Prognostic Factors for Mortality in Acute Mesenteric Ischemia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Definitions
2.2. Standard Clinical Management of AMI Patients
2.3. Data Extraction and Quality Management
2.4. Statistical Analysis
3. Results
3.1. Preoperative, Operative and Postoperative Data
3.2. Univariate and Multivariable Analysis of Postoperative Mortality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bala, M.; Kashuk, J.; Moore, E.E.; Kluger, Y.; Biffl, W.; Gomes, C.A.; Ben-Ishay, O.; Rubinstein, C.; Balogh, Z.J.; Civil, I.; et al. Acute mesenteric ischemia: Guidelines of the World Society of Emergency Surgery. World J. Emerg. Surg. 2017, 12, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renner, P.; Kienle, K.; Dahlke, M.H.; Heiss, P.; Pfister, K.; Stroszczynski, C.; Piso, P.; Schlitt, H.J. Intestinal ischemia: Current treatment concepts. Langenbeck’s Arch. Surg. Dtsch. Ges. Fur Chir. 2011, 396, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Dahlke, M.H.; Asshoff, L.; Popp, F.C.; Feuerbach, S.; Lang, S.A.; Renner, P.; Slowik, P.; Stoeltzing, O.; Schlitt, H.J.; Piso, P. Mesenteric ischemia—Outcome after surgical therapy in 83 patients. Dig. Surg. 2008, 25, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Tilsed, J.V.T.; Casamassima, A.; Kurihara, H.; Mariani, D.; Martinez, I.; Pereira, J.; Ponchietti, L.; Shamiyeh, A.; al-Ayoubi, F.; Barco, L.A.B.; et al. ESTES guidelines: Acute mesenteric ischaemia. Eur. J. Trauma Emerg. Surg. 2016, 42, 253–270. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.H.; Chang, Y.C.; Yen, D.H.; Kao, W.F.; Chen, J.D.; Wang, L.M.; Huang, C.I.; Lee, C.H. Clinical factors and outcomes in patients with acute mesenteric ischemia in the emergency department. J. Chin. Med. Assoc. 2005, 68, 299–306. [Google Scholar] [CrossRef] [Green Version]
- Adaba, F.; Askari, A.; Dastur, J.; Patel, A.; Gabe, S.M.; Vaizey, C.J.; Faiz, O.; Nightingale, J.M.D.; Warusavitarne, J. Mortality after acute primary mesenteric infarction: A systematic review and meta-analysis of observational studies. Colorectal Dis. 2015, 17, 566–577. [Google Scholar] [CrossRef]
- Nuzzo, A.; Guedj, K.; Curac, S.; Hercend, C.; Bendavid, C.; Gault, N.; Tran-Dinh, A.; Ronot, M.; Nicoletti, A.; Bouhnik, Y.; et al. Accuracy of citrulline, I-FABP and d-lactate in the diagnosis of acute mesenteric ischemia. Sci. Rep. 2021, 11, 18929. [Google Scholar] [CrossRef]
