Visual Outcomes of Pupilloplasty in Ocular Trauma and Iatrogenic Damage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surgical Technique
2.2. Statistical Analysis
3. Results
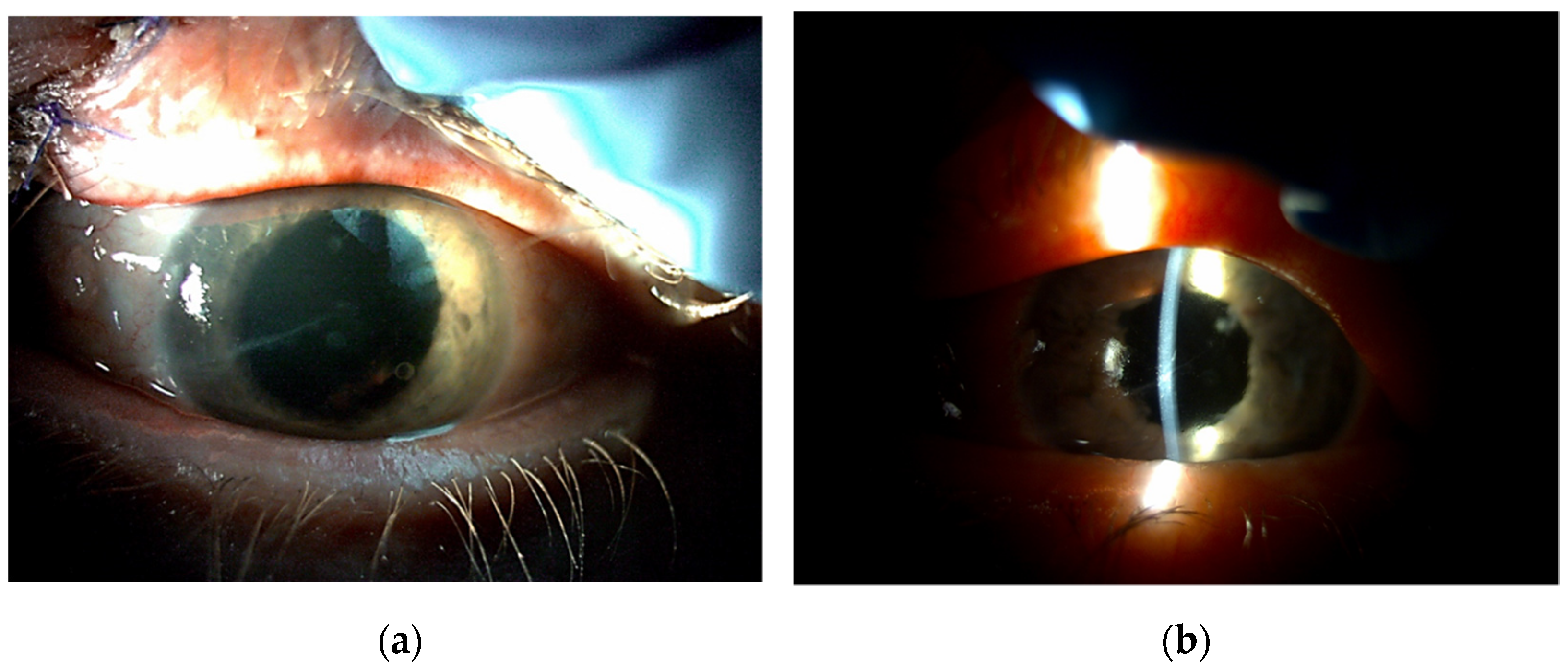
3.1. Iris Damage
3.2. Surgical Technique
3.3. Visual Acuity
3.4. Additional Surgery
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bennett, F.D. Bilateral irydodyalysis with amblyopia and contracted fields due to exploding shrapnel. Br. Med. J. 1915, 2, 848–849. [Google Scholar] [CrossRef] [Green Version]
- Key, B.W. Extensive iridodialysis; operation, reattachment: A report of two cases. Arch. Ophthalmol. 1932, 7, 748–756. [Google Scholar] [CrossRef]
- Tamm, E.R.; Ohlmann, A. Development of the human eye. Ophthalmologe 2012, 109, 911–928. [Google Scholar] [CrossRef] [PubMed]
- Yousif, M.O. Single suture customized loop for large iridodialysis repair. Clin. Ophthalmol. 2016, 10, 1883–1890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, S.; Miller, D.; Atabara, N.A.; Blance, E. A quantitative animal model of traumatic iridodialysis. Acta Ophthalmol. 1990, 68, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Nowomiejska, K.; Haszcz, D.; Onyszkiewicz, M.; Choragiewicz, T.; Czarnek-Chudzik, A.; Szpringer-Wabicz, A.; Baltaziak, K.; Brzozowska, A.; Toro, M.D.; Rejdak, R. Double-Needle Yamane Technique Using Flanged Haptics in Ocular Trauma-A Retrospective Survey of Visual Outcomes and Safety. J. Clin. Med. 2021, 10, 2562. [Google Scholar] [CrossRef]
- Nowomiejska, K.; Choragiewicz, T.; Borowicz, D.; Brzozowska, A.; Moneta-Wielgos, J.; Maciejewski, R.; Jünemann, A.G.; Rejdak, R. Surgical Management of Traumatic Retinal Detachment with Primary Vitrectomy in Adult Patients. J. Ophthalmol. 2017, 2017, 5084319. [Google Scholar] [CrossRef] [Green Version]
- Duke-Elder, S. Textbook of ophthalmology. Br. Med. J. 1950, 1, 650. [Google Scholar] [CrossRef]
- Duke-Elder, S. System of Ophthalmology XIV Part 1: Mechanical Injuries, 1st ed.; Henry Kimpton: London, UK, 1972; pp. 477–649. [Google Scholar]
- Orlin, S.E.; Farber, M.G.; Brucker, A.J.; Frayer, W.C. The unexpected guest: Problem of iris reposition. Surv. Ophthalmol. 1990, 35, 59–66. [Google Scholar] [CrossRef]
- Pallin, S.L. Closed chamber iridoplasty. Ophthalmic Surg. 1981, 12, 213–214. [Google Scholar] [CrossRef]
- Yildirim, T.M.; Khoramnia, R.; Masyk, M.; Son, H.S.; Auffarth, G.U.; Mayer, C.S. Aesthetics of iris reconstruction with a custom-made artificial iris prosthesis. PLoS ONE 2020, 15, e0237616. [Google Scholar]
