Stool Elastase as an Independent Prognostic Factor in Patients with Pancreatic Head Cancer
Abstract
1. Introduction
2. Materials and Methods
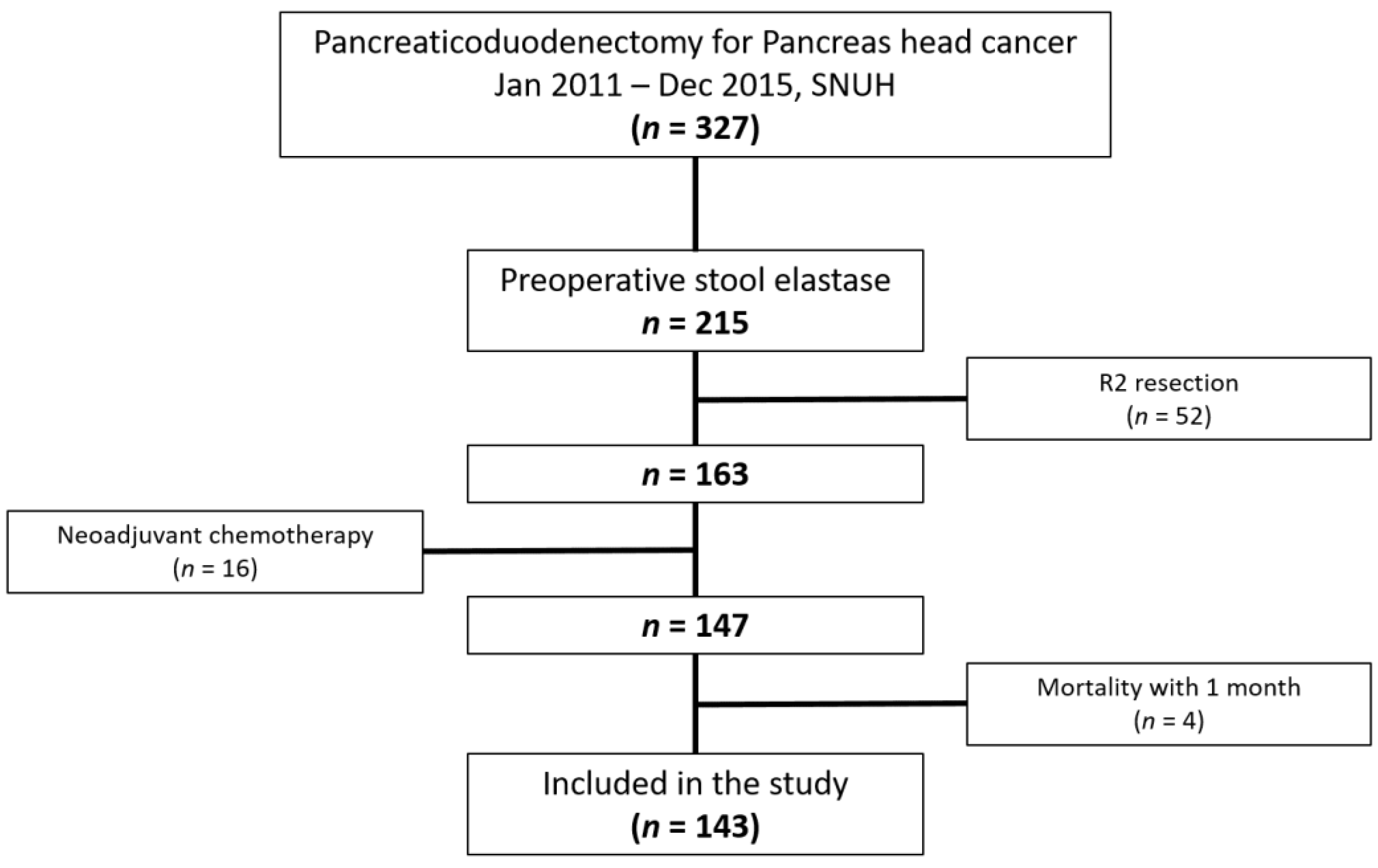
2.1. Patient Selection and Data Collection
2.2. Stool Elastase Level Measurement
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
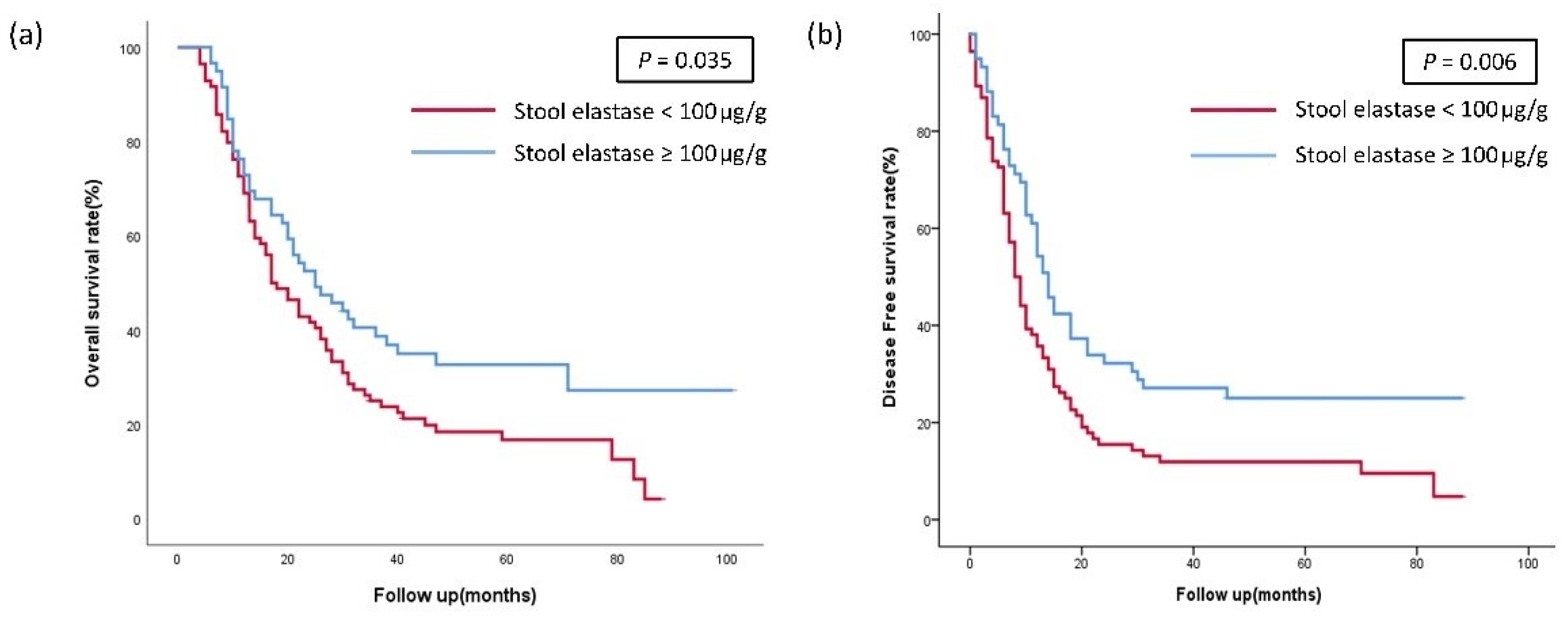
3.2. Survival Analysis According to the Stool Elastase Group
3.3. Prognostic Factors for Survival
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ilic, M.; Ilic, I. Epidemiology of pancreatic cancer. World J. Gastroenterol. 2016, 22, 9694–9705. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Yagi, S.; Kinoshita, H.; Sakamoto, Y.; Okada, K.; Uryuhara, K.; Morimoto, T.; Kaihara, S.; Hosotani, R. Long-term survival after resection of pancreatic cancer: A single-center retrospective analysis. World J. Gastroenterol. 2015, 21, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Kanda, M.; Fujii, T.; Kodera, Y.; Nagai, S.; Takeda, S.; Nakao, A. Nutritional predictors of postoperative outcome in pancreatic cancer. Br. J. Surg. 2011, 98, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Partelli, S.; Frulloni, L.; Minniti, C.; Bassi, C.; Barugola, G.; D’Onofrio, M.; Crippa, S.; Falconi, M. Faecal elastase-1 is an independent predictor of survival in advanced pancreatic cancer. Dig. Liver Dis. 2012, 44, 945–951. [Google Scholar] [CrossRef]
- Tran, T.C.K.; van‘t Hof, G.; Kazemier, G.; Hop, W.C.; Pek, C.; Van Toorenenbergen, A.W.; van Dekken, H.; Van Eijck, C.H.J. Pancreatic Fibrosis Correlates with Exocrine Pancreatic Insufficiency after Pancreatoduodenectomy. Dig. Surg. 2008, 25, 311–318. [Google Scholar] [CrossRef]
- Keller, J.; Layer, P. Diagnosis of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreapedia 2015. [Google Scholar] [CrossRef]
- Richter, E.; Denecke, A.; Klapdor, S.; Klapdor, R. Parenteral nutrition support for patients with pancreatic cancer—Improvement of the nutritional status and the therapeuric outcome. Anticancer Res. 2012, 32, 2111–2118. [Google Scholar]
- Sikkens, E.C.; Cahen, D.L.; de Wit, J.; Looman, C.W.; van Eijck, C.; Bruno, M.J. A prospective assessment of the natural course of the exocrine pancreatic function in patients with a pancreatic head tumor. J. Clin. Gastroenterol. 2014, 48, e43–e46. [Google Scholar] [CrossRef]