- Björck, M.; Koelemay, M.; Acosta, S.; Bastos Goncalves, F.; Kölbel, T.; Kolkman, J.J.; Lees, T.; Lefevre, J.H.; Menyhei, G.; Oderich, G.; et al. Editor’s Choice—Management of the Diseases of Mesenteric Arteries and Veins: Clinical Practice Guidelines of the European Society of Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2017, 53, 460–510. [Google Scholar] [CrossRef] [Green Version]
- Kougias, P.; Lau, D.; El Sayed, H.F.; Zhou, W.; Huynh, T.T.; Lin, P.H. Determinants of mortality and treatment outcome following surgical interventions for acute mesenteric ischemia. J. Vasc. Surg. 2007, 46, 467–474. [Google Scholar] [CrossRef] [Green Version]
- Acosta-Merida, M.A.; Marchena-Gomez, J.; Hemmersbach-Miller, M.; Roque-Castellano, C.; Hernandez-Romero, J.M. Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J. Surg. 2006, 30, 1579–1585. [Google Scholar] [CrossRef]
- Grotelüschen, R.; Bergmann, W.; Welte, M.N.; Reeh, M.; Izbicki, J.R.; Bachmann, K. What predicts the outcome in patients with intestinal ischemia? A single center experience. J. Visc. Surg. 2019, 156, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Aliosmanoglu, I.; Gul, M.; Kapan, M.; Arikanoglu, Z.; Taskesen, F.; Basol, O.; Aldemir, M. Risk factors effecting mortality in acute mesenteric ischemia and mortality rates: A single center experience. Int. Surg. 2013, 98, 76–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paladino, N.C.; Inviati, A.; Di Paola, V.; Busuito, G.; Amodio, E.; Bonventre, S.; Scerrino, G. Predictive factors of mortality in patients with acute mesenteric ischemia. A retrospective study. Ann. Ital. Chir. 2014, 85, 265–270. [Google Scholar] [PubMed]
- Schoots, I.G.; Koffeman, G.I.; Legemate, D.A.; Levi, M.; van Gulik, T.M. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. Br. J. Surg. 2004, 91, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Liu, J.; Zhou, Z. Preoperative Risk Factors for Short-Term Postoperative Mortality of Acute Mesenteric Ischemia after Laparotomy: A Systematic Review and Meta-Analysis. Emerg. Med. Int. 2020, 2020, 1382475. [Google Scholar] [CrossRef]
- Matthaei, H.; Klein, A.; Branchi, V.; Kalff, J.C.; Koscielny, A. Acute mesenteric ischemia (AMI): Absence of renal insufficiency and performance of early bowel resection may indicate improved outcomes. Int. J. Colorectal Dis. 2019, 34, 1781–1790. [Google Scholar] [CrossRef]
- Pedersoli, F.; Schönau, K.; Schulze-Hagen, M.; Keil, S.; Isfort, P.; Gombert, A.; Alizai, P.H.; Kuhl, C.K.; Bruners, P.; Zimmermann, M. Endovascular Revascularization with Stent Implantation in Patients with Acute Mesenteric Ischemia due to Acute Arterial Thrombosis: Clinical Outcome and Predictive Factors. Cardiovasc. Interv. Radiol. 2021, 44, 1030–1038. [Google Scholar] [CrossRef]
