Photo-Dependent Reflex Seizures—A Scoping Review with Proposal of Classification
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Methodological Quality
2.3. Eligibility Criteria
- P (patients)—pediatric participants with photo-dependent reflex seizures;
- I (intervention)—all types of stimulation: self-, pattern-, TV-, video-game induced and fixation-off, scotosensitive induced;
- C (comparison)—studies comparing different stimulants;
- O (outcomes/results)—effect of stimulation, i.e., detection of reflex seizures and/or epileptiform discharges in EEG;
- S (study design)—full-text original research, regardless of the study type.
2.4. Data Collection Process
2.5. Summary Measures
3. Results
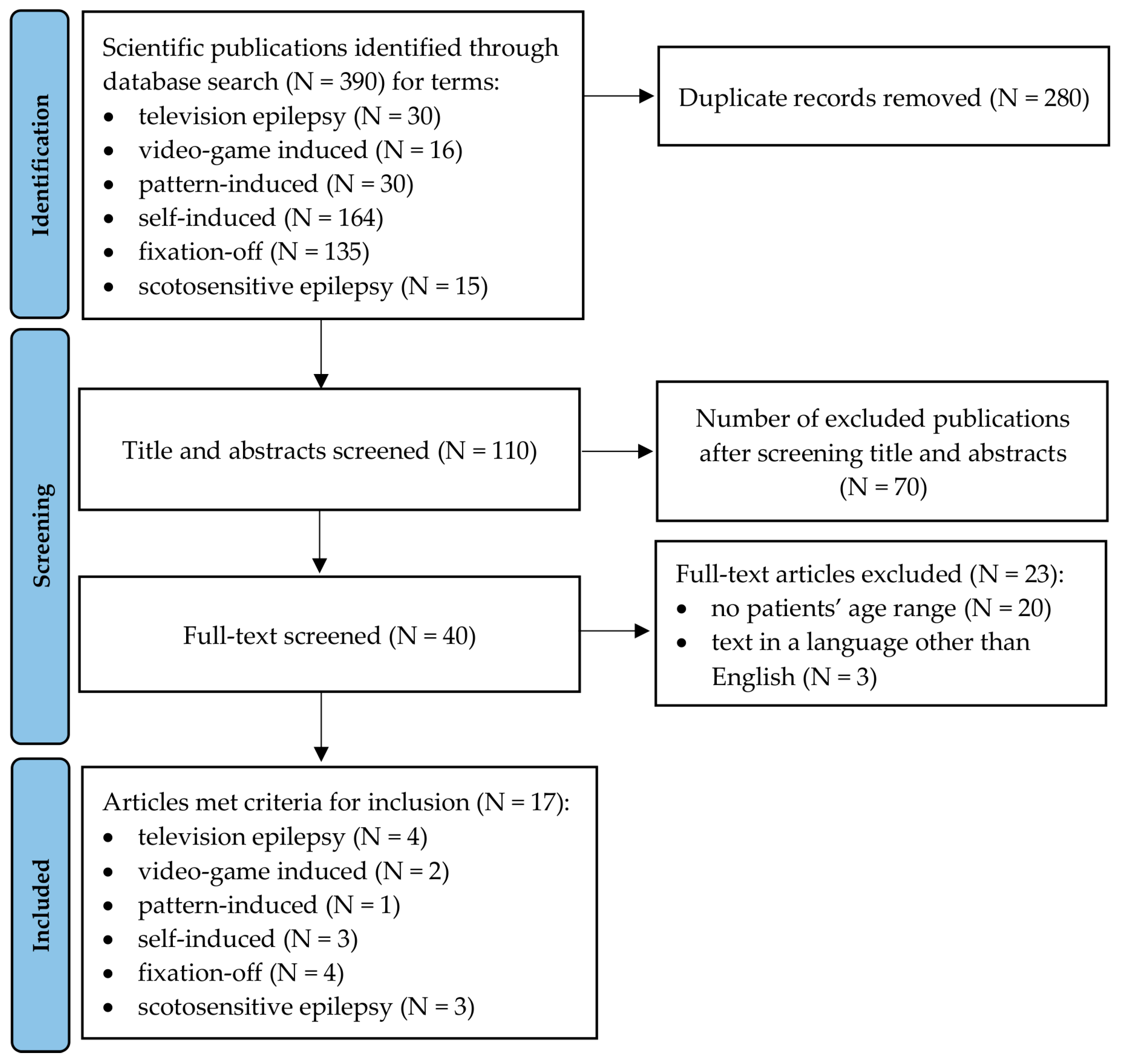
3.1. Study Selection and Available Literature
3.2. Study Characteristics
3.3. Qualitative and Quantitative Synthesis Findings
3.4. Overall Assessment of Patients and Kinds of Stimulation
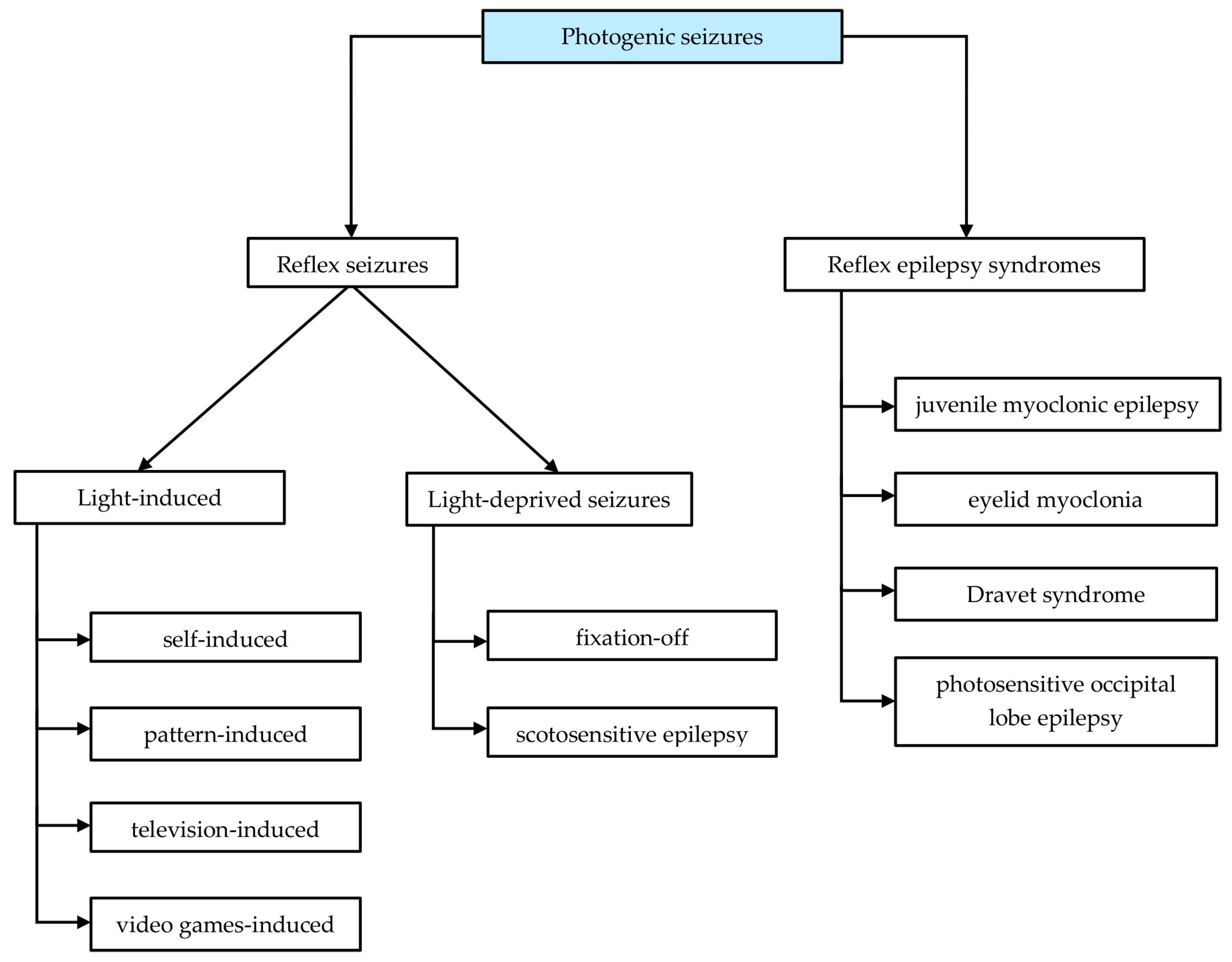
3.5. Proposal of Photodependent Seizures Classification
- -
- Reflex epilepsy syndromes
- -
- Photo-dependent reflex seizures (PDRS)
4. Discussion
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harding, G. The reflex epilepsies with emphasis on photosensitive epilepsy. Suppl. Clin. Neurophysiol. 2004, 57, 433–438. [Google Scholar]
- Gowers, W.R. Epilepsy and Other Chronic Convulsive Diseases: Their Causes, Symptoms and Treatment; William Wood & Company: New York, NY, USA, 1885. [Google Scholar]
- Newton, R.W. The Epilepsies: Seizures, Syndromes and Management. J. R. Soc. Med. 2006, 99, 42–43. [Google Scholar] [CrossRef] [Green Version]
- Kasteleijn-Nolst Trenite, D.G.A. Photosensitivity in epilepsy. Electrophysiological and clinical correlates. Acta. Neurol. Scand. Suppl. 1989, 125, 3–149. [Google Scholar] [PubMed]
- Kasteleijn-Nolst Trenité, D.G.A.; Martins da Silva, A.; Ricci, S.; Rubboli, G.; Tassinari, C.A.; Lopes, J.; Bettencourt, M.; Oosting, J.; Segers, J.P. Video games are exciting: A European study of video game-induced seizures and epilepsy. Epileptic. Disord. 2002, 4, 121–128. [Google Scholar] [PubMed]
- Fisher, R.S.; Acevedo, C.; Arzimanoglou, A.; Bogacz, A.; Cross, J.H.; Elger, C.E.; Engel, J.; Forsgren, L.; French, J.A.; Glynn, M.; et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia 2014, 55, 475–482. [Google Scholar] [CrossRef] [Green Version]
- McHugh, J.C.; Delanty, N. Chapter 2 Epidemiology and Classification of Epilepsy. Gender Comparisons. Int. Rev. Neurobiol. 2008, 83, 11–26. [Google Scholar]
- Strzelecka, J.; Skadorwa, T. The symptoms and management of the photosensitivity in children and adolescents with tension headaches—The symptoms and prevention. A single center experience. Pediatr. Pol. 2016, 91, 240–245. [Google Scholar] [CrossRef]
