Combined Assessment of the Obstetrical Conjugate and Fetal Birth Weight Predicts Birth Mode Outcome in Vaginally Intended Breech Deliveries of Primiparous Women—A Frabat Study
Abstract
:1. Introduction
2. Materials and Methods
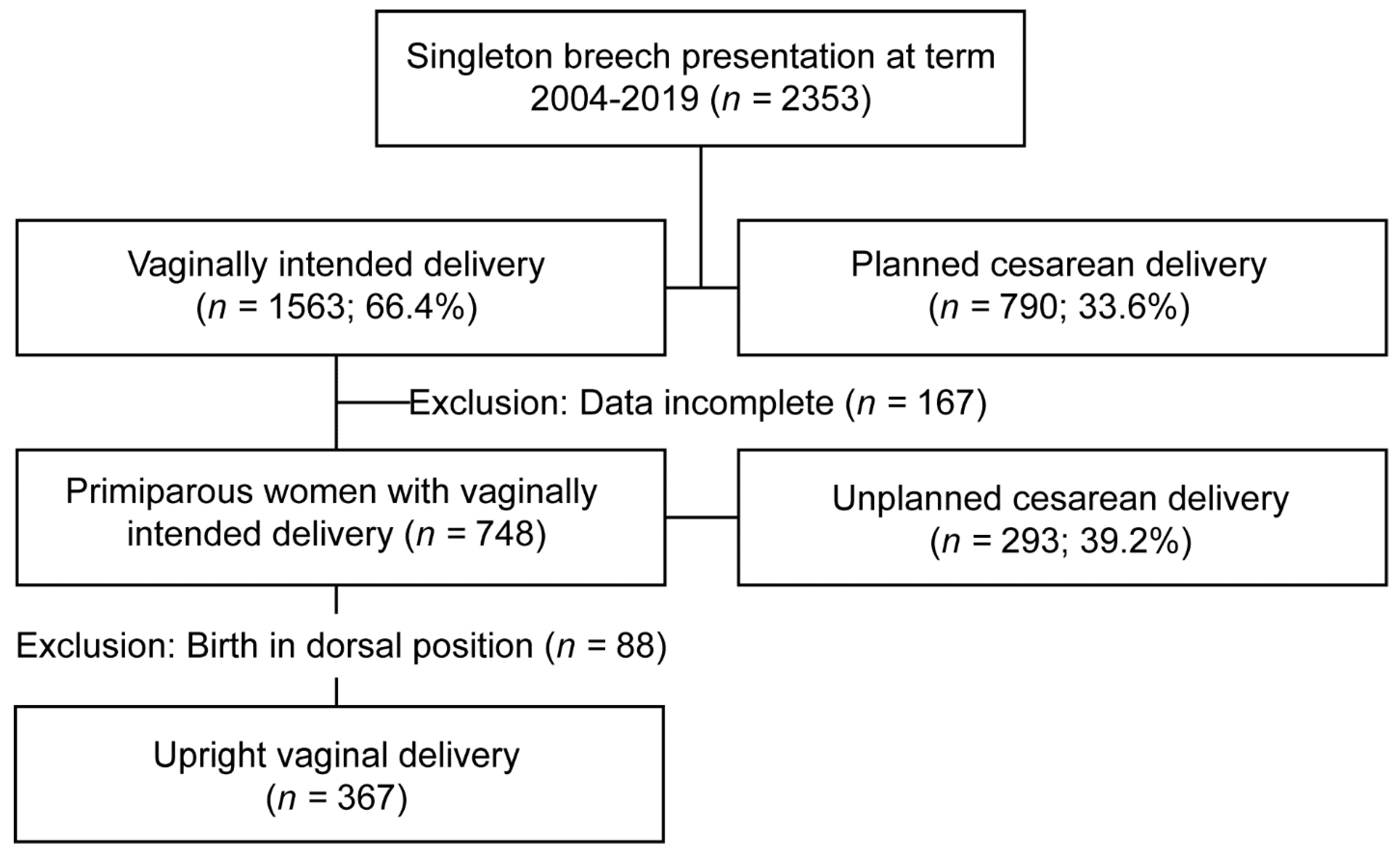
2.1. Patient Cohort and Patient Selection
2.2. Data Collection
2.3. Data Preparation
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Uotila, J.; Tuimala, R.; Kirkinen, P. Good perinatal outcome in selective vaginal breech delivery at term. Acta Obstet. Gynecol. Scand. 2005, 84, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Daviss, B.-A.; Johnson, K.C.; Lalonde, A.B. Evolving evidence since the term breech trial: Canadian response, European dissent, and potential solutions. J. Obstet. Gynaecol. Can. 2010, 32, 217–224. [Google Scholar] [CrossRef]
- Whyte, H.; Hannah, M.E.; Saigal, S.; Hannah, W.J.; Hewson, S.; Amankwah, K.; Cheng, M.; Gafni, A.; Guselle, P.; Helewa, M.; et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: The international randomized Term Breech Trial. Am. J. Obstet. Gynecol. 2004, 191, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Goffinet, F.; Carayol, M.; Foidart, J.M.; Alexander, S.; Uzan, S.; Subtil, D.; Bréart, G.; PREMODA Study Group. Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium. Am. J. Obstet. Gynecol. 2006, 194, 1002–1011. [Google Scholar] [CrossRef] [PubMed]
