Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Registration and Reporting Format
2.2. Inclusion Criteria
- Comparing different dental materials for the restoration of carious lesions in primary teeth (the use of local anaesthesia and/or rubber dam isolation was not a limitation);
- With a clear definition of lesion location, size, and depth;
- With asymptomatic teeth (no history of pain, pulp exposure, infection, swelling, or evidence of periapical pathology);
- With at least two-arm comparisons;
- With a follow-up period of at least 12 months.
2.3. Exclusion Criteria
2.4. PICO Format for the Included Studies
- Participants: Children up to the age of 12 years with deep carious lesions in their primary dentition, with no restrictions on participants’ demographic characteristics.
- Intervention: Any dental material placed as restoration in primary teeth: amalgam (A), resin composite (RC), compomer (CO), GIC, RMGIC, metal-reinforced GIC (MRGIC), HVGIC, and stainless steel crowns (SSC).
- Comparator group: Any of the above restorative materials.
- Outcomes: Primary outcomes were treatment failure/success (criteria used were not a limitation) and restoration quality (surface roughness, colour match, marginal integrity, tooth integrity, filling integrity, proximal contact, change of sensitivity, hypersensitivity, and radiographic assessment) [22].
2.5. Search Strategy
2.6. Data Collection and Analysis
2.7. Analysis of the Degree of Overlap
2.8. Estimation of a Common Effect Size
2.9. Risk of Bias Assessment
3. Results
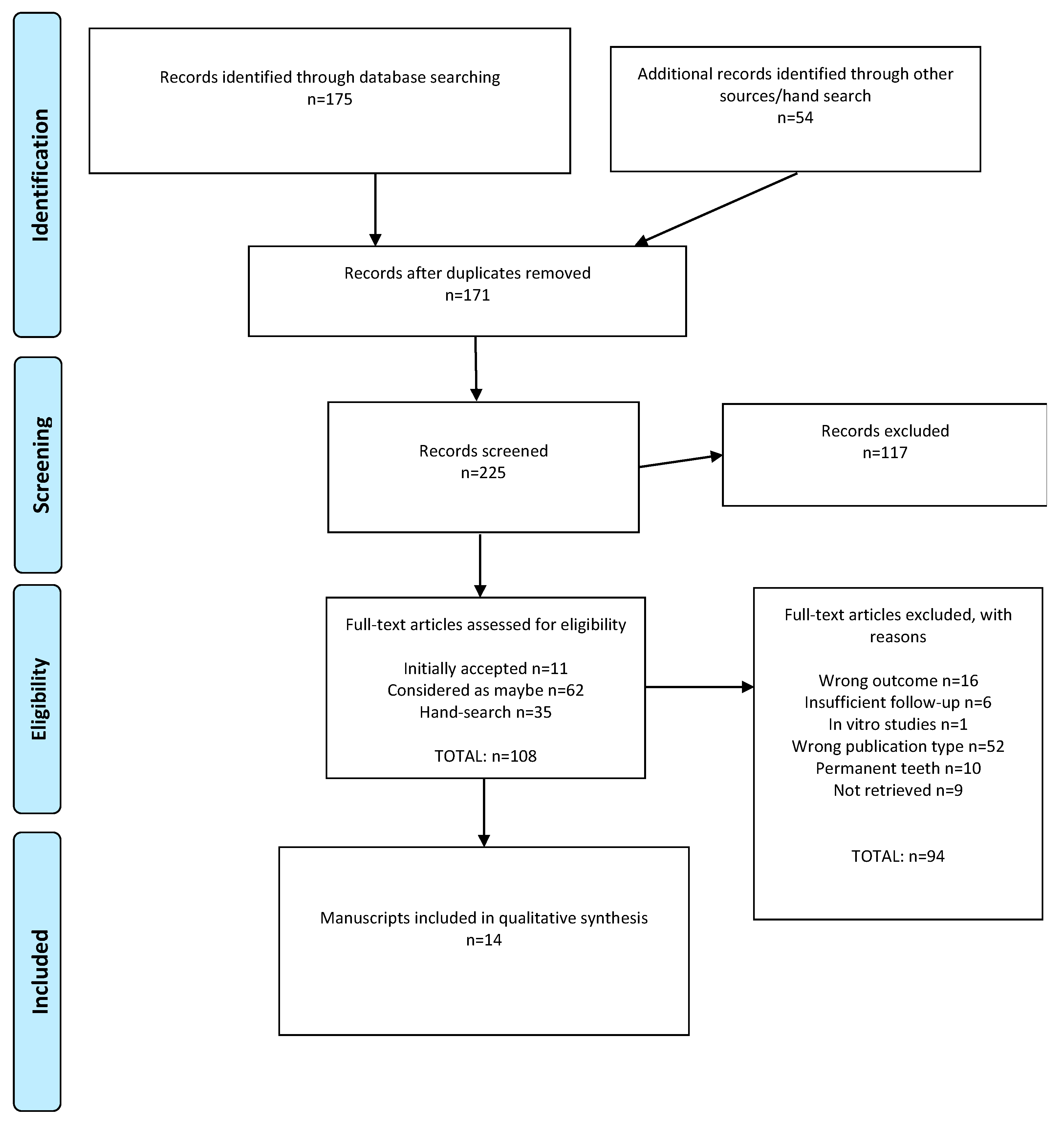
3.1. Literature Search Results
3.2. Overlap of Studies
3.3. Study Characteristics
3.4. Risk of Bias Assessment
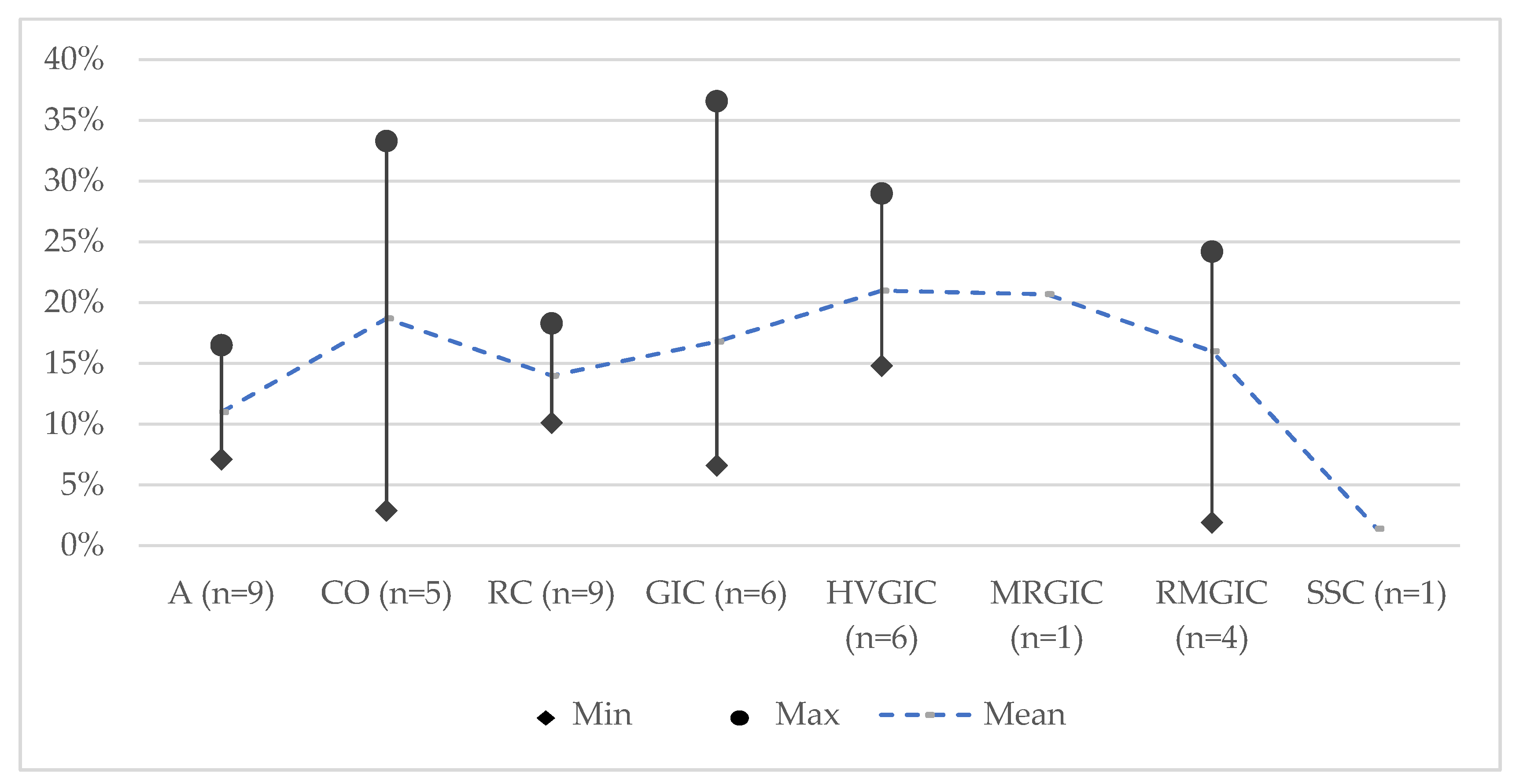
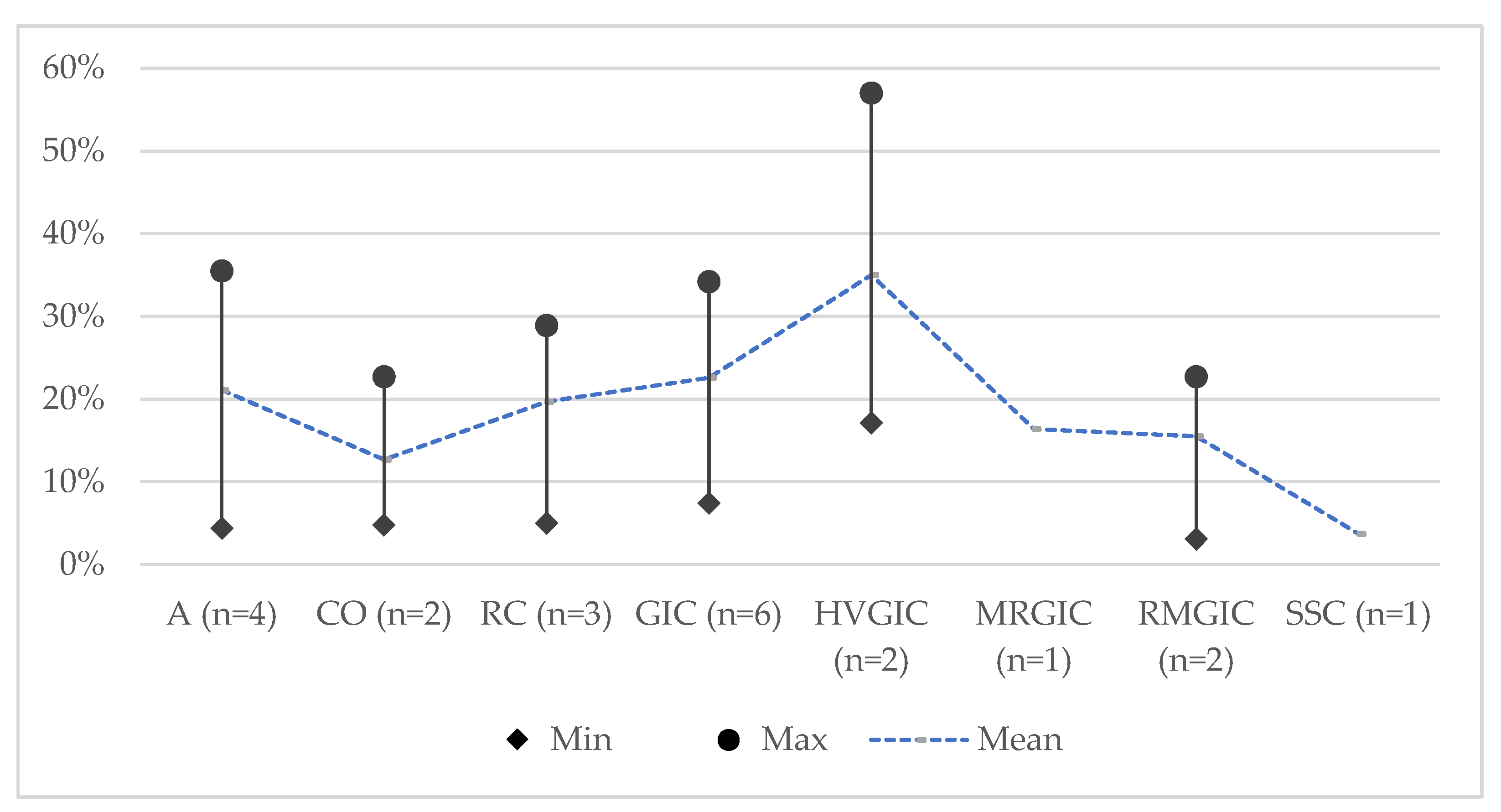
3.5. Findings of the Reviews
3.5.1. Amalgam (A)
3.5.2. Resin Composite (RC)
3.5.3. Glass-ionomer Cements (GICs)
3.5.4. Compomer (CO)
3.5.5. Stainless Steel Crowns (SSC)
3.5.6. Secondary Outcomes
3.5.7. Factors Affecting the Outcome
4. Discussion
4.1. Strengths and Limitations