- Bai, J.; Zhang, W.J.; Ruan, Z.F.; Chen, B.B.; Zhao, G.; Wang, D.; Dang, J.X.; Liu, Y.H. Photosensitive epilepsy and photosensitivity of patients with possible epilepsy in Chinese Han race: A prospective multicenter study. J. Clin. Neurosci. 2019, 69, 15–20. [Google Scholar] [CrossRef] [Green Version]
- Quirk, J.A.; Fish, D.R.; Smith, S.J.M.; Sander, J.W.A.S.; Shorvon, S.D.; Allen, P.J. First seizures associated with playing electronic screen games: A community-based study in Great Britain. Ann. Neurol. 1995, 37, 733–737. [Google Scholar] [CrossRef]
- Poleon, S.; Szaflarski, J.P. Photosensitivity in generalized epilepsies. Epilepsy Behav. 2017, 68, 225–233. [Google Scholar] [CrossRef]
- Fisher, R.S.; Harding, G.; Erba, G.; Barkley, G.L.; Wilkins, A. Photic- and pattern-induced seizures: A review for the epilepsy foundation of america working group. Epilepsia 2005, 46, 1426–1441. [Google Scholar] [CrossRef] [PubMed]
- Verrotti, A.; Trotta, D.; Salladini, C.; di Corcia, G.; Latini, G.; Cutarella, R.; Chiarelli, F. Photosensitivity and epilepsy: A follow-up study. Dev. Med. Child. Neurol. 2004, 46, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Martins da Silva, A.; Leal, B. Photosensitivity and epilepsy: Current concepts and perspectives—A narrative review. Seizure 2017, 50, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Giri, M.; Xia, Z.; Subedi, Y.N.; Li, Y. Genetic and epigenetic mechanisms of epilepsy: A review. Neuropsychiatr. Dis. Treat. 2017, 13, 1841–1859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Italiano, D.; Striano, P.; Russo, E.; Leo, A.; Spina, E.; Zara, F.; Striano, S.; Gambardella, A.; Labate, A.; Gasparini, S.; et al. Genetics of reflex seizures and epilepsies in humans and animals. Epilepsy Res. 2016, 121, 47–54. [Google Scholar] [CrossRef]
- Dos Santos, B.P.; Marinho, C.R.M.; Marques, T.E.B.S.; Angelo, L.K.G.; Malta, M.V.D.S.; Duzzioni, M.; De Castro, O.W.; Leite, J.P.; Barbosa, F.T.; Gitaí, D.L.G. Genetic susceptibility in Juvenile Myoclonic Epilepsy: Systematic review of genetic association studies. PLoS ONE 2017, 12, e0179629. [Google Scholar] [CrossRef] [Green Version]
- Hempelmann, A.; Heils, A.; Sander, T. Confirmatory evidence for an association of the connexin-36 gene with juvenile myoclonic epilepsy. Epilepsy Res. 2006, 71, 223–228. [Google Scholar] [CrossRef]
- Marini, C.; Romoli, M.; Parrini, E.; Costa, C.; Mei, D.; Mari, F.; Parmeggiani, L.; Procopio, E.; Metitieri, T.; Cellini, E.; et al. Clinical features and outcome of 6 new patients carrying de novo KCNB1 gene mutations. Neurol. Genet. 2017, 3, e206. [Google Scholar] [CrossRef] [Green Version]
