Cell-Derived Exosomes as Therapeutic Strategies and Exosome-Derived microRNAs as Biomarkers for Traumatic Brain Injury
Abstract
:1. Introduction
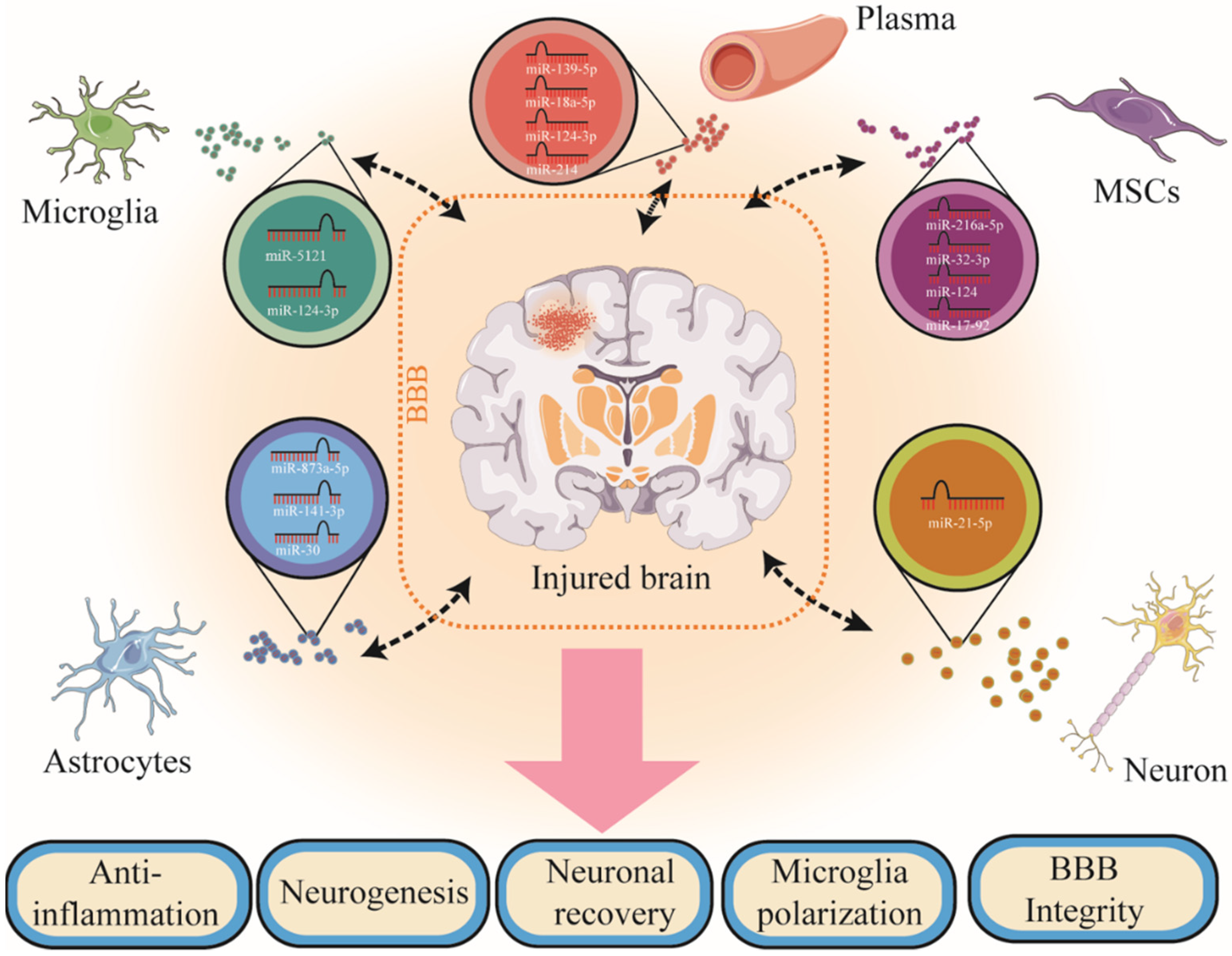
2. Cell-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.1. Microglia-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.2. Astrocyte-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.3. Neuron-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.4. Mesenchymal Stem Cell-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.5. Other Stem Cell-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.6. Humoral Cell-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.7. Other Cell-Derived Exosomes and Exosome-Derived microRNAs in TBI
2.8. Brain-Derived Exosomes and Exosome-Derived microRNAs in TBI
3. Challenges and Opportunities
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Johnson, W.D.; Griswold, D.P. Traumatic brain injury: A global challenge. Lancet Neurol. 2017, 16, 949–950. [Google Scholar] [CrossRef]
- Majdan, M.; Plancikova, D.; Brazinova, A.; Rusnak, M.; Nieboer, D.; Feigin, V.; Maas, A. Epidemiology of traumatic brain injuries in Europe: A cross-sectional analysis. Lancet Public Health 2016, 1, e76–e83. [Google Scholar] [CrossRef]
- Rosenfeld, J.V.; Maas, A.I.; Bragge, P.; Morganti-Kossmann, M.C.; Manley, G.T.; Gruen, R.L. Early management of severe traumatic brain injury. Lancet 2012, 380, 1088–1098. [Google Scholar] [CrossRef]
- Schwulst, S.J.; Trahanas, D.M.; Saber, R.; Perlman, H. Traumatic brain injury-induced alterations in peripheral immunity. J. Trauma Acute Care Surg. 2013, 75, 780–788. [Google Scholar] [CrossRef] [Green Version]
- Levin, H.; Smith, D. Traumatic brain injury: Networks and neuropathology. Lancet Neurol. 2013, 12, 15–16. [Google Scholar] [CrossRef] [Green Version]
- Kalluri, R.; LeBleu, V.S. The biology function and biomedical applications of exosomes. Science 2020, 367, eaau6977. [Google Scholar] [CrossRef]
- Kumar, A.; Stoica, B.A.; Loane, D.J.; Yang, M.; Abulwerdi, G.; Khan, N.; Kumar, A.; Thom, S.R.; Faden, A.I. Microglial-derived microparticles mediate neuroinflammation after traumatic brain injury. J. Neuroinflammation 2017, 14, 47. [Google Scholar] [CrossRef] [Green Version]
- Kalani, A.; Tyagi, A.; Tyagi, N. Exosomes: Mediators of neurodegeneration, neuroprotection and therapeutics. Mol. Neurobiol. 2014, 49, 590–600. [Google Scholar] [CrossRef] [Green Version]
- Budnik, V.; Ruiz-Cañada, C.; Wendler, F. Extracellular vesicles round off communication in the nervous system. Nat. Rev. Neurosci. 2016, 17, 160–172. [Google Scholar] [CrossRef] [Green Version]
- Thompson, A.G.; Gray, E.; Heman-Ackah, S.M.; Mäger, I.; Talbot, K.; Andaloussi, S.E.; Wood, M.J.; Turner, M.R. Extracellular vesicles in neurodegenerative disease-pathogenesis to biomarkers. Nat. Rev. Neurol. 2016, 12, 346–357. [Google Scholar] [CrossRef]
- Horstman, L.L.; Jy, W.; Minagar, A.; Bidot, C.J.; Jimenez, J.J.; Alexander, J.S.; Ahn, Y.S. Cell-derived microparticles and exosomes in neuroinflammatory disorders. Int. Rev. Neurobiol. 2007, 79, 227–268. [Google Scholar] [PubMed]
- Anderson, M.R.; Pleet, M.L.; Enose-Akahata, Y.; Erickson, J.; Monaco, M.C.; Akpamagbo, Y.; Velluci, A.; Tanaka, Y.; Azodi, S.; Lepene, B.; et al. Viral antigens detectable in CSF exosomes from patients with retrovirus associated neurologic disease: Functional role of exosomes. Clin. Transl. Med. 2018, 7, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, T.; Pu, J.; Chen, Y.; Mao, Y.; Guo, Z.; Pan, H.; Zhang, L.; Zhang, H.; Sun, B.; Zhang, B. Plasma Exosomes Spread and Cluster Around β-Amyloid Plaques in an Animal Model of Alzheimer’s Disease. Front. Aging Neurosci. 2017, 9, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yáñez-Mó, M.; Siljander, P.R.M.; Andreu, Z.; Zavec, A.B.; Borràs, F.E.; Buzas, E.I.; Buzas, K.; Casal, E.; Cappello, F.; Carvalho, J.; et al. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 2015, 4, 27066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suryadevara, V.; Govindugari, V. Exosomes and Microparticles: The Nanosized Vesicles Released from the Cells that Act as Biomarkers for Disease and Treatment—Riveting on Lung Diseases. Mater. Today Proc. 2015, 2, 4626–4631. [Google Scholar] [CrossRef]
- Fineberg, S.K.; Kosik, K.S.; Davidson, B.L. MicroRNAs potentiate neural development. Neuron 2009, 64, 303–309. [Google Scholar] [CrossRef] [Green Version]
- Martinez, B.; Peplow, P.V. MicroRNAs as diagnostic markers and therapeutic targets for traumatic brain injury. Neural Regen. Res. 2017, 12, 1749–1761. [Google Scholar] [CrossRef]
- Meissner, L.; Gallozzi, M.; Balbi, M.; Schwarzmaier, S.; Tiedt, S.; Terpolilli, N.A.; Plesnila, N. Temporal Profile of MicroRNA Expression in Contused Cortex after Traumatic Brain Injury in Mice. J. Neurotrauma 2016, 33, 713–720. [Google Scholar] [CrossRef]
- Xavier, A.L.; Menezes, J.R.L.; Goldman, S.A.; Nedergaard, M. Fine-tuning the central nervous system: Microglial modelling of cells and synapses. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130593. [Google Scholar] [CrossRef] [Green Version]
- Tremblay, M.-È.; Stevens, B.; Sierra, A.; Wake, H.; Bessis, A.; Nimmerjahn, A. The role of microglia in the healthy brain. J. Neurosci. 2011, 31, 16064–16069. [Google Scholar] [CrossRef]
- Salter, M.W.; Beggs, S. Sublime microglia: Expanding roles for the guardians of the CNS. Cell 2014, 158, 15–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnoux, I.; Audinat, E. Fractalkine Signaling and Microglia Functions in the Developing Brain. Neural Plast. 2015, 2015, 689404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goetzl, E.J.; Yaffe, K.; Peltz, C.B.; Ledreux, A.; Gorgens, K.; Davidson, B.; Granholm, A.-C.; Mustapic, M.; Kapogiannis, D.; Tweedie, D.; et al. Traumatic brain injury increases plasma astrocyte-derived exosome levels of neurotoxic complement proteins. FASEB J. 2020, 34, 3359–3366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paolicelli, R.C.; Bergamini, G.; Rajendran, L. Cell-to-cell Communication by Extracellular Vesicles: Focus on Microglia. Neuroscience 2019, 405, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Lemaire, Q.; Raffo-Romero, A.; Arab, T.; Van Camp, C.; Drago, F.; Forte, S.; Gimeno, J.-P.; Begard, S.; Colin, M.; Vizioli, J.; et al. Isolation of microglia-derived extracellular vesicles: Towards miRNA signatures and neuroprotection. J. Nanobiotechnol. 2019, 17, 119. [Google Scholar] [CrossRef] [PubMed]
