Monthly Follow-Ups of Functional Status in People with COPD: A Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Data Analysis
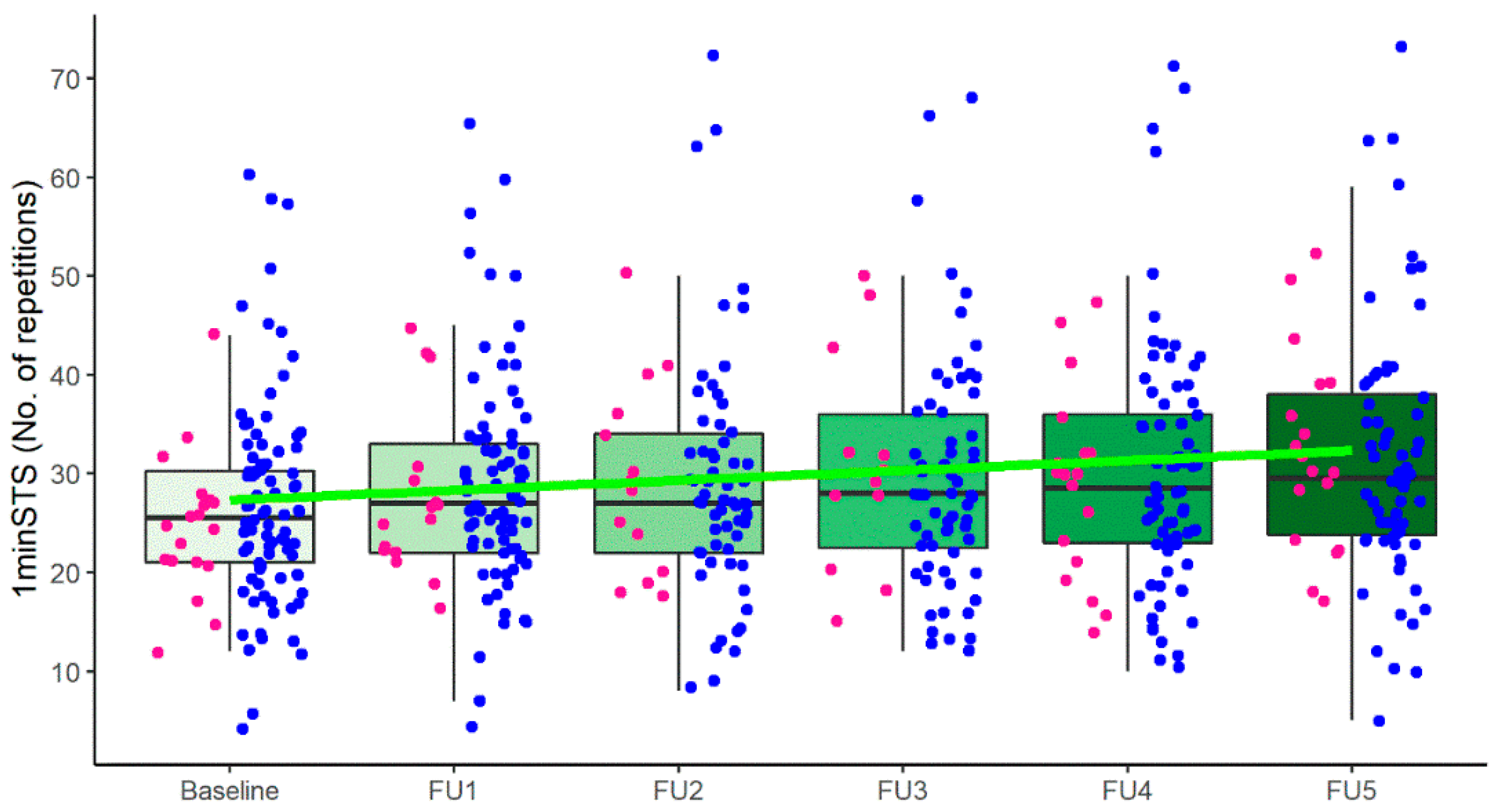
