How Bronchoscopic Dye Marking Can Help Minimally Invasive Lung Surgery
Abstract
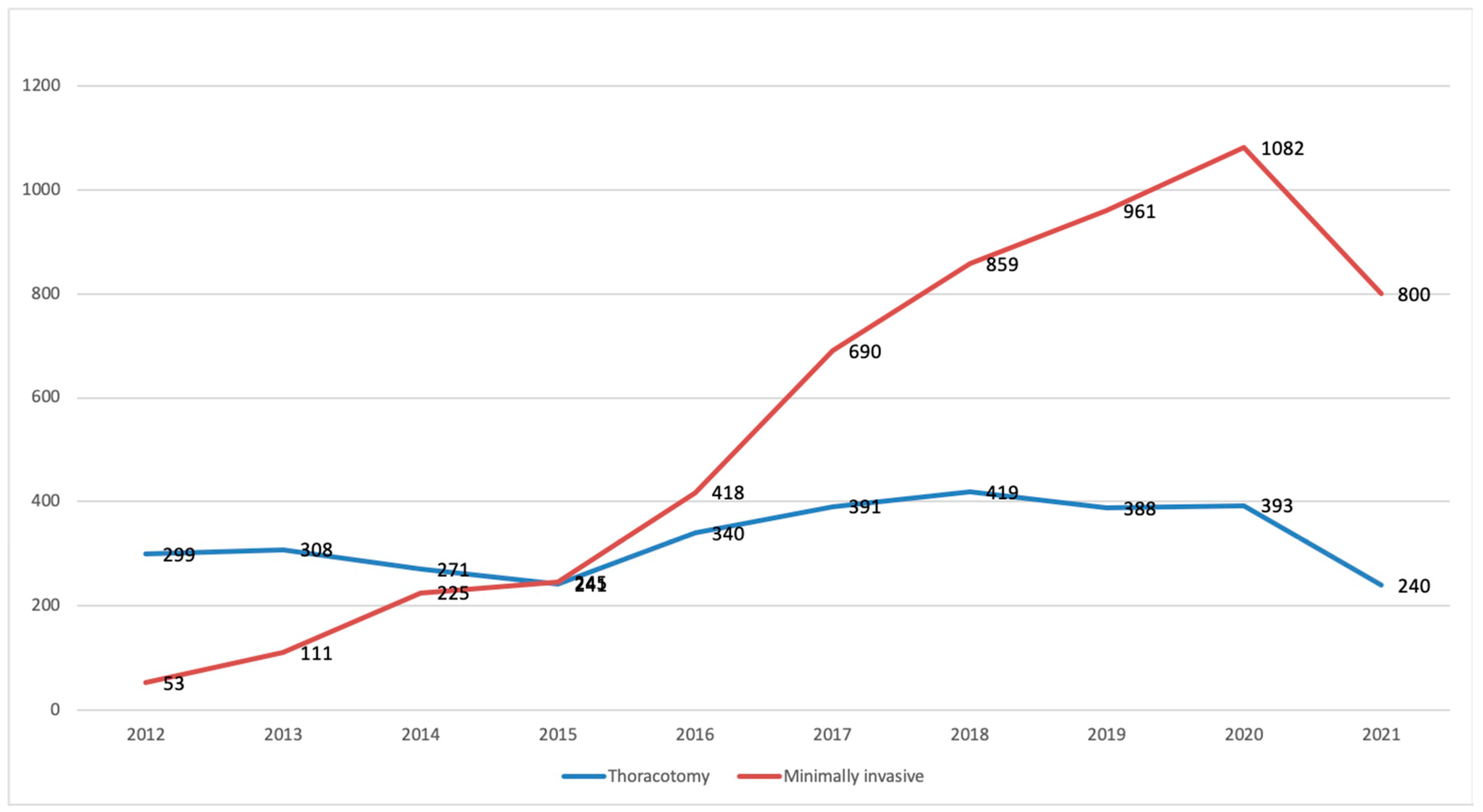
:1. Surgery in Lung Cancer
2. A Word on Endobronchially Delivered Markers
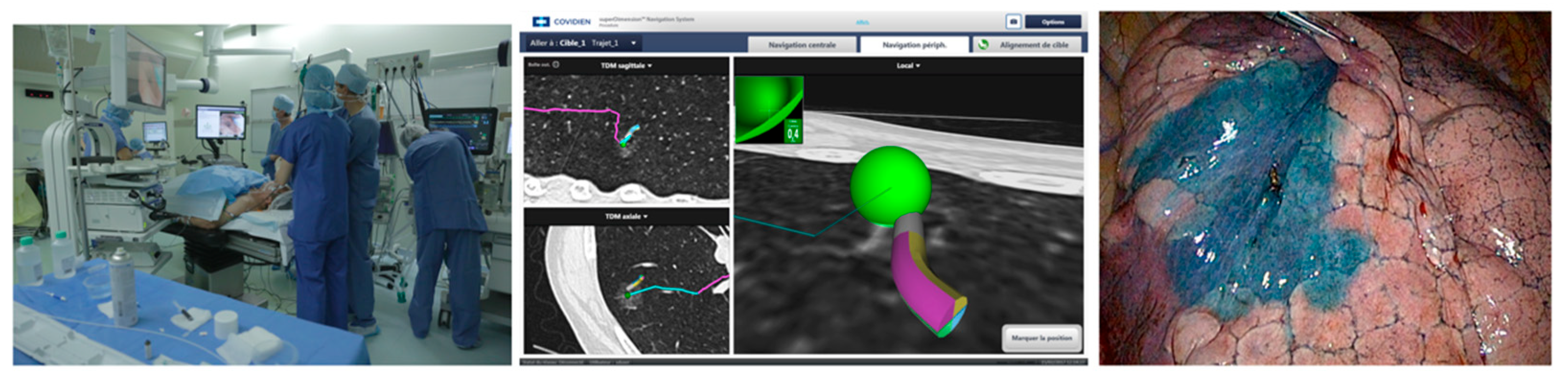
3. Electromagnetic Navigation Bronchoscopy
4. Virtual-Assisted Lung Mapping (VAL-MAP)
5. Virtual Bronchoscopy Combined with Radial EBUS
6. Robot-Assisted Broncho-Navigation
7. Conclusions
Funding
Conflicts of Interest
References
- Ost, D.; Fein, A.M.; Feinsilver, S.H. Clinical practice. The solitary pulmonary nodule. N. Engl. J. Med. 2003, 348, 2535–2542. [Google Scholar] [CrossRef] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Koning, H.J.; van der Aalst, C.M.; de Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef]
- Bedetti, B.; Bertolaccini, L.; Rocco, R.; Schmidt, J.; Solli, P.; Scarci, M. Segmentectomy versus lobectomy for stage I non-small cell lung cancer: A systematic review and meta-analysis. J. Thorac. Dis. 2017, 9, 1615–1623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, S.; Stiles, B.; Altorki, N. What is the role of wedge resection for T1a lung cancer? J. Thorac. Dis. 2018, 10, S1157–S1162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dai, C.; Shen, J.; Ren, Y.; Zhong, S.; Zheng, H.; He, J.; Xie, J.H.; Fei, K.; Liang, W.; Jiang, G. Choice of Surgical Procedure for Patients with Non–Small-Cell Lung Cancer ≤1 cm or >1 to 2 cm Among Lobectomy, Segmentectomy, and Wedge Resection: A Population-Based Study. J. Clin. Oncol. 2016, 34, 3175–3182. [Google Scholar] [CrossRef] [PubMed]
