Complications of Autologous Stem Cell Transplantation in Multiple Myeloma: Results from the CALM Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Characteristics
3.2. Transplant Complications
3.3. Complications by Patients’ Characteristics
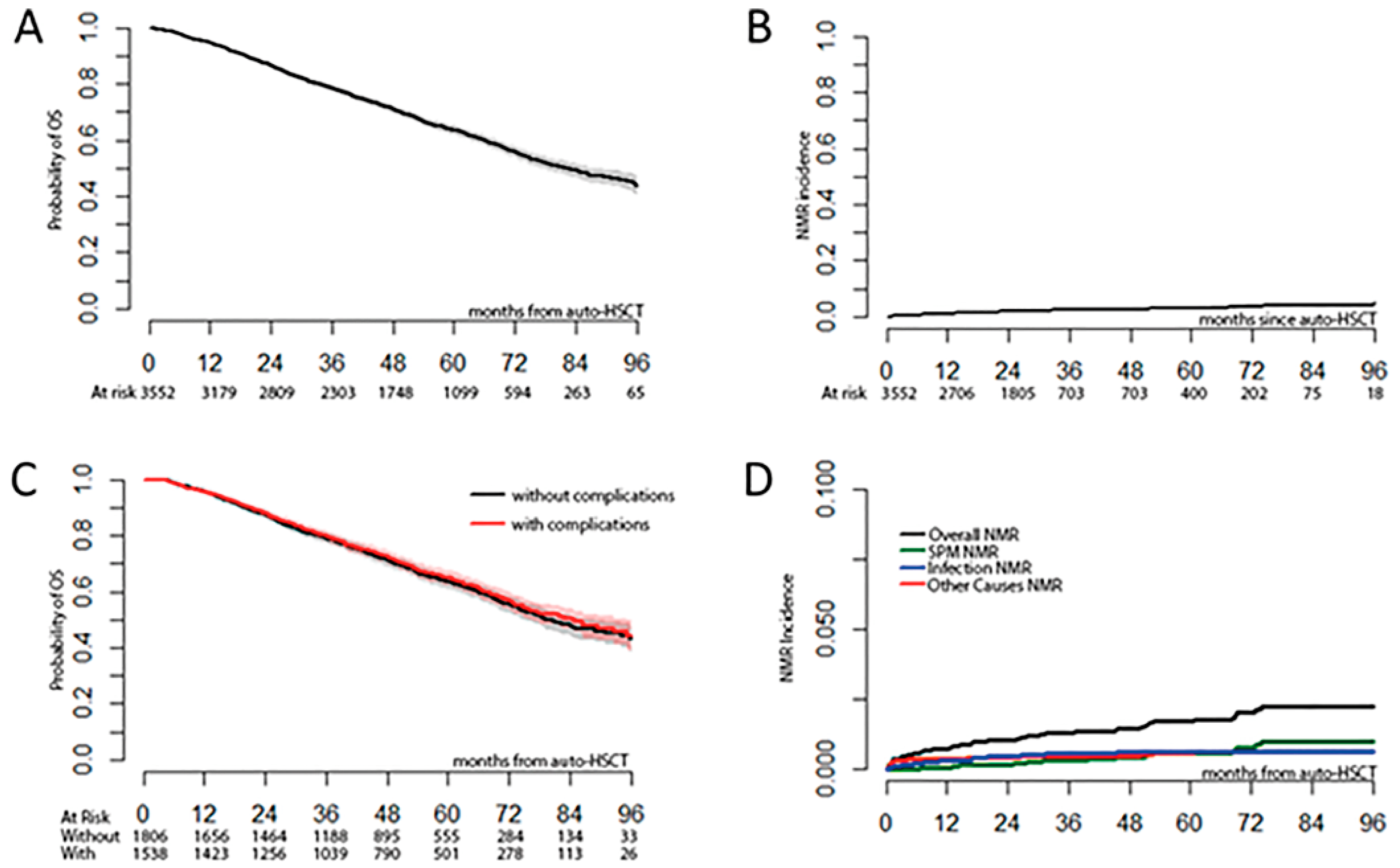
3.4. Survival
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sureda, A.; Chabannon, C.; Masszi, T.; Pohlreich, D.; Scheid, C.; Thieblemont, C.; Wahlin, B.E.; Sakellari, I.; Russell, N.; Janikova, A.; et al. Analysis of data collected in the European Society for Blood and Marrow Transplantation (EBMT) Registry on a cohort of lymphoma patients receiving plerixafor. Bone Marrow Transplant. 2020, 55, 613–622. [Google Scholar] [CrossRef]
- Morris, C.; Chabannon, C.; Masszi, T.; Russell, N.; Nahi, H.; Kobbe, G.; Krejci, M.; Auner, H.W.; Pohlreich, D.; Hayden, P.; et al. Results from a multicenter, noninterventional registry study for multiple myeloma patients who received stem cell mobilization regimens with and without plerixafor. Bone Marrow Transplant. 2020, 55, 356–366. [Google Scholar] [CrossRef] [PubMed]
- Iacobelli, S. Suggestions on the use of statistical methodologies in studies of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2013, 48, S1–S37. [Google Scholar] [CrossRef] [PubMed]
- Van der Velden, W.J.; Blijlevens, N.M.; Feuth, T.; Donnelly, J.P. Febrile mucositis in haematopoietic SCT recipients. Bone Marrow Transplant. 2009, 43, 55–60. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Waszczuk-Gajda, A.; Drozd-Sokołowska, J.; Basak, G.W.; Piekarska, A.; Mensah-Glanowska, P.; Sadowska-Klasa, A.; Wierzbowska, A.; Rzepecki, P.; Tomaszewska, A.; Mańko, J.; et al. Infectious Complications in Patients With Multiple Myeloma After High-Dose Chemotherapy Followed by Autologous Stem Cell Transplant: Nationwide Study of the Infectious Complications Study Group of the Polish Adult Leukemia Group. Transplant. Proc. 2020, 52, 2178–2185. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Rybicki, L.; Hamilton, B.K.; Pohlman, B.; Jagadeesh, D.; Cober, E.; Kalaycio, M.; Dean, R.; Sobecks, R.; Mossad, S.B.; et al. Early infectious complications after autologous hematopoietic cell transplantation for multiple myeloma. Transplant. Infect. Dis. 2019, 21, e13114. [Google Scholar] [CrossRef] [PubMed]
- Czyżewski, K.; Styczyński, J.; Giebel, S.; Frączkiewicz, J.; Salamonowicz, M.; Zając-Spychala, O.; Zaucha-Prażmo, A.; Drozd-Sokołowska, J.; Waszczuk-Gajda, A.; Dybko, J.; et al. Age-dependent determinants of infectious complications profile in children and adults after hematopoietic cell transplantation: Lesson from the nationwide study. Ann. Hematol. 2019, 98, 2197–2211. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, V.R.; Loberiza, F.R., Jr.; Jing, H.; Bociek, R.G.; Bierman, P.J.; Maness, L.J.; Vose, J.M.; Armitage, J.O.; Akhtari, M. Mortality patterns among recipients of autologous hematopoietic stem cell transplantation for lymphoma and myeloma in the past three decades. Clin. Lymphoma Myeloma Leuk. 2015, 15, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Teh, B.W.; Harrison, S.J.; Slavin, M.A.; Worth, L.J. Epidemiology of bloodstream infections in patients with myeloma receiving current era therapy. Eur. J. Haematol. 2017, 98, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Teh, B.W.; Harrison, S.J.; Worth, L.J.; Spelman, T.; Thursky, K.A.; Slavin, M.A. Risks, severity and timing of infections in patients with multiple myeloma: A longitudinal cohort study in the era of immunomodulatory drug therapy. Br. J. Haematol. 2015, 171, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, M.A.; Sonneveld, P.; Leung, N.; Merlini, G.; Ludwig, H.; Kastritis, E.; Goldschmidt, H.; Joshua, D.; Orlowski, R.Z.; Powles, R.; et al. International Myeloma Working Group Recommendations for the Diagnosis and Management of Myeloma-Related Renal Impairment. J. Clin. Oncol. 2016, 34, 1544–1557. [Google Scholar] [CrossRef] [PubMed]
