Urgent Coronary Artery Bypass Grafting Complicated by Systemic Inflammatory Response from Fulminant Herpes Zoster Successfully Managed with Adjunct Extracorporeal Hemoadsorption: A Case Report †
Abstract
:1. Introduction
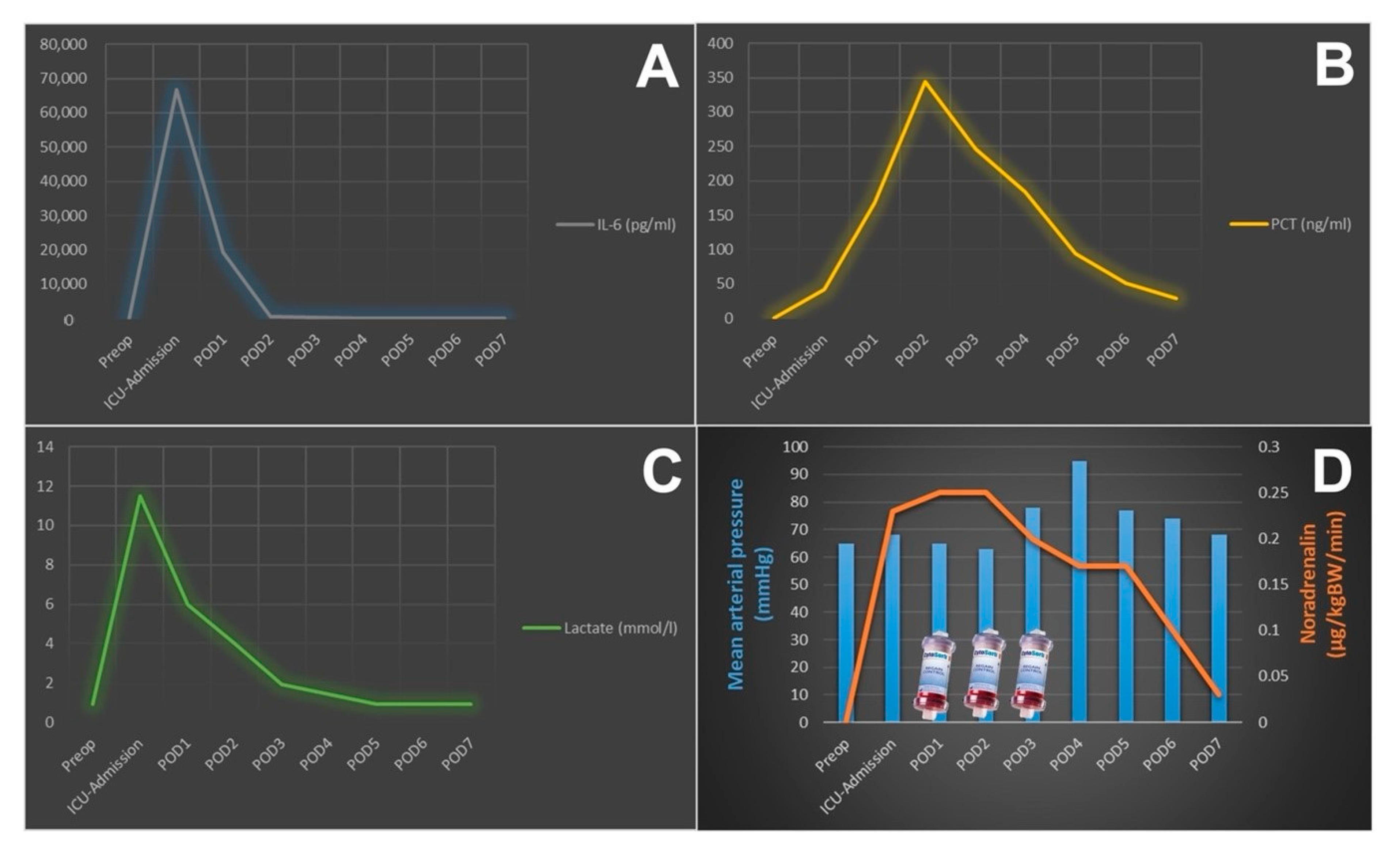
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Boss, K.; Jahn, M.; Wendt, D.; Haidari, Z.; Demircioglu, E.; Thielmann, M.; Ruhparwar, A.; Kribben, A.; Tyczynski, B. Extracorporeal cytokine adsorption: Significant reduction of catecholamine requirement in patients with AKI and septic shock after cardiac surgery. PLoS ONE 2021, 8, e0246299. [Google Scholar] [CrossRef] [PubMed]
- Berlot, G.; Samola, V.; Barbaresco, I.; Tomasini, A.; di Maso, V.; Bianco, F.; Gerini, U. Effects of the timing and intensity of treatment on septic shock patients treated with CytoSorb®: Clinical experience. Int. J. Artif. Organs 2022, 45, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Song, T.; Hayanga, J.; Durham, L.; Garrison, L.; McCarthy, P.; Barksdale, A.; Smith, D.; Bartlett, R.; Jaros, M.; Nelson, P.; et al. CytoSorb Therapy in COVID-19 (CTC) Patients Requiring Extracorporeal Membrane Oxygenation: A Multicenter, Retrospective Registry. Front. Med. 2021, 20, 773461. [Google Scholar] [CrossRef] [PubMed]
- Supady, A.; Weber, E.; Rieder, M.; Lother, A.; Niklaus, T.; Zahn, T.; Frech, F.; Müller, S.; Kuhl, M.; Benk, C.; et al. Cytokine adsorption in patients with severe COVID-19 pneumonia requiring extracorporeal membrane oxygenation (CYCOV): A single centre, open-label, randomised, controlled trial. Lancet Respir. Med. 2021, 9, 755–762. [Google Scholar] [CrossRef]
- Träger, K.; Skrabal, C.; Fischer, G.; Datzmann, T.; Schroeder, J.; Fritzler, D.; Hartmann, J.; Liebold, A.; Reinelt, H. Hemoadsorption treatment of patients with acute infective endocarditis during surgery with cardiopulmonary bypass—A case series. Int. J. Artif. Organs 2017, 40, 240–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernardi, M.H.; Rinoesl, H.; Dragosits, K.; Ristl, R.; Hoffelner, F.; Opfermann, P.; Lamm, C.; Preißing, F.; Wiedemann, D.; Hiesmayr, M.J.; et al. Effect of hemoadsorption during cardiopulmonary bypass surgery—A blinded, randomized, controlled pilot study using a novel adsorbent. Crit. Care 2016, 20, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diab, M.; Lehmann, T.; Bothe, W.; Akhyari, P.; Platzer, S.; Wendt, D.; Deppe, A.C.; Strauch, J.; Hagel, S.; Günther, A.; et al. Cytokine Hemoadsorption During Cardiac Surgery Versus Standard Surgical