- Azria, E.; Kayem, G.; Langer, B.; Marchand-Martin, L.; Marret, S.; Fresson, J.; Pierrat, V.; Arnaud, C.; Goffinet, F.; Kaminski, M.; et al. Neonatal mortality and long-term outcome of infants born between 27 and 32 weeks of gestational age in breech presentation: The EPIPAGE cohort study. PLoS ONE 2016, 11, e0145768. [Google Scholar] [CrossRef] [Green Version]
- Louwen, F.; Daviss, B.A.; Johnson, K.C.; Reitter, A. Does breech delivery in an upright position instead of on the back improve outcomes and avoid cesareans? Int. J. Gynecol. Obstet. 2017, 136, 151–161. [Google Scholar] [CrossRef] [Green Version]
- Kotaska, A.; Menticoglou, S.; Gagnon, R.; Farine, D.; Basso, M.; Bos, H.; Delisle, M.F.; Grabowska, K.; Hudon, L.; Mundle, W.; et al. SOGC clinical practice guideline: Vaginal delivery of breech presentation: No. 226, June 2009. Int. J. Gynaecol. Obstet. 2009, 107, 169–176. [Google Scholar] [CrossRef]
- Impey, L.W.; Murphy, D.J.; Griffiths, M.; Penna, L.K.; Adamson, K.; Akaba, G.; Azria, E.; Barrett, J.F.; Bisits, A.; Blum, R.; et al. Management of Breech Presentation: Green-top Guideline No. 20b. BJOG Int. J. Obstet. Gynaecol. 2017, 124, e151–e177. [Google Scholar] [CrossRef]
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). The Management of Breech Presentation at Term. 2013. Available online: https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27sHealth/Statementandguidelines/Clinical-Obstetrics/Management-of-breech-presentation-at-term(-C-Obs-11)-Review-July-2016.pdf?ext=.pdf (accessed on 23 April 2022).