- Cavo, M.; Rajkumar, S.V.; Palumbo, A.; Moreau, P.; Orlowski, R.; Bladé, J.; Sezer, O.; Ludwig, H.; Dimopoulos, M.A.; Attal, M.; et al. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood 2011, 117, 6063–6073. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S.; Rybicki, L.A.; Corrigan, D.; Bolwell, B.; Dean, R.; Liu, H.; Gerds, A.T.; Hanna, R.; Hill, B.; Jagadeesh, D.; et al. Prognostic Factors for Mortality among Day +100 Survivors after Allogeneic Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2018, 24, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Auner, H.W.; Iacobelli, S.; Sbianchi, G.; Knol-Bout, C.; Blaise, D.; Russell, N.H.; Apperley, J.F.; Pohlreich, D.; Browne, P.V.; Kobbe, G.; et al. Melphalan 140 mg/m(2) or 200 mg/m(2) for autologous transplantation in myeloma: Results from the Collaboration to Collect Autologous Transplant Outcomes in Lymphoma and Myeloma (CALM) study. A report by the EBMT Chronic Malignancies Working Party. Haematologica 2018, 103, 514–521. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Patients, n (%) |
|---|---|
| No. of patients | 3552 |
| Male gender | 2055 (57.9) |
| Age at the first transplant | |
| <65 years | 2847 (80.2) |
| ≥65 years | 705 (19.8) |
| Diagnosis, subtype of MM | |
| IgA | 684 (19.3) |
| Other Ig | 1973 (55.5) |
| Light chain or NS | 816 (23.0) |
| Missing | 79 |
| ISS stage at diagnosis | |
| I | 836 (39.2) |
| II | 776 (36.4) |
| III | 519 (24.3) |
| Missing | 1421 |
| HCT-CI = 0 (low risk) | 979 (63.4) |
| Missing | 2007 |
| KPS at the first transplant ≥80 | 3069 (94.8) |
| Missing | 314 |
| Renal function at the first transplant | |
| Normal | 2585 (90.4) |
| Missing | 693 |
| Number of treatments before transplant | |
| 1 | 1903 (64.8) |
| Missing | 617 |
| Disease status at the first transplant |  |
| CR | 557 (16.0) |
| Missing | 62 |
| Patients with second ASCT | 846 (23.8) |
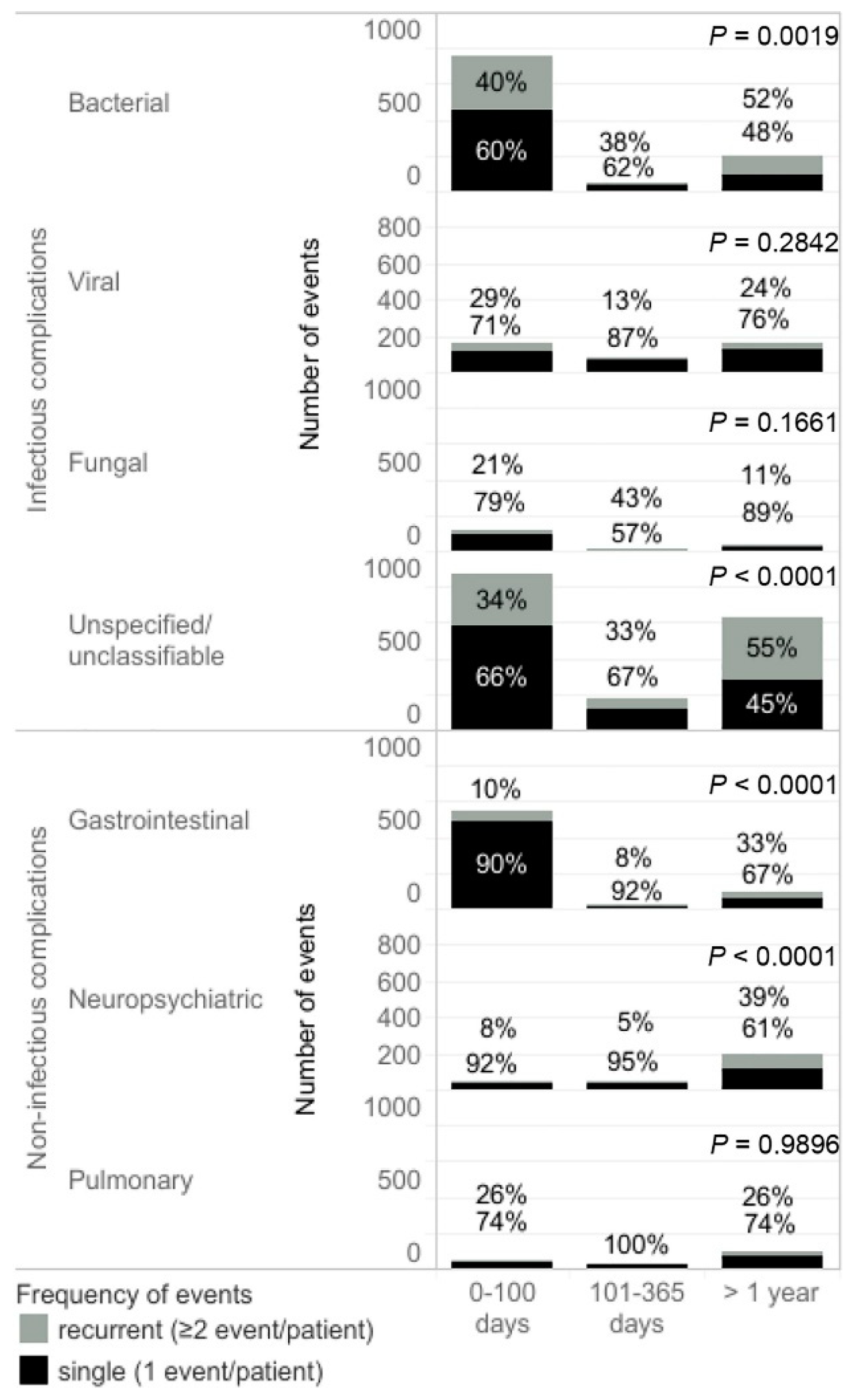
| Complication | 0–100 Days after the Transplant | 101 Days–1 Year after the Transplant | >1 Year after the Transplant |