Care for Infective Endocarditis (REMOVE): Results From a Multicenter Randomized Controlled Trial. Circulation 2022, 145, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Haidari, Z.; Wendt, D.; Thielmann, M.; Mackowiak, M.; Neuhäuser, M.; Jakob, H.; Ruhparwar, A.; El-Gabry, M. Intraoperative Hemoadsorption in Patients With Native Mitral Valve Infective Endocarditis. Ann. Thorac. Surg. 2020, 110, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Kogelmann, K.; Hübner, T.; Schwameis, F.; Drüner, M.; Scheller, M.; Jarczak, D. First Evaluation of a New Dynamic Scoring System Intended to Support Prescription of Adjuvant CytoSorb Hemoadsorption Therapy in Patients with Septic Shock. J. Clin. Med. 2021, 10, 2939. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haidari, Z.; Weißenberger, W.; Tyczynski, B.; Demircioglu, E.; Deliargyris, E.; Christ, M.; Thielmann, M.; El Gabry, M.; Ruhparwar, A.; Wendt, D. Urgent Coronary Artery Bypass Grafting Complicated by Systemic Inflammatory Response from Fulminant Herpes Zoster Successfully Managed with Adjunct Extracorporeal Hemoadsorption: A Case Report. J. Clin. Med. 2022, 11, 3106. https://doi.org/10.3390/jcm11113106
Haidari Z, Weißenberger W, Tyczynski B, Demircioglu E, Deliargyris E, Christ M, Thielmann M, El Gabry M, Ruhparwar A, Wendt D. Urgent Coronary Artery Bypass Grafting Complicated by Systemic Inflammatory Response from Fulminant Herpes Zoster Successfully Managed with Adjunct Extracorporeal Hemoadsorption: A Case Report. Journal of Clinical Medicine. 2022; 11(11):3106. https://doi.org/10.3390/jcm11113106
Chicago/Turabian StyleHaidari, Zaki, Wilko Weißenberger, Bartosz Tyczynski, Ender Demircioglu, Efthymios Deliargyris, Martin Christ, Matthias Thielmann, Mohamed El Gabry, Arjang Ruhparwar, and Daniel Wendt. 2022. "Urgent Coronary Artery Bypass Grafting Complicated by Systemic Inflammatory Response from Fulminant Herpes Zoster Successfully Managed with Adjunct Extracorporeal Hemoadsorption: A Case Report" Journal of Clinical Medicine 11, no. 11: 3106. https://doi.org/10.3390/jcm11113106
APA StyleHaidari, Z., Weißenberger, W., Tyczynski, B., Demircioglu, E., Deliargyris, E., Christ, M., Thielmann, M., El Gabry, M., Ruhparwar, A., & Wendt, D. (2022). Urgent Coronary Artery Bypass Grafting Complicated by Systemic Inflammatory Response from Fulminant Herpes Zoster Successfully Managed with Adjunct Extracorporeal Hemoadsorption: A Case Report. Journal of Clinical Medicine, 11(11), 3106. https://doi.org/10.3390/jcm11113106