- Jennewein, L.; Kielland-Kaisen, U.; Paul, B.; Möllmann, C.J.; Klemt, A.-S.; Schulze, S.; Bock, N.; Schaarschmidt, W.; Brüggmann, D.; Louwen, F. Maternal and neonatal outcome after vaginal breech delivery at term of children weighing more or less than 3.8 kg: A FRABAT prospective cohort study. PLoS ONE 2018, 13, e0202760. [Google Scholar] [CrossRef] [Green Version]
- Klemt, A.-S.; Schulze, S.; Brüggmann, D.; Louwen, F. MRI-based pelvimetric measurements as predictors for a successful vaginal breech delivery in the Frankfurt Breech at term cohort (FRABAT). Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 232, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, J.; Thomassen, K.; Stumpp, P.; Grothoff, M.; Engel, C.; Kahn, T.; Stepan, H. New MRI criteria for successful vaginal breech delivery in primiparae. PLoS ONE 2016, 11, e0161028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kielland-Kaisen, U.; Paul, B.; Jennewein, L.; Klemt, A.; Möllmann, C.J.; Bock, N.; Schaarschmidt, W.; Brüggmann, D.; Louwen, F. Maternal and neonatal outcome after vaginal breech delivery of nulliparous versus multiparous women of singletons at term—A prospective evaluation of the Frankfurt breech at term cohort (FRABAT). Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 583–587. [Google Scholar] [CrossRef]
- Kielland-Kaisen, U.; Paul, B.; Jennewein, L.; Klemt, A.; Möllmann, C.J.; Bock, N.; Schaarschmidt, W.; Brüggmann, D.; Louwen, F.; FRABAT FRAnkfurt Breech at Term Study Group. Maternal and neonatal outcome after vaginal breech delivery at term after cesarean section—A prospective cohort study of the Frankfurt breech at term cohort (FRABAT). Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 252, 594–598. [Google Scholar]
- Möllmann, C.J.; Kielland-Kaisen, U.; Paul, B.; Schulze, S.; Louwen, F.; Jennewein, L.; Brüggmann, D. Vaginal breech delivery of pregnancy before and after the estimated due date—A FRABAT prospective cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Rozen, G.; Ugoni, A.M.; Sheehan, P.M. A new perspective on VBAC: A retrospective cohort study. Women Birth 2011, 24, 3–9. [Google Scholar] [CrossRef]
- Jennewein, L.; Brueggmann, D.; Fischer, K.; Raimann, F.; Pfeifenberger, H.; Agel, L.; Zander, N.; Eichbaum, C.; Louwen, F. Learning Breech Birth in an Upright Position Is Influenced by Preexisting Experience–A FRABAT Prospective Cohort Study. J. Clin. Med. 2021, 10, 2117. [Google Scholar] [CrossRef] [PubMed]
- Amoa, A.B.; Klufio, C.A.; Wat, S.; Kariwiga, G.; Mathias, A. A retrospective survey of patients with one previous caesarean section delivered at the Port Moresby General Hospital: A comparative study of those delivered vaginally and those delivered by repeat caesarean section. Papua New Guin. Med. J. 1997, 40, 127–135. [Google Scholar]
- Chen, C.; Yang, M.; Zheng, W.; Yang, X.; Chen, Y.; Dong, T.; Lv, M.; Xi, F.; Jiang, Y.; Ying, X.; et al. Magnetic Resonance Imaging-Based Nomogram to Antenatal Predict Cesarean Delivery for Cephalopelvic Disproportion in Primiparous Women. J. Magn. Reson. Imaging 2022. [Google Scholar] [CrossRef]
- Kotaska, A.; Menticoglou, S. No.384—Management of Breech Presentation at Term. J. Obstet. Gynaecol. Can. 2019, 41, 1193–1205. [Google Scholar] [CrossRef] [Green Version]
- Jennewein, L.; Allert, R.; Möllmann, C.J.; Paul, B.; Kielland-Kaisen, U.; Raimann, F.J.; Brüggmann, D.; Louwen, F. The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term—A FRABAT prospective cohort study. PLoS ONE 2019, 14, e0225546. [Google Scholar] [CrossRef]
- Vlemmix, F.; Bergenhenegouwen, L.; Schaaf, J.M.; Ensing, S.; Rosman, A.N.; Ravelli, A.C.; Van Der Post, J.A.; Verhoeven, A.; Visser, G.H.; Mol, B.W.; et al. Term breech deliveries in the Netherlands: Did the increased cesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet. Gynecol. Scand. 2014, 93, 888–896. [Google Scholar] [CrossRef]
- Tsakiridis, I.; Mamopoulos, A.; Athanasiadis, A.; Dagklis, T. Management of Breech Presentation: A Comparison of Four National Evidence-Based Guidelines. Am. J. Perinatol. 2020, 37, 1102–1109. [Google Scholar] [CrossRef]
- Carbillon, L.; Benbara, A.; Tigaizin, A.; Murtada, R.; Fermaut, M.; Belmaghni, F.; Bricou, A.; Boujenah, J. Revisiting the management of term breech presentation: A proposal for overcoming some of the controversies. BMC Pregnancy Childbirth 2020, 20, 263. [Google Scholar] [CrossRef] [PubMed]
- Milner, J.; Arezina, J. The accuracy of ultrasound estimation of fetal weight in comparison to birth weight: A systematic review. Ultrasound 2018, 26, 32–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jennewein, L.; Theissen, S.; Pfeifenberger, H.R.; Zander, N.; Fischer, K.; Eichbaum, C.; Louwen, F. Differences in Biometric Fetal Weight Estimation Accuracy and Doppler Examination Results in Uncomplicated Term Singleton Pregnancies between Vertex and Breech Presentation. J. Clin. Med. 2021, 10, 3252. [Google Scholar] [CrossRef] [PubMed]
- Black, M.; Bhattacharya, S.; Philip, S.; Norman, J.E.; McLernon, D.J. Planned Cesarean Delivery at Term and Adverse Outcomes in Childhood Health. JAMA 2015, 314, 2271. [Google Scholar] [CrossRef] [PubMed]
- NICE. 4-Year Surveillance (2017)—Summary of New Evidence Cesarean Section (2011) NICE Guideline CG132. Available online: https://www.nice.org.uk/guidance/cg132/evidence/appendix-a-summary-of-new-evidence-pdf-2736386032 (accessed on 23 April 2022).