|---|---|---|---|
| Patients with ≥1 complication, N | 1624 | 376 | 846 |
| Complications rate, cases per 100 patient-years (95% CI) | |||
| Overall | 24.85 (23.95–25.78) | 2.31 (2.13–2.50) | 2.22 (2.13–2.32) |
| Infectious complications | 16.56 (15.82–17.32) | 1.24 (1.11–1.38) | 1.05 (0.99–1.12) |
| Non-infectious complications | 8.29 (7.78–8.83) | 1.07 (0.95–1.20) | 1.17 (1.10–1.24) |
| Patients with ≥1 infectious complication, n (%) | |||
| Bacterial | 584 (36.0) | 37 (9.8) | 134 (15.8) |
| Viral | 136 (8.4) | 78 (20.7) | 140 (16.5) |
| Fungal | 107 (6.6) | 11 (2.9) | 34 (4.0) |
| Parasitic | 2 (0.1) | 0 | 1 (0.1) |
| Unspecified | 710 (43.7) | 141 (37.5) | 424 (50.1) |
| Patients with ≥1 non-infectious complication, n (%) | |||
| Gastrointestinal | 517 (31.8) | 24 (6.4) | 72 (8.5) |
| Neuropsychiatric | 49 (3.0) | 42 (11.2) | 148 (17.5) |
| Pulmonary | 36 (2.2) | 18 (4.8) | 80 (9.5) |
| Hepatic | 7 (0.4) | 3 (0.8) | 9 (1.1) |
| Characteristic | Complications Rate, Cases per 100 Patient-Years (95% CI) | Univariable Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| Rate Ratio (95% CI) | p-Value | Rate Ratio (95% CI) | p-Value | ||
| Gender | |||||
| Male | 23.70 (22.55–24.90) | 0.9 (0.83–0.97) | 0.0042 | 0.88 (0.81–0.95) | 0.003 |
| Female | 26.42 (25.00–27.90) | ||||
| Age | |||||
| <65 years | 24.24 (23.25–25.27) | 0.89 (0.81–0.97) | 0.0095 | 0.98 (0.88–1.10) | 0.754 |
| ≥65 years | 27.32 (25.22–29.56) | ||||
| Diagnosis | |||||
| IgA | 24.16 (22.16–26.29) | 0.95 (0.86–1.05) | 0.3075 | - | - |
| Other Ig | 25.45 (24.23–26.71) | 0.97 (0.87–1.09) | 0.6799 | ||
| LC or NS | 24.79 (22.93–26.76) | 1.03 (0.94–1.13) | 0.5880 | ||
| HCT-CI | |||||
| Low | 22.67 (21.05–24.38) | 0.67 (0.6–0.75) | <0.001 | - | - |
| Other | 33.64 (31.04–36.39) | ||||
| KPS | |||||
| ≥80 | 24.43 (23.47–25.42) | 0.8 (0.68–0.94) | 0.0075 | 0.70 (0.59–0.83) | <0.001 |
| <80 | 30.54 (26.09–35.54) | ||||
| ISS | |||||
| I–II | 26.43 (25.06–27.85) | 0.93 (0.84–1.04) | 0.191 | - | - |