4.2. Recommendations for Future Research
5. Conclusions
- All restorative materials have acceptable mean failure rates and their use for the treatment of carious primary teeth is supported.
- Among common conventional restorative materials, amalgam and resin composite had the lowest mean failure rates at 24 months and compomer at 36 months.
- Stainless steel crowns had the lowest failure rate at 24 months and 36 months compared to all other restorative materials for primary teeth.
- Limited reviews indicated that single-surface restorations and restorations placed using rubber dam isolation exhibited lower failure rates.
- The main reasons reported for the failure of both Class–I and Class–II restorations were secondary caries, restoration loss, and chipping of the marginal ridge with approximal contact loss.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lagerweij, M.D.; van Loveren, C. Declining Caries Trends: Are We Satisfied? Curr. Oral Health Rep. 2015, 2, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.B.D.O.D.; Bernabe, E.; Marcenes, W.; Hernandez, C.R.; Bailey, J.; Abreu, L.G.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z.; et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabe, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W.; Collaborators, G.B.D.O.H. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Santamaria, R.M.; Abudrya, M.H.; Gul, G.; Mourad, M.S.; Gomez, G.F.; Zandona, A.G.F. How to Intervene in the Caries Process: Dentin Caries in Primary Teeth. Caries Res. 2020, 54, 306–323. [Google Scholar] [CrossRef]
- BaniHani, A.; Santamaria, R.M.; Hu, S.; Maden, M.; Albadri, S. Minimal intervention dentistry for managing carious lesions into dentine in primary teeth: An umbrella review. Eur. Arch. Paediatr. Dent. 2021. [Google Scholar] [CrossRef]
- Schwendicke, F.; Frencken, J.E.; Bjorndal, L.; Maltz, M.; Manton, D.J.; Ricketts, D.; Van Landuyt, K.; Banerjee, A.; Campus, G.; Domejean, S.; et al. Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal. Adv. Dent. Res. 2016, 28, 58–67. [Google Scholar] [CrossRef]