- Matsumoto, J.; Traverso, L.W. Exocrine function following the whipple operation as assessed by stool elastase. J. Gastrointest. Surg. 2006, 10, 1225–1229. [Google Scholar] [CrossRef]
- Vujasinovic, M.; Valente, R.; Del Chiaro, M.; Permert, J.; Lohr, J.M. Pancreatic Exocrine Insufficiency in Pancreatic Cancer. Nutrients 2017, 9, 183. [Google Scholar] [CrossRef]
- Luth, S.; Teyssen, S.; Forssmann, K.; Kolbel, C.; Krummenauer, F.; Singer, M.V. Fecal elastase-1 determination: ‘gold standard’ of indirect pancreatic function tests? Scand. J. Gastroenterol. 2001, 36, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Lindkvist, B. Diagnosis and treatment of pancreatic exocrine insufficiency. World J. Gastroenterol. 2013, 19, 7258–7266. [Google Scholar] [CrossRef] [PubMed]
- Struyvenberg, M.R.; Martin, C.R.; Freedman, S.D. Practical guide to exocrine pancreatic insufficiency—Breaking the myths. BMC Med. 2017, 15, 29. [Google Scholar] [CrossRef]
- Löser, C.; Möllgaard, A.; Fölsch, U.R. Faecal elastase 1: A novel, highly sensitive, and specific tubeless pancreatic function test. Gut 1996, 39, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Nandhakumar, N.; Green, M.R. Interpretations: How to use faecal elastase testing. Arch. Dis. Child. Educ. Pract. Ed. 2010, 95, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Kang, J.S.; Han, Y.; Kim, H.; Kwon, W.; Kim, J.R.; Kim, S.W.; Jang, J.Y. Influence of preoperative nutritional status on clinical outcomes after pancreatoduodenectomy. HPB 2018, 20, 1051–1061. [Google Scholar] [CrossRef]
- Park, J.W.; Jang, J.Y.; Kim, E.J.; Kang, M.J.; Kwon, W.; Chang, Y.R.; Han, I.W.; Kim, S.W. Effects of pancreatectomy on nutritional state, pancreatic function and quality of life. Br. J. Surg. 2013, 100, 1064–1070. [Google Scholar] [CrossRef]
- Lankisch, P.G. Exocrine pancreatic function tests. Gut 1982, 23, 777–798. [Google Scholar] [CrossRef]
- Erchinger, F.; Engjom, T.; Tjora, E.; Hoem, D.; Hausken, T.; Gilja, O.H.; Dimcevski, G. Quantification of pancreatic function using a clinically feasible short endoscopic secretin test. Pancreas 2013, 42, 1101–1106. [Google Scholar] [CrossRef]
- Fine, K.D.; Ogunji, F. A new method of quantitative fecal fat microscopy and its correlation with chemically measured fecal fat output. Am. J. Clin. Pathol. 2000, 113, 528–534. [Google Scholar] [CrossRef]