- Raffo-Romero, A.; Arab, T.; Al-Amri, I.S.; Le Marrec-Croq, F.; Van Camp, C.; Lemaire, Q.; Salzet, M.; Vizioli, J.; Sautiere, P.-E.; Lefebvre, C. Medicinal Leech CNS as a Model for Exosome Studies in the Crosstalk between Microglia and Neurons. Int. J. Mol. Sci. 2018, 19, 4124. [Google Scholar] [CrossRef] [Green Version]
- DeLeo, A.M.; Ikezu, T. Extracellular Vesicle Biology in Alzheimer’s Disease and Related Tauopathy. J. Neuroimmune Pharmacol. 2018, 13, 292–308. [Google Scholar] [CrossRef]
- Xia, Y.; Zhang, G.; Han, C.; Ma, K.; Guo, X.; Wan, F.; Kou, L.; Yin, S.; Liu, L.; Huang, J.; et al. Microglia as modulators of exosomal alpha-synuclein transmission. Cell Death Dis. 2019, 10, 174. [Google Scholar] [CrossRef]
- Izzy, S.; Liu, Q.; Fang, Z.; Lule, S.; Wu, L.; Chung, J.Y.; Sarro-Schwartz, A.; Brown-Whalen, A.; Perner, C.; Hickman, S.E.; et al. Time-Dependent Changes in Microglia Transcriptional Networks Following Traumatic Brain Injury. Front. Cell. Neurosci. 2019, 13, 307. [Google Scholar] [CrossRef] [Green Version]
- Madathil, S.K.; Wilfred, B.S.; Urankar, S.E.; Yang, W.; Leung, L.Y.; Gilsdorf, J.S.; Shear, D.A. Early Microglial Activation Following Closed-Head Concussive Injury Is Dominated by Pro-Inflammatory M-1 Type. Front. Neurol. 2018, 9, 964. [Google Scholar] [CrossRef] [Green Version]
- Zhao, C.; Deng, Y.; He, Y.; Huang, X.; Wang, C.; Li, W. Decreased Level of Exosomal miR-5121 Released from Microglia Suppresses Neurite Outgrowth and Synapse Recovery of Neurons Following Traumatic Brain Injury. Neurotherapeutics 2021, 18, 1273–1294. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Guo, M.; Hu, T.; Li, W.; Huang, S.; Yin, Z.; Li, Y.; Chen, F.; Zhu, L.; Kang, C.; et al. Increased Microglial Exosomal miR-124-3p Alleviates Neurodegeneration and Improves Cognitive Outcome after rmTBI. Mol. Ther. 2020, 28, 503–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.; Huang, S.; Yin, Z.; Zhu, J.; Ge, X.; Han, Z.; Tan, J.; Zhang, S.; Zhao, J.; Chen, F.; et al. Increases in miR-124-3p in Microglial Exosomes Confer Neuroprotective Effects by Targeting FIP200-Mediated Neuronal Autophagy Following Traumatic Brain Injury. Neurochem. Res. 2019, 44, 1903–1923. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Ge, X.; Yu, J.; Han, Z.; Yin, Z.; Li, Y.; Chen, F.; Wang, H.; Zhang, J.; Lei, P. Increased miR-124-3p in microglial exosomes following traumatic brain injury inhibits neuronal inflammation and contributes to neurite outgrowth their transfer into neurons. FASEB J. 2018, 32, 512–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, N.J.; Rönnbäck, L.; Hansson, E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat. Rev. Neurosci. 2006, 7, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Dallérac, G.; Zapata, J.; Rouach, N. Versatile control of synaptic circuits by astrocytes: Where, when and how? Nat. Rev. Neurosci. 2018, 19, 729–743. [Google Scholar] [CrossRef]
- Hamilton, N.B.; Attwell, D. Do astrocytes really exocytose neurotransmitters? Nat. Rev. Neurosci. 2010, 11, 227–238. [Google Scholar] [CrossRef]
- Bazargani, N.; Attwell, D. Astrocyte calcium signaling: The third wave. Nat. Neurosci. 2016, 19, 182–189. [Google Scholar] [CrossRef]
- Anderson, M.A.; Ao, Y.; Sofroniew, M.V. Heterogeneity of reactive astrocytes. Neurosci. Lett. 2014, 565, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Hu, G.; Yao, H.; Chaudhuri, A.D.; Duan, M.; Yelamanchili, S.V.; Wen, H.; Cheney, P.D.; Fox, H.S.; Buch, S. Exosome-mediated shuttling of microRNA-29 regulates HIV Tat and morphine-mediated neuronal dysfunction. Cell Death Dis. 2012, 3, e381. [Google Scholar] [CrossRef] [Green Version]
- Upadhya, R.; Zingg, W.; Shetty, S.; Shetty, A.K. Astrocyte-derived extracellular vesicles: Neuroreparative properties and role in the pathogenesis of neurodegenerative disorders. J. Control. Release 2020, 323, 225–239. [Google Scholar] [CrossRef] [PubMed]
- You, Y.; Borgmann, K.; Edara, V.V.; Stacy, S.; Ghorpade, A.; Ikezu, T. Activated human astrocyte-derived extracellular vesicles modulate neuronal uptake, differentiation and firing. J. Extracell. Vesicles 2020, 9, 1706801. [Google Scholar] [CrossRef]
- Taylor, A.R.; Robinson, M.B.; Gifondorwa, D.J.; Tytell, M.; Milligan, C.E. Regulation of heat shock protein 70 release in astrocytes: Role of signaling kinases. Dev. Neurobiol. 2007, 67, 1815–1829. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Cesca, F.; Loers, G.; Schweizer, M.; Buck, F.; Benfenati, F.; Schachner, M.; Kleene, R. Synapsin I is an oligomannose-carrying glycoprotein, acts as an oligomannose-binding lectin, and promotes neurite outgrowth and neuronal survival when released via glia-derived exosomes. J. Neurosci. 2011, 31, 7275–7290. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, R.-D.; Meylan, P.; Decosterd, I. Extracellular microvesicles from astrocytes contain functional glutamate transporters: Regulation by protein kinase C and cell activation. Front. Cell. Neurosci. 2013, 7, 251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Zheng, P.; Hong, T.; Wang, Y.; Liu, N.; He, B.; Zou, S.; Ren, D.; Duan, J.; Zhao, L.; et al. Astrocytes-derived exosomes induce neuronal recovery after traumatic brain injury via delivering gap junction alpha 1–20 k. J. Tissue Eng. Regen. Med. 2020, 14, 412–423. [Google Scholar] [CrossRef]
- Zhang, W.; Hong, J.; Zhang, H.; Zheng, W.; Yang, Y. Astrocyte-derived exosomes protect hippocampal neurons after traumatic brain injury by suppressing mitochondrial oxidative stress and apoptosis. Aging 2021, 13, 21642–21658. [Google Scholar] [CrossRef]
- He, B.; Chen, W.; Zeng, J.; Tong, W.; Zheng, P. Long noncoding RNA NKILA transferred by astrocyte-derived extracellular vesicles protects against neuronal injury by upregulating NLRX1 through binding to mir-195 in traumatic brain injury. Aging 2021, 13, 8127–8145. [Google Scholar] [CrossRef]