- Bücher, K.; Metz, I.; Pitchika, V.; Hickel, R.; Kühnisch, J. Survival characteristics of composite restorations in primary teeth. Clin. Oral Investig. 2015, 19, 1653–1662. [Google Scholar] [CrossRef]
- Chisini, L.A.; Collares, K.; Cademartori, M.G.; de Oliveira, L.J.C.; Conde, M.C.M.; Demarco, F.F.; Correa, M.B. Restorations in primary teeth: A systematic review on survival and reasons for failures. Int. J. Paediatr. Dent. 2018, 28, 123–139. [Google Scholar] [CrossRef]
- Fuks, A.B. The use of amalgam in pediatric dentistry: New insights and reappraising the tradition. Pediatr. Dent. 2015, 37, 125–132. [Google Scholar]
- Welbury, R.R.; Walls, A.W.; Murray, J.J.; McCabe, J.F. The 5-year results of a clinical trial comparing a glass polyalkenoate (ionomer) cement restoration with an amalgam restoration. Br. Dent. J. 1991, 170, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Kavvadia, K.; Kakaboura, A.; Vanderas, A.P.; Papagiannoulis, L. Clinical evaluation of a compomer and an amalgam primary teeth class II restorations: A 2-year comparative study. Pediatr. Dent. 2004, 26, 245–250. [Google Scholar]
- Dutta, B.N.; Gauba, K.; Tewari, A.; Chawla, H.S. Silver amalgam versus resin modified GIC class-II restorations in primary molars: Twelve month clinical evaluation. J. Indian Soc. Pedod. Prev. Dent. 2001, 19, 118–122. [Google Scholar] [PubMed]
- Duggal, M.S.; Toumba, K.J.; Sharma, N.K. Clinical performance of a compomer and amalgam for the interproximal restoration of primary molars: A 24-month evaluation. Br. Dent. J. 2002, 193, 339–342. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barr-Agholme, M.; Oden, A.; Dahllof, G.; Modeer, T. A two-year clinical study of light-cured composite and amalgam restorations in primary molars. Dent. Mater. 1991, 7, 230–233. [Google Scholar] [CrossRef]
- Minamata Convention on Mercury. Available online: https://www.mercuryconvention.org/Convention/Text/tabid/3426/language/en-US/Default.aspx (accessed on 8 June 2021).
