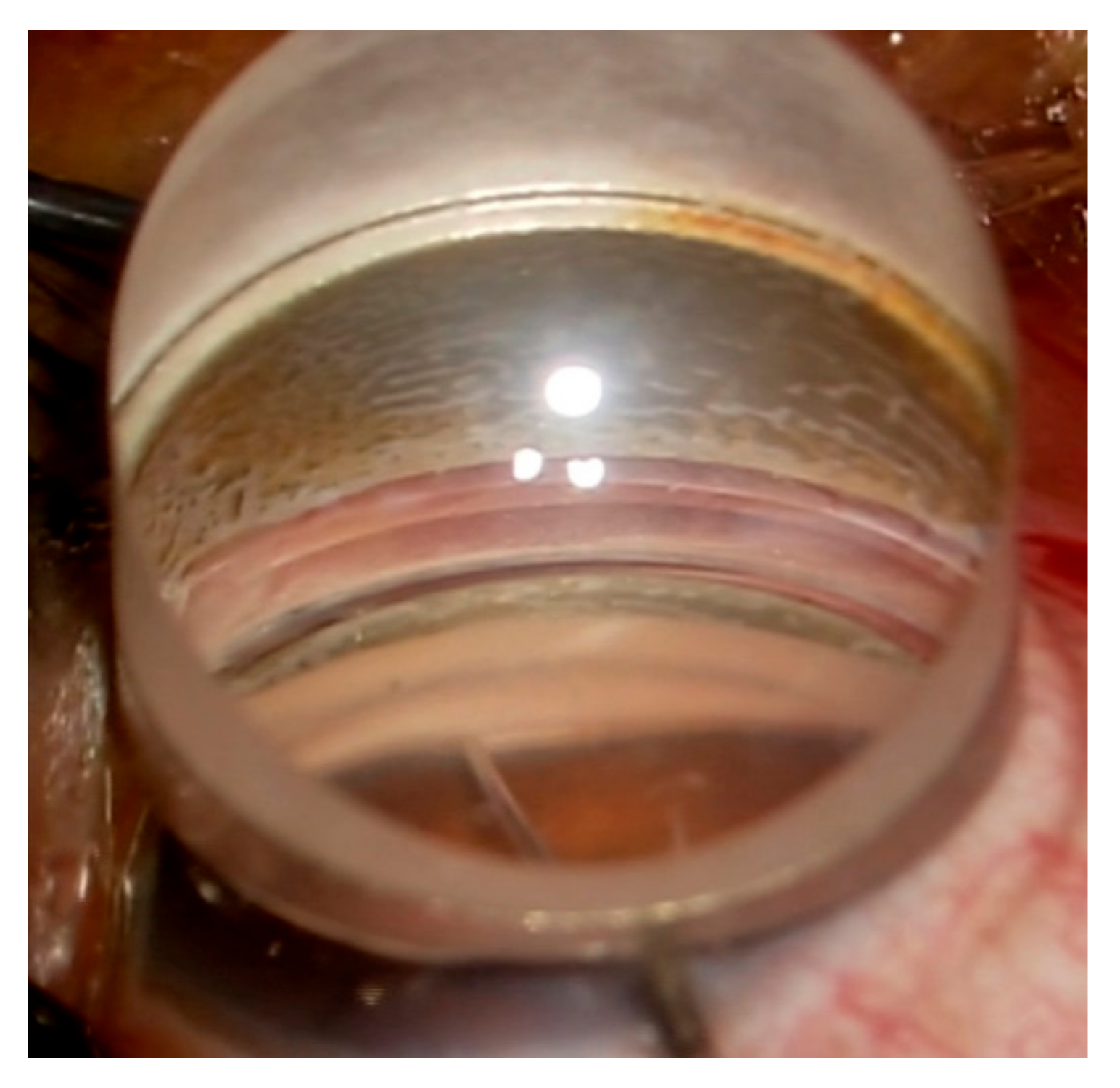
2.3. Surgical Procedure
2.4. Outcomes
2.5. Statistical Analyses
3. Results
3.1. Preoperative Characteristics
3.2. Surgical Outcomes
3.3. Change in Inflammation
3.4. Complications
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Daniel, E.; Pistilli, M.; Kothari, S.; Khachatryan, N.; Kacmaz, R.O.; Gangaputra, S.S.; Sen, H.N.; Suhler, E.B.; Thorne, J.E.; Foster, C.S.; et al. Risk of Ocular Hypertension in Adults with Noninfectious Uveitis. Ophthalmology 2017, 124, 1196–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsirouki, T.; Dastiridou, A.; Symeonidis, C.; Tounakaki, O.; Brazitikou, I.; Kalogeropoulos, C.; Androudi, S. A Focus on the Epidemiology of Uveitis. Ocul. Immunol. Inflamm. 2018, 26, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Panek, W.C.; Holland, G.N.; Lee, D.A.; Christensen, R.E. Glaucoma in patients with uveitis. Br. J. Ophthalmol. 1990, 74, 223–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merayo-Lloves, J.; Power, W.J.; Rodriguez, A.; Pedroza-Seres, M.; Foster, C.S. Secondary glaucoma in patients with uveitis. Ophthalmologica 1999, 213, 300–304. [Google Scholar] [CrossRef]
- Herbert, H.M.; Viswanathan, A.; Jackson, H.; Lightman, S.L. Risk factors for elevated intraocular pressure in uveitis. J. Glaucoma 2004, 13, 96–99. [Google Scholar] [CrossRef]
- Neri, P.; Azuara-Blanco, A.; Forrester, J.V. Incidence of glaucoma in patients with uveitis. J. Glaucoma 2004, 13, 461–465. [Google Scholar] [CrossRef]
- Kanda, T.; Shibata, M.; Taguchi, M.; Ishikawa, S.; Harimoto, K.; Takeuchi, M. Prevalence and aetiology of ocular hypertension in acute and chronic uveitis. Br. J. Ophthalmol. 2014, 98, 932–936. [Google Scholar] [CrossRef]
- Al Rubaie, K.; Al Dhahri, H.; Al Fawaz, A.; Hemachandran, S.; Mousa, A.; Mohamed, A.G.; Al-Obeidan, S.A.; Abu El-Asrar, A.M. Incidence and Risk Factors for Developing Glaucoma Among Patients with Uveitis in a University-based Tertiary Referral Center in Riyadh, Saudi Arabia. Ocul. Immunol. Inflamm. 2016, 24, 571–578. [Google Scholar] [CrossRef]
- Tomkins-Netzer, O.; Talat, L.; Bar, A.; Lula, A.; Taylor, S.R.; Joshi, L.; Lightman, S. Long-term clinical outcome and causes of vision loss in patients with uveitis. Ophthalmology 2014, 121, 2387–2392. [Google Scholar] [CrossRef]