- Long, X.; Yao, X.; Jiang, Q.; Yang, Y.; He, X.; Tian, W.; Zhao, K.; Zhang, H. Astrocyte-derived exosomes enriched with miR-873a-5p inhibit neuroinflammation via microglia phenotype modulation after traumatic brain injury. J. Neuroinflammation 2020, 17, 89. [Google Scholar] [CrossRef]
- Wong, J.; Hoe, N.W.; Zhiwei, F.; Ng, I. Apoptosis and traumatic brain injury. Neurocritical Care 2005, 3, 177–182. [Google Scholar] [CrossRef]
- Wang, B.; Han, S. Modified Exosomes Reduce Apoptosis and Ameliorate Neural Deficits Induced by Traumatic Brain Injury. ASAIO J. 2019, 65, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Gayen, M.; Bhomia, M.; Balakathiresan, N.; Knollmann-Ritschel, B. Exosomal MicroRNAs Released by Activated Astrocytes as Potential Neuroinflammatory Biomarkers. Int. J. Mol. Sci. 2020, 21, 2312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winston, C.N.; Romero, H.K.; Ellisman, M.; Nauss, S.; Julovich, D.A.; Conger, T.; Hall, J.R.; Campana, W.; O’Bryant, S.E.; Nievergelt, C.M.; et al. Assessing Neuronal and Astrocyte Derived Exosomes From Individuals With Mild Traumatic Brain Injury for Markers of Neurodegeneration and Cytotoxic Activity. Front. Neurosci. 2019, 13, 1005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mustapic, M.; Eitan, E.; Werner, J.K.; Berkowitz, S.T.; Lazaropoulos, M.P.; Tran, J.; Goetzl, E.J.; Kapogiannis, D. Plasma Extracellular Vesicles Enriched for Neuronal Origin: A Potential Window into Brain Pathologic Processes. Front. Neurosci. 2017, 11, 278. [Google Scholar] [CrossRef] [Green Version]
- Yin, Z.; Han, Z.; Hu, T.; Zhang, S.; Ge, X.; Huang, S.; Wang, L.; Yu, J.; Li, W.; Wang, Y.; et al. Neuron-derived exosomes with high miR-21-5p expression promoted polarization of M1 microglia in culture. Brain Behav. Immun. 2020, 83, 270–282. [Google Scholar] [CrossRef]
- Li, D.; Huang, S.; Zhu, J.; Hu, T.; Han, Z.; Zhang, S.; Zhao, J.; Chen, F.; Lei, P. Exosomes from MiR-21-5p-Increased Neurons Play a Role in Neuroprotection by Suppressing Rab11a-Mediated Neuronal Autophagy In Vitro After Traumatic Brain Injury. Med. Sci. Monit. 2019, 25, 1871–1885. [Google Scholar] [CrossRef]
- Goetzl, L.; Merabova, N.; Darbinian, N.; Martirosyan, D.; Poletto, E.; Fugarolas, K.; Menkiti, O. Diagnostic Potential of Neural Exosome Cargo as Biomarkers for Acute Brain Injury. Ann. Clin. Transl. Neurol. 2018, 5, 4–10. [Google Scholar] [CrossRef] [Green Version]
- Goetzl, E.J.; Peltz, C.B.; Mustapic, M.; Kapogiannis, D.; Yaffe, K. Neuron-Derived Plasma Exosome Proteins after Remote Traumatic Brain Injury. J. Neurotrauma 2020, 37, 382–388. [Google Scholar] [CrossRef]
- Goetzl, E.J.; Elahi, F.M.; Mustapic, M.; Kapogiannis, D.; Pryhoda, M.; Gilmore, A.; Gorgens, K.A.; Davidson, B.; Granholm, A.-C.; Ledreux, A. Altered levels of plasma neuron-derived exosomes and their cargo proteins characterize acute and chronic mild traumatic brain injury. FASEB J. 2019, 33, 5082–5088. [Google Scholar] [CrossRef]
- Shang, F.; Liu, S.; Ming, L.; Tian, R.; Jin, F.; Ding, Y.; Zhang, Y.; Zhang, H.; Deng, Z.; Jin, Y. Human Umbilical Cord MSCs as New Cell Sources for Promoting Periodontal Regeneration in Inflammatory Periodontal Defect. Theranostics 2017, 7, 4370–4382. [Google Scholar] [CrossRef]
- Xie, X.; Wang, Y.; Zhao, C.; Guo, S.; Liu, S.; Jia, W.; Tuan, R.S.; Zhang, C. Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regeneration. Biomaterials 2012, 33, 7008–7018. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Cao, W.; Shi, Y. Plasticity of mesenchymal stem cells in immunomodulation: Pathological and therapeutic implications. Nat. Immunol. 2014, 15, 1009–1016. [Google Scholar] [CrossRef]
- Si, Y.-L.; Zhao, Y.-L.; Hao, H.-J.; Fu, X.-B.; Han, W.-D. MSCs: Biological characteristics, clinical applications and their outstanding concerns. Ageing Res. Rev. 2011, 10, 93–103. [Google Scholar] [CrossRef]
- Chopp, M.; Li, Y. Treatment of neural injury with marrow stromal cells. Lancet Neurol. 2002, 1, 92–100. [Google Scholar] [CrossRef]
- Li, Y.; Chopp, M. Marrow stromal cell transplantation in stroke and traumatic brain injury. Neurosci. Lett. 2009, 456, 120–123. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, A.; Lu, D.; Chopp, M. Intravenous administration of marrow stromal cells (MSCs) increases the expression of growth factors in rat brain after traumatic brain injury. J. Neurotrauma 2004, 21, 33–39. [Google Scholar] [CrossRef]
- Nichols, J.E.; Niles, J.A.; DeWitt, D.; Prough, D.; Parsley, M.; Vega, S.; Cantu, A.; Lee, E.; Cortiella, J. Neurogenic and neuro-protective potential of a novel subpopulation of peripheral blood-derived CD133+ ABCG2+CXCR4+ mesenchymal stem cells: Development of autologous cell-based therapeutics for traumatic brain injury. Stem Cell Res. Ther. 2013, 4, 3. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.X.; Guan, L.X.; Zhang, K.; Zhang, Q.; Dai, L.J. A combined procedure to deliver autologous mesenchymal stromal cells to patients with traumatic brain injury. Cytotherapy 2008, 10, 134–139. [Google Scholar] [CrossRef]
- Cox, C.S.; Baumgartner, J.E.; Harting, M.T.; Worth, L.L.; Walker, P.A.; Shah, S.K.; Ewing-Cobbs, L.; Hasan, K.M.; Day, M.-C.; Lee, D.; et al. Autologous bone marrow mononuclear cell therapy for severe traumatic brain injury in children. Neurosurgery 2011, 68, 588–600. [Google Scholar] [CrossRef]
- Jeong, J.-O.; Han, J.W.; Kim, J.-M.; Cho, H.-J.; Park, C.; Lee, N.; Kim, D.-W.; Yoon, Y.-S. Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ. Res. 2011, 108, 1340–1347. [Google Scholar] [CrossRef] [Green Version]
- Xiong, Y.; Mahmood, A.; Chopp, M. Emerging potential of exosomes for treatment of traumatic brain injury. Neural Regen. Res. 2017, 12, 19–22. [Google Scholar] [CrossRef]
- Nooshabadi, V.T.; Mardpour, S.; Yousefi-Ahmadipour, A.; Allahverdi, A.; Izadpanah, M.; Daneshimehr, F.; Ai, J.; Banafshe, H.R.; Ebrahimi-Barough, S. The extracellular vesicles-derived from mesenchymal stromal cells: A new therapeutic option in regenerative medicine. J. Cell. Biochem. 2018, 119, 8048–8073. [Google Scholar] [CrossRef]