- Galizia, E.C.; Myers, C.T.; Leu, C.; De Kovel, C.G.F.; Afrikanova, T.; Cordero-Maldonado, M.L.; Martins, T.G.; Jacmin, M.; Drury, S.; Chinthapalli, V.K.; et al. CHD2 variants are a risk factor for photosensitivity in epilepsy. Brain 2015, 138, 1198–1207. [Google Scholar] [CrossRef] [Green Version]
- Hauser, W.A.; Annegers, J.F.; Kurland, L.T. Prevalence of Epilepsy in Rochester, Minnesota: 1940–1980. Epilepsia 1991, 32, 429–445. [Google Scholar] [CrossRef]
- Wolf, P. Basic principles of the ILAE syndrome classification. Epilepsy Res. 2006, 70, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Panayiotopoulos, C.P. The new ILAE report on terminology and concepts for organization of epileptic seizures: A clinician’s critical view and contribution. Epilepsia 2011, 52, 2155–2160. [Google Scholar] [CrossRef] [PubMed]
- Okudan, Z.V.; Özkara, Ç. Reflex epilepsy: Triggers and management strategies. Neuropsychiatr. Dis. Treat. 2018, 14, 327–337. [Google Scholar] [CrossRef] [Green Version]
- Kasteleijn-Nolst Trenité, D.G.; Guerrini, R.; Binnie, C.D.; Genton, P. Visual sensitivity and epilepsy: A proposed terminology and classification for clinical and EEG phenomenology. Epilepsia 2001, 42, 692–701. [Google Scholar] [CrossRef]
- Scheffer, I.E.; Berkovic, S.; Capovilla, G.; Connolly, M.B.; French, J.; Guilhoto, L.; Hirsch, E.; Jain, S.; Mathern, G.W.; Moshé, S.L.; et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017, 58, 512–521. [Google Scholar] [CrossRef] [Green Version]
- Aaberg, K.M.; Surén, P.; Søraas, C.L.; Bakken, I.J.; Lossius, M.I.; Stoltenberg, C.; Chin, R. Seizures, syndromes, and etiologies in childhood epilepsy: The International League Against Epilepsy 1981, 1989, and 2017 classifications used in a population-based cohort. Epilepsia 2017, 58, 1880–1891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riney, K.; Bogacz, A.; Somerville, E.; Hirsch, E.; Nabbout, R.; Scheffer, I.E.; Zuberi, S.M.; Alsaadi, T.; Jain, S.; French, J.; et al. International League Against Epilepsy classification and definition of epilepsy syndromes with onset at a variable age: Position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia 2022, 63, 1443–1474. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Wilkins, A.J.; Darby, C.E.; Binnie, C.D.; Stefansson, S.B.; Jeavons, P.M.; Harding, G.F.A. Television epilepsy—The role of pattern. Electroencephalogr. Clin. Neurophysiol. 1979, 47, 163–171. [Google Scholar] [CrossRef]
- Takahashi, T.; Tsukahara, Y. Pocket Monster incident and low luminance visual stimuli: Special reference to deep red flicker stimulation. Pediatr. Int. 1998, 40, 631–637. [Google Scholar] [CrossRef]
- Etemadifar, M.; Raoufi, M.; Maghzi, A.-H.; Ebrahimi, A.; Kaji-Esfahani, M.; Mousavi, S.-A. Television-Provoked Epilepsy in Children: A Follow-Up Survey from Isfahan, Iran. Arch. Iran. Med. 2008, 11, 649–653. [Google Scholar] [PubMed]