- Donly, K.J.; Mendez, M.J.C.; Contreras, C.I.; Liu, J.A. Prospective randomized clinical trial of primary molar crowns: 36-month results. Am. J. Dent. 2020, 33, 165–168. [Google Scholar]
- Krämer, N.; Lohbauer, U.; Frankenberger, R. Restorative materials in the primary dentition of poli-caries patients. Eur. Arch. Paediatr. Dent. 2007, 8, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, N.M.; Murray, J.J.; McCabe, J.F. The use of a reinforced glass-ionomer cermet for the restoration of primary molars: A clinical trial. Br. Dent. J. 1995, 179, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Dermata, A.; Papageorgiou, S.N.; Fragkou, S.; Kotsanos, N. Comparison of resin modified glass ionomer cement and composite resin in class II primary molar restorations: A 2-year parallel randomised clinical trial. Eur. Arch. Paediatr. Dent. 2018, 19, 393–401. [Google Scholar] [CrossRef]
- Tedesco, T.K.; Calvo, A.F.; Lenzi, T.L.; Hesse, D.; Guglielmi, C.A.; Camargo, L.B.; Gimenez, T.; Braga, M.M.; Raggio, D.P. ART is an alternative for restoring occlusoproximal cavities in primary teeth–evidence from an updated systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 201–209. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ryge, G.; Snyder, M. Evaluating the clinical quality of restorations. J. Am. Dent. Assoc. 1973, 87, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Pieper, D.; Antoine, S.L.; Mathes, T.; Neugebauer, E.A.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savovic, J.; Higgins, J.P.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R.; ROBIS group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Kilpatrick, N.M.; Neumann, A. Durability of amalgam in the restoration of class II cavities in primary molars: A systematic review of the literature. Eur. Arch. Paediatr. Dent. 2007, 8, 5–13. [Google Scholar] [CrossRef]
- Ruengrungsom, C.; Palamara, J.E.A.; Burrow, M.F. Comparison of ART and conventional techniques on clinical performance of glass-ionomer cement restorations in load bearing areas of permanent and primary dentitions: A systematic review. J. Dent. 2018, 78, 1–21. [Google Scholar] [CrossRef]
- Van ‘t Hof, M.A.; Frencken, J.E.; van Palenstein Helderman, W.H.; Holmgren, C.J. The atraumatic restorative treatment (ART) approach for managing dental caries: A meta-analysis. Int. Dent. J. 2006, 56, 345–351. [Google Scholar] [CrossRef]
- Innes, N.P.; Ricketts, D.; Chong, L.Y.; Keightley, A.J.; Lamont, T.; Santamaria, R.M. Preformed crowns for decayed primary molar teeth. Cochrane Database Syst. Rev. 2015, 2015, CD005512. [Google Scholar] [CrossRef]
- Dias, A.G.A.; Magno, M.B.; Delbem, A.C.B.; Cunha, R.F.; Maia, L.C.; Pessan, J.P. Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: A systematic review and meta-analysis. J. Dent. 2018, 73, 1–13. [Google Scholar] [CrossRef]
- Pires, C.W.; Pedrotti, D.; Lenzi, T.L.; Soares, F.Z.M.; Ziegelmann, P.K.; Rocha, R.O. Is there a best conventional material for restoring posterior primary teeth? A network meta-analysis. Braz. Oral Res. 2018, 32, e10. [Google Scholar] [CrossRef]
- Delgado, A.H.S.; Jamal, H.; Young, A.; Ashley, P. Scoping review of trials evaluating adhesive strategies in pediatric dentistry: Where do simplified strategies lie? BMC Oral Health 2021, 21, 33. [Google Scholar] [CrossRef] [PubMed]
- Mickenautsch, S.; Yengopal, V.; Banerjee, A. Atraumatic restorative treatment versus amalgam restoration longevity: A systematic review. Clin. Oral Investig. 2010, 14, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Tedesco, T.K.; Gimenez, T.; Floriano, I.; Montagner, A.F.; Camargo, L.B.; Calvo, A.F.B.; Morimoto, S.; Raggio, D.P. Scientific evidence for the management of dentin caries lesions in pediatric dentistry: A systematic review and network meta-analysis. PLoS ONE 2018, 13, e0206296. [Google Scholar] [CrossRef] [PubMed]
- Mickenautsch, S.; Yengopal, V. Absence of carious lesions at margins of glass-ionomer cement and amalgam restorations: An update of systematic review evidence. BMC Res. Notes 2011, 4, 58. [Google Scholar] [CrossRef] [PubMed]
- Frencken, J.E.; Liang, S.; Zhang, Q. Survival estimates of atraumatic restorative treatment versus traditional restorative treatment: A systematic review with meta-analyses. Br. Dent. J. 2021. [Google Scholar] [CrossRef]
- Siokis, V.; Michailidis, T.; Kotsanos, N. Tooth-coloured materials for class II restorations in primary molars: Systematic review and meta-analysis. Eur. Arch. Paediatr. Dent. 2021, 22, 1003–1013. [Google Scholar] [CrossRef]