- Zhang, Y.; Chopp, M.; Meng, Y.; Katakowski, M.; Xin, H.; Mahmood, A.; Xiong, Y. Effect of exosomes derived from multipluripotent mesenchymal stromal cells on functional recovery and neurovascular plasticity in rats after traumatic brain injury. J. Neurosurg. 2015, 122, 856–867. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Chopp, M.; Zhang, Z.G.; Katakowski, M.; Xin, H.; Qu, C.; Ali, M.; Mahmood, A.; Xiong, Y. Systemic administration of cell-free exosomes generated by human bone marrow derived mesenchymal stem cells cultured under 2D and 3D conditions improves functional recovery in rats after traumatic brain injury. Neurochem. Int. 2017, 111, 69–81. [Google Scholar] [CrossRef]
- Kim, D.-k.; Nishida, H.; An, S.Y.; Shetty, A.K.; Bartosh, T.J.; Prockop, D.J. Chromatographically isolated CD63+CD81+ extracellular vesicles from mesenchymal stromal cells rescue cognitive impairments after TBI. Proc. Natl. Acad. Sci. USA 2016, 113, 170–175. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Yang, Y.-Y.; Ren, J.-L.; Xu, F.; Chen, F.-M.; Li, A. Exosomes secreted by stem cells from human exfoliated deciduous teeth contribute to functional recovery after traumatic brain injury by shifting microglia M1/M2 polarization in rats. Stem Cell Res. Ther. 2017, 8, 198. [Google Scholar] [CrossRef] [Green Version]
- Xu, H.; Jia, Z.; Ma, K.; Zhang, J.; Dai, C.; Yao, Z.; Deng, W.; Su, J.; Wang, R.; Chen, X. Protective effect of BMSCs-derived exosomes mediated by BDNF on TBI via miR-216a-5p. Med. Sci. Monit. 2020, 26, e920855. [Google Scholar] [CrossRef]
- Xian, P.; Hei, Y.; Wang, R.; Wang, T.; Yang, J.; Li, J.; Di, Z.; Liu, Z.; Baskys, A.; Liu, W.; et al. Mesenchymal stem cell-derived exosomes as a nanotherapeutic agent for amelioration of inflammation-induced astrocyte alterations in mice. Theranostics 2019, 9, 5956–5975. [Google Scholar] [CrossRef]
- Yuan, F.-Y.; Zhang, M.-X.; Shi, Y.-H.; Li, M.-H.; Ou, J.-Y.; Bai, W.-F.; Zhang, M.-S. Bone marrow stromal cells-derived exosomes target DAB2IP to induce microglial cell autophagy, a new strategy for neural stem cell transplantation in brain injury. Exp. Ther. Med. 2020, 20, 2752–2764. [Google Scholar] [CrossRef]
- Ni, H.; Yang, S.; Siaw-Debrah, F.; Hu, J.; Wu, K.; He, Z.; Yang, J.; Pan, S.; Lin, X.; Ye, H.; et al. Exosomes Derived From Bone Mesenchymal Stem Cells Ameliorate Early Inflammatory Responses Following Traumatic Brain Injury. Front. Neurosci. 2019, 13, 14. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Ye, Y.; Kong, C.; Su, X.; Zhang, X.; Bai, W.; He, X. MiR-124 Enriched Exosomes Promoted the M2 Polarization of Microglia and Enhanced Hippocampus Neurogenesis After Traumatic Brain Injury by Inhibiting TLR4 Pathway. Neurochem. Res. 2019, 44, 811–828. [Google Scholar] [CrossRef]
- Chen, Y.; Li, J.; Ma, B.; Li, N.; Wang, S.; Sun, Z.; Xue, C.; Han, Q.; Wei, J.; Zhao, R.C. MSC-derived exosomes promote recovery from traumatic brain injury via microglia/macrophages in rat. Aging 2020, 12, 18274–18296. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.M.; Bhatti, U.F.; Brown, J.F.; Biesterveld, B.E.; Kathawate, R.G.; Graham, N.J.; Chtraklin, K.; Siddiqui, A.Z.; Dekker, S.E.; Andjelkovic, A.; et al. Early single-dose treatment with exosomes provides neuroprotection and improves blood-brain barrier integrity in swine model of traumatic brain injury and hemorrhagic shock. J. Trauma Acute Care Surg. 2020, 88, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.M.; Higgins, G.A.; Bhatti, U.F.; Biesterveld, B.E.; Dekker, S.E.; Kathawate, R.G.; Tian, Y.; Wu, Z.; Kemp, M.T.; Wakam, G.K.; et al. Early treatment with exosomes following traumatic brain injury and hemorrhagic shock in a swine model promotes transcriptional changes associated with neuroprotection. J. Trauma Acute Care Surg. 2020, 89, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.M.; Wu, Z.; Bhatti, U.F.; Biesterveld, B.E.; Kemp, M.T.; Wakam, G.K.; Vercruysse, C.A.; Chtraklin, K.; Siddiqui, A.Z.; Pickell, Z.; et al. Early single-dose exosome treatment improves neurologic outcomes in a 7-day swine model of traumatic brain injury and hemorrhagic shock. J. Trauma Acute Care Surg. 2020, 89, 388–396. [Google Scholar] [CrossRef]
- Williams, A.M.; Dennahy, I.S.; Bhatti, U.F.; Halaweish, I.; Xiong, Y.; Chang, P.; Nikolian, V.C.; Chtraklin, K.; Brown, J.; Zhang, Y.; et al. Mesenchymal Stem Cell-Derived Exosomes Provide Neuroprotection and Improve Long-Term Neurologic Outcomes in a Swine Model of Traumatic Brain Injury and Hemorrhagic Shock. J. Neurotrauma 2019, 36, 54–60. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Chopp, M.; Zhang, Z.G.; Mahmood, A.; Xiong, Y. Mesenchymal Stem Cell-Derived Exosomes Improve Functional Recovery in Rats After Traumatic Brain Injury: A Dose-Response and Therapeutic Window Study. Neurorehabilit. Neural Repair 2020, 34, 616–626. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Chopp, M.; Pang, H.; Zhang, Z.G.; Mahmood, A.; Xiong, Y. MiR-17-92 Cluster-Enriched Exosomes Derived from Human Bone Marrow Mesenchymal Stromal Cells Improve Tissue and Functional Recovery in Rats after Traumatic Brain Injury. J. Neurotrauma 2021, 38, 1535–1550. [Google Scholar] [CrossRef]
- Moss, L.D.; Sode, D.; Patel, R.; Lui, A.; Hudson, C.; Patel, N.A.; Bickford, P.C. Intranasal delivery of exosomes from human adipose derived stem cells at forty-eight hours post injury reduces motor and cognitive impairments following traumatic brain injury. Neurochem. Int. 2021, 150, 105173. [Google Scholar] [CrossRef]
- Patel, N.A.; Moss, L.D.; Lee, J.-Y.; Tajiri, N.; Acosta, S.; Hudson, C.; Parag, S.; Cooper, D.R.; Borlongan, C.V.; Bickford, P.C. Long noncoding RNA MALAT1 in exosomes drives regenerative function and modulates inflammation-linked networks following traumatic brain injury. J. Neuroinflammation 2018, 15, 204. [Google Scholar] [CrossRef] [Green Version]
- Sun, M.K.; Passaro, A.P.; Latchoumane, C.-F.; Spellicy, S.E.; Bowler, M.; Goeden, M.; Martin, W.J.; Holmes, P.V.; Stice, S.L.; Karumbaiah, L. Extracellular Vesicles Mediate Neuroprotection and Functional Recovery after Traumatic Brain Injury. J. Neurotrauma 2020, 37, 1358–1369. [Google Scholar] [CrossRef] [PubMed]
- Rubartelli, A. DAMP-Mediated Activation of NLRP3-Inflammasome in Brain Sterile Inflammation: The Fine Line between Healing and Neurodegeneration. Front. Immunol. 2014, 5, 99. [Google Scholar] [CrossRef] [PubMed]