- Ohno, S.; Umebayashi, I.; Matsukawa, M.; Goto, T.; Yano, T. Safety and efficacy of infliximab in the treatment of refractory uveoretinitis in Behcet’s disease: A large-scale, long-term postmarketing surveillance in Japan. Arthritis Res. Ther. 2019, 21, 2. [Google Scholar] [CrossRef] [Green Version]
- Jaffe, G.J.; Dick, A.D.; Brezin, A.P.; Nguyen, Q.D.; Thorne, J.E.; Kestelyn, P.; Barisani-Asenbauer, T.; Franco, P.; Heiligenhaus, A.; Scales, D.; et al. Adalimumab in Patients with Active Noninfectious Uveitis. N. Engl. J. Med. 2016, 375, 932–943. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, Q.D.; Merrill, P.T.; Jaffe, G.J.; Dick, A.D.; Kurup, S.K.; Sheppard, J.; Schlaen, A.; Pavesio, C.; Cimino, L.; Van Calster, J.; et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): A multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet 2016, 388, 1183–1192. [Google Scholar] [CrossRef] [Green Version]
- Suhler, E.B.; Adan, A.; Brezin, A.P.; Fortin, E.; Goto, H.; Jaffe, G.J.; Kaburaki, T.; Kramer, M.; Lim, L.L.; Muccioli, C.; et al. Safety and Efficacy of Adalimumab in Patients with Noninfectious Uveitis in an Ongoing Open-Label Study: VISUAL III. Ophthalmology 2018, 125, 1075–1087. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.W.; Kusuhara, S.; Imai, H.; Sotani, N.; Nishisho, R.; Matsumiya, W.; Nakamura, M. Outcomes of Primary 27-Gauge Vitrectomy for 73 Consecutive Cases with Uveitis-Associated Vitreoretinal Disorders. Front. Med. 2021, 8, 755816. [Google Scholar] [CrossRef]
- Ma, T.; Sims, J.L.; Bennett, S.; Chew, S.; Niederer, R.L. High rate of conversion from ocular hypertension to glaucoma in subjects with uveitis. Br. J. Ophthalmol. 2021. [Google Scholar] [CrossRef]
- Liu, X.; Kelly, S.R.; Montesano, G.; Bryan, S.R.; Barry, R.J.; Keane, P.A.; Denniston, A.K.; Crabb, D.P. Evaluating the Impact of Uveitis on Visual Field Progression Using Large-Scale Real-World Data. Am. J. Ophthalmol. 2019, 207, 144–150. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://www.aaojournal.org/article/S0161-6420(20)31024-1/fulltext (accessed on 18 June 2022).