- Domínguez-Muñoz, J.E.; Hieronymus, C.; Sauerbruch, T.; Malfertheiner, P. Fecal elastase test: Evaluation of a new noninvasive pancreatic function test. Am. J. Gastroenterol. 1995, 90, 1834–1837. [Google Scholar] [PubMed]
- Lim, J.H.; Park, J.S.; Yoon, D.S. Preoperative fecal elastase-1 is a useful prognostic marker following curative resection of pancreatic cancer. HPB 2017, 19, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Erickson, J.A.; Aldeen, W.E.; Grenache, D.G.; Ashwood, E.R. Evaluation of a fecal pancreatic elastase-1 enzyme-linked immunosorbent assay: Assessment versus an established assay and implication in classifying pancreatic function. Clin. Chim. Acta 2008, 397, 87–91. [Google Scholar] [CrossRef]
- Stocken, D.D.; Hassan, A.B.; Altman, D.G.; Billingham, L.J.; Bramhall, S.R.; Johnson, P.J.; Freemantle, N. Modelling prognostic factors in advanced pancreatic cancer. Br. J. Cancer 2008, 99, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Pawlik, T.M.; Gleisner, A.L.; Cameron, J.L.; Winter, J.M.; Assumpcao, L.; Lillemoe, K.D.; Wolfgang, C.; Hruban, R.H.; Schulick, R.D.; Yeo, C.J.; et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 2007, 141, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Braga, M.; Ljungqvist, O.; Soeters, P.; Fearon, K.; Weimann, A.; Bozzetti, F. ESPEN guidelines on parenteral nutrition: Surgery. Clin. Nutr. 2009, 28, 378–386. [Google Scholar] [CrossRef]
- Dintinjana, R.D.; Redzović, A.; Cubranić, A.; Dintinjana, M.; Vanis, N. Nutrition in cancer patients. Coll. Antropol. 2014, 38, 1271–1275. [Google Scholar]
- Mitchell, T.; Clarke, L.; Goldberg, A.; Bishop, K.S. Pancreatic cancer cachexia: The role of nutritional interventions. Healthcare 2019, 7, 89. [Google Scholar] [CrossRef]
- Choe, Y.M.; Lee, K.Y.; Oh, C.A.; Lee, J.B.; Choi, S.K.; Hur, Y.S.; Kim, S.J.; Cho, Y.U.; Ahn, S.I.; Hong, K.C.; et al. Risk factors affecting pancreatic fistulas after pancreaticoduodenectomy. World J. Gastroenterol. 2008, 14, 6970–6974. [Google Scholar] [CrossRef]
| Variables | Total (n = 143) | Low SE Group <100 µg/g (n = 84) | High SE Group ≥100 µg/g (n = 59) | p-Value |
|---|---|---|---|---|
| Sex (Male/Female) (%) | 87 (60.8)/56 (39.2) | 53 (63.1)/31 (36.9) | 34 (57.6)/25 (42.4) | 0.602 |