- Mickenautsch, S.; Yengopal, V.; Leal, S.C.; Oliveira, L.B.; Bezerra, A.C.; Bonecker, M. Absence of carious lesions at margins of glass-ionomer and amalgam restorations: A meta-analysis. Eur. J. Paediatr. Dent. 2009, 10, 41–46. [Google Scholar]
- Jamali, Z.; Najafpour, E.; Ebrahim Adhami, Z.; Sighari Deljavan, A.; Aminabadi, N.A.; Shirazi, S. Does the length of dental procedure influence children’s behavior during and after treatment? A systematic review and critical appraisal. J. Dent. Res. Dent. Clin. Dent. Prospects 2018, 12, 68–76. [Google Scholar] [CrossRef]
- Hübel, S.; Mejare, I. Conventional versus resin-modified glass-ionomer cement for Class II restorations in primary molars. A 3-year clinical study. Int. J. Paediatr. Dent. 2003, 13, 2–8. [Google Scholar] [CrossRef]
- Cury, J.A.; de Oliveira, B.H.; dos Santos, A.P.; Tenuta, L.M. Are fluoride releasing dental materials clinically effective on caries control? Dent. Mater. 2016, 32, 323–333. [Google Scholar] [CrossRef]
- Schwendicke, F.; Göstemeyer, G.; Blunck, U.; Paris, S.; Hsu, L.Y.; Tu, Y.K. Directly Placed Restorative Materials: Review and Network Meta-analysis. J. Dent. Res. 2016, 95, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.B.; Calvao, C.; Vieira, F.S.; Neves, J.A.; Mendes, J.J.; Machado, V.; Botelho, J. Vital and Nonvital Pulp Therapy in Primary Dentition: An Umbrella Review. J. Clin. Med. 2021, 11, 85. [Google Scholar] [CrossRef] [PubMed]
- Göstemeyer, G.; Blunck, U.; Paris, S.; Schwendicke, F. Design and Validity of Randomized Controlled Dental Restorative Trials. Materials 2016, 9, 372. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; for the CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Gizani, S.; Seremidi, K.; Stratigaki, E.; Tong, H.J.; Duggal, M.; Kloukos, D. Vital Pulp Therapy in Primary Teeth with Deep Caries: An Umbrella Review. Pediatr. Dent. 2021, 43, 426–437. [Google Scholar]
- Demarco, F.F.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Marquillier, T.; Domejean, S.; Le Clerc, J.; Chemla, F.; Gritsch, K.; Maurin, J.C.; Millet, P.; Perard, M.; Grosgogeat, B.; Dursun, E. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. J. Dent. 2018, 68, 1–9. [Google Scholar] [CrossRef]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjor, I.; Bayne, S.; Peters, M.; Hiller, K.A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef]
| Author, Year | Total Number and Study Designs Included | Intervention | Comparator Group | Outcomes | Criteria | Follow-Up (Months) | Quantitative Synthesis Performed |
|---|---|---|---|---|---|---|---|
| Siokis et al., 2021 [37] | 10 RCTs (5 split-mouth and 4 parallel-arm) | Tooth-coloured materials | Between each other | Failure rate | NR | 18–48 | Six studies included |
| Chisini et al., 2018 [8] | 17 RCTs (8 split-mouth and 5 parallel-arm); 14 non-RCTs (6 parallel-arm and 1 split-mouth) | Conventional restorative materials (A, GIC, CO, RC, MRGIC, RMGIC,) and SSC | Materials, techniques, and related factors associated with restoration failure | Annual failure rate, survival rate, and success rate | Modified USPHS (n = 21); FDI (n = 2); own criteria (n = 8) | 12–48 | Not performed |
| Delgado et al., 2021 [32] | 7 RCTs (6 split-mouth); 1 non-RCT | RC which varied the resin-based composite, underlying adhesive strategy, or the application strategy/mode | Between each other | Survival rate and retention | Modified USPHS (n = 6); FDI (n = 2) | 12–36 | Not performed |
| Dias et al., 2018 [30] | 10 RCTs (6 split-mouth and 4 parallel-arm) | GIC and RMGIC | RC | Clinical performance (secondary caries, marginal discolouration/adaptation, longevity, retention, wear, and anatomical form) | Modified USPHS (n = 7); FDI (n = 2); own criteria (n = 1) | 6–48 | Nine studies included |
| Frencken et al., 2021 [36] | 6 RCTs (3 split-mouth and 3 parallel-arm) | Combination of ART and HVGIC | A and RC | Survival rate | ART (n = 4); USPHS (n = 1); ART/USPHS (n = 1) | 24–36 | Not performed |
| Innes et al., 2015 [29] | 5 RCTs (3 split-mouth and 1 parallel-arm) | Preformed crowns | Conventional restorative materials | Major failure | NR | 12–60 | Three studies included |
| Kilpatrick et al., 2007 [26] | 17 RCTs (11 split-mouth and 5 parallel-arm) | A | CO, RC, and GIC | Failure rate | ART (n = 1); USPHS (n = 10); ART/USPHS (n = 1); DPDHS (n = 1) | 24–96 | Not performed |
| Mickenautsch et al., 2009 [38] | 3 RCTs (2 split-mouth and 1 parallel-arm) | ART using GIC | A | Longevity (dichotomous success/failure rates) | ART (n = 3) | 12–36 | Two studies included |
| Mickenautsch et al., 2011 [35] | 6 RCTs (2 split-mouth, 1 parallel-arm, and 3 partial split-mouth) | GIC | A | Recurrent caries, caries on margins, and caries progression | ART (n = 2); USPHS (n = 3); DPDHS (n = 1) | 12–60 | Two studies included |