- Chen, D.Z.; Sng, C.C.A. Safety and Efficacy of Microinvasive Glaucoma Surgery. J. Ophthalmol. 2017, 2017, 3182935. [Google Scholar] [CrossRef]
- Bicket, A.K.; Le, J.T.; Azuara-Blanco, A.; Gazzard, G.; Wormald, R.; Bunce, C.; Hu, K.; Jayaram, H.; King, A.; Otarola, F.; et al. Minimally Invasive Glaucoma Surgical Techniques for Open-Angle Glaucoma: An Overview of Cochrane Systematic Reviews and Network Meta-analysis. JAMA Ophthalmol. 2021, 139, 983–989. [Google Scholar] [CrossRef]
- Pereira, I.C.F.; van de Wijdeven, R.; Wyss, H.M.; Beckers, H.J.M.; den Toonder, J.M.J. Conventional glaucoma implants and the new MIGS devices: A comprehensive review of current options and future directions. Eye 2021, 35, 3202–3221. [Google Scholar] [CrossRef]
- Tanito, M. Microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery. Clin. Ophthalmol. 2018, 12, 43–48. [Google Scholar] [CrossRef] [Green Version]
- Tanito, M.; Matsuo, M. Ab-interno trabeculotomy-related glaucoma surgeries. Taiwan J. Ophthalmol. 2019, 9, 67–71. [Google Scholar] [CrossRef]
- Nussenblatt, R.B.; Palestine, A.G.; Chan, C.C.; Roberge, F. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology 1985, 92, 467–471. [Google Scholar] [CrossRef]
- Mori, S.; Murai, Y.; Ueda, K.; Sakamoto, M.; Kurimoto, T.; Yamada-Nakanishi, Y.; Nakamura, M. Comparison of efficacy and early surgery-related complications between one-quadrant and two-quadrant microhook ab interno trabeculotomy: A propensity score matched study. Acta Ophthalmol. 2021, 99, 898–903. [Google Scholar] [CrossRef] [PubMed]
- Okuda, M.; Mori, S.; Takano, F.; Murai, Y.; Ueda, K.; Sakamoto, M.; Kurimoto, T.; Yamada-Nakanishi, Y.; Nakamura, M. Association of the prolonged use of anti-glaucoma medications with the surgical failure of ab interno microhook trabeculotomy. Acta Ophthalmol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Miserocchi, E.; Carassa, R.G.; Bettin, P.; Brancato, R. Viscocanalostomy in patients with glaucoma secondary to uveitis: Preliminary report. J. Cataract Refract. Surg. 2004, 30, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Anton, A.; Heinzelmann, S.; Ness, T.; Lubke, J.; Neuburger, M.; Jordan, J.F.; Wecker, T. Trabeculectomy ab interno with the Trabectome(R) as a therapeutic option for uveitic secondary glaucoma. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 1973–1978. [Google Scholar] [CrossRef]
- Voykov, B.; Dimopoulos, S.; Leitritz, M.A.; Doycheva, D.; William, A. Long-term results of ab externo trabeculotomy for glaucoma secondary to chronic uveitis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2016, 254, 355–360. [Google Scholar] [CrossRef]
- Miller, V.J.; Young, C.E.C.; SooHoo, J.R.; Seibold, L.K.; Kahook, M.Y.; Pecen, P.E.; Palestine, A.G.; Pantcheva, M.B. Efficacy of Goniotomy with Kahook Dual Blade in Patients with Uveitis-associated Ocular Hypertension. J. Glaucoma 2019, 28, 744–748. [Google Scholar] [CrossRef]