| Characteristic | Lr BW/CVO < 257.8 kg/cm n = 374 | HR BW/CVO ≥ 257.8 kg/cm n = 374 | p Value |
|---|---|---|---|
| Age (mean, standard deviation (SD); year (y)) | 31.4 (±3.8) | 31.2 (±4.1) | 0.795 |
| BMI (mean, SD; kg/m2) | 22.6 (±3.5) | 23.3 (±3.6) | 0.001 |
| Duration of pregnancy (mean, SD; days) | 277 (±8) | 282 (±7) | <0.001 |
| Maternal preconditions | 57 (15.2%) | 43 (11.5%) | 0.133 |
| Birth weight (mean, SD; gram) | 3064.7 (±261) | 3613.1 (±339) | <0.001 |
| Obstetric conjugate (mean, SD; cm) | 13.14 (0.87) | 12.65 (0.82) | <0.001 |
| Cesarean section rate (n, %) | 106 (28.3%) | 188 (50.3%) | <0.001 |
| Epidural anesthesia | 232 (62.0%) | 259 (69.3%) | 0.038 |
| Arterial umbilical chord pH < 7 | 4 (1.08%) | 1 (0.27%) | 0.177 |
| 5 min APGAR < 4 | 2 (0.6%) | 3 (0.4%) | 0.661 |
| NICU > 4 days | 19 (5.1%) | (27 7.2%) | 0.223 |
| Intubation > 24 h | 7 (1.9%) | 3 (0.8%) | 0.203 |
| Neurological deficit | 2 (0.5%) | 2 (0.5%) | >0.99 |
| Birth injury of the newborn | 3 (0.8%) | 4 (1.1%) | 0.704 |
| Newborn Infection | 18 (4.8%) | 26 (7.0%) | 0.214 |
| Congenital illness | 10 (2.7%) | 9 (2.4%) | 0.816 |
| PREMODA Score | 21 (5.6%) | 28 (7.5%) | 0.301 |
| PREMODA Score possibly related to birth mode | 8 (2.1%) | 13 (3.5%) | 0.268 |
| Variable 1 | Variable 2 | r2 | p Value | Inverted Prediction CS-Rate = 0.3 | Inverted Prediction CS Rate = 0.5 |
|---|---|---|---|---|---|
| CS rate | BW/CVO ratio | 0.065 | <0.001 | 240.0 g/cm | 283.8 g/cm |
| CS rate | Birth weight | 0.047 | <0.001 | 3039 g | 3691 g |
| CS rate | CVO | 0.007 | 0.012 | 14.7 cm | 11.0 cm |
| Characteristic | cLR BW/CVO < 257.8 kg/cm n = 106 | cHR BW/CVO ≥ 257.8 kg/cm n = 188 | p Value |
|---|---|---|---|
| Mother’s wish | 5 (4.7%) | 9 (4.8%) | 0.978 |
| Birth arrest in stage I | 38 (35.9%) | 79 (42.2%) | 0.299 |
| Birth arrest in stage II | 32 (30.2%) | 53 (28.2%) | 0.717 |
| Non-reassuring fetal heart rate | 41 (38.7%) | 40 (21.3%) | 0.001 |
| Prolapse of umbilical cord | 4 (3.8%) | 5 (2.7%) | 0.594 |
| Feto-pelvical disproportion | 2 (1.9%) | 17 (9.0%) | 0.017 |
| Suspected amniotic infection | 4 (3.8%) | 3 (1.6%) | 0.240 |
| Characteristic | vLR BW/CVO < 257.8 kg/cm n = 218 | vHR BW/CVO ≥ 257.8 kg/cm n = 148 | p Value |
|---|---|---|---|
| Epidural anesthesia | 124 (56.9%) | 100 (67.6%) | 0.040 |
| Manual assistance required | 91 (41.7%) | 73 (49.3%) | 0.152 |
| Manually assisted head delivery (‘Frank Nudge’) | 84 (38.5%) | 69 (46.6%) | 0.124 |