- Zetterberg, H.; Blennow, K. Fluid biomarkers for mild traumatic brain injury and related conditions. Nat. Rev. Neurol 2016, 12, 563–574. [Google Scholar] [CrossRef] [PubMed]
- Kenney, K.; Qu, B.-X.; Lai, C.; Devoto, C.; Motamedi, V.; Walker, W.C.; Levin, H.S.; Nolen, T.; Wilde, E.A.; Diaz-Arrastia, R.; et al. Higher exosomal phosphorylated tau and total tau among veterans with combat-related repetitive chronic mild traumatic brain injury. Brain Inj. 2018, 32, 1276–1284. [Google Scholar] [CrossRef]
- Gill, J.; Mustapic, M.; Diaz-Arrastia, R.; Lange, R.; Gulyani, S.; Diehl, T.; Motamedi, V.; Osier, N.; Stern, R.A.; Kapogiannis, D. Higher exosomal tau, amyloid-beta 42 and IL-10 are associated with mild TBIs and chronic symptoms in military personnel. Brain Inj. 2018, 32, 1277–1284. [Google Scholar] [CrossRef]
- Peltz, C.B.; Kenney, K.; Gill, J.; Diaz-Arrastia, R.; Gardner, R.C.; Yaffe, K. Blood biomarkers of traumatic brain injury and cognitive impairment in older veterans. Neurology 2020, 95, e1126–e1133. [Google Scholar] [CrossRef]
- Mondello, S.; Guedes, V.A.; Lai, C.; Czeiter, E.; Amrein, K.; Kobeissy, F.; Mechref, Y.; Jeromin, A.; Mithani, S.; Martin, C.; et al. Circulating Brain Injury Exosomal Proteins following Moderate-To-Severe Traumatic Brain Injury: Temporal Profile, Outcome Prediction and Therapy Implications. Cells 2020, 9, 977. [Google Scholar] [CrossRef] [Green Version]
- Moyron, R.B.; Gonda, A.; Selleck, M.J.; Luo-Owen, X.; Catalano, R.D.; O’Callahan, T.; Garberoglio, C.; Turay, D.; Wall, N.R. Differential protein expression in exosomal samples taken from trauma patients. Proteom. Clin. Appl. 2017, 11, 1700061. [Google Scholar] [CrossRef]
- Puffer, R.C.; Cumba Garcia, L.M.; Himes, B.T.; Jung, M.-Y.; Meyer, F.B.; Okonkwo, D.O.; Parney, I.F. Plasma extracellular vesicles as a source of biomarkers in traumatic brain injury. J. Neurosurg. 2020, 134, 1921–1928. [Google Scholar] [CrossRef]
- Vorn, R.; Suarez, M.; White, J.C.; Martin, C.A.; Kim, H.-S.; Lai, C.; Yun, S.-J.; Gill, J.M.; Lee, H. Exosomal microRNA Differential Expression in Plasma of Young Adults with Chronic Mild Traumatic Brain Injury and Healthy Control. Biomedicines 2021, 10, 36. [Google Scholar] [CrossRef]
- Devoto, C.; Lai, C.; Qu, B.-X.; Guedes, V.A.; Leete, J.; Wilde, E.; Walker, W.C.; Diaz-Arrastia, R.; Kenney, K.; Gill, J. Exosomal MicroRNAs in Military Personnel with Mild Traumatic Brain Injury: Preliminary Results from the Chronic Effects of Neurotrauma Consortium Biomarker Discovery Project. J. Neurotrauma 2020, 37, 2482–2492. [Google Scholar] [CrossRef]
- Ghai, V.; Fallen, S.; Baxter, D.; Scherler, K.; Kim, T.-K.; Zhou, Y.; Meabon, J.S.; Logsdon, A.F.; Banks, W.A.; Schindler, A.G.; et al. Alterations in Plasma microRNA and Protein Levels in War Veterans with Chronic Mild Traumatic Brain Injury. J. Neurotrauma 2020, 37, 1418–1430. [Google Scholar] [CrossRef] [PubMed]
- Guedes, V.A.; Lai, C.; Devoto, C.; Edwards, K.A.; Mithani, S.; Sass, D.; Vorn, R.; Qu, B.-X.; Rusch, H.L.; Martin, C.A.; et al. Extracellular Vesicle Proteins and MicroRNAs Are Linked to Chronic Post-Traumatic Stress Disorder Symptoms in Service Members and Veterans With Mild Traumatic Brain Injury. Front. Pharmacol. 2021, 12, 745348. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Ma, H.; Zhang, Y.; Zeng, R.; Yu, J.; Liu, R.; Jin, X.; Zhao, Y. Plasma Exosome-derived MicroRNAs as Novel Biomarkers of Traumatic Brain Injury in Rats. Int. J. Med. Sci. 2020, 17, 437–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhai, K.; Duan, H.; Wang, W.; Zhao, S.; Khan, G.J.; Wang, M.; Zhang, Y.; Thakur, K.; Fang, X.; Wu, C.; et al. Ginsenoside Rg1 ameliorates blood-brain barrier disruption and traumatic brain injury attenuating macrophages derived exosomes miR-21 release. Acta Pharm. Sin. B 2021, 11, 3493–3507. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Hemphill, M.; Yang, Z.; Sewell, E.; Na, Y.J.; Sandsmark, D.K.; Haber, M.; Fisher, S.A.; Torre, E.A.; Svane, K.C.; et al. Diagnosis of traumatic brain injury using miRNA signatures in nanomagnetically isolated brain-derived extracellular vesicles. Lab Chip 2018, 18, 3617–3630. [Google Scholar] [CrossRef]
- Ko, J.; Hemphill, M.; Yang, Z.; Beard, K.; Sewell, E.; Shallcross, J.; Schweizer, M.; Sandsmark, D.K.; Diaz-Arrastia, R.; Kim, J.; et al. Multi-Dimensional Mapping of Brain-Derived Extracellular Vesicle MicroRNA Biomarker for Traumatic Brain Injury Diagnostics. J. Neurotrauma 2020, 37, 2424–2434. [Google Scholar] [CrossRef]
- Andrews, A.M.; Lutton, E.M.; Merkel, S.F.; Razmpour, R.; Ramirez, S.H. Mechanical Injury Induces Brain Endothelial-Derived Microvesicle Release: Implications for Cerebral Vascular Injury during Traumatic Brain Injury. Front. Cell. Neurosci. 2016, 10, 43. [Google Scholar] [CrossRef] [Green Version]
- Gao, W.; Li, F.; Liu, L.; Xu, X.; Zhang, B.; Wu, Y.; Yin, D.; Zhou, S.; Sun, D.; Huang, Y.; et al. Endothelial colony-forming cell-derived exosomes restore blood-brain barrier continuity in mice subjected to traumatic brain injury. Exp. Neurol 2018, 307, 99–108. [Google Scholar] [CrossRef]
- Manek, R.; Moghieb, A.; Yang, Z.; Kumar, D.; Kobessiy, F.; Sarkis, G.A.; Raghavan, V.; Wang, K.K.W. Protein Biomarkers and Neuroproteomics Characterization of Microvesicles/Exosomes from Human Cerebrospinal Fluid Following Traumatic Brain Injury. Mol. Neurobiol. 2018, 55, 6112–6128. [Google Scholar] [CrossRef]
- Muraoka, S.; Jedrychowski, M.P.; Tatebe, H.; DeLeo, A.M.; Ikezu, S.; Tokuda, T.; Gygi, S.P.; Stern, R.A.; Ikezu, T. Proteomic Profiling of Extracellular Vesicles Isolated From Cerebrospinal Fluid of Former National Football League Players at Risk for Chronic Traumatic Encephalopathy. Front. Neurosci. 2019, 13, 1059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuharić, J.; Grabušić, K.; Tokmadžić, V.S.; Štifter, S.; Tulić, K.; Shevchuk, O.; Lučin, P.; Šustić, A. Severe Traumatic Brain Injury Induces Early Changes in the Physical Properties and Protein Composition of Intracranial Extracellular Vesicles. J. Neurotrauma 2019, 36, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.; Lei, Q.; Ma, J.; Gao, S.; Ju, R. Endothelial Progenitor Cell-Derived Microvesicles Promote Angiogenesis in Rat Brain Microvascular Endothelial Cells. Front. Cell. Neurosci. 2021, 15, 638351. [Google Scholar] [CrossRef] [PubMed]