- Brinciotti, M.; Matricardi, M. Paroxysmal eyelid movements in patients with visual-sensitive reflex seizures. Epileptic Disord. 2015, 17, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Piccioli, M.; Vigevano, F.; Buttinelli, C.; Kasteleijn-Nolst Trenité, D.G.A. Do video games evoke specific types of epileptic seizures? Epilepsy Behav. 2005, 7, 524–530. [Google Scholar] [CrossRef]
- Radhakrishnan, K.; St. Louis, E.K.; Johnson, J.A.; McClelland, R.L.; Westmoreland, B.F.; Klass, D.W. Pattern-sensitive epilepsy: Electroclinical characteristics, natural history, and delineation of the epileptic syndrome. Epilepsia 2005, 46, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Baumer, F.M.; Porter, B.E. Clinical and electrographic features of sunflower syndrome. Epilepsy Res. 2018, 142, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Barnett, J.R.; Fleming, B.M.; Geenen, K.R.; Sourbron, J.; Freedman, J.H.; Bruno, P.L.; Thiele, E.A. Characterizing Sunflower syndrome: A clinical series. Epileptic Disord. 2020, 22, 273–280. [Google Scholar] [CrossRef]
- Boel, M.; Casaer, P. Add-on therapy of fenfluramine in intractable self-induced epilepsy. Neuropediatrics 1996, 27, 171–173. [Google Scholar] [CrossRef]
- Koutroumanidis, M.; Tsatsou, K.; Sanders, S.; Michael, M.; Tan, S.V.; Agathonikou, A.; Panayiotopoulos, C.P. Fixation-off sensitivity in epilepsies other than the idiopathic epilepsies of childhood with occipital paroxysms: A 12-year clinical-video EEG study. Epileptic Disord. 2009, 11, 20–36. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Zhang, Y.; Zhang, W.; Shen, C.; Jin, L.; Chen, B.; Jiang, Z.; Tao, J.X.; Liu, Y. The electroclinical features of idiopathic generalized epilepsy patients presenting with fixation-off sensitivity. Epileptic Disord. 2018, 20, 479–489. [Google Scholar] [CrossRef]
- Karkare, K.D.; Menon, R.N.; Radhakrishnan, A.; Cherian, A.; Thomas, S.V. Electroclinical characteristics and syndromic associations of “eye-condition” related visual sensitive epilepsies-A cross-sectional study. Seizure 2018, 58, 62–71. [Google Scholar] [CrossRef] [Green Version]
- Dede, H.Ö.; Bebek, N.; Emekli, S.; Baykan, B.; Yapıcı, Z.; Gökyiğit, A. The clinical significance and electrophysiologic findings of fixation-off and closure of the eyes sensitivity: Data from a prospective unselected population. Epilepsy Res. 2021, 170, 106541. [Google Scholar] [CrossRef] [PubMed]
- Suresh-babu, S. The Spectrum of Epilepsies with Fixation off Sensitivity: A Case Report and Review of Literature. J. Neurol. Neurosci. 2017, 8, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Agathonikou, A.; Koutroumanidis, M.; Panayiotopoulos, C.P. Fixation-off (scoto) sensitivity combined with photosensitivity. Epilepsia 1998, 39, 552–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lugaresi, E.; Cirignotta, F.; Montagna, P. Occipital Lobe Epilepsy with Scotosensitive Seizures: The Role of Central Vision. Epilepsia 1984, 25, 115–120. [Google Scholar] [CrossRef]