- Lian, R.R.; Siepser, S.B.; Afshari, N.A. Iris reconstruction suturing techniques. Curr. Opin. Ophthalmol. 2020, 31, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Chorągiewicz, T.; Nowomiejska, K.; Haszcz, D.; Nowakowska, D.; Avitabile, T.; Reibaldi, M.; Jünemann, A.G.M.; Toro, M.D.; Rejdak, R. Transscleral Fixation of Black Diaphragm Intraocular Lens in Complete Aniridia and Aphakia Due to Posttraumatic Eye Rupture: A Pilot Study. J. Clin. Med. 2019, 8, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crawford, A.; Freundlich, S.; Zhang, J.; McGhee, C.N.J. Iris reconstruction: A perspective on the modern surgical armamentarium. Oman J. Ophthalmol. 2021, 14, 69–73. [Google Scholar]
- Siepser, S.B. The closed chamber slipping suture technique for iris repair. Ann. Ophthalmol. 1994, 26, 71–72. [Google Scholar]
- Snyder, M.E.; Lindsell, L.B. Nonappositional repair of iridodialysis. J. Cataract Refract. Surg. 2011, 37, 625–628. [Google Scholar] [CrossRef]
- Narang, P.; Agarwal, A. Single-pass four-throw technique for pupilloplasty. Eur. J. Ophthalmol. 2016, 27, 506–508. [Google Scholar] [CrossRef]
- McCannel, M.A. A retrievable suture idea for anterior uveal problems. Ophthalmic Surg. 1976, 7, 98–103. [Google Scholar] [CrossRef]
- Ogawa, G.S. The iris cerclage suture for permanent mydriasis: A running suture technique. Ophthalmic Surg. Lasers 1998, 29, 1001–1009. [Google Scholar] [CrossRef]
- Lumi, X.; Lumi, A.; Pajic, S.P. Iris cerclage pupilloplasty and IOL implantation for traumatic mydriasis and aphakia after the blunt trauma of the eye. Indian J. Ophthalmol. 2021, 69, 1314–1317. [Google Scholar] [CrossRef]
- Mayer, C.S.; Reznicek, L.; Hoffmann, A.E. Pupillary Reconstruction and Outcome after Artificial Iris Implantation. Ophthalmology 2016, 123, 1011–1018. [Google Scholar] [CrossRef]
- Schulze-Bonsel, K.; Feltgen, N.; Burau, H.; Hansen, L.; Bach, M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1236–1240. [Google Scholar] [CrossRef] [PubMed]
- Behndig, A. Small incision single-suture-loop pupilloplasty for postoperative atonic pupil. J. Cataract Refract. Surg. 1998, 24, 1429–1431. [Google Scholar] [CrossRef]
- Nunziata, B.R. Repair of iridodialysis using a 17-millimeter straight needle. Ophthalmic Surg. 1993, 24, 627–629. [Google Scholar] [CrossRef] [PubMed]
- Stopa, M.; Rakowicz, P. Sutureless Iris Repair: Cauterization Technique. Retina 2015, 35, 2647–2649. [Google Scholar] [CrossRef]
- De Francesco, T.; Ma, J.; Ahmed, I. Endothermal pupilloplasty to optimize pupil centration, size, and contour. J. Cataract. Refract. Surg. 2021, 47, e80–e83. [Google Scholar] [CrossRef]
- Osher, R.H.; Snyder, M.E.; Cionni, R.J. Modification of the Siepser slip-knot technique. J. Cataract Refract. Surg. 2005, 31, 1098–1100. [Google Scholar] [CrossRef]
- Ma, K.T.; Kang, S.Y.; Shin, J.Y.; Kim, N.R.; Seong, G.J.; Kim, C.Y. Modified Siepser sliding knot technique for scleral fixation of subluxated posterior chamber intraocular lens. J. Cataract Refract. Surg. 2010, 36, 6–8. [Google Scholar] [CrossRef]