- Shiono, S.; Okumura, T.; Boku, N.; Hishida, T.; Ohde, Y.; Sakao, Y.; Yoshiya, K.; Hyodo, I.; Mori, K.; Kondo, H. Outcomes of segmentectomy and wedge resection for pulmonary metastases from colorectal cancer. Eur. J. Cardio Thorac. Surg. 2017, 51, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Sawabata, N.; Kawase, A.; Takahashi, N.; Kawaguchi, T.; Woo, T.; Saito, Y.; Shiono, S.; Matsutani, N.; From The International Lung-Clinical-Study Organization (ILO). Validating margin status in lung wedge resection for clinical stage I non-small cell lung cancer. Surg. Today 2018, 48, 963–967. [Google Scholar] [CrossRef]
- Schuchert, M.J.; Normolle, D.P.; Awais, O.; Pennathur, A.; Wilson, D.O.; Luketich, J.D.; Landreneaua, R.J. Factors influencing recurrence following anatomic lung resection for clinical stage I non-small cell lung cancer. Lung Cancer Amst. Neth. 2019, 128, 145–151. [Google Scholar] [CrossRef]
- Sato, M.; Kobayashi, M.; Kojima, F.; Tanaka, F.; Yanagiya, M.; Kosaka, S.; Ryuta, F.; Nakajima, J. Effect of virtual-assisted lung mapping in acquisition of surgical margins in sublobar lung resection. J. Thorac. Cardiovasc. Surg. 2018, 156, 1691–1701.e5. [Google Scholar] [CrossRef] [Green Version]
- S.F.C.T.C.V. Société Française de Chirurgie Thoracique et Cardio-Vasculaire [Internet]. Société Française de Chirurgie Thoracique et Cardio-Vasculaire. Available online: https://www.sfctcv.org (accessed on 10 February 2020).