| Pires et al., 2018 [31] | 17 RCTs (10 split-mouth, 1 split-mouth in most samples, and 6 parallel-arm) | Conventional restorative materials (A, CO, RC, GIC, RMGIC, HVGIC, and MRGIC) | Between each other | Survival rate | USPHS (n = 15); FDI (n = 2) | 12–60 | Seventeen studies included |
| Ruengrungsom et al., 2018 [27] | 32 RCTs (13 split-mouth and 19 parallel-arm); 3 retrospective studies | GIC (ART and conventional) restorations | Other tested materials | AFR and qualitative description (five studies) | (Modified) USPHS (n = 15); ART (n = 10); ART/USPHS (n = 2); FDI (n = 2); Roeleveld (n = 2); Gemert–Schrik’s criteria (n = 1); own criteria (n = 8) | 18–84 | Not performed |
| Tedesco et al., 2017 [20] | 4 RCTs (2 split-mouth and 2 parallel-arm) | ART restorations with HVGIC | Conventional Class–II restorations with A and RC | Longevity, pulp damage, and caries lesion progression | Modified USPHS (n = 1); ART (n = 3) | 24–36 | Four studies included |
| Tedesco et al., 2018 [34] | 14 RCTs (5 split-mouth and 9 parallel-arm); 1 observational study | CRT, ART, and HVGIC | Between each other | Success rate and caries lesion arrestment | ART (n = 4); ART and USPHS (n = 1); USPHS (n = 1); criteria by Innes et al., 2007 (n = 2); criteria by Aguilar et al., 2007 (n = 1); criteria by Houpt et al., 1983 (n = 1); based on Miller, 1959 and Kidd, 2010 (n = 1); PUFA-Index (n = 1); visual and tactile characteristics of caries lesion arrestment (n = 2); according to the dentist’s assessment (n = 1) | 6–84 s | Thirteen studies included |
| van’t Hof et al., 2006 [28] | 7 RCTs (3 split-mouth and 4 parallel-arm); 1 longitudinal; and 1 NR | ART restorations using medium and high-viscosity GIC | Between each other | Success rate and mean AFR | Most used ART criteria | 12–36 | Ten studies included |
| Author, Year | Quality Assessment Tool Used | Review Process | Risk of Bias | Concerns | |||
|---|---|---|---|---|---|---|---|
| SEC | ISS | DCSA | SF | ||||
| Siokis et al., 2021 [37] | Cochrane Collaboration tool |  |  |  |  |  | Meta-analysis performed using studies of unclear or high risk of bias |
| Chisini et al., 2018 [8] | Cochrane Collaboration tool |  |  |  |  |  | Language restrictions |
| Delgado et al., 2021 [32] | Cochrane Collaboration tool |  |  |  |  |  | Publication date restrictions |
| Dias et al., 2018 [30] | Cochrane Collaboration tool |  |  |  |  |  | Inclusion criteria and outcomes not clearly mentioned, a meta-analysis performed using studies of high risk of bias |
| Frencken et al., 2021 [36] | Criteria by De Amorim et al., 2017 |  |  |  |  |  | Search strategy not reproducible; inclusion criteria not clearly mentioned; outcomes not pre-defined; no details given on data collection and appraisal; no clear data synthesis; and risk of bias tool not validated |
| Innes et al., 2015 [29] | Cochrane Collaboration Tool |  |  |  |  |  | — |
| Kilpatrick et al., 2007 [26] | Criteria by Curzon and Toumba, 2006 |  |  |  |  |  | Restricted data search; language restrictions; risk of bias tool not validated; no evaluation of clinical and methodological heterogeneity; and limited data on data collection and synthesis |
| Mickenautsch et al., 2010 [33] | Cochrane Collaboration tool |  |  |  |  |  | Language restrictions |
| Mickenautsch et al., 2011 [35] | Based on the availability of evidence indicating successful prevention of selection and detection/performance bias from start to the end of each trial |  |  |  |  |  | Risk of bias tool not validated; meta-analysis performed using studies of unclear or high risk of bias |
| Pires et al., 2018 [31] | Cochrane Collaboration Tool |  |  |  |  |  | Meta-analysis performed using studies of unclear or high risk of bias |
| Ruengrungsom et al., 2018 [27] | Cochrane Collaboration Tool |  |  |  |  |  | Restricted search strategy and data search; language restrictions; no details given on data collection and appraisal; primary studies with clinical and methodological heterogeneity; a majority of studies with an unclear risk of bias; and no meta-analysis performed |
| Tedesco et al., 2017 [20] | Cochrane Collaboration Tool |  |  |  |  |  | Meta-analysis performed using studies of unclear risk of bias; heterogeneity and publication bias of primary studies |
| Tedesco et al., 2018 [34] | Cochrane Collaboration Tool |  |  |  |  |  | Meta-analysis performed using studies of unclear or high risk of bias |
| van’t Hof et al., 2006 [28] | NR |  |  |  |  |  | Language restrictions; search strategy not reproducible; restricted data search; inclusion criteria not clearly mentioned; and risk of bias tool not reported |
 = Low risk of bias.