- Kasteleijn-Nolst Trenite, D.; Genton, P.; Brandt, C.; Reed, R.C. The ‘Photosensitivity Model’ is (also) a model for focal (partial) seizures. Epilepsy Res. 2017, 133, 113–120. [Google Scholar] [CrossRef]
- Hennessy, M.J.; Binnie, C.D. Photogenic partial seizures. Epilepsia 2000, 41, 59–64. [Google Scholar] [CrossRef]
- Lu, Y.; Waltz, S.; Stenzel, K.; Muhle, H.; Stephani, U. Photosensitivity in epileptic syndromes of childhood and adolescence. Epileptic Disord. 2008, 10, 136–143. [Google Scholar]
- Radovici, M.M.A.; Misirliou, V.L.; Gluckman, M. Epilepsy reflex provoquee par excitations optiques des rayons solaires. Rev. Neurol. 1932, 1, 1305–1307, [Translated by Koutroumanidis, M. Reflex epilepsy provoked by optic excitation by (means of) sunrays]. In: Duncan, J.S., Panayiotopoulo, C.P. (eds.), Eyelid myoclonia with absences. John Libbey, London 1996, 103–105. [Google Scholar]
- Kasteleijn-Nolst Trenité, D.G.A. Provoked and reflex seizures: Surprising or common? Epilepsia 2012, 53, 105–113. [Google Scholar] [CrossRef]
- Geenen, K.R.; Patel, S.; Thiele, E.A. Sunflower syndrome: A poorly understood photosensitive epilepsy. Dev. Med. Child. Neurol. 2021, 63, 259–262. [Google Scholar] [CrossRef]
- Jeavons, P.M.; Harding Graham, F.A. Photosensitive Epilepsy (Clinics in Developmental Medicine); Mac Keith Press: London, UK, 1995. [Google Scholar]
- Kasteleijn-Nolst Trenite, D. Photosensitivity and Epilepsy. In Clinical Electroencephalography; Mecarelli, O., Ed.; Springer: Cham, Switzerland, 2019; pp. 487–495. [Google Scholar]
- Panayiotopoulos, C.P. Fixation-off, scotosensitive, and other visual-related epilepsies. Adv. Neurol. 1998, 75, 139–157. [Google Scholar] [PubMed]
| Author, Year | Patients | Intervention | Comparison | Outcome | Study Design |
| Light-induced seizures | |||||
| Television-induced | |||||
| Wilkins A. et al. (1979) [30] | N = 21: F:M = 4:3; age 6–31 years | TV induced - patterned and diffuse IPS, - monochrome and colour television, - static and moving patterns of stripes | Lack of comparisons | From 21 patients: - 16 patients were sensitive to diffused IPS, - 19 patients were sensitive to patterned IPS, - 16 patients were sensitive to the monochrome set, - 13 were sensitive to the colour TV | prospective study non-randomized |