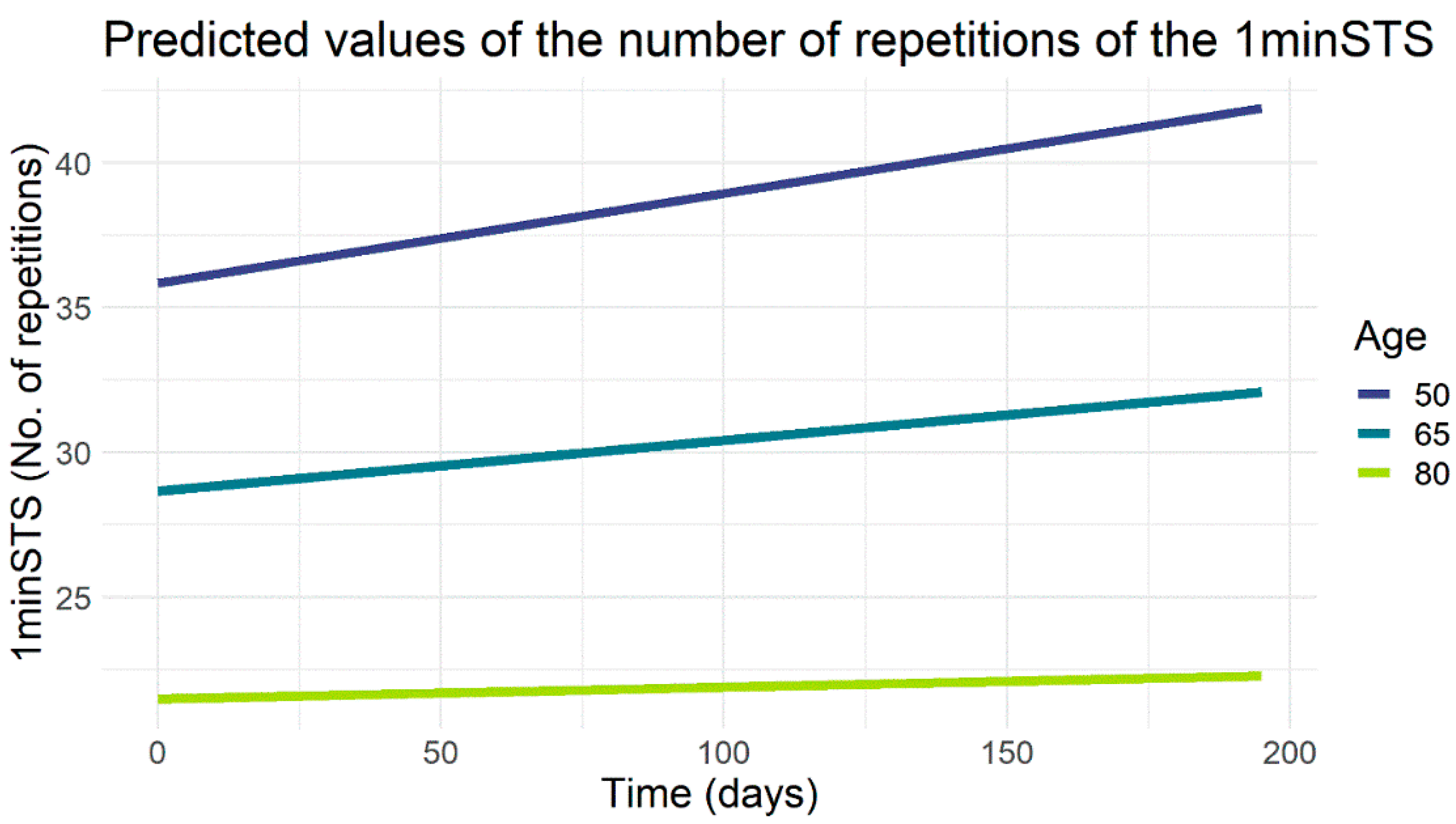
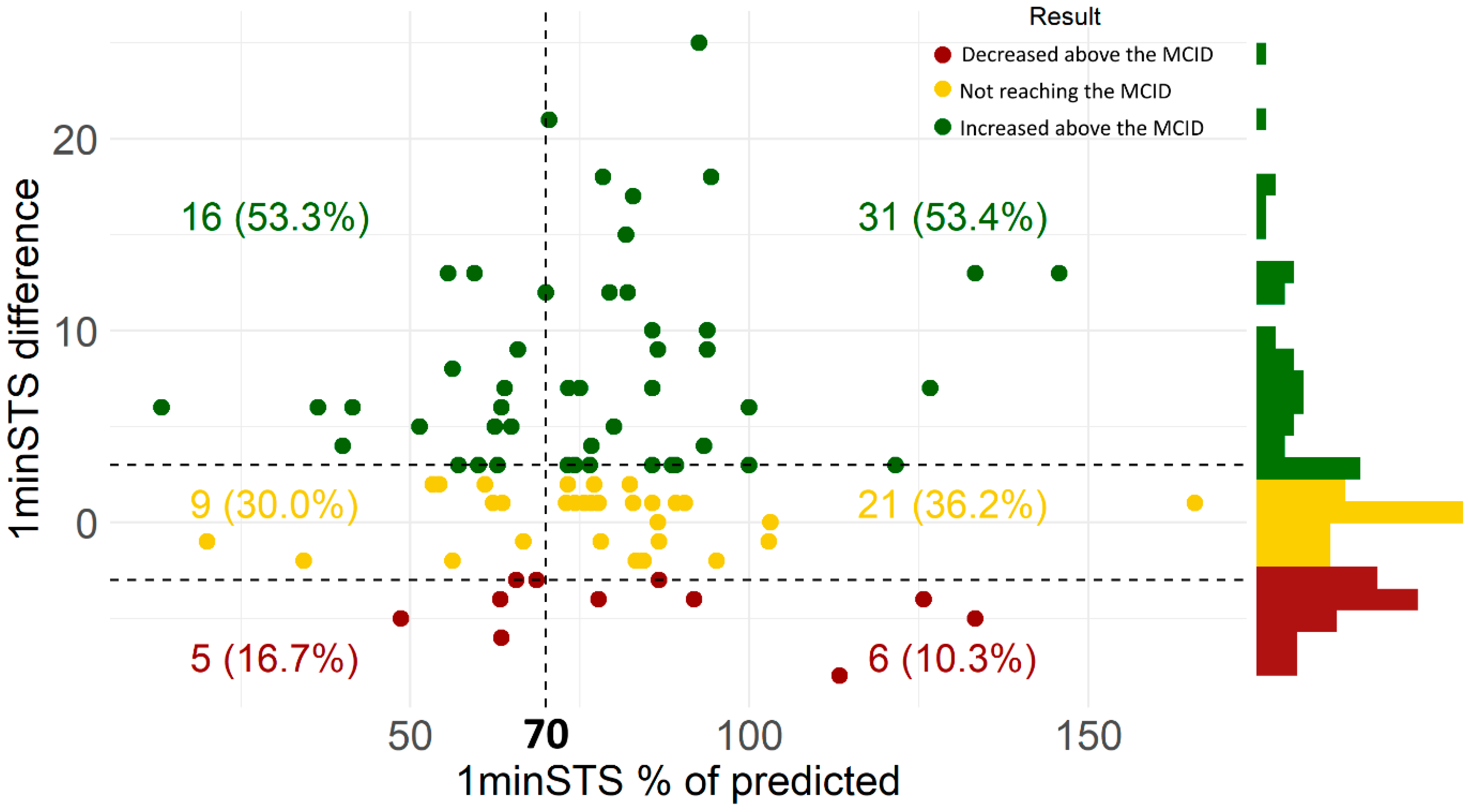
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The WHO Global Estimates from 2000-2019: Chronic Obstructive Pulmonary Disease Key Facts; WHO: Geneve, Switzerland, 2021. [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022 Report). 2022. Available online: https://goldcopd.org/ (accessed on 17 June 2021).