| III | 28.37 (25.88–31.03) | ||||
| Renal function | |||||
| Normal | 4.27 (23.23–25.35) | 0.67 (0.59–0.75) | <0.001 | 0.68 (0.60–0.77) | <0.001 |
| Impaired | 36.32 (32.46–40.52) | ||||
| Treatments before transplant | |||||
| 1 | 26.55 (25.29–27.87) | 95 (0.88–1.03) | 0.244 | - | - |
| >1 | 27.88 (26.11–29.73) | ||||
| Disease status at transplant | |||||
| CR | 17.87 (15.98–19.93) | 0.68 (0.6–0.76) | <0.001 | 0.79 (0.69–0.91) | 0.001 |
| Other | 26.45 (25.43 –27.50) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waszczuk-Gajda, A.; Penack, O.; Sbianchi, G.; Koster, L.; Blaise, D.; Reményi, P.; Russell, N.; Ljungman, P.; Trneny, M.; Mayer, J.; et al. Complications of Autologous Stem Cell Transplantation in Multiple Myeloma: Results from the CALM Study. J. Clin. Med. 2022, 11, 3541. https://doi.org/10.3390/jcm11123541
Waszczuk-Gajda A, Penack O, Sbianchi G, Koster L, Blaise D, Reményi P, Russell N, Ljungman P, Trneny M, Mayer J, et al. Complications of Autologous Stem Cell Transplantation in Multiple Myeloma: Results from the CALM Study. Journal of Clinical Medicine. 2022; 11(12):3541. https://doi.org/10.3390/jcm11123541
Chicago/Turabian StyleWaszczuk-Gajda, Anna, Olaf Penack, Giulia Sbianchi, Linda Koster, Didier Blaise, Péter Reményi, Nigel Russell, Per Ljungman, Marek Trneny, Jiri Mayer, and et al. 2022. "Complications of Autologous Stem Cell Transplantation in Multiple Myeloma: Results from the CALM Study" Journal of Clinical Medicine 11, no. 12: 3541. https://doi.org/10.3390/jcm11123541
APA StyleWaszczuk-Gajda, A., Penack, O., Sbianchi, G., Koster, L., Blaise, D., Reményi, P., Russell, N., Ljungman, P., Trneny, M., Mayer, J., Iacobelli, S., Kobbe, G., Scheid, C., Apperley, J., Touzeau, C., Lenhoff, S., Jantunen, E., Anagnostopoulos, A., Paris, L., ... Basak, G. W. (2022). Complications of Autologous Stem Cell Transplantation in Multiple Myeloma: Results from the CALM Study. Journal of Clinical Medicine, 11(12), 3541. https://doi.org/10.3390/jcm11123541