- Cudnik, M.T.; Darbha, S.; Jones, J.; Macedo, J.; Stockton, S.W.; Hiestand, B.C. The diagnosis of acute mesenteric ischemia: A systematic review and meta-analysis. Acad. Emerg. Med. 2013, 20, 1087–1100. [Google Scholar] [CrossRef]
- Treskes, N.; Persoon, A.M.; van Zanten, A.R.H. Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: A systematic review and meta-analysis. Intern. Emerg. Med. 2017, 12, 821–836. [Google Scholar] [CrossRef]
- Leone, M.; Bechis, C.; Baumstarck, K.; Ouattara, A.; Collange, O.; Augustin, P.; Annane, D.; Arbelot, C.; Asehnoune, K.; Baldési, O.; et al. Outcome of acute mesenteric ischemia in the intensive care unit: A retrospective, multicenter study of 780 cases. Intensive Care Med. 2015, 41, 667–676. [Google Scholar] [CrossRef]
- Emile, S.H.; Khan, S.M.; Barsoum, S.H. Predictors of bowel necrosis in patients with acute mesenteric ischemia: Systematic review and meta-analysis. Updates Surg. 2021, 73, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Della Seta, M.; Kloeckner, R.; Pinto Dos Santos, D.; Walter-Rittel, T.C.; Hahn, F.; Henze, J.; Gropp, A.; Pratschke, J.; Hamm, B.; Geisel, D.; et al. Pneumatosis intestinalis and porto-mesenteric venous gas: A multicenter study. BMC Med. Imaging 2021, 21, 129. [Google Scholar] [CrossRef] [PubMed]
- Destek, S.; Yabacı, A.; Abik, Y.N.; Gül, V.O.; Değer, K.C. Predictive and prognostic value of L-lactate, D-dimer, leukocyte, C-reactive protein and neutrophil/lymphocyte ratio in patients with acute mesenteric ischemia. Ulus Travma Acil Cerrahi Derg. 2020, 26, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Yang, L.; Zhou, Z. Clinical Features and Factors Affecting Postoperative Mortality for Obstructive Acute Mesenteric Ischemia in China: A Hospital- Based Survey. Vasc. Health Risk Manag. 2020, 16, 479–487. [Google Scholar] [CrossRef]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Bednarsch, J.; Czigany, Z.; Lurje, I.; Trautwein, C.; Ludde, T.; Strnad, P.; Gaisa, N.T.; Barabasch, A.; Bruners, P.; Ulmer, T.; et al. Intraoperative Transfusion of Fresh Frozen Plasma Predicts Morbidity Following Partial Liver Resection for Hepatocellular Carcinoma. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2020, 25, 1212–1223. [Google Scholar] [CrossRef]