- Grogan, E.L.; Jones, D.R.; Kozower, B.D.; Simmons, W.D.; Daniel, T.M. Identification of Small Lung Nodules: Technique of Radiotracer-Guided Thoracoscopic Biopsy. Ann. Thorac. Surg. 2008, 85, S772–S777. [Google Scholar] [CrossRef]
- Chen, S.; Zhou, J.; Zhang, J.; Hu, H.; Luo, X.; Zhang, Y.; Chen, H. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg. Endosc. 2011, 25, 1723–1729. [Google Scholar] [CrossRef]
- Sancheti, M.S.; Lee, R.; Ahmed, S.U.; Pickens, A.; Fernandez, F.G.; Small, W.C.; Nour, S.G.; Force, S.D. Percutaneous fiducial localization for thoracoscopic wedge resection of small pulmonary nodules. Ann. Thorac. Surg. 2014, 97, 1914–1918, discussion 1919. [Google Scholar] [CrossRef]
- Matsumoto, S.; Hirata, T.; Ogawa, E.; Fukuse, T.; Ueda, H.; Koyama, T.; Nakamura, T.; Wada, H. Ultrasonographic evaluation of small nodules in the peripheral lung during video-assisted thoracic surgery (VATS). Eur. J. Cardio Thorac. Surg. 2004, 26, 469–473. [Google Scholar] [CrossRef] [Green Version]
- Wicky, S.; Mayor, B.; Cuttat, J.F.; Schnyder, P. CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. Chest 1994, 106, 1326–1328. [Google Scholar] [CrossRef]
- Watanabe, K.I.; Nomori, H.; Ohtsuka, T.; Kaji, M.; Naruke, T.; Suemasu, K. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: Experience with 174 nodules. J. Thorac. Cardiovasc. Surg. 2006, 132, 320–324. [Google Scholar] [CrossRef] [Green Version]
- Yanagiya, M.; Kawahara, T.; Ueda, K.; Yoshida, D.; Yamaguchi, H.; Sato, M. A meta-analysis of preoperative bronchoscopic marking for pulmonary nodules. Eur. J. Cardio Thorac. Surg. 2020, 58, 40–50. [Google Scholar] [CrossRef]
- Sharma, A.; McDermott, S.; Mathisen, D.J.; Shepard, J.A.O. Preoperative Localization of Lung Nodules with Fiducial Markers: Feasibility and Technical Considerations. Ann. Thorac. Surg. 2017, 103, 1114–1120. [Google Scholar] [CrossRef] [Green Version]
- Finley, R.J.; Mayo, J.R.; Grant, K.; Clifton, J.C.; English, J.; Leo, J.; Lam, S. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: A prospective randomized controlled trial. J. Thorac. Cardiovasc. Surg. 2015, 149, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Sakamoto, T.; Takada, Y.; Endoh, M.; Matsuoka, H.; Tsubota, N. Bronchoscopic dye injection for localization of small pulmonary nodules in thoracoscopic surgery. Ann. Thorac. Surg. 2001, 72, 296–297. [Google Scholar] [CrossRef]
- Krimsky, W.S.; Minnich, D.J.; Cattaneo, S.M.; Sarkar, S.A.; Harley, D.P.; Finley, D.J.; Browning, R.F.; Parrish, S.C. Thoracoscopic detection of occult indeterminate pulmonary nodules using bronchoscopic pleural dye marking. J. Community Hosp. Intern. Med. Perspect. 2014, 4, 23084. [Google Scholar] [CrossRef] [Green Version]
- Vandoni, R.E.; Cuttat, J.F.; Wicky, S.; Suter, M. CT-guided methylene-blue labelling before thoracoscopic resection of pulmonary nodules. Eur. J. Cardio Thorac. Surg. 1998, 14, 265–270. [Google Scholar] [CrossRef] [Green Version]
- Anayama, T.; Qiu, J.; Chan, H.; Nakajima, T.; Weersink, R.; Daly, M.; McConnell, J.; Waddell, T.; Keshavjee, S.; Jaffray, D. Localization of pulmonary nodules using navigation bronchoscope and a near-infrared fluorescence thoracoscope. Ann. Thorac. Surg. 2015, 99, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Misaki, N.; Chang, S.S.; Gotoh, M.; Yamamoto, Y.; Satoh, K.; Yokomise, H. A novel method for determining adjacent lung segments with infrared thoracoscopy. J. Thorac. Cardiovasc. Surg. 2009, 138, 613–618. [Google Scholar] [CrossRef] [Green Version]