- Wang, T.-J. Concept analysis of functional status. Int. J. Nurs. Stud. 2004, 41, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Antoniu, S.; Boiculese, L.; Prunoiu, V. Frailty, a Dimension of Impaired Functional Status in Advanced COPD: Utility and Clinical Applicability. Medicina 2021, 57, 474. [Google Scholar] [CrossRef] [PubMed]
- Leidy, N.K. Functional status and the forward progress of merry-go-rounds: Toward a coherent analytical framework. Nurs. Res. 1994, 43, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Fan, V.S.; Ramsey, S.D.; Make, B.J.; Martinez, F.J. Physiologic Variables and Functional Status Independently Predict COPD Hospitalizations and Emergency Department Visits in Patients with Severe COPD. COPD J. Chronic Obstr. Pulm. Dis. 2007, 4, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Crook, S.; Frei, A.; Ter Riet, G.; Puhan, M.A. Prediction of long-term clinical outcomes using simple functional exercise performance tests in patients with COPD: A 5-year prospective cohort study. Respir. Res. 2017, 18, 1–4. [Google Scholar] [CrossRef]
- Lareau, S.C.; Blackstock, F.C. Functional status measures for the COPD patient: A practical categorization. Chronic Respir. Dis. 2018, 16, 64. [Google Scholar] [CrossRef] [PubMed]
- Kocks, J.W.H.; Asijee, G.M.; Tsiligianni, I.G.; Kerstjens, H.; Van Der Molen, T. Functional status measurement in COPD: A review of available methods and their feasibility in primary care. Prim. Care Respir. J. 2011, 20, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Li, H.; Ding, N.; Wang, N.; Wen, D. Functional Status Assessment of Patients with COPD: A Systematic Review of Performance-Based Measures and Patient-Reported Measures. Medicine 2016, 95, e3672. [Google Scholar] [CrossRef]
- Souto-Miranda, S.; Rodrigues, G.; Spruit, M.A.; Marques, A. Pulmonary rehabilitation outcomes in individuals with chronic obstructive pulmonary disease: A systematic review. Ann. Phys. Rehabil. Med. 2022, 65, 10564. [Google Scholar] [CrossRef]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Crouch, R. 1-Minute Sit-to-Stand Test: Systematic review of procedures, performance, and clinimetric properties. J. Cardiopulm. Rehabil. Prev. 2019, 39, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, T.; de Bisschop, C.; Beaumont, M.; Ouksel, H.; Jean, V.; Dessables, F.; Chambellan, A. Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 2609–2616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crook, S.; Büsching, G.; Schultz, K.; Lehbert, N.; Jelusic, D.; Keusch, S.; Wittmann, M.; Schuler, M.; Radtke, T.; Frey, M.; et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur. Respir. J. 2017, 49, 1601871. [Google Scholar] [CrossRef] [Green Version]
- Souto-Miranda, S.; Mendes, M.A.; Cravo, J.; Andrade, L.; Spruit, M.A.; Marques, A. Functional Status Following Pulmonary Rehabilitation: Responders and Non-Responders. J. Clin. Med. 2022, 11, 518. [Google Scholar] [CrossRef]
- OECD/Eurostat/UNESCO Institute for Statistics. ISCED 2011 Operational Manual: Guidelines for Classifying National Education Programmes and Related Qualifications; OECD Publishing: Paris, France, 2015. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for Controlling and Monitoring the Tobacco Epidemic WHO Tobacco or Health Programme; WHO: Geneva, Switzerland, 1997. [Google Scholar]