- Sarani, B.; Dunkman, W.J.; Dean, L.; Sonnad, S.; Rohrbach, J.I.; Gracias, V.H. Transfusion of fresh frozen plasma in critically ill surgical patients is associated with an increased risk of infection. Crit. Care Med. 2008, 36, 1114–1118. [Google Scholar] [CrossRef]
- Refaai, M.A.; Blumberg, N. Transfusion immunomodulation from a clinical perspective: An update. Expert. Rev. Hematol. 2013, 6, 653–663. [Google Scholar] [CrossRef]
- Haglund, U.; Bergqvist, D. Intestinal ischemia—The basics. Langenbeck’s Arch. Surg. 1999, 384, 233–238. [Google Scholar] [CrossRef]
- Rosenblum, J.D.; Boyle, C.M.; Schwartz, L.B. THE MESENTERIC CIRCULATION: Anatomy and Physiology. Surg. Clin. N. Am. 1997, 77, 289–306. [Google Scholar] [CrossRef]
- van Petersen, A.S.; Kolkman, J.J.; Meerwaldt, R.; Huisman, A.B.; van der Palen, J.; Zeebregts, C.J.; Geelkerken, R.H. Mesenteric stenosis, collaterals, and compensatory blood flow. J. Vasc. Surg. 2014, 60, 111–119.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | Overall Cohort (n = 179) | Arterial (n = 104) | Venous (n = 21) | NOMI (n = 54) |
|---|---|---|---|---|
| Demographics | ||||
| Gender, m/f, n (%) | 87 (48.6)/92 (51.4) | 46 (44.2)/58 (55.8) | 10 (47.6)/11 (52.4) | 31 (57.4)/23 (42.6) |
| Age, years | 71 (60–81) | 75 (63–82) | 65 (49–69) | 71 (59–78) |
| BMI, kg/m2 | 26 (23–29) | 25 (22–28) | 29 (27–37) | 26 (24–29) |
| ASA, n (%) | ||||
| I | 1 (0.6) | 0 | 1 (4.8) | 0 |
| II | 13 (7.3) | 8 (7.7) | 5 (23.8) | 0 |
| III | 126 (70.4) | 78 (75) | 13 (61.9) | 35 (64.8) |
| IV | 37 (20.7) | 17 (16.3) | 2 (9.5) | 18 (33.3) |
| Etiology, n (%) | ||||
| Embolic | 57 (54.8) | |||
| Thrombotic | 41 (39.4) | |||
| Compression | 4 (3.8) | |||
| Dissection | 1 (1) | |||
| Unknown | 1 (1) | |||
| Occluded vessel, n (%) | ||||
| TC | 3 (2.9) | |||
| SMA | 66 (63.5) | |||
| IMA | 8 (7.7) | |||
| TC+ SMA | 19 (18.3) | |||
| TC+ IMA | 1 (1) | |||
| SMA+ IMA | 5 (4.8) | |||
| TC+ SMA+ IMA | 2 (1.9) | |||
| Location of occlusion, n (%) * | ||||
| Proximal | 72 (69.2) | |||
| Distal | 31 (29.8) | |||
| Refferal from another hospital, n (%) | 53 (29.6) | 35 (33.7) | 11 (52.4) | 7 (13.2) |
| Radiological characteristics | ||||
| Pneumatosis intestinalis, n (%) | 48 (26.8) | 23 (22.1) | 1 (4.8) | 24 (44.4) |
| PMVG, n (%) | 20 (11.2) | 10 (9.6) | 0 | 10 (18.5) |
| Bowel distension, n (%) | 80 (44.7) | 42 (40.4) | 5 (23.8) | 33 (61.1) |
| Bowel wall thickening, n (%) | 99 (55.3) | 49 (47.1) | 18 (85.7) | 32 (59.3) |
| Pneumoperitoneum, n (%) | 21 (11.7) | 8 (7.7) | 0 | 13 (24.1) |
| Ascites, n (%) | 56 (31.3) | 16 (15.4) | 15 (71.4) | 25 (46.3) |