- Kox, M.; Vaneker, M.; van der Hoeven, J.G.; Scheffer, G.-J.; Hoedemaekers, C.W.; Pickkers, P. Effects of vagus nerve stimulation and vagotomy on systemic and pulmonary inflammation in a two-hit model in rats. PLoS ONE 2012, 7, e34431. [Google Scholar] [CrossRef]
- Anthony, D.C.; Couch, Y. The systemic response to CNS injury. Exp. Neurol. 2014, 258, 105–111. [Google Scholar] [CrossRef]
- Hazelton, I.; Yates, A.; Dale, A.; Roodselaar, J.; Akbar, N.; Ruitenberg, M.J.; Anthony, D.C.; Couch, Y. Exacerbation of Acute Traumatic Brain Injury by Circulating Extracellular Vesicles. J. Neurotrauma 2018, 35, 639–651. [Google Scholar] [CrossRef]
- Gonzalez-Begne, M.; Lu, B.; Han, X.; Hagen, F.K.; Hand, A.R.; Melvin, J.E.; Yates, J.R. Proteomic analysis of human parotid gland exosomes by multidimensional protein identification technology (MudPIT). J. Proteome Res. 2009, 8, 1304–1314. [Google Scholar] [CrossRef] [Green Version]
- Kapsogeorgou, E.K.; Abu-Helu, R.F.; Moutsopoulos, H.M.; Manoussakis, M.N. Salivary gland epithelial cell exosomes: A source of autoantigenic ribonucleoproteins. Arthritis Rheum. 2005, 52, 1517–1521. [Google Scholar] [CrossRef]
- Cheng, Y.; Pereira, M.; Raukar, N.; Reagan, J.L.; Queseneberry, M.; Goldberg, L.; Borgovan, T.; LaFrance, W.C.; Dooner, M.; Deregibus, M.; et al. Potential biomarkers to detect traumatic brain injury by the profiling of salivary extracellular vesicles. J. Cell. Physiol. 2019, 234, 14377–14388. [Google Scholar] [CrossRef] [Green Version]
- Matuk, R.; Pereira, M.; Baird, J.; Dooner, M.; Cheng, Y.; Wen, S.; Rao, S.; Quesenberry, P.; Raukar, N.P. The role of salivary vesicles as a potential inflammatory biomarker to detect traumatic brain injury in mixed martial artists. Sci. Rep. 2021, 11, 8186. [Google Scholar] [CrossRef]
- Singleton, Q.; Vaibhav, K.; Braun, M.; Patel, C.; Khayrullin, A.; Mendhe, B.; Lee, B.R.; Kolhe, R.; Kaiser, H.; Awad, M.E.; et al. Bone Marrow Derived Extracellular Vesicles Activate Osteoclast Differentiation in Traumatic Brain Injury Induced Bone Loss. Cells 2019, 8, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, E.B.; Hochfelder, C.G.; Lamberty, B.G.; Meays, B.M.; Morsey, B.M.; Kelso, M.L.; Fox, H.S.; Yelamanchili, S.V. Traumatic brain injury increases levels of miR-21 in extracellular vesicles: Implications for neuroinflammation. FEBS Open Bio 2016, 6, 835–846. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Guo, Y.; Yang, W.; Chen, L.; Ren, D.; Wu, C.; He, B.; Zheng, P.; Tong, W. Phosphorylation of connexin 43 induced by traumatic brain injury promotes exosome release. J. Neurophysiol. 2018, 119, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.-T.; Zhou, J.; Dong, X.-L.; Bi, C.-W.; Jiang, R.-C.; Dong, J.-F.; Tian, Y.; Yuan, H.-J.; Zhang, J.-N. Circular Ribonucleic Acid Expression Alteration in Exosomes from the Brain Extracellular Space after Traumatic Brain Injury in Mice. J. Neurotrauma 2018, 35, 2056–2066. [Google Scholar] [CrossRef]
- Muraoka, S.; Lin, W.; Takamatsu-Yukawa, K.; Hu, J.; Ikezu, S.; DeTure, M.A.; Dickson, D.W.; Emili, A.; Ikezu, T. Enrichment of Phosphorylated Tau (Thr181) and Functionally Interacting Molecules in Chronic Traumatic Encephalopathy Brain-derived Extracellular Vesicles. Aging Dis. 2021, 12, 1376–1388. [Google Scholar] [CrossRef]
- Wang, B.; Han, S. Exosome-associated tau exacerbates brain functional impairments induced by traumatic brain injury in mice. Mol. Cell. Neurosci. 2018, 88, 158–166. [Google Scholar] [CrossRef]
- Hu, T.; Han, Z.; Xiong, X.; Li, M.; Guo, M.; Yin, Z.; Wang, D.; Cheng, L.; Li, D.; Zhang, S.; et al. Inhibition of Exosome Release Alleviates Cognitive Impairment After Repetitive Mild Traumatic Brain Injury. Front. Cell. Neurosci. 2022, 16, 832140. [Google Scholar] [CrossRef]
- Zhou, Y.; Cai, W.; Zhao, Z.; Hilton, T.; Wang, M.; Yeon, J.; Liu, W.; Zhang, F.; Shi, F.-D.; Wu, X.; et al. Lactadherin promotes microvesicle clearance to prevent coagulopathy and improves survival of severe TBI mice. Blood 2018, 131, 563–572. [Google Scholar] [CrossRef] [Green Version]
- Dong, X.; Liu, W.; Shen, Y.; Houck, K.; Yang, M.; Zhou, Y.; Zhao, Z.; Wu, X.; Blevins, T.; Koehne, A.L.; et al. Anticoagulation targeting membrane-bound anionic phospholipids improves outcomes of traumatic brain injury in mice. Blood 2021, 138, 2714–2726. [Google Scholar] [CrossRef]
- Wang, C.; Börger, V.; Sardari, M.; Murke, F.; Skuljec, J.; Pul, R.; Hagemann, N.; Dzyubenko, E.; Dittrich, R.; Gregorius, J.; et al. Mesenchymal Stromal Cell-Derived Small Extracellular Vesicles Induce Ischemic Neuroprotection by Modulating Leukocytes and Specifically Neutrophils. Stroke 2020, 51, 1825–1834. [Google Scholar] [CrossRef]
- Costa, L.A.; Eiro, N.; Fraile, M.; Gonzalez, L.O.; Saá, J.; Garcia-Portabella, P.; Vega, B.; Schneider, J.; Vizoso, F.J. Functional heterogeneity of mesenchymal stem cells from natural niches to culture conditions: Implications for further clinical uses. Cell. Mol. Life Sci. 2021, 78, 447–467. [Google Scholar] [CrossRef] [PubMed]
- de Almeida Fuzeta, M.; Bernardes, N.; Oliveira, F.D.; Costa, A.C.; Fernandes-Platzgummer, A.; Farinha, J.P.; Rodrigues, C.A.V.; Jung, S.; Tseng, R.-J.; Milligan, W.; et al. Scalable Production of Human Mesenchymal Stromal Cell-Derived Extracellular Vesicles Under Serum-/Xeno-Free Conditions in a Microcarrier-Based Bioreactor Culture System. Front. Cell Dev. Biol. 2020, 8, 553444. [Google Scholar] [CrossRef] [PubMed]
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| MD-Exos | mouse | miR-5121 | RGMa | Promote neurite outgrowth and synapse recovery of neurons; improve motor coordination function | Zhao et al., 2021 [31] |
| MD-Exos | mouse | miR-124-3p | Rela ApoE | Promote neurite outgrowth of neurons; regulate neurodegenerative indicators expression; inhibit Aβ abnormalities; improve cognitive outcome | Ge et al., 2020 [32] |
| MD-Exos | mouse | miR-124-3p | FIP200 | Inhibit neuronal autophagy; reduce neuronal injury | Li et al., 2019 [33] |