- Doherty, D.E.; Belfer, M.H.; Brunton, S.A.; Fromer, L.; Morris, C.M.; Snader, T.C. Chronic obstructive pulmonary disease: Consensus recommendations for early diagnosis and treatment. J. Fam. Pract. 2006, 55, S1. [Google Scholar]
- Jones, P. Quality of life, symptoms and pulmonary function in asthma: Long-term treatment with nedocromil sodium examined in a controlled multicentre trial. Eur. Respir. J. 1994, 7, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.; Szatrowski, T.P.; Peterson, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Strassmann, A.; Steurer-Stey, C.; Lana, K.D.; Zoller, M.; Turk, A.J.; Suter, P.; Puhan, M.A. Population-based reference values for the 1-min sit-to-stand test. Int. J. Public Health 2013, 58, 949–953. [Google Scholar] [CrossRef] [Green Version]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 48. [Google Scholar] [CrossRef]
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H.B. lmerTest Package: Tests in linear mixed effects models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef] [Green Version]
- Akaike, H. Maximum likelihood identification of Gaussian autoregressive moving average models. Biometrika 1973, 60, 255–265. [Google Scholar] [CrossRef]
- Nakagawa, S.; Johnson, P.C.D.; Schielzeth, H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J. R. Soc. Interface 2017, 14, 20170213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinheiro, J.; Bates, D.; R-core. Linear and Nonlinear Mixed-Effects Models; 1998; Available online: https://newprairiepress.org/cgi/viewcontent.cgi?article=1273&context=agstatconference (accessed on 17 October 2021).
- Lüdecke, D. ggeffects: Tidy Data Frames of Marginal Effects from Regression Models. J. Open Source Softw. 2018, 3. [Google Scholar] [CrossRef] [Green Version]
- RStudio Team. RStudio: Integrated Development Environment for R; RStudio: Boston, MA, USA, 2021; Available online: https://www.rstudio.com/ (accessed on 17 October 2021).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013; Available online: https://www.R-project.org/ (accessed on 17 October 2021).
- Waschki, B.; Spruit, M.A.; Watz, H.; Albert, P.S.; Shrikrishna, D.; Groenen, M.; Smith, C.; Man, W.D.-C.; Tal-Singer, R.; Edwards, L.; et al. Physical activity monitoring in COPD: Compliance and associations with clinical characteristics in a multicenter study. Respir. Med. 2012, 106, 522–530. [Google Scholar] [CrossRef] [Green Version]
- Ohashi, C.; Akiguchi, S.; Ohira, M. Development of a Remote Health Monitoring System to Prevent Frailty in Elderly Home-Care Patients with COPD. Sensors 2022, 22, 2670. [Google Scholar] [CrossRef]
- Cordova, F.C.; Ciccolella, D.; Grabianowski, C.; Gaughan, J.; Brennan, K.; Goldstein, F.; Jacobs, M.R.; Criner, G.J. A Telemedicine-Based Intervention Reduces the Frequency and Severity of COPD Exacerbation Symptoms: A Randomized, Controlled Trial. Telemed. e-Health 2016, 22, 114–122. [Google Scholar] [CrossRef] [Green Version]