| Preoperative laboratory values | ||||
| Leukocytes, 1/nL | 15.2 (10.9–23.5) | 14.9 (10.6–22.9) | 14.9 (10.9–26.9) | 17.4 (10.4–23.8) |
| C-Reactive-Protein, mg/L | 127 (37–230) | 127 (25–230) | 84 (53–161) | 157 (97–197) |
| Hemoglobin, g/dL | 12.0 (9.4–13.7) | 12.1 (10.8–14.0) | 13.9 (12.6–16.2) | 9.0 (8.2–12.0) |
| Thrombocytes, 1/nL | 228 (142–329) | 249 (160–354) | 294 (175–359) | 149 (113–239) |
| Prothrombin time, % | 70 (52–82) | 72 (55–85) | 71 (54–83) | 64 (49–78) |
| INR | 1.25 (1.12–1.53) | 1.24 (1.10–1.49) | 1.25 (1.10–1.47) | 1.30 (1.17–1.59) |
| Bilirubin, mg/dL | 0.7 (0.4–1.2) | 0.7 (0.5–1.1) | 0.9 (0.3–1.5) | 0.8 (0.4–1.5) |
| AP, U/L | 89 (69–129) | 87 (67–112) | 85 (72–120) | 116 (70–174) |
| GGT, U/I | 45 (24–93) | 38 (23–87) | 49 (23.3–114.3) | 59 (34–132) |
| Albumin, g/dL | 2.5 (1.8–3.4) | 3.3 (1.9–3.8) | 3.0 (2.5–3.6) | 2.0 (1.6–2.7) |
| AST, U/L | 44 (26–115) | 40 (25–111) | 28 (22–37) | 88 (37–208) |
| ALT, U/L | 38 (20–102) | 31 (18–105) | 25 (19–39) | 51 (26–216) |
| Creatinine, mg/dL | 1.3 (0.9–2.2) | 1.3 (0.9–2.1) | 1.1 (0.7 –1.5) | 1.5 (1.0–3.2) |
| Lactate, mmol/L | 3.3 (1.8–6.5) | 3.3 (1.9–6.4) | 2.3 (1.2–3.6) | 4.0 (1.9–9.3) |
| Therapy Characteristics | ||||
| Extent of bowel resection, n (%) | ||||
| Small bowel | 57 (31.8) | 28 (26.9) | 20 (95.2) | 9 (16.7) |
| Colon | 56 (31.3) | 27 (26.0) | 0 | 29 (53.7) |
| Small bowel and colon | 30 (16.8) | 20 (19.2) | 0 | 10 (18.5) |
| No resection | 12 (6.7) | 11 (10.6) | 1 (4.8) | 0 |
| Fatal | 24 (13.4) | 18 (17.3) | 0 | 6 (11.1) |
| Technique of revascularization, n (%) | ||||
| Endovascular | 27 (15.1) | |||
| Open | 40 (22.3) | |||
| Thrombectomy | 30 (17.8) | |||
| Bypass, prosthetic, | 4 (2.2) | |||
| antegrade | ||||
| Bypass, prosthetic, | 4 (2.2) | |||
| retrograde | ||||
| Bypass, autologous vein, | 2 (1.2) | |||
| retrograde | ||||
| Combination | 4 (2.2) | |||
| Sequence of therapy | ||||
| Revascularization before resection | 17 (9.5) | |||
| Resection before revascularization | 20 (11.2) | |||
| Simultaneous | 18 (10.1) | |||
| Enterostomy, n (%) | 124 (69.3) | 68 (60.6) | 15 (71.4) | 46 (85.2) |
| Primary bowel anastomosis, n (%) | 14 (7.8) | 7 (6.7) | 5 (23.8) | 2 (3.7) |
| Intraoperative FFP transfusion, n (%) | 34 (19) | 12 (11.5) | 3 (14.3) | 19 (35.2) |
| Intraoperative blood transfusion, n (%) | 69 (38.5) | 38 (36.5) | 6 (28.6) | 25 (46.3) |
| Primary treatment time, minutes | 130 (99–180) | 129 (100–179) | 124 (99–179) | 140 (95–180) |