| Manually assisted arm delivery (‘Louwen maneuver’) | 39 (17.9%) | 37 (25.0%) | 0.100 |
| Duration of Birth (mean, SD; minutes) | 414 (±260) | 557 (±331) | <0.001 |
| PREMODA Score | 7 (3.2%) | 10 (6.8%) | 0.114 |
| PREMODA Score possibly related to birth mode | 2 (0.9%) | 5 (3.4%) | 0.092 |
| Non-perineal injuries (vaginal tear, labial or clitoral tear) | 85 (39.0%) | 67 (45.3%) | 0.232 |
| Perineal injury | 126 (58.6%) | 79 (54.9%) | 0.482 |
| III° and IV° Perineal injury | 4 (1.8%) | 6 (4.1%) | 0.201 |
| Variable 1 | Variable 2 | r2 | p Value |
|---|---|---|---|
| Manual assistance | Birth weight/CVO | 0.0042 | 0.146 |
| Manual assistance | Birth weight | 0.0045 | 0.135 |
| Manual assistance | CVO | 0.0000 | 0.989 |
| Assisted head delivery | Birth weight/CVO | 0.0044 | 0.141 |
| Assisted head delivery | Birth weight | 0.0056 | 0.095 |
| Assisted head delivery | CVO | 0.0002 | 0.766 |
| Assisted arm delivery | Birth weight/CVO | 0.0147 | 0.020 |
| Assisted arm delivery | Birth weight | 0.0215 | 0.005 |
| Assisted arm delivery | CVO | 0.002 | 0.386 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zander, N.; Raimann, F.J.; Al Naimi, A.; Brüggmann, D.; Louwen, F.; Jennewein, L. Combined Assessment of the Obstetrical Conjugate and Fetal Birth Weight Predicts Birth Mode Outcome in Vaginally Intended Breech Deliveries of Primiparous Women—A Frabat Study. J. Clin. Med. 2022, 11, 3201. https://doi.org/10.3390/jcm11113201
Zander N, Raimann FJ, Al Naimi A, Brüggmann D, Louwen F, Jennewein L. Combined Assessment of the Obstetrical Conjugate and Fetal Birth Weight Predicts Birth Mode Outcome in Vaginally Intended Breech Deliveries of Primiparous Women—A Frabat Study. Journal of Clinical Medicine. 2022; 11(11):3201. https://doi.org/10.3390/jcm11113201
Chicago/Turabian StyleZander, Nadja, Florian J. Raimann, Ammar Al Naimi, Dörthe Brüggmann, Frank Louwen, and Lukas Jennewein. 2022. "Combined Assessment of the Obstetrical Conjugate and Fetal Birth Weight Predicts Birth Mode Outcome in Vaginally Intended Breech Deliveries of Primiparous Women—A Frabat Study" Journal of Clinical Medicine 11, no. 11: 3201. https://doi.org/10.3390/jcm11113201
APA StyleZander, N., Raimann, F. J., Al Naimi, A., Brüggmann, D., Louwen, F., & Jennewein, L. (2022). Combined Assessment of the Obstetrical Conjugate and Fetal Birth Weight Predicts Birth Mode Outcome in Vaginally Intended Breech Deliveries of Primiparous Women—A Frabat Study. Journal of Clinical Medicine, 11(11), 3201. https://doi.org/10.3390/jcm11113201