- Tomasic, I.; Tomasic, N.; Trobec, R.; Krpan, M.; Kelava, T. Continuous remote monitoring of COPD patients—justification and explanation of the requirements and a survey of the available technologies. Med. Biol. Eng. Comput. 2018, 56, 547–569. [Google Scholar] [CrossRef] [Green Version]
- Bestall, J.; Paul, E.; Garrod, R.; Garnham, R.; Jones, P.; Wedzicha, J. Longitudinal trends in exercise capacity and health status after pulmonary rehabilitation in patients with COPD. Respir. Med. 2003, 97, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, A.R.; Gowler, H.; Curtis, F.; Holden, N.S.; Bridle, C.; Jones, A.W. Efficacy of supervised maintenance exercise following pulmonary rehabilitation on health care use: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 257–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health and Care Excellence (NICE). Chronic Obstructive Pulmonary Disease in over 16s: Diagnosis and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2019. [Google Scholar]
- Spruit, M.A.; Pitta, F.; McAuley, E.; ZuWallack, R.L.; Nici, L. Pulmonary Rehabilitation and Physical Activity in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2015, 192, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.-C.; et al. An Official American Thoracic Society/European Respiratory Society Statement: Key Concepts and Advances in Pulmonary Rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef]
- Nici, L.; ZuWallack, R. An Official American Thoracic Society Workshop Report: The Integrated Care of the COPD Patient. Proc. Am. Thorac. Soc. 2012, 9, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Corlateanu, A.; Montanari, G.; Botnaru, V. Influence of age in the functional status of COPD patients. Eur. Respir. J. 2014, 44, P1456. [Google Scholar]
- Tudorache, E.; Fildan, A.P.; Frandes, M.; Dantes, E.; Tofolean, D.E. Aging and extrapulmonary effects of chronic obstructive pulmonary disease. Clin. Interv. Aging 2017, 12, 1281–1287. [Google Scholar] [CrossRef] [Green Version]
- Hartman, J.; Boezen, H.M.; Zuidema, M.J.; De Greef, M.H.; Hacken, N.H.T. Physical Activity Recommendations in Patients with Chronic Obstructive Pulmonary Disease. Respiration 2014, 88, 92–100. [Google Scholar] [CrossRef]
- Luk, E.K.; Khan, F.; Irving, L. Maintaining Gains Following Pulmonary Rehabilitation. Lung 2015, 193, 709–715. [Google Scholar] [CrossRef]
- Guo, Y.; Logan, H.L.; Glueck, D.H.; E Muller, K. Selecting a sample size for studies with repeated measures. BMC Med. Res. Methodol. 2013, 13, 100. [Google Scholar] [CrossRef] [Green Version]
- Gillissen, A.; Marseille, A.; Skowasch, D.; Ritz, J.; Mattiucci-Guehlke, M.; Pabst, S.; Greulich, T.; Koczulla, R. Health and functional status of tiotropium/olodaterol-treated patients with COPD: Results from the AERIAL® non-interventional study. ERJ Open Res. 2021, 7, 4. [Google Scholar] [CrossRef]
- Vogelmeier, C.F.; Román-Rodríguez, M.; Singh, D.; Han, M.K.; Rodríguez-Roisin, R.; Ferguson, G.T. Goals of COPD treatment: Focus on symptoms and exacerbations. Respir. Med. 2020, 166, 105938. [Google Scholar] [CrossRef] [PubMed]
| Characteristics (n = 108) | |
|---|---|
| Age, years—mean (SD) | 66.9 (9.5) |
| Male | 89 (82.4) |
| BMI, kg/m2—mean (SD) | 26.9 (4.4) |
| Educational level, years | |
| ≤4 (ISCED 0–1) | 52 (48.1) |
| 5–9 (ISCED 2) | 29 (26.9) |
| ≥10 (ISCED 3–8) | 27 (25.0) |