| Time to treatment, minutes | 191 (110–363) | 162 (100–269) | 593 (315–770) | 189 (113–339) |
| Intensive care stay, days | 4 (1–15) | 3.5 (1–14) | 8 (2–28) | 4 (1–16) |
| Postoperative data | ||||
| Postoperative complications, n (%) | ||||
| Clavien–Dindo I | 0 | 0 | 0 | 0 |
| Clavien–Dindo II | 13 (7.3) | 8 (7.7) | 4 (19.1) | 1 (1.9) |
| Clavien–Dindo IIIa | 9 (5) | 3 (2.9) | 2 (9.5) | 4 (7.4) |
| Clavien–Dindo IIIb | 17 (9.5) | 11 (10.6) | 4 (19.1) | 2 (3.7) |
| Clavien–Dindo IVa | 19 (10.6) | 10 (9.6) | 1 (4.8) | 8 (14.8) |
| Clavien–Dindo IVb | 19 (10.6) | 10 (9.6) | 6 (28.6) | 3 (5.6) |
| Clavien–Dindo V | 100 (55.9) | 61 (58.7) | 3 (14.3) | 36 (66.7) |
| Variable | Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|---|
| n | Hazard Ratio | 95% CI | p-Value | Hazard Ratio | 95% CI | p-Value | |
| Sex | 0.905 | ||||||
| Age | 1.02 | 1–1.05 | 0.040 | 0.961 | |||
| BMI, kg/m2 | 0.440 | ||||||
| ASA | 0.004 | 0.124 | |||||
| I/II | 15 | 1 | |||||
| III/IV | 162 | 20.89 | 2.68–162.77 | ||||
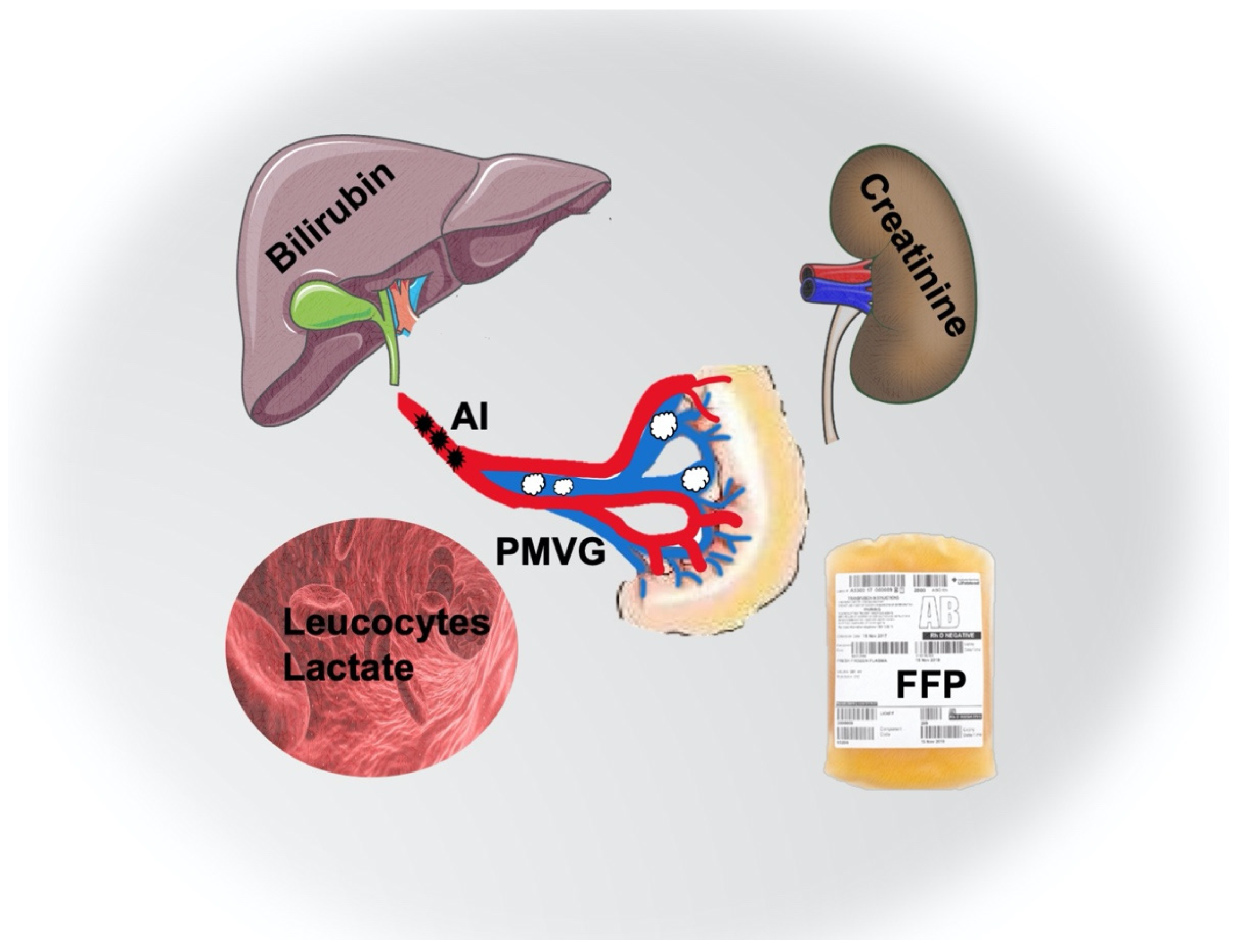
| Leukocytes, 1/nL | 1.04 | 1.01–1.07 | 0.025 | 1.08 | 1.02–1.15 | 0.008 | |
| C-Reactive-Protein, mg/L | 0.808 | ||||||
| Lactate, mmol/L | 1.45 | 1.25–1.69 | <0.001 | 1.25 | 1.05–1.47 | 0.010 | |
| Hemoglobin, g/dL | 0.90 | 0.81–0.99 | 0.048 | 0.361 | |||
| Albumin, g/L | 0.832 | ||||||
| AST, U/L | 0.077 | ||||||
| ALT, U/L | 0.653 | ||||||
| GGT, U/L | 0.178 | ||||||
| Bilirubin, mg/dL | 1.6 | 1.06–2.41 | 0.026 | 2.05 | 1.02–4.12 | 0.045 | |
| Alkaline phosphatase, U/L | 1.01 | 1–1.01 | 0.034 | ||||
| Platelet count, 1/nL | 0.290 | ||||||
| Prothrombin time, % | 0.97 | 0.96–0.98 | <0.001 | 0.377 | |||
| INR | 2.13 | 1.18–3.85 | 0.012 | 0.724 | |||
| Etiology | 0.001 | 0.038 | |||||
| Arterial | 104 | 1 | 1 | ||||
| Venous | 21 | 0.12 | 0.03–0.42 | 0.12 | 0.02–0.89 | ||
| NOMI | 54 | 1.41 | 0.71–2.8 | 0.97 | 0.32–2.97 | ||
| Pneumatosis intestinalis | 0.007 | 0.774 | |||||
| No | 121 | 1 | |||||
| Yes | 48 | 2.74 | 1.32–5.68 | ||||
| Portomesenteric vein gas | 0.005 | 0.012 | |||||
| No | 149 | 1 | 1 | ||||
| Yes | 20 | 18.25 | 2.38–139.85 | 23.02 | 2.01–263.11 | ||
| Bowel Distension | 0.030 | 0.838 | |||||
| <6 cm | 89 | 1 | |||||
| ≥6 cm | 80 | 1.99 | 1.07–3.69 | ||||
| Bowel wall thickening | 0.074 | ||||||
| Ascites | 0.415 | ||||||
| Pneumoperitoneum | 0.575 | ||||||
| Extent of resection | 0.003 | 0.284 | |||||
| Small bowel | 57 | 1 | |||||
| Colon | 56 | 1.48 | 0.7–3.13 | ||||
| Small bowel and colon | 30 | 4.38 | 1.66–11.53 | ||||