| N = 8: M = 6, F = 2; age 11–42 years | TV induced - small TV screen, - large TV screen, - large TV screen covered by a mask containing a central aperture the same size as the small screen | - large screen—distance 3 m - small and masked screen—distance 1.5 m | Proportion of PhS patients affected by television increases as the viewing distance is reduced; small screen television was less epileptogenic than a large screen television viewed at the same distance | prospective study non-randomized | |
| Takahashi T. et al. (1998) [31] | N = nearly 700 people, mostly children | TV induced - Pokemon Monsters program - visual stimulation of low luminance - deep red flicker and flickering geometric pattern stimuli with 10–20 cdm2 luminosity - ordinary high luminance stroboscopic IPS | Lack of comparisons | Healthy youngsters may have latent PhS and sensitivity might be disclosed by use of low luminance deep red flicker stimulation. Deep red flicker stimulation is more provocative of PPR than ordinary high luminance stroboscopic IPS | prospective study non-randomized |
| Etemadifar M. et al. (2008) [32] | N = 1705; N = 30 TV epilepsy: M = 13, F = 17; age < 12 years | TV induced - seizures triggered by watching TV, - abnormal EEG findings, - patients had PPR to IPS | Lack of comparisons | 57% pure TV epilepsy: patients had: absence (3.3%), myoclonic (3.3%), GTCS (93,3%) seizures in response to IPS; 43% TV epilepsy and other types generalized seizure | retrospective study non-randomized |
| Brinciotti M. et al. (2015) [33] | N = 26: M = 12, F = 14; mean age 14 years | TV induced Video-EEG recordings: - at rest - during IPS, - during pattern stimulation (PS), - during TV watching Blink rate was evaluated: - at rest, - during a TV-viewing period, - during the occurrence of PEM | Lack of comparisons | EM were recorded in all patients. The frequency of EM ranged from 8 to 12.5 Hz (average: 9.6 ± 1.5). Visually-induced seizures were recorded in 20 patients, triggered by stimuli (IPS and PS) in 11 patients; seizures were triggered by PS (but not IPS)—5 patients, IPS (but not PS)—3 patients, TV watching (but not PS or IPS)—1 patient | prospective study non-randomized |
| Video-game induced (VG induced) | |||||
| Piccioli M. et al. (2005) [34] | N = 29: M = 12, F = 17; mean age 14.7 years there were selected those with generalized epileptiform discharges of at least 0.5-s duration during VG provocation: 8 M, 7 F; | VG induced Children were visually stimulated with IPS and black-and-white striped patterns before they started playing the VG (Super Mario World, Super Mario, Mario Kart, Street Fighter II, Super Bomberman II, The Magical Quest, Super Mario All Stars, Super Aleste) | Comparison symptoms evoked by VG and IPS | All patients showed generalized epileptiform activity either spontaneously or evoked by IPS and by playing VG (all). The majority reacted to 4–5 of the 12 VG tested, while Super Mario World was provocative in all patients. | retrospective study non-randomized |