| Smoking status | |
| Never | 13 (12.0) |
| Former | 81 (75.0) |
| Current | 14 (13.0) |
| Pack-years—median (Q1–Q3) | 45.0 (17.7–75.9) |
| mMRC—median (IQR) | 1 (1.0; 2.0) |
| AECOPD, in previous year | |
| 0 | 79 (73.1) |
| 1 | 10 (9.3) |
| >1 | 19 (17.6) |
| Lung function | |
| FEV1, % predicted—median (Q1–Q3) | 58.0 (41.0–75.0) |
| FEV1/FVC—median (Q1–Q3) | 54.7 (45.3–63.0) |
| GOLD grades | |
| 1 | 23 (21.3) |
| 2 | 44 (40.7) |
| 3 | 27 (25.0) |
| 4 | 13 (12.0) |
| CAT, total score—median (Q1–Q3) | 11.0 (8.0–18.0) |
| Long-term oxygen therapy | 16 (15.0) |
| Non-invasive ventilation | 18 (16.7) |
| GOLD groups | |
| A | 39 (36.1) |
| B | 47 (43.5) |
| C | 1 (0.9) |
| D | 21 (19.4) |
| CCI score | |
| Mild (1–2 points) | 25 (23.1) |
| Moderate (3–4 points) | 58 (53.8) |
| Severe (≥5 points) | 25 (23.1) |
| Medication | |
| Bronchodilators | |
| ICS | 11 (10.2) |
| LAMA | 23 (21.3) |
| SABA | 16 (14.8) |
| LABA | 10 (9.3) |
| SAMA | 1 (0.9) |
| Combination ICS/LABA | 31 (28.7) |
| Combination LABA/LAMA | 34 (31.5) |
| Combination LABA/LAMA/ICS | 2 (1.9) |
| Xanthines | 11 (10.2) |
| Expectorants | 6 (5.6) |
| LTRA | 5 (4.6) |
| Anti-fibrotics/ Immunosuppressants | 1 (0.9) |
| 1minSTS, number of repetitions—median (Q1–Q3) | 25.5 (21.0–30.3) |
| <70% predicted | 45 (41.7) |
| ≥70% predicted | 63 (58.3) |
| (n = 108) | 1minSTS |
|---|---|
| Fixed effects (factors) | Estimate (95%CI) |
| (Intercept) | 78.23 (63.55; 92.90) |
| Sex (Female) | −4.19 (−8.15; −0.23) |
| Age | −0.48 (−0.64; −0.32) |
| BMI | −0.51 (−0.84; −0.17) |
| mMRC | −2.89 (−4.24; −1.55) |
| Time | 0.08 (0.03; 0.12) |
| Sex (Female) * Time | 0.02 (−2.57 × 10 −4; 0.03) |
| Age * Time | −8.89 ×10−4 (−1.61 ×10−3; −1.86 ×10−4) |
| Random Effects | |
| σ2 | 9.84 |
| τ00 | 52.90Participant |
| τ11 | 0.01Participant.Time |
| ρ01 | 0.47Participant |
| Observations | 535 |
| Marginal/Conditional R2 | 0.37/0.92 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rocha, V.; Cabral, J.; Souto-Miranda, S.; Machado, A.F.; Jácome, C.; Cruz, J.; Martins, V.; Simão, P.; Mendes, M.A.; Afreixo, V.; et al. Monthly Follow-Ups of Functional Status in People with COPD: A Longitudinal Study. J. Clin. Med. 2022, 11, 3052. https://doi.org/10.3390/jcm11113052
Rocha V, Cabral J, Souto-Miranda S, Machado AF, Jácome C, Cruz J, Martins V, Simão P, Mendes MA, Afreixo V, et al. Monthly Follow-Ups of Functional Status in People with COPD: A Longitudinal Study. Journal of Clinical Medicine. 2022; 11(11):3052. https://doi.org/10.3390/jcm11113052
Chicago/Turabian StyleRocha, Vânia, Jorge Cabral, Sara Souto-Miranda, Ana Filipa Machado, Cristina Jácome, Joana Cruz, Vitória Martins, Paula Simão, Maria Aurora Mendes, Vera Afreixo, and et al. 2022. "Monthly Follow-Ups of Functional Status in People with COPD: A Longitudinal Study" Journal of Clinical Medicine 11, no. 11: 3052. https://doi.org/10.3390/jcm11113052
APA StyleRocha, V., Cabral, J., Souto-Miranda, S., Machado, A. F., Jácome, C., Cruz, J., Martins, V., Simão, P., Mendes, M. A., Afreixo, V., & Marques, A. (2022). Monthly Follow-Ups of Functional Status in People with COPD: A Longitudinal Study. Journal of Clinical Medicine, 11(11), 3052. https://doi.org/10.3390/jcm11113052