- Chang, D.F. Siepser slipknot for McCannel iris-suture fixation of subluxated intraocular lenses. J. Cataract Refract. Surg. 2004, 30, 1170–1176. [Google Scholar] [CrossRef]
- Kanclerz, P.; Toto, F.; Grzybowski, A.; Alio, J.L. Extended Depth-of-Field Intraocular Lenses: An Update. Asia Pac. J. Ophthalmol. 2020, 9, 194–202. [Google Scholar] [CrossRef]
- Frisina, R.; Parrozzani, R.; Tozzi, L.; Pilotto, E.; Midena, E. Pupil cerclage technique for treatment of traumatic mydriasis. Eur. J. Ophthalmol. 2020, 30, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, Y.; Yamada, S.; Akimoto, M. Suturing repair of subtotal iridodialysis. Int. Ophthalmol. 2018, 38, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, M.S.; Nessmann, A.; Wagner, J.; Yoeruek, E.; Bartz-Schmidt, K.U.; Szurman, P.; Szurman, G.B. Customized humanoptics silicone iris prosthesis in eyes with posttraumatic iris loss: Outcomes and complications. Acta Ophthalmol. 2016, 94, 301–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundmacher, R.; Reinhard, T.; Althaus, C. Black-diaphragm intraocular lens for correction of aniridia. Ophthalmic Surg. 1994, 25, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.A.; Agarwal, A.; Chandrasekar, R.; Jaganathasamy, N. Iris and knot configuration after Single Pass Four Throw (SFT) pupilloplasty as imaged by the spectral-domain optical coherence tomography. Indian J. Ophthalmol. 2019, 67, 209–212. [Google Scholar] [PubMed]







| Cause of Iris Damage | Type of Iris Damage | Total n (%) | ||
|---|---|---|---|---|
| Mydriasis n (%) | Focal Defect n (%) | Dialysis n (%) | ||
| Trauma | 31 | 17 | 8 | 56 |
| 55.36% | 30.35% | 14.29% | 100.00% | |
| Surgery | 4 | 0 | 10 | 14 |
| 28.57% | 0.00% | 71.43% | 100.00% | |
| Total | 35 | 17 | 18 | 70 |
| 50.00% | 24.29% | 25.71% | 100.00% | |
| Chi2 = 20.08; p = 0.00004 * | ||||
| Type of Surgery | Time Span to Surgery | Mean | Median | Lower Quartile | Upper Quartile | Standard Deviation | Statistical Analysis | |
|---|---|---|---|---|---|---|---|---|
| Z | p | |||||||
| Slip-knot technique n = 60 | before | 1.05 | 0.70 | 0.40 | 1.85 | 0.83 | 4.51 | 0.000007 * |
| after | 0.70 | 0.52 | 0.22 | 1.00 | 0.65 | |||
| Suture to the sclera n = 8 | before | 1.26 | 1.02 | 0.46 | 2.15 | 0.99 | 1.36 | 0.17 |
| after | 0.76 | 0.26 | 0.13 | 1.50 | 0.91 | |||
| Lasso technique n = 4 | before | 0.44 | 0.45 | 0.23 | 0.65 | 0.26 | 0.00 | 1.00 |
| after | 0.36 | 0.30 | 0.23 | 0.50 | 0.24 | |||
| Type of Damage | Time Span to Surgery | Mean | Median | Lower Quartile | Upper Quartile | Standard Deviation | Statistical Analysis | |
|---|---|---|---|---|---|---|---|---|
| Z | p | |||||||
| Mydriasis | before | 0.87 | 0.70 | 0.40 | 1.00 | 0.75 | 3.02 | 0.003 * |
| after | 0.56 | 0.52 | 0.22 | 0.70 | 0.49 | |||
| Focal defect of the iris | before | 1.22 | 0.70 | 0.40 | 2.30 | 0.98 | 2.31 | 0.02 * |