| MD-Exos | mouse | miR-124-3p | PDE4B mTOR | Suppress neuronal inflammation; promote neurite outgrowth | Huang et al., 2018 [34] |
| MD-MVs | mouse | miR-155 | -- | Propagate neuroinflammation from the CNS to the circulatory system | Kumar et al., 2017 [7] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| AD-Exos | rat | -- | GJA1-20 k Cx43 | Protect and repair damaged neurons; protect and restore mitochondrial function; down-regulate apoptosis rate | Chen et al., 2020 [46] |
| AD-Exos | rat mouse | -- | Nrf2 HO-1 | Reduce neuronal cell loss and atrophy; protect neuronal oxidative stress and apoptosis; attenuate memory and learning deficits | Zhang et al., 2021 [47] |
| AD-EVs | mouse | -- | NLRX1 NKILA | Suppress neuronal injury and neuronal apoptosis; promote neuronal proliferation; enhance brain recovery | He et al., 2021 [48] |
| Plasma AD-Exos | human | -- | complement C5b-9 TCC C3b, CR1 | Repair injured synapses and damaged neurons; predict the prognosis of patients | Goetzl et al., 2020 [23] |
| AD-Exos | mouse human | miR-873a-5p | NF-κB Erk | Inhibit microglia-mediated neuroinflammation via microglia phenotype modulation; improve neurological deficits | Long et al., 2020 [49] |
| Modified AD-Exos | mouse | -- | Bcl-2 Bax | Suppress apoptosis; ameliorate neurological and functional deficits | Wang et al., 2019 [51] |
| AD-Exos | mouse | miR-141-3p miR-30, et al. | -- | Inhibit neuroinflammation and oxidative stress | Gayen et al., 2020 [52] |
| Plasma AD-Exos | human | -- | Aβ42, p-tau NRGN postsynaptic protein | Discriminate military service personnel with mTBI from those without TBI | Winston et al. 2019 [53] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| ND-Exos | mouse | miR-21-5p | -- | Increase M1 microglia polarization; accelerate neuroinflammation factors release; increase the accumulation of p-tau protein; inhibit the neurite outgrowth; promote the apoptosis of neurons | Yin et al., 2020 [55] |
| ND-Exos | mouse | miR-21-5p | Rab11a | Regulate excessive neuronal autophagy; improve neuronal injury | Li et al., 2019 [56] |
| Plasma ND-Exos | human | -- | SYNPO | Find a promising biomarker in TBI | Goetzl et al., 2018 [57] |
| Plasma ND-Exos | human | -- | claudin-5 annexin VII aquaporin 4 PrPc, p-tau Aβ42, IL-6 | Find promising biomarkers after remote TBI to improve cognitive impairment | Goetzl et al., 2020 [58] |
| Plasma ND-Exos | human | -- | annexin VII claudin aquaporin 4 p-tau, et al. | Find promising biomarkers to characterize acute and chronic mTBI | Goetzl et al., 2019 [59] |
| Plasma ND-Exos | human | -- | Aβ42 p-tau NRGN Postsynaptic protein | Discriminate military service personnel with mTBI from those without TBI | Winston et al., 2019 [53] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| BDNF-rBM- MSCs-Exos | rat | miR-216a-5p | -- | Improve neuronal regeneration, cell migration; inhibit inflammation and apoptosis; improve spatial learning ability and sensorimotor function | Xu et al., 2020 [77] |
| hUC- MSCs-Exos | mouse | -- | Nrf2 NF-κB | Improve inflammatory astrocyte alterations; improve mitochondrial dysfunction; improve learning and memory impairments | Xian et al., 2019 [78] |
| mBM-MSCs-Exos | mouse | miR-32-3p | DAB2IP | Induce microglia autophagy | Yuan et al., 2020 [79] |
| mBM-MSCs-Exos | mouse | -- | Bcl-2 Bax TNF-α | Inhibit early neuroinflammation; modulate microglia/macrophages polarization; reduce the lesion size | Ni et al., 2019 [80] |
| rBM- MSCs-Exos | rat | miR-124 | TLR4 NF-κB | Promote M2 polarization of microglia; promote hippocampal neurogenesis; promote functional recovery | Yang et al., 2019 [81] |
| hAD- MSCs-Exos | rat | -- | NF-κB MAPK | Suppress microglia/macrophages activation; increase neurogenesis; suppress neuroinflammation; reduce neuronal apoptosis | Chen et al. 2020 [82] |
| hBM- MSCs-Exos | swine | -- | GFAP laminin claudin-5 | Attenuate cerebral swelling and lesion size; decrease blood-based cerebral biomarker level; improve BBB integrity | Williams et al. 2020 [83] |
| hBM- MSCs-Exos | swine | -- | BDNF NTRK2 lipocalin 2 HIF1α et al. | RNA sequencing data analysis: improve neuronal development, synaptogenesis, neurogenesis, neuroplasticity, neuroinflammation, and stability of BBB | Williams et al. 2020 [84] |
| hBM- MSCs-Exos | swine | -- | Interleukin NF-κB BAX et al. | Decrease inflammatory markers; decrease apoptotic markers; increase neurotrophic factor and granulocyte-macrophage colony-stimulating factor | Williams et al. 2020 [85] |
| hBM-MSCs -Exos | swine | -- | -- | Improve neurological functions | Williams et al. 2020 [86] |
| hBM- MSCs-EVs | mouse | -- | -- | Suppress neuroinflammation; improve spatial learning and pattern separation deficits | Kim et al., 2016 [75] |
| rBM- MSCs-Exos | rat | -- | -- | Promote neurovascular remodeling; reduce neuroinflammation; improve functional recovery | Zhang et al., 2015 [73] |
| hBM- MSCs-Exos | rat | -- | -- | 2D or 3D cultured hUC-MSCs-Exos could promote neurovascular remodeling; reduce neuroinflammation; improve functional recovery | Zhang et al., 2020 [74] |
| hBM- MSCs-Exos | rat | -- | -- | Explore the range of effective doses and therapeutic window | Zhang et al., 2020 [87] |
| hBM- MSCs-Exos | rat | miR-17-92 | -- | Promote neurovascular remodeling; reduce neuroinflammation; improve functional recovery | Zhang et al., 2021 [88] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| hADSC- Exos | mouse | MALAT1 (a lncRNA) | NRTK3 (TrkC) MAPK | Reduce motor and cognitive impairments; reduce the cortical damage | Moss et al., 2021 [89] |
| hADSC- Exos | rat | MALAT1 (a lncRNA) | -- | Drive regenerative function; modulate inflammation-linked networks; MALAT1 affects mRNA and ncRNA expression | Patel et al., 2018 [90] |
| hADSC- Exos | rat | -- | TNF-α IL-6 | Shift microglia M1/M2 polarization; promote motor functional recovery; decelerate neuroinflammation | Li et al., 2017 [76] |
| heNSC -EVs | rat | -- | VEGF VEGFR2 | Increase endogenous NSCs and their migration; increase VEGF activity; promote recovery of motor function | Sun et al., 2020 [91] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| PCD-Exos | human | -- | p-tau tau | Associate with the loss of consciousness or post-traumatic amnesia; find peripheral-to-central biomarkers | Kenney et al., 2018 [94] |