- Tanito, M.; Sugihara, K.; Tsutsui, A.; Hara, K.; Manabe, K.; Matsuoka, Y. Midterm Results of Microhook ab Interno Trabeculotomy in Initial 560 Eyes with Glaucoma. J. Clin. Med. 2021, 10, 814. [Google Scholar] [CrossRef]
- Mori, S.; Tanito, M.; Shoji, N.; Yokoyama, Y.; Kameda, T.; Shoji, T.; Mizoue, S.; Saito, Y.; Ishida, K.; Ueda, T.; et al. Noninferiority of Microhook to Trabectome: Trabectome versus Ab Interno Microhook Trabeculotomy Comparative Study (Tram Trac Study). Ophthalmol. Glaucoma 2021. [Google Scholar] [CrossRef]



| Characteristics | Data | |
|---|---|---|
| Number of patients/affected eyes, n/n | 30/36 | |
| Age (years), median (IQR) | 68.5 (52.5, 72) | |
| Sex, n (%) | ||
| Male | 11 (37) | |
| Female | 19 (63) | |
| Eye, n (%) | ||
| Right | 20 (56) | |
| Left | 16 (44) | |
| Cause of uveitis, n (%) | ||
| Sarcoidosis | 11 (31) | |
| Posner–Schlossman syndrome | 7 (19) | |
| Cytomegalovirus anterior uveitis | 4 (11) | |
| Vogt–Koyanagi–Harada disease | 3 (8) | |
| Scleritis | 3 (8) | |
| Syphilitic uveitis | 1 (3) | |
| Behçet’s disease | 1 (3) | |
| Unclassified | 6 (17) | |
| Previous intraocular surgery, n (%) | ||
| Cataract surgery | 19 (53) | |
| Vitreous surgery | 8 (22) | |
| Glaucoma surgery | 5 (14) | |
| Best-corrected visual acuity (decimal), median (IQR) | 1.0 (0.5, 1.2) | |
| Best-corrected visual acuity (logMAR), median (IQR) | 0.000 (−0.079, 0.301) | |
| Intraocular pressure (mmHg), median (IQR) | 30.5 (24.75, 39) | |
| Glaucoma drug score, median (IQR) | 5 (4, 6) | |
| Mean deviation of visual field (dB), median (IQR) | −11.9 (−17.0, −5.36) | |
| Use of antithrombotic drugs, n (%) | ||
| yes | 4 (11) | |
| no | 32 (89) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sotani, N.; Kusuhara, S.; Matsumiya, W.; Okuda, M.; Mori, S.; Sotani, R.; Kim, K.W.; Nishisho, R.; Nakamura, M. Outcomes of Microhook ab Interno Trabeculotomy in Consecutive 36 Eyes with Uveitic Glaucoma. J. Clin. Med. 2022, 11, 3768. https://doi.org/10.3390/jcm11133768
Sotani N, Kusuhara S, Matsumiya W, Okuda M, Mori S, Sotani R, Kim KW, Nishisho R, Nakamura M. Outcomes of Microhook ab Interno Trabeculotomy in Consecutive 36 Eyes with Uveitic Glaucoma. Journal of Clinical Medicine. 2022; 11(13):3768. https://doi.org/10.3390/jcm11133768
Chicago/Turabian StyleSotani, Noriyuki, Sentaro Kusuhara, Wataru Matsumiya, Mina Okuda, Sotaro Mori, Rei Sotani, Kyung Woo Kim, Ryuto Nishisho, and Makoto Nakamura. 2022. "Outcomes of Microhook ab Interno Trabeculotomy in Consecutive 36 Eyes with Uveitic Glaucoma" Journal of Clinical Medicine 11, no. 13: 3768. https://doi.org/10.3390/jcm11133768
APA StyleSotani, N., Kusuhara, S., Matsumiya, W., Okuda, M., Mori, S., Sotani, R., Kim, K. W., Nishisho, R., & Nakamura, M. (2022). Outcomes of Microhook ab Interno Trabeculotomy in Consecutive 36 Eyes with Uveitic Glaucoma. Journal of Clinical Medicine, 11(13), 3768. https://doi.org/10.3390/jcm11133768