| Age (mean ± SD, years) | 64.5 ± 9.4 | 63.8 ± 9.1 | 65.5 ± 9.9 | 0.345 |
| BMI (mean ± SD, kg/m2) | 22.6 ± 2.8 | 22.6 ± 2.6 | 22.6 ± 3.1 | 0.461 |
| ASA class (%) | 0.708 | |||
| I II III | 30 (21.0) 01 (70.6) 12 (8.4) | 16 (19.0) 60 (71.4) 8 (9.5) | 14 (23.7) 41 (69.5) 4 (6.8) | |
| DM, Yes (%) | 58 (40.6) | 37 (44.0) | 21 (35.6) | 0.387 |
| Smoking, Yes (%) | 24 (16.8) | 15 (17.9) | 9 (15.3) | 0.821 |
| Pre-op CA19-9, U/mL (mean ± SD) | 901 ± 2669 | 913 ± 2397 | 884 ± 3037 | 0.501 |
| Pre-op transferrin, mg/dL (mean ± SD) | 234 ± 43 | 232 ± 41 | 236 ± 46 | 0.438 |
| Pre-op prealbumin, mg/dL (mean ± SD) | 23.8 ± 7.3 | 23.1 ± 7.3 | 24.8 ± 7.4 | 0.681 |
| Pre-op protein, g/dL (mean ± SD) | 6.9 ± 0.6 | 6.9 ± 0.6 | 6.9 ± 0.5 | 0.415 |
| Pre-op albumin, g/dL (mean ± SD) | 3.9 ± 0.4 | 3.9 ± 0.4 | 3.9 ± 0.4 | 0.406 |
| Postoperative hospital day (mean ± SD, day) | 16.0 ± 9.6 | 15.0 ± 7.8 | 17.4 ± 11.6 | 0.449 |
| R0 resection status (%) | 124 (86.7) | 70 (83.3) | 54 (91.5) | 0.212 |
| Complication CD grade ≥ 3 (%) | 22 (15.4) | 9 (10.7) | 13 (22.0) | 0.098 |
| POPF (%) | <0.001 | |||
| No Biochemical leak Grade B | 103 (84.6) 29 (20.3) 11 (7.7) | 72 (85.7) 9 (10.7) 3 (3.6) | 31 (52.5) 20 (33.9) 9 (13.6) | |
| T stage (%) | 0.114 | |||
| 1 2 3 4 | 21 (14.7) 97 (67.8) 22 (15.4) 3 (2.1) | 14 (16.7) 51 (60.7) 16 (19.0) 3 (3.6) | 7 (11.9) 46 (78.0) 6 (10.2) 0 (0.0) | |
| n stage (%) | 0.296 | |||
| Negative Positive | 55 (38.5) 88 (61.5) | 29 (34.5) 55 (65.5) | 26 (44.1) 33 (55.9) | |
| Adjuvant chemotherapy (%) | 121 (84.6) | 69 (82.1) | 52 (88.1) | 0.358 |
| Adjuvant radiotherapy (%) | 81 (56.6) | 47 (56.0) | 34 (57.6) | 0.865 |
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Sex, (male) vs. female | 0.995 | 0.680–1.455 | 0.979 | |||
| Age, years (≤65) vs. >65 | 1.053 | 0.873–1.269 | 0.590 | |||
| BMI, kg/m2 (≤23) vs. >23 | 1.035 | 0.858–1.250 | 0.719 | |||
| ASA class (I) II III | 1.443 0.915 | 1.024–2.034 0.687–1.219 | 0.095 0.036 0.545 | 1.405 0.869 | 0.989–1.996 0.667–1.202 | 0.121 0.058 0.463 |
| Pre-op CA 19–9, U/mL (≤37) vs. >37 | 1.772 | 1.151–2.727 | 0.009 | 1.495 | 0.958–2.332 | 0.076 |
| Stool elastase, µg/g (≥100) vs. <100 | 1.501 | 1.019–2.211 | 0.040 | 1.487 | 1.003–2.206 | 0.048 |