| PCD-Exos | human | -- | Aβ42 tau IL-10 | Identify biomarkers in plasma and PD-Exos that relate to chronic post-concussive and behavioral symptoms following TBI | Gill et al., 2018 [95] |
| PCD-Exos | human | -- | p-tau TNF-α NFL IL-6 | Determine whether blood-based biomarkers can differentiate older veterans with and without TBI and cognitive impairment | Peltz et al., 2020 [96] |
| PCD-Exos | human | -- | NFL GFAP UCH-L1 | Identify biomarkers in plasma and PD-Exos; PD-Exos NFL/UCH-L1 are sensitive indicators of axonal injury/early mortality, respectively | Mondello et al., 2020 [97] |
| PCD-Exos | human | -- | many | Analyze differential protein expression in PD-Exos samples by mass spectrometry | Moyron et al., 2017 [98] |
| PCD-EVs | human | miR-1-3p miR-143-3p miR-151, et al. | GFAP et al. | Find promising biomarkers and pathways targeting consciousness | Puffer et al., 2020 [99] |
| PBCD-Exos | human | miR-223-3p miR-29b-3p miR-107, et al. | -- | Find promising biomarkers in chronic mild TBI | Vorn et al., 2021 [100] |
| PCD-Exos | human | miR-139-5p miR-18a-5p et al. | TP53 IGF-1 TGF-β, et al. | Find promising biomarkers and pathways associated with pathobiology of chronic symptoms | Devoto et al., 2020 [101] |
| PCD-EVs | human | miR-106a-5p miR-106b-5p et al. | MME et al. | Identify biomarkers and pathways for blast-related chronic mild TBI | Ghai et al., 2020 [102] |
| PCD-EVs | human | miR-139-5p miR-3190-3p et al. | NFL Aβ-42 et al. | Find links between NFL and severity of PTSD symptoms; find links between persistent PTSD symptoms and PD-EVs-miRNAs levels | Guedes et al., 2021 [103] |
| PCD-Exos | rat | miR-106b-5p miR-124-3p et al. | MAPK Rap1 Ras, et al. | Find promising biomarkers and pathways | Wang et al., 2020 [104] |
| PCD-Exos | rat | miR-21 miR-21-5p | Rg1 GFAP NF-κB ZO-1, et al. | Improve cerebrovascular endothelial injury; protect the BBB integrity; restore neural function | Zhai et al., 2021 [105] |
| PBCD-EVs | mouse human | miR-203b-5p miR-203a-3p miR-206, et al. | MAPK PI3K-Akt et al. | Find promising biomarkers and pathways associated with TBI diagnosis | Ko et al., 2019 [106] 2020 [107] |
| hbECFCD- Exos | human | -- | PTEN occludin AKT, ZO-1 | Restore the BBB continuity; Reduce brain edema | Gao et al., 2018 [108] |
| PECD-MVs | mouse | -- | occludin et al. | Improve vascular remodeling; restore the BBB continuity | Andrews et al., 2016 [109] |
| CSFCD-Exos/MVs | human | -- | UCH-L1 GFAP, et al. | Find unique protein contents in CSF-Exos/MVs from severe TBI patients | Manek et al., 2018 [110] |
| CSFCD-EVs | human | -- | MAPT p-tau181 t-tau, et al. | Find potential monitoring biomarkers in TBI players at risk for chronic traumatic encephalopathy | Muraoka et al., 2019 [111] |
| CSFCD-EVs | human | -- | Rab7a Arf6 flotillin-1 | Assessed physical properties of CSF-EVs after severe TBI within 7 days and their proteins associated with neuroregeneration | Kuharic et al., 2019 [112] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| MPD-EVs BVEC-EVs PD-EVs | mouse | -- | -- | Increase CNS/hepatic leukocyte recruitment; exacerbate the CNS injury | Hazelton et al., 2018 [116] |
| SD-EVs | human | -- | CDC2, CSNK1A1 CTSD, et al. | Find potential biomarkers to detect TBI by the profiling of SD-EVs | Cheng et al., 2019 [119] |
| SD-EVs | human | -- | MAPK ALOX5 Rap1, et al. | Find promising inflammatory biomarkers to detect TBI by the profiling of SD-EVs | Matuk et al., 2021 [120] |
| BM-EVs | mouse | -- | NF-κB | Activate osteoclast differentiation; inhibit bone loss and fracture rates | Singleton et al., 2019 [121] |
| Origin | Model Species | Involved miRNAs | Other Molecules | Biological Functions/Findings | Study |
|---|---|---|---|---|---|
| BD-EVs | mouse | miR-21 miR-212 miR-146, et al. | -- | Find promising biomarkers and potential BD-EVs cargoes for TBI | Harrison et al., 2016 [122] |
| BD-Exos | rat | -- | CX43 ERK | Find the biomarkers that promote hippocampal BD-Exos release | Chen et al., 2018 [123] |
| BD-EVs | mouse | miR-883a3p miR-3057-5p miR-6980-3p et al. | cAMP et al. | Find promising circRNA-miRNA network biomarkers and potential signaling pathways after TBI | Zhao et al., 2018 [124] |
| BD-EVs | human | -- | p-tau PLXNA4 SNAP-25 UBA1, et al. | Find potential monitoring biomarkers and functionally interacting molecules in BD-EVs of CTE after TBI | Muraoka et al., 2021 [125] |
| BD-Exos | mouse | -- | tau p-tau | Identify that BD-Exos could exacerbate motor and cognitive impairments | Wang et al., 2018 [126] |
| BD-Exos | mouse | -- | p-tau TLR-4 p-STAT3 | Identify that the inhibition of BD-EV release could alleviate cognitive impairment | Hu et al., 2019 [127] |
| BD-MVs | mouse | -- | lactadherin | Identify that lactadherin could promote BD-MV clearance and improve coagulopathy and the survival of severe TBI | Zhou et al., 2018 [128] |
| BD-EVs | mouse | -- | anionic phospholipids | Identify that anticoagulation targeting membrane-bound anionic phospholipids could improve outcomes of TBI | Dong et al., 2021 [129] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.; Wang, J.; Li, X.; Shu, K. Cell-Derived Exosomes as Therapeutic Strategies and Exosome-Derived microRNAs as Biomarkers for Traumatic Brain Injury. J. Clin. Med. 2022, 11, 3223. https://doi.org/10.3390/jcm11113223
Wang J, Wang J, Li X, Shu K. Cell-Derived Exosomes as Therapeutic Strategies and Exosome-Derived microRNAs as Biomarkers for Traumatic Brain Injury. Journal of Clinical Medicine. 2022; 11(11):3223. https://doi.org/10.3390/jcm11113223
Chicago/Turabian StyleWang, Jing, Junwen Wang, Xinyan Li, and Kai Shu. 2022. "Cell-Derived Exosomes as Therapeutic Strategies and Exosome-Derived microRNAs as Biomarkers for Traumatic Brain Injury" Journal of Clinical Medicine 11, no. 11: 3223. https://doi.org/10.3390/jcm11113223
APA StyleWang, J., Wang, J., Li, X., & Shu, K. (2022). Cell-Derived Exosomes as Therapeutic Strategies and Exosome-Derived microRNAs as Biomarkers for Traumatic Brain Injury. Journal of Clinical Medicine, 11(11), 3223. https://doi.org/10.3390/jcm11113223