| No resection in primary operation | 12 | 1.14 | 0.32–4.03 | ||||
| Fatal | 24 | >10 | 0–n.a. | ||||
| Treatment time, minutes | 0.655 | ||||||
| Blood transfusions | 0.190 | ||||||
| Intraoperative FFP transfusion | 0.004 | 0.118 | |||||
| No | 144 | 1 | |||||
| Yes | 34 | 3.75 | 1.54–9.16 | ||||
| Time to treatment | 0.128 | ||||||
| Referral from another hospital | 0.841 |
| Variable | Mortality | ||
|---|---|---|---|
| Hazard Ratio | 95% CI | p-Value | |
| Age, years | 0.961 | ||
| ASA | 0.159 | ||
| Leucocytes, 1/nL | 1.09 | 1.03–1.15 | 0.004 |
| Lactate, mmol/L | 1.27 | 1.08–1.48 | 0.003 |
| Hemoglobin, g/dL | 0.361 | ||
| Bilirubin, mg/dL | 0.166 | ||
| Prothrombin time, % | 0.377 | ||
| INR | 0.724 | ||
| Creatinine, mg/dL | 0.710 | ||
| Etiology | 0.024 | ||
| AI | 1 | ||
| VI | 0.08 | 0.01–0.49 | |
| NOMI | 0.71 | 0.24–2.1 | |
| Pneumatosis intestinalis | 0.774 | ||
| PMVG | 17.02 | 1.62–178.58 | 0.018 |
| Bowel distension | 0.838 | ||
| Extent of resection | 0.233 | ||
| Intraoperative FFP transfusion | 4.4 | 1.2–16.11 | 0.025 |
| Variable | Mortality | |||
|---|---|---|---|---|
| n | Hazard Ratio | 95% CI | p-Value | |
| Lactate, mmol/L | ||||
| ≤2 | 48 | 1 | <0.001 | |
| >2; ≤4 | 57 | 2.52 | 1.09–5.80 | 0.030 |
| >4; ≤8 | 34 | 9.75 | 3.49–27.23 | <0.001 |
| >8 | 32 | 45 | 9.33–217.04 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otto, C.C.; Czigany, Z.; Heise, D.; Bruners, P.; Kotelis, D.; Lang, S.A.; Ulmer, T.F.; Neumann, U.P.; Klink, C.; Bednarsch, J. Prognostic Factors for Mortality in Acute Mesenteric Ischemia. J. Clin. Med. 2022, 11, 3619. https://doi.org/10.3390/jcm11133619
Otto CC, Czigany Z, Heise D, Bruners P, Kotelis D, Lang SA, Ulmer TF, Neumann UP, Klink C, Bednarsch J. Prognostic Factors for Mortality in Acute Mesenteric Ischemia. Journal of Clinical Medicine. 2022; 11(13):3619. https://doi.org/10.3390/jcm11133619
Chicago/Turabian StyleOtto, Carlos Constantin, Zoltan Czigany, Daniel Heise, Philipp Bruners, Drosos Kotelis, Sven Arke Lang, Tom Florian Ulmer, Ulf Peter Neumann, Christian Klink, and Jan Bednarsch. 2022. "Prognostic Factors for Mortality in Acute Mesenteric Ischemia" Journal of Clinical Medicine 11, no. 13: 3619. https://doi.org/10.3390/jcm11133619
APA StyleOtto, C. C., Czigany, Z., Heise, D., Bruners, P., Kotelis, D., Lang, S. A., Ulmer, T. F., Neumann, U. P., Klink, C., & Bednarsch, J. (2022). Prognostic Factors for Mortality in Acute Mesenteric Ischemia. Journal of Clinical Medicine, 11(13), 3619. https://doi.org/10.3390/jcm11133619