- Okusanya, O.T.; Holt, D.; Heitjan, D.; Deshpande, C.; Venegas, O.; Jiang, J.; Judy, R.; de Jesus, E.; Madajewski, B.; Oh, K. Intraoperative Near-Infrared Imaging Can Identify Pulmonary Nodules. Ann. Thorac. Surg. 2014, 98, 1223–1230. [Google Scholar] [CrossRef] [Green Version]
- Schwarz, Y.; Greif, J.; Becker, H.D.; Ernst, A.; Mehta, A. Real-time electromagnetic navigation bronchoscopy to peripheral lung lesions using overlaid CT images: The first human study. Chest 2006, 129, 988–994. [Google Scholar] [CrossRef]
- Khandhar, S.J.; Bowling, M.R.; Flandes, J.; Gildea, T.R.; Hood, K.L.; Krimsky, W.S.; Minnich, D.J.; Murgu, S.D.; Pritchett, M.; Toloza, E.M. Electromagnetic navigation bronchoscopy to access lung lesions in 1,000 subjects: First results of the prospective, multicenter NAVIGATE study. BMC Pulm. Med. 2017, 17, 59. [Google Scholar] [CrossRef]
- Folch, E.E.; Pritchett, M.A.; Nead, M.A.; Bowling, M.R.; Murgu, S.D.; Krimsky, W.S.; Murillo, B.A.; LeMense, G.P.; Minnich, D.J.; Bansal, S.; et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J. Thorac. Oncol. 2019, 14, 445–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folch, E.E.; Bowling, M.R.; Pritchett, M.A.; Murgu, S.D.; Nead, M.A.; Flandes, J.; Krimsky, W.S.; Mahajan, A.K.; LeMense, G.P.; Murillo, B.A.; et al. NAVIGATE 24-Month Results: Electromagnetic Navigation Bronchoscopy for Pulmonary Lesions at 37 Centers in Europe and the United States. J. Thorac. Oncol. 2022, 17, 519–531. [Google Scholar] [CrossRef] [PubMed]
- Bowling, M.R.; Folch, E.E.; Khandhar, S.J.; Arenberg, D.A.; Awais, O.; Minnich, D.J.; Rickman, O.B.; Sztejman, E.; Anciano, C.J. Pleural dye marking of lung nodules by electromagnetic navigation bronchoscopy. Clin. Respir. J. 2019, 13, 700–707. [Google Scholar] [CrossRef]
- Sato, M.; Omasa, M.; Chen, F.; Sato, T.; Sonobe, M.; Bando, T.; Date, H. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J. Thorac. Cardiovasc. Surg. 2014, 147, 1813–1819. [Google Scholar] [CrossRef] [Green Version]
- Sato, M.; Nagayama, K.; Kuwano, H.; Nitadori, J.I.; Anraku, M.; Nakajima, J. Role of post-mapping computed tomography in virtual-assisted lung mapping. Asian Cardiovasc. Thorac. Ann. 2017, 25, 123–130. [Google Scholar] [CrossRef]
- Sato, M.; Shinohara, Y.; Yanagiya, M.; Karasaki, T.; Kitano, K.; Nagayama, K.; Nakajima, J. Use of electromagnetic navigation bronchoscopy in virtual-assisted lung mapping: The effect of on-site adjustment. Gen. Thorac. Cardiovasc. Surg. 2019, 67, 1062–1069. [Google Scholar] [CrossRef]
- Sato, M. Precise sublobar lung resection for small pulmonary nodules: Localization and beyond. Gen. Thorac. Cardiovasc. Surg. 2020, 68, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Uemura, Y.; Sato, M. Protocol for the VAL-MAP 2.0 trial: A multicentre, single-arm, phase III trial to evaluate the effectiveness of virtual-assisted lung mapping by bronchoscopic dye injection and microcoil implementation in patients with small pulmonary nodules in Japan. BMJ Open 2019, 9, e028018. Available online: https://bmjopen.bmj.com/content/9/9/e028018 (accessed on 10 February 2020). [CrossRef] [PubMed] [Green Version]
- Yamaguchi, H.; Sato, M.; Yamamoto, K.; Ueda, K.; Date, H.; Chen-Yoshikawa, T.; Yamada, Y.; Tokuno, J.; Yanagiya, M.; Kojima, F.; et al. Virtual-assisted lung mapping in sublobar resection of small pulmonary nodules, long-term results. Eur. J. Cardio Thorac. Surg. 2022, 61, 761–768. [Google Scholar] [CrossRef]