| Kasteleijn-Nolst Trenite D.G.A. et al. (2002) [5] | N = 352: M = 41% F = 59%; age 13–18 years | VG induced Different types of video games | Lack of comparisons | 83% (N = 294) had a history of epileptic seizures, visually-induced seizures were in 77% (N = 225) of those with a seizure history. VG Super Mario World was the most provocative | prospective study non-randomized |
| Pattern-induced | |||||
| Radhakrishnan K. et al. (2005) [35] | N = 73; M = 30, F = 43; median age 12.8 years | Pattern-induced Different patterns: window screens, garments, tablecloths, and ceiling tiles | Lack of comparisons | Patients exhibited absence, myoclonic, partial seizures, GTCS in various combinations | retrospective study non-randomized |
| Self-induced | |||||
| Baumer F.M. et al. (2018) [36] | N = 13: F = 77%, M = 23%; age 2–8 years | Self-induced—Sunflower Syndrome The background in EEG was normal. 10 patients had generalized 3–4 Hz spike wave discharges, with a bifrontal predominance; 9 of the 10 had multiple runs lasting longer than 3 s. 8 patients had polyspikes or frontal fast activity | Lack of comparisons | 5 patients had EM 6 patients—EM and absence 2 patients—absence seizures | retrospective study non-randomized |
| Barnett J.R. et al. (2020) [37] | N = 24: F = 18, M = 6; age 6.4–25 years | Self-induced—Sunflower Syndrome | Lack of comparisons | Sunflower syndrome—generalized, pharmacoresistant epilepsy with childhood onset Absence seizures | retrospective study non-randomized |
| Boel M. et al. (1996) [38] | N = 11: F = 7, M = 4; mean age 8 years | Self-induced Intellectual disability in all patients. | Lack of comparisons | All patients had GTCS, 5 patients had absence seizures | study reports |
| Light-deprivated seizures | |||||
| Fixation-off (FOS) | |||||
| Koutroumanidis M. et al. (2009) [39] | N = 14: F = 10, F = 4, age 9–48 years | FOS EEG database were analyzed to find all patients with video-EEG-documented FOS | Lack of comparisons | FOS can occur in non-PhS and PhS patients; FOS can be in mild and medically intractable epilepsies, and in patients without obvious epileptic seizures. All had epileptiform activity—focal, generalized or both. An approximate incidence of 0.2% | retrospective study non-randomized |
| Wang X. et al. (2018) [40] | N = 8: F = 3, M = 5; age 8–14 years | FOS | Lack of comparisons | PhS was in 6 patients. PPR was elicited during IPS at frequencies 10–20 Hz Patients had seizures: 4—EM, 2—JME, 1—PhS epilepsy, 1-GTCS | retrospective study non-randomized |
| Karkare K.D. et al. (2018) [41] | N = 52: F = 25, M = 27; mean age 10.3 years | FOS Open eyes/close eyes | Lack of comparisons | Seizure consisted of visual auras (subjective symptoms), tonic and versive seizures, autonomic seizures, EM, with or without absences, limb myoclonus and GTCS | cross-sectional study |