| after | 0.85 | 0.40 | 0.22 | 1.40 | 0.83 | |||
| Dialysis and synechiae | before | 1.12 | 0.82 | 0.40 | 2.00 | 0.83 | 2.55 | 0.01 * |
| after | 0.76 | 0.55 | 0.22 | 1.00 | 0.70 | |||
| Type of Surgery | Time Span to Surgery | Mean | Median | Lower Quartile | Upper Quartile | Standard Deviation | Statistical Analysis | |
|---|---|---|---|---|---|---|---|---|
| Z | p | |||||||
| Corneal suturing | before | 0.93 | 0.70 | 0.52 | 1.00 | 0.82 | 0.73 | 0.47 |
| after | 0.79 | 0.70 | 0.15 | 1.40 | 0.75 | |||
| Cataract removal with IOL implantation | before | 1.12 | 0.70 | 0.40 | 2.00 | 0.89 | 2.40 | 0.02 * |
| after | 0.56 | 0.22 | 0.15 | 1.00 | 0.68 | |||
| Secondary IOL implantation | before | 1.17 | 0.82 | 0.40 | 2.30 | 0.90 | 3.81 | 0.0001 * |
| after | 0.67 | 0.40 | 0.22 | 1.00 | 0.61 | |||
| Anterior vitrectomy | before | 1.08 | 0.70 | 0.40 | 2.00 | 0.84 | 3.10 | 0.002 * |
| after | 0.58 | 0.26 | 0.15 | 0.70 | 0.66 | |||
| Pars plana vitrectomy | before | 1.70 | 2.30 | 0.70 | 2.30 | 0.90 | 2.38 | 0.02 * |
| after | 1.22 | 1.00 | 0.52 | 2.30 | 0.80 | |||
| Yamane scleral fixation | before | 1.25 | 1.00 | 0.52 | 2.30 | 0.91 | 3.14 | 0.002 * |
| after | 0.76 | 0.56 | 0.30 | 1.00 | 0.60 | |||
| Type of Surgery | Time Span to Surgery | Mean | Median | Lower Quartile | Upper Quartile | Standard Deviation | Statistical Analysis | |
|---|---|---|---|---|---|---|---|---|
| Z | p | |||||||
| Pupilloplasty alone | before | 0.58 | 0.52 | 0.40 | 0.70 | 0.20 | 2.34 | 0.02 * |
| after | 0.45 | 0.46 | 0.30 | 0.70 | 0.20 | |||
| Pupilloplasty combined with other surgeries | before | 1.13 | 0.70 | 0.40 | 2.30 | 0.90 | 4.02 | 0.0001 * |
| after | 0.74 | 0.46 | 0.22 | 1.00 | 0.70 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowomiejska, K.; Haszcz, D.; Adamczyk, K.; Brzozowska, A.; Bonfiglio, V.; Toro, M.D.; Rejdak, R. Visual Outcomes of Pupilloplasty in Ocular Trauma and Iatrogenic Damage. J. Clin. Med. 2022, 11, 3177. https://doi.org/10.3390/jcm11113177
Nowomiejska K, Haszcz D, Adamczyk K, Brzozowska A, Bonfiglio V, Toro MD, Rejdak R. Visual Outcomes of Pupilloplasty in Ocular Trauma and Iatrogenic Damage. Journal of Clinical Medicine. 2022; 11(11):3177. https://doi.org/10.3390/jcm11113177
Chicago/Turabian StyleNowomiejska, Katarzyna, Dariusz Haszcz, Katarzyna Adamczyk, Agnieszka Brzozowska, Vincenza Bonfiglio, Mario Damiano Toro, and Robert Rejdak. 2022. "Visual Outcomes of Pupilloplasty in Ocular Trauma and Iatrogenic Damage" Journal of Clinical Medicine 11, no. 11: 3177. https://doi.org/10.3390/jcm11113177
APA StyleNowomiejska, K., Haszcz, D., Adamczyk, K., Brzozowska, A., Bonfiglio, V., Toro, M. D., & Rejdak, R. (2022). Visual Outcomes of Pupilloplasty in Ocular Trauma and Iatrogenic Damage. Journal of Clinical Medicine, 11(11), 3177. https://doi.org/10.3390/jcm11113177