= Low risk of bias.  = High risk of bias.
= High risk of bias.  = Unclear risk of bias.
= Unclear risk of bias.| Author, Year | Restorative Material Assessed (Number of Studies) | Type of Teeth | Number of Teeth Assessed (Initially/Latest Follow-Up) | Type of Cavity | Isolation | Caries Removal Technique | Conclusions |
|---|---|---|---|---|---|---|---|
| Siokis et al., 2021 [37] | CO (n = 4); GIC (n = 3); HVGIC (n = 1); RC (n = 8); RMGIC (n = 7) | Posterior | 1023 restorations | Class–II | NR | NR | Resin-based restorative materials (RC and CO) and RMGIC appeared to have no statistically significant differences based on a “moderate” level of evidence. |
| Chisini et al., 2018 [8] | A (n = 6); CO (n = 9); GIC (n = 5); MRGIC (n = 4); RC (n = 6); RMGIC (n = 10); SSC (n = 3) | Posterior | 8679/7392, range: 40–1834 | Class–I (n = 1); Class–II (n = 15); Class–I/II (n = 12); crown restorations (n = 3) | RD (n = 11); no isolation (n = 10); yes/no (n = 3) | NR | Resin composite exhibited the lowest failure rates, whereas MRGIC exhibited the highest. SSC had the highest success rate. Higher success rates were observed in restorations of a single tooth surface and those performed with rubber dam isolation. Secondary caries was the main reason for failure. |
| Delgado et al., 2021 [32] | RC (n = 5); adhesive systems (n = 2); surface pre-treatments (n = 1); reducing etching time of an etch-and-rinse contemporary adhesive (n = 1); novel self-adhesive composites (n = 2); application modes of a universal adhesive (n = 1); bulk-fill RC (n = 1); sonic-resin placement system in bulk (n = 1); novel base RC (n = 1); contemporary adhesives (n = 1) | NR | 723 restorations | Class–I (n = 494); Class–II (n = 229) | RD (n = 6) | CCR (n = 7); SCR (n = 1) | Novel approaches such as bulk-fill resin composites, self-adhesive restoratives, and adhesives have comparable performance to traditional materials. All materials were deemed clinically acceptable in children. |
| Dias et al., 2018 [30] | RMGIC (n = 6); GIC (n = 4); RC (n = 10) | Posterior | 1425/932, range:75–344/8–207 | Class–II | RD (n = 7); CR (n = 3) | NR | GIC and RC presented a similar clinical performance for all criteria analysed, except for secondary carious lesions in which GIC presented superior performance, especially for the RMGIC and with rubber dam isolation. |
| Frencken et al., 2021 [36] | A (n = 4); GIC (n = 6); RC (n = 2) | Posterior | 2067 restorations | Class–I/II (n = 6) | NR | NR | No statistically significant difference was found between the weighted mean survival percentages of ART/HVGIC and traditional treatments in both single- and multiple-surface restorations in the primary molars. |
| Innes et al., 2015 [29] | PMC (n = 5); open sandwich using RMGIC or RC (n = 2); restorative materials (n = 2); aesthetic crown (n = 1); non-restorative treatment (n = 1) | Posterior | 80–264 teeth | Multiple-surface | NR | CCR +/− PCR (n = 1); pulpotomy (n = 2) | Crowns placed on primary teeth with carious lesions reduce the risk of major failure or pain in the long term compared to fillings. |
| Kilpatrick et al., 2007 [26] | A (n = 17); CO (n = 8); GIC (n = 8); RC (n = 3) | Posterior | Range: 40–1035 | Class–II | RD (n = 8); no RD (n = 5) | NR | Amalgam used to restore interproximal (Class–II) cavities in primary molars can be expected to survive a minimum of 3.5 years, but potentially in excess of 7 years, remains an appropriate treatment option for the management of caries in children. |
| Mickenautsch et al., 2010 [33] | A (n = 3); HVGIC (n = 3) | Posterior | 1951 restorations at latest follow-up, range: 5–610 | Class–I (n = 1); Class–I/II (n = 2) | NR | NR | ART restorations with HVGIC appear to be equally successful, and their survival rate may even exceed that of amalgam fillings. |
| Mickenautsch et al., 2011 [35] | GIC (n = 9); A (n = 9) | Posterior | Range: 32–1035 teeth | Single-surface (n = 3); multiple-surface (n = 2); combination (n = 4) | NR | NR | GIC-restored cavities show less recurrent carious lesions than cavities restored with amalgam. |
| Pires et al., 2018 [31] | A (n = 8); CO (n = 9); GIC (n = 3); RC (n = 10); RMGIC (n = 7) | Posterior | 2687 teeth | Class–I/II (n = 7); Class–II (n = 10) | RD (n = 9); no RD (n = 6); NR (n = 2) | NR | There is no advantage among restorative treatments using CO, RMGIC, A, and RC, although GIC conventional restorations have a higher risk of failure. |