| Dede H.O. et al. (2021) [42] | N = 200: F = 106, M = 94; age 4–80 years | FOS Open eyes/close eyes All the patients encountered with FOS were children in this study | Lack of comparisons | 20 of the analyzed EEG recordings revealed generalized epileptiform discharges. 51 recordings indicated focal epileptiform abnormalities, 42 were abnormal background activity, 87 were normal EEG. Seizures: temporal, frontal, occipital, centroparietal, temporo-parieto-occipital | prospective study non-randomized |
| Scotosensitive epilepsy | |||||
| Suresh-babu S. (2017) [43] | N = 1: F; 11 years | Scotosensitive epilepsy Open eyes/close eyes | Lack of comparisons | Patient had absence seizures, EM, and rarely GTCS occipital epileptiform discharges which appeared only during eye closure | case report |
| Agathonikou A. et al. (1998) [44] | N = 1: M; 16 years | Scotosensitive epilepsy Open eyes/close eyes Central vision and fixation were eliminated with vision through +10 spherical lenses or underwater goggles covered with semitransparent tape | Lack of comparisons | IPS elicits generalized discharges of multiple spike and slow waves even when the eyes are open, and the ictal clinical manifestations enhance when IPS is combined with eye-closure, absence and myoclonic jerks | case report |
| Lugaresi E. et al. (1984) [45] | N = 4: F = 1, M = 3; age 12–14 years | Scotosensitive epilepsy Open eyes/close eyes seizures induced by eye closure and darkness | Lack of comparisons | Spike-and-wave discharges evoked by eye closure and by darkness, and blocked by eye opening | cases report |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strzelecka, J.; Mazurkiewicz, D.W.; Skadorwa, T.; Gąsior, J.S.; Jóźwiak, S. Photo-Dependent Reflex Seizures—A Scoping Review with Proposal of Classification. J. Clin. Med. 2022, 11, 3766. https://doi.org/10.3390/jcm11133766
Strzelecka J, Mazurkiewicz DW, Skadorwa T, Gąsior JS, Jóźwiak S. Photo-Dependent Reflex Seizures—A Scoping Review with Proposal of Classification. Journal of Clinical Medicine. 2022; 11(13):3766. https://doi.org/10.3390/jcm11133766
Chicago/Turabian StyleStrzelecka, Jolanta, Dariusz Wojciech Mazurkiewicz, Tymon Skadorwa, Jakub S. Gąsior, and Sergiusz Jóźwiak. 2022. "Photo-Dependent Reflex Seizures—A Scoping Review with Proposal of Classification" Journal of Clinical Medicine 11, no. 13: 3766. https://doi.org/10.3390/jcm11133766
APA StyleStrzelecka, J., Mazurkiewicz, D. W., Skadorwa, T., Gąsior, J. S., & Jóźwiak, S. (2022). Photo-Dependent Reflex Seizures—A Scoping Review with Proposal of Classification. Journal of Clinical Medicine, 11(13), 3766. https://doi.org/10.3390/jcm11133766