| T stage (T1, T2) vs. (T3, T4) | 1.011 | 0.621–1.645 | 0.965 | |||
| n stage (Negative) vs. Positive | 2.098 | 1.404–3.134 | <0.001 | 1.852 | 1.210–2.835 | 0.005 |
| Adjuvant Chemotherapy (No) vs. Yes | 1.111 | 0.858–1.439 | 0.424 | |||
| Adjuvant Radiotherapy (No) vs. Yes | 1.086 | 0.900–1.311 | 0.389 | |||
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Sex, (male) vs. female | 1.026 | 0.708–1.487 | 0.891 | |||
| Age, years (≤65) vs. >65 | 1.107 | 0.772–1.588 | 0.580 | |||
| BMI, kg/m2 (≤23) vs. >23 | 0.969 | 0.675–1.391 | 0.864 | |||
| ASA class (I) II III | 1.491 0.890 | 0.744–2.991 0.473–1.675 | 0.064 0.260 0.718 | 1.353 0.790 | 0.565–2.790 0.407–1.534 | 0.050 0.413 0.486 |
| Pre-op CA 19-9, U/mL (≤37) vs. >37 | 1.925 | 1.269–2.923 | 0.002 | 1.525 | 0.980–2.373 | 0.061 |
| Stool elastase, µg/g (≥100) vs. <100 | 1.651 | 1.137–2.399 | 0.008 | 1.894 | 1.238–2.895 | 0.003 |
| T stage (T1, T2) vs. (T3, T4) | 1.280 | 0.798–2.054 | 0.305 | |||
| n stage (Negative) vs. Positive | 2.089 | 1.417–3.079 | <0.001 | 1.605 | 1.103–2.337 | 0.014 |
| Adjuvant Chemotherapy (No) vs. Yes | 1.049 | 0.628–1.754 | 0.855 | |||
| Adjuvant Radiotherapy (No) vs. Yes | 1.028 | 0.857–1.233 | 0.767 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, H.; Kim, H.; Sohn, H.J.; Lee, M.; Kim, H.S.; Han, Y.; Kwon, W.; Jang, J.-Y. Stool Elastase as an Independent Prognostic Factor in Patients with Pancreatic Head Cancer. J. Clin. Med. 2022, 11, 3718. https://doi.org/10.3390/jcm11133718
Hwang H, Kim H, Sohn HJ, Lee M, Kim HS, Han Y, Kwon W, Jang J-Y. Stool Elastase as an Independent Prognostic Factor in Patients with Pancreatic Head Cancer. Journal of Clinical Medicine. 2022; 11(13):3718. https://doi.org/10.3390/jcm11133718
Chicago/Turabian StyleHwang, Honam, Hongbeom Kim, Hee Ju Sohn, Mirang Lee, Hyeong Seok Kim, Youngmin Han, Wooil Kwon, and Jin-Young Jang. 2022. "Stool Elastase as an Independent Prognostic Factor in Patients with Pancreatic Head Cancer" Journal of Clinical Medicine 11, no. 13: 3718. https://doi.org/10.3390/jcm11133718
APA StyleHwang, H., Kim, H., Sohn, H. J., Lee, M., Kim, H. S., Han, Y., Kwon, W., & Jang, J.-Y. (2022). Stool Elastase as an Independent Prognostic Factor in Patients with Pancreatic Head Cancer. Journal of Clinical Medicine, 11(13), 3718. https://doi.org/10.3390/jcm11133718