- Lachkar, S.; Baste, J.M.; Thiberville, L.; Peillon, C.; Rinieri, P.; Piton, N.; Guisier, F.; Salaun, M. Pleural Dye Marking Using Radial Endobronchial Ultrasound and Virtual Bronchoscopy before Sublobar Pulmonary Resection for Small Peripheral Nodules. Respir. Int. Rev. Thorac. Dis. 2018, 95, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.C.; Gillespie, C.T. Robotic Endoscopic Airway Challenge: REACH Assessment. Ann. Thorac. Surg. 2018, 106, 293–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yarmus, L.; Hospital, F.J.H.; Wahidi, M.; Lee, H.; Chen, A.; Molena, D.; Yu, D.; Akulian, J.; Maldonado, F.; Vachani, A. The Precision-1 Study: A Prospective Single-Blinded Randomized Comparative Study of Three Guided Bronchoscopic Approaches for Investigating Pulmonary Nodules. Chest 2019, 156, A2256–A2257. [Google Scholar] [CrossRef]

| Dye Marking Accuracy | Requirements | In Clinical Practice | Limitations | Cost | |
|---|---|---|---|---|---|
| Virtual bronchoscopy combined with Radial-EBUS | (85-96%) depending on the publication. | Chest CT scan (preferably infra millimetric slices). EBUS catheters and virtual bronchoscopy software. | Nodule dye marking can be done at the OR just before surgery | Precision | € * |
| Electromagnetic Navigation Bronchoscopy (ENB) | 91.3% according to the Navigate study | Chest CT scan (preferably infra millimetric slices) ENB navigation system and planning software | Nodule dye marking can be done at the OR just before surgery Requires placing a field generator behind the patient | Cost CT to body divergence | €€ * |
| Virtual assisted lung mapping (VAL-MAP) | 92.6 %(Currently considered to be the most precise method). | Pre interventional CT scan Virtual planning software post interventional CT scan In VALMAP 2.0 ENB navigation system | Dye marking is usually done within 48 h of the surgery.Control by CT scan is required before surgery | Cost Logistics (2 CT scans). Inability to mark the lesion intraoperatively | €€ * |
| Robot-assisted broncho-navigation | Cadaveric small studies show 100% accuracy rate More clinical data are needed to validate this aspect. | - Robotic platform - Special infrastructure at the OR. - Add cone beam CT scan at the OR. | Allows intraoperative nodule marking and biopsies in big OR (To fit surgical robot, bronchoscopy robot and Cone beam CT). | Cost Nodule dye marking and surgery would probably be performed in 2 different OR as it’s hard to fit both robots in one room. | €€€ * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarsam, M.; Baste, J.-M.; Thiberville, L.; Salaun, M.; Lachkar, S. How Bronchoscopic Dye Marking Can Help Minimally Invasive Lung Surgery. J. Clin. Med. 2022, 11, 3246. https://doi.org/10.3390/jcm11113246
Sarsam M, Baste J-M, Thiberville L, Salaun M, Lachkar S. How Bronchoscopic Dye Marking Can Help Minimally Invasive Lung Surgery. Journal of Clinical Medicine. 2022; 11(11):3246. https://doi.org/10.3390/jcm11113246
Chicago/Turabian StyleSarsam, Matthieu, Jean-Marc Baste, Luc Thiberville, Mathieu Salaun, and Samy Lachkar. 2022. "How Bronchoscopic Dye Marking Can Help Minimally Invasive Lung Surgery" Journal of Clinical Medicine 11, no. 11: 3246. https://doi.org/10.3390/jcm11113246
APA StyleSarsam, M., Baste, J.-M., Thiberville, L., Salaun, M., & Lachkar, S. (2022). How Bronchoscopic Dye Marking Can Help Minimally Invasive Lung Surgery. Journal of Clinical Medicine, 11(11), 3246. https://doi.org/10.3390/jcm11113246