| Ruengrungsom et al., 2018 [27] | A (n = 9); CO (n = 4); GIC (n = 7); Giomer (n = 1); HVGIC (n = 23); RC (n = 8); RMGIC (n = 13); MRGIC (n = 4) | Posterior | Conventional restorations: 3976/3381, range: 13–456; ART restorations: 6959/4588, range: 13–425 | Class–I; Class–II; multiple-surface | RD (n = 10); partially RD (n = 1); no RD (n = 2); NR (n = 27) | NR | The conventional technique showed a higher survival rate than ART for Class–I and multi-surface restorations with GIC. For both restorative approaches, the AFRs of Class–II and multi-surface GIC restorations were increased compared to those of Class–I restorations. The main reasons for the failure of Class–I and Class–II restorations were restoration loss and chipping of the marginal ridge with approximal contact loss. |
| Tedesco et al., 2017 [20] | A (n = 3); HVGIC (n = 4); RC (n = 1) | Posterior | ART restorations: 985/NR, range: 9–610; conventional restorations: 786/NR, range: 9–425 | Class–II | NR | Spoon excavator (ART); NR (conventional) | ART Class–II restorations with HVGIC presented a similar survival rate compared to conventional Class–II restorations with RC/A. |
| Tedesco et al., 2018 [34] | A (n = 4); CO (n = 2); HT (n = 2) HVGIC (n = 8); NR (n = 1); NRCT (n = 1); RC (n = 3); RMGIC (n = 1); RS (n = 2); SSC (n = 1); SDF (n = 3); UCT (n = 1) | Posterior (probably) | 8064 teeth, range: 9–1107 | Class–I (n = 11); Class–II (n = 10); smooth surface (n = 3) | NR | Hand instrument (ART); rotary (conventional) | CRT with resin composite demonstrated better performance compared to resin sealant. |
| van’t Hof et al., 2006 [28] | GIC (n = 1); HVGIC (n = 8) | NR (probably posterior) | NR | Single-surface; multiple-surface | NR | NR | While single-surface ART restorations with HVGIC exhibited high survival rates, those of multi-surface ART restorations were low. |
| Review | Restorative Material | ||||
|---|---|---|---|---|---|
| RC | GIC | HVGIC | RMGIC | Crowns | |
| Siokis et al., 2021 [37] | RC vs. CO: RR 1.12 (0.41, 3.02); p = 0.83; I2 = 57% RC vs. RMGIC: RR 1.10 (0.74, 1.63); p = 0.65; I2 = 0% | RMGIC vs. CO: RR 1.04 (0.59, 1.84); p = 0.88; I2 = 1% | |||
| Dias et al., 2018 [30] | CO vs. GIC: Overall: RR 0.03 (–0.00, 0.06); p = 0.06; I2 = 27% Marginal adaptation: RR 0.00 (–0.05, 0.05); p = 1.00; I2 = 0% Marginal discoloration: RR 0.07 (–0.08, 0.21); p = 0.38; I2 = 77% Anatomic form: RR 0.01 (–0.03, 0.06); p = 0.58; I2 = 0% Secondary caries: RR 0.06 (0.02, 0.10); p = 0.008; I2 = 0% | ||||
| Innes et al., 2015 [29] | Crowns vs. fillings: Major failure: RR 0.18, 95% CI (0.06, 0.56), I2 = 0% at 24 months Crowns vs. NRCT: Major failure: RR 0.12; 95% CI (0.01, 2.18) at 12 months | ||||
| Mickenautsch et al., 2009 [38] | GIC vs. A: OR 2.00; CI (0.06–5.05); p = 0.10 at 36 months | ||||
| Mickenautsch et al., 2010 [33] | GIC vs. A: RR 0.93; 95% CI (0.83, 1.06); p = 0.26 at 12 months RR 1.07; 95% CI (0.91, 1.27); p = 0.39 at 24 months | ||||
| Pires et al., 2018 [31] | GIC vs. RC: RR 4.00; 95% CI (1.19, 13.41) GIC vs. RMGIC: RR 4.70; 95% CI (1.09, 20.27) GIC vs. A: RR 1.62; 95% CI (1.05, 2.52) | RMGIC vs. A: RR 0.6; 95% CI (0.42, 0.86) | |||
| Tedesco et al., 2017 [20] | Pooled estimate for ART success: OR 0.887, 95% CI (0.574, 1.371) | ||||
| Tedesco et al., 2018 [34] | RC vs. RS: Overall: RR 11.16, 95% CI (2.46, 50.62) Caries arrest: RR 7.89, 95% CI (0.39, 160.91) | ||||
| van’t Hof et al., 2006 [28] | Weighted mean % for survival (95% CI) for single-surface ART: 12 months 95 (94, 97) 24 months 91 (88, 93) 36 months 86 (83, 90). Weighted mean % for survival (95% CI) for multiple-surface ART: 12 months 73 (70, 77) 24 months 59 (55, 64) 36 months 49 (44, 54) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amend, S.; Seremidi, K.; Kloukos, D.; Bekes, K.; Frankenberger, R.; Gizani, S.; Krämer, N. Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review. J. Clin. Med. 2022, 11, 3490. https://doi.org/10.3390/jcm11123490
Amend S, Seremidi K, Kloukos D, Bekes K, Frankenberger R, Gizani S, Krämer N. Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review. Journal of Clinical Medicine. 2022; 11(12):3490. https://doi.org/10.3390/jcm11123490
Chicago/Turabian StyleAmend, Stefanie, Kyriaki Seremidi, Dimitrios Kloukos, Katrin Bekes, Roland Frankenberger, Sotiria Gizani, and Norbert Krämer. 2022. "Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review" Journal of Clinical Medicine 11, no. 12: 3490. https://doi.org/10.3390/jcm11123490
APA StyleAmend, S., Seremidi, K., Kloukos, D., Bekes, K., Frankenberger, R., Gizani, S., & Krämer, N. (2022). Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review. Journal of Clinical Medicine, 11(12), 3490. https://doi.org/10.3390/jcm11123490